Back to Journals » Cancer Management and Research » Volume 14
Effects of Radiotherapy on Survival of Esophageal Cancer Patients Receiving Immunotherapy: Propensity Score Analysis and Nomogram Construction
Authors Nie Y , Yao G, Li L, Feng A, Zhang W, Xu X, Li Q, Yang Z
Received 9 June 2022
Accepted for publication 27 July 2022
Published 7 August 2022 Volume 2022:14 Pages 2357—2371
DOI https://doi.org/10.2147/CMAR.S375821
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Yuanliu Nie,1 Guangyue Yao,1 Liang Li,2 Alei Feng,3 Wentao Zhang,4 Xiaoying Xu,5 Qiang Li,1,3 Zhe Yang1,3
1Tumor Research and Therapy Center, Shandong Provincial Hospital, Shandong University, Jinan, Shandong, 250021, People’s Republic of China; 2Department of Thoracic Surgery, Shandong Provincial Hospital, Shandong University, Jinan, Shandong, 250021, People’s Republic of China; 3Tumor Research and Therapy Center, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, Shandong, 250021, People’s Republic of China; 4Shandong First Medical University, Jinan, Shandong, 250021, People’s Republic of China; 5Shandong First Medical University, College of Basic Medicine, Shandong First Medical University-Shandong Academy of Medical Sciences, Jinan, Shandong, 250000, People’s Republic of China
Correspondence: Qiang Li; Zhe Yang, Tumor Research and Therapy Center, Shandong Provincial Hospital, Shandong University, Jinan, Shandong, 250021, People’s Republic of China, Tel +86 15053162586; +86 13791089059, Email [email protected]; [email protected]
Purpose: The present study assessed the effects of radiotherapy on overall survival (OS) and progression-free survival time (PFS) in patients with stage II or higher esophageal cancer receiving immunotherapy; evaluated factors independently prognostic of OS and PFS in these patients; and utilized these factors to establish a prognostic nomogram.
Patients and Methods: This study enrolled 134 patients with stage II or higher esophageal cancer treated with chemotherapy (platinum-based agents plus paclitaxel or fluorouracil) and immunotherapy. These patients were divided into two groups, a radiotherapy (RT) group (n = 55) and a non-radiotherapy (non-RT) group (n = 79). Following 1:1 propensity score matching, OS and PFS were compared by the Kaplan–Meier method, and factors associated with survival were determined by univariate and multifactorial Cox regression analyses. These factors were used to construct a prognostic nomogram.
Results: After propensity matching, all covariates were well balanced in the two groups (all P > 0.05). After matching, both median PFS (15.70 months [95% confidence interval (CI) 8.68– 22.72 months] vs 5.70 months [95% CI 3.38– 8.02 months], P = 0.002) and median OS (15.72 months [95% CI 12.94– 18.46 months] vs 12.06 months [95% CI 9.91– 14.20 months], P = 0.036) were significantly longer in the RT than in the non-RT group. Univariate and multifactorial analyses showed that RT, neutrophil-lymphocyte ratios, and tumor differentiation were independently prognostic of OS, with all hazard ratios (HRs) < 1 and all P-values < 0.05. A nomogram based on these factors was constructed, and its accuracy was verified.
Conclusion: Immunotherapy plus RT resulted in better survival outcomes than immunotherapy alone. A nomogram based on prognostic factors can guide personalized treatment and monitor prognosis.
Keywords: prognosis, combination therapy, survival, neutrophil-lymphocyte ratio, NLR
Introduction
Esophageal cancer is the sixth leading killer of all types of cancer worldwide,1 with more than 50% of patients worldwide living in China.2 Although surgery, endoscopic therapy, radiotherapy, chemotherapy, and immunotherapy have been utilized in the comprehensive treatment of esophageal cancer, patients with this disease have a poor prognosis, with 5-year overall survival (OS) rates of 15% to 25%.3,4 Late diagnosis is one of the main causes of poor prognosis, as most patients are diagnosed with advanced stage tumors, making them ineligible for surgery and endoscopic treatment.5,6 Treatment of these patients consists of combinations of radiotherapy and chemotherapy,5,6 with platinum- and fluoropyrimidine-containing agents commonly used to treat advanced esophageal cancer.7 These chemotherapy agents, however, are frequently associated with cytotoxic side effects.
Immunotherapy, including immune checkpoint inhibitors (ICIs) such as monoclonal antibodies targeting anti-programmed cell death protein 1 (PD-1) and its ligand (PD-L1), has been shown effective against several types of solid tumors, including esophageal cancer.8 Although these agents have been associated with significantly prolonged OS in patients with esophageal cancer, only a small proportion of patients can benefit from ICIs alone.9,10 Studies are needed to determine whether combinations of immunotherapy with and other types of treatment can prolong survival in patients with esophageal cancer.
The KEYNOTE-590 trial (NCT03189719) found that pembrolizumab plus chemotherapy significantly improved progression-free survival (PFS) and OS in patients with advanced esophageal or esophagogastric junction (EGJ) cancer when compared with chemotherapy alone (ie 5-fluorouracil plus cisplatin).7,11 Moreover, the combination of radiotherapy plus immunotherapy has shown benefits in some patients with metastatic cancer. Radiotherapy can trigger a systemic anti-tumor response, which is enhanced by immunotherapy.12 In addition, the ability of radiotherapy to kill tumor cells may increase the effect of immunotherapy.13 A Phase Ib clinical study showed that patients with locally advanced esophageal squamous cell carcinoma treated with a combination of the anti-PD1 monoclonal antibody camrelizumab and radiotherapy have a longer median OS (15.3 months vs 12.0 months) and a 30% lower risk of death than patients treated with camrelizumab alone.10 Moreover, ICIs combined with other treatments were shown to improve the efficacy of ICIs alone in patients with esophageal cancer.7,14
An increase in the number of lymphocytes in the tumor microenvironment has been associated with better patient prognosis.15 In addition, neutrophils produced in these microenvironments were shown to be prognostic in patients with head and neck tumors.16 Neutrophil-lymphocyte ratio (NLR) in peripheral blood was shown to be a prognostic indicator in patients with various malignant tumors.17,18 However, the ability of NLRs following immunotherapy to predict outcomes in patients with esophageal cancer remains unclear. Factors associated with the prognosis of patients with esophageal cancer include age, pathological tumor type, primary tumor site, tumor grade, radiotherapy and surgery.19 Although identifying independent prognostic factors is important for selecting appropriate treatment strategies, few studies have assessed factors predictive of survival in patients with esophageal cancer receiving immunotherapy. The present study analyzed the effects of radiotherapy on OS and PFS in patients with stage II or higher esophageal cancer receiving immunotherapy, evaluated factors independently prognostic factor of survival outcomes, and utilized these factors to establish a prognostic nomogram.
Patients and Methods
Patient Selection
This single-center, Phase II cohort study enrolled patients with esophageal cancer who had received at least four cycles of immunotherapy combined with first-line chemotherapy, consisting of platinum-based drugs plus paclitaxel or fluorouracil-based agents, in the Provincial Hospital of Shandong First Medical University between January 2019 and January 2022. Electronic patient records were examined retrospectively, and relevant data were recorded. Patients were excluded if their esophageal malignancy was not the first or only primary malignancy; if they did not have stage II–IV esophageal cancer, as determined by the American Joint Committee on Cancer (AJCC) eighth edition; or if a pathological diagnosis was missing from patient records. Patients were also excluded if they were allergic to or had contraindications to immunotherapy drugs; if they also had other serious underlying diseases, such as cardiovascular disease or abnormal liver or kidney function; if they had experienced a disturbance of consciousness or cognitive impairment; or if their medical records were incomplete. Patients with unknown survival status who did not receive systemic chemotherapy and immunotherapy were also excluded.
The study enrolled 134 eligible patients, divided into two groups: a radiotherapy (RT) group, consisting of 55 patients who received chemotherapy, immunotherapy, and RT; and a non-RT group, consisting of 79 patients who received group chemotherapy and immunotherapy. Treatment strategies were based on pathological and imaging findings, including the results of contrast-enhanced computed tomography (CT) and/or magnetic resonance imaging (MRI) and endoscopic ultrasonography. Most patients received at least four 3-week cycles of cisplatin and fluorouracil/paclitaxel. Specifically, patients received intravenous infusions of cisplatin (60 mg/m2) on day 1 of each cycle; and continuous microinfusions of 5-fluorouracil (1 g/m2/day) on days 1–2 or intravenous infusions of paclitaxel (150 mg/m2) on day 1. Immunotherapy consisted of a single dose of 200 mg of camrelizumab/pembrolizumab.
Patients were started on intensity-modulated RT (IMRT) on day 1 of the first cycle of chemotherapy, consisting of 30 fractions of 2 Gy each, for a total irradiation dose of 60 Gy. In IMRT, the intensity of the radiation beam is modulated based on an optimized algorithm, optimizing uniform to tumor treatment and overall dosimetry results.20,21
The study protocol was approved by the Ethics Committee of Provincial Hospital affiliated to Shandong University (LCYJ: No.2019–090), and all data were anonymized. Each included patient provided written informed consent.
Data Collection
The clinicopathological characteristics of the 134 patients were recorded, including demographic characteristics, such as gender and age; pathologic characteristics, including tumor location, size, pathological type, local infiltration, stage, and treatment; neutrophil and lymphocyte counts and their ratio after treatment; disease progression; and survival status. Side effects during treatment were also recorded, including bone marrow suppression, gastrointestinal adverse events (eg nausea, and vomiting), immune-related adverse reactions (eg immune myocarditis, immune acute kidney injury, and immune hepatitis), arthritis, and hair loss. Myelosuppression was defined as an absolute neutrophil count <1.5*10^9/L or an absolute platelet count <70*10^9/L. Immune myocarditis was based on the results of endomyocardial biopsy22 or on guideline-recommended clinical scores for suspected myocarditis, calculated from clinical blood biomarkers, imaging features, and item data.23 Immune-induced acute kidney injury (AKI) was defined as a ≥1.5-fold increase in serum creatinine (SCr) concentration from baseline within 6 months of starting ICI therapy at our center.24,25 Immune hepatitis was defined as asymptomatic increases in liver transaminases and bilirubin, with or without fever, after immunotherapy despite normal liver function test results at baseline before initial treatment. Hepatitis was defined as AST/ALT levels >5 times the upper limit of normal (ULN) or bilirubin levels >3 times ULN.26
Contrast-enhanced CT and MRI were used to delineate the target volume for RT, tumor TNM stage, and the efficacy of RT. Two pathologists confirmed the pathological type and differentiation of each esophageal tumor, both by observation and hematoxylin-eosin (HE) staining. TNM stage was determined according to the 8th edition of the AJCC TNM staging guidelines.
Patients were followed-up every 3 months for 1 year and every 6 months for the next 2 years until disease progression. Follow-up included routine blood tests; barium swallowing; enhanced CT of the upper gastrointestinal tract, abdomen, and chest; and quality of life assessment. The numbers of granulocytes and lymphocytes were measured in blood samples obtained after treatment, and their ratio was calculated. The last follow-up was performed on January 22, 2022.
Measurement of for Hematologic Biomarkers
Neutrophil, lymphocyte, and granulocyte counts, along with NLR and granulocyte-to-lymphocyte ratios after treatment of 88 patients with esophageal cancer were determined using X-tile software (Figure 1). The optimal critical values were determined based on survival status and OS using the minimum P-value method, with these critical values considered categorical variables.27 Specifically, patients with absolute numbers of neutrophils ≤ 9.5*10^9/L and >9.5*10^9/L were considered the low and high neutrophil groups, respectively; patients with absolute numbers of lymphocytes ≤ 0.5 *10^9/L and >0.5*10^9/L were considered the low and high lymphocyte groups, respectively; and patients with NLRs ≤ 8.9 and > 8.9 were considered the low and high NLR groups, respectively.
Propensity Score Matching (PSM)
To reduce the risk of confounding bias in this cohort, patients in the RT and non-RT groups were subjected to 1:1 propensity score matching (PSM) using RStudio.28 Data in each group were pooled using the Create Table One package. PSM baseline variables included sex, age, tumor differentiation, adverse effects, and tumor pathology, with these variables used to balance the baseline characteristics of the two groups. Propensity scores (PS) were determined by logistic regression analysis, with the nearest neighbor method used to assess balance and overlap. Categorical variables were expressed as numbers and frequencies (%), whereas continuous variables were expressed as medians ranges or means ± standard deviations. The means of continuous variables were compared using independent sample t-tests. Categorical variables were compared using the Pearson x2 test. P-values were calculated for each parameter before and after matching. PSM yielded 44 matched patients in each group.
Survival Analysis
PFS was defined as the period from the start of immunotherapy to the first disease progression after immunotherapy, to the second progression after RT, or to death from any cause. OS was defined as the period from the onset of immunotherapy to death from any cause or last follow-up.
OS and PFS in the two PSM groups and between-group differences in NLR after treatment were analyzed by the Kaplan–Meier method and compared by Log rank tests, as well as by regression analysis, all performed using SPSS software. All the variables shown in Table 1 were also subjected to univariate and multivariate Cox regression analyses using RStudio software. Variables with P<0.2 on univariate analyses were included in the multivariate analysis to determine factors independently prognostic of OS. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated to assess the relationship between survival time and prognostic factors.
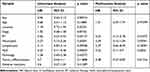 |
Table 1 Univariate and Multivariate Analysis of Factors Prognostic of Overall Survival (OS) |
Creation of the Nomogram
Nomograms predicting OS after 0.5, 1, and 2 years OS for each patient in the cohort were constructed from the variables found to be statistically significant on multivariate analysis. The performance of the nomogram was assessed by time-dependent subject receiver operating characteristic curves (ROC), calibration curves, and decision curve analysis (DCA). The sensitivity and specificity of columnar plots for predicting efficacy were assessed using ROC; calibration curves were plotted to estimate consistent accuracy for OS at 0.5, 1, and 2 years; and the validity and clinical utility of columnar plots were validated using DCA to quantify the net benefit of columnar plots relative to those assessed using NLR or RT alone.
Statistical Analysis
Statistical analyses were per formed using IBM SPSS Statistics 25 (IBM, Inc., Armonk, NY), X-tile 3.6.1 (Yale University, New Haven, CT, USA) and R version 4.1.2 (https:\www.R-project.org\) software, with the R package including “rms”, “knitr”, “kableExtra”, “tableone”, “MatchIt”, “Matching”, “rms”, “survivalsvm”, “ggplot2”, “survminer”, “survival”, and “timeROC”. Except for the one-way analysis, in which P<0.2 was considered significant, P<0.05 was considered statistically significant.
Results
Patient Characteristics and PSM Analysis
Clinical information was obtained from 134 patients who received immunotherapy for intermediate to advanced esophageal cancer, including 55 who also received RT and 79 who did not (Table 2). The clinicopathological characteristics of all patients are shown in Table 2 and baseline characteristics before and after PSM are shown in Table 3. Before PSM, the RT and non-RT groups showed significant differences in esophageal lesion location (P=0.024), NLR (P=0.006), and degree of tumor differentiation (P=0.047). To exclude the influence of confounding factors, 1:1 PSM was performed, resulting in matching of 44 patients in the RT and 44 in the non-RT group. After matching, all covariates were well balanced in the two groups, with all the baseline characteristics being similar (all P>0.05; Table 3).
 |
Table 2 Demographic and Clinical Characteristics of Included Patients |
 |
Table 3 Clinicopathologic Characteristics of Patients Before and After Propensity Score Matching |
To assess the effect of RT on patient outcomes, PFS and OS of patients in the two groups were analyzed before and after PSM. Kaplan–Meier analysis of all 134 patients showed that both OS (16.35 months [95% CI 13.94–18.76 months] vs 10.80 months [95% CI 9.31–12.29 months, P < 0.001; Figure 2A) and PFS (15.6 months [95% CI 9.87–21.33 months] vs 6.15 months [95% CI 4.16–8.19 months], P < 0.001; Figure 2B) were significantly longer in the RT than in the Non-RT group.
Kaplan–Meier analysis of the PSM cohort of 88 patients after matching also showed that both OS (15.72 months [95% CI 12.94–18.46 months] vs 12.06 months [95% CI 9.91–14.20 months], P=0.036; Figure 2C) and PFS (15.70 months [95% CI 8.68–22.72 months] vs 5.70 months [95% CI 3.38–8.02 months], P=0.002; Figure 2D) remained significantly longer in the RT than in the Non-RT group.
Univariate and Multivariate Analyses of Factors Associated with Survival
Univariate analysis of the 88 patients in the PSM cohort showed that age, RT, neutrophil and lymphocyte counts, NLR, and tumor differentiation were each significantly associated with OS (all p <0.20), with all HRs <1 (Table 1). Factors with p <0.20 on univariate analysis were entered into the multivariate model, with multivariate Cox regression analysis showing that RT (p=0.01075; HR=0.33, 95% CI:0.14–0.78), NLR (p=0.0302; HR=0.32, 95% CI:0.11–0.9), and tumor differentiation (p=0.01216; HR=0.48, 95% CI:0.27–0.85) were independently prognostic of OS, whereas age and neutrophil and lymphocyte counts were not (all P>0.05). Figure 3 shows forest plots of these factors for OS.
 |
Figure 3 Forest plots of clinicopathologic characteristics in the RT and Non-RT groups by (A) univariate and (B) multivariate analyses. P-values were calculated using the Cox regression model. |
The effect of RT on post-treatment granulocytosis ratio was assessed by comparing NLR with granulocytosis ratio in the RT and non-RT groups. Because the data were not normally distributed, NLR was logarithmically transformed, resulting in a normal distribution (Figure 4A). Linear regression analysis of the relationship between the logarithm of NLR and granulocytosis ratio showed that granulocytosis ratio was significantly lower in the RT than in the non-RT group (p < 0.001; Figure 4B).
Prognostic Nomogram for OS and Internal Validation of Predictive Accuracy
To better predict OS at 0.5, 1, and 2 years in patients with esophageal cancer after receiving immunotherapy, a nomogram model was designed; this easy-to-use tool was based on the independent predictors of OS calculated determined by multivariate Cox regression analysis (Table 1). The nomogram (Figure 5) depicts the predictors of OS. The calibration curves for the probability of survival at 0.5, 1, and 2 years after treatment showed that the nomogram prediction was consistent with actual clinical outcomes (Figure 6A). Further comparison of the ROC curves (Figure 6B) showed that the clinical responses using this nomogram had AUCs of 0.860, 0.822, and 0.859 at 0.5, 1, and 2 years, respectively, indicating that the nomogram was both sensitive and specific in predicting OS. Decision curve analysis (DCA) validated the clinical validity of the nomogram (Figure 6C). The net benefit of using the nomogram was consistently higher than other prediction models, such as NLR and RT alone, in predicting OS at 0.5, 1, and 2 years. Taken together, these findings indicated that the nomogram is accurate in predicting survival in patients with esophageal cancer.
Discussion
To our knowledge, this study is the first to use a PSM cohort to assess the effects of RT on the prognosis of esophageal cancer patients treated with immunotherapy. Kaplan–Meier analysis showed that OS and PFS were significantly longer in the RT than in the non-RT group, both before and after PSM. PSM is a statistical method that matches baseline covariates in a population and reduces the limitations of multivariate models. By reducing the effects of confounding factors on the results, PSM improves the accuracy of prediction. PSM is also widely used to assess the effectiveness of a certain treatment on outcomes.29–32
Following PSM of the RT and non-RT groups, none of the possible confounding factors, such as lesion location, NLR (>8.9 or ≤8.9), and tumor differentiation, differed significantly. Both PFS and OS in the PSM cohort were significantly longer in esophageal cancer patients treated with chemotherapy + immunotherapy combined with concurrent RT than in patients treated with chemotherapy + immunotherapy alone. Similar results were observed in the multicenter, phase II TENERGY trial, which, despite the lack of PSM, found that the combination of chemoradiotherapy and the anti-PD-L1 monoclonal antibody atezolizumab significantly increased the confirmed complete response rate, thus improving patient survival.33
Changes in the tumor microenvironment (TME) are closely associated with tumor progression and patient prognosis.34–36 The TME responds to changes in neutrophil and lymphocyte counts, as well as to proteins such as plasma fibrinogen and serum albumin, indicators that play important roles in immune and inflammatory responses to cancer.37 NLR is an indicator of prognosis in patients with esophageal cancer, with higher NLR associated with a later TNM stage and poorer prognosis.38,39 NLR is therefore receiving increasing attention as a potential predictive marker for patients receiving ICI therapy.
The present study found that post-treatment NLR was significantly lower in patients who received RT plus immunotherapy than in those who received immunotherapy alone. Inclusion of clinicopathological data, neutrophil and lymphocyte counts, and NLR in univariate and multivariate Cox regression analyses showed that RT, NLR, and tumor differentiation were independently prognostic of survival. In contrast, age was not a prognostic risk factor, perhaps because these patients had stage II and higher esophageal cancer, with worsening of some chronic underlying diseases of the cardiovascular system.19 Factors independently prognostic of survival, including RT, NLR, and tumor differentiation, were therefore included in a nomogram to predict 0.5, 1, and 2 year OS in patients with esophageal cancer receiving immunotherapy. Use of this nomogram may enable more effective individualized management of patients.
Clinical prediction models, such as nomograms is a statistical tool that combines clinicopathological factors in predictive models, which are both simple and intuitive.40,41 Nomograms have been widely used in the prognostic evaluation of patients with several diseases, including gastric cancer and rectal cancer.42,43 The present study showed that the developed nomogram was predictive of patient prognosis. ROC, calibration, and decision curve analyses showed that this nomogram was sensitive, accurate, and valid, respectively, in predicting OS. The AUC of ROC curves could determine the sensitivity and specificity of the nomogram,44 whereas DCA was based on a threshold probability to determine the clinical decision with the greatest net benefit.45 This nomogram was found to accurately predict OS within 2 years based on a history of RT, NLR, and the degree of tumor differentiation. In addition, the AUCs for 0.5, 1, and 2 year OS were higher than 0.80, indicating good predictive sensitivity.
The predictive model also showed that RT enhanced OS and PFS, suggesting that the combination of RT and immunotherapy can improve the prognosis of patients with esophageal cancer. The prognosis of patients with esophageal cancer was also affected by the degree of tumor cell differentiation. For example, a retrospective analysis in patients with esophageal squamous cell carcinoma found that tumor size, depth of tumor invasion, degree of tumor differentiation, and lymphovascular invasion were significantly predictors of lymph node metastasis (LNM).46 These findings were consistent with the present results, which suggested that patients with well-differentiated pathology on the nomogram had lower scores and a better prognosis. Therefore, the early pathological diagnosis of esophageal cancer patients is important in evaluating patient prognosis. The present study also found that patients with low NLR (<8.9) had a better prognosis. Similarly, a previous meta-analysis found that high NLR before treatment was an indicator of poor prognosis in patients with solid tumors.47
The present study described the development of a new nomogram by evaluating the effect of RT combined with immunotherapy on survival in patients with esophageal cancer and assessed the ability of the nomogram to predict 2-year OS. Immunotherapy can synergize with RT to achieve a better anti-tumor effect. However, RT can induce side effects, such as radiation pneumonitis and radiation esophagitis.48,49
The present study had several limitations, the most important being its retrospective design. Patients or their family members may have recall bias for treatment status and time of death during follow-up, resulting in errors. In addition, this study included only 134 patients, with the small number possibly affecting the robustness of the results. Multicenter, prospective studies with larger sample size and longer follow-up are therefore needed. Third, this study did not assess whether the pre-treatment level of PD-L1 expression could affect patient outcomes, suggesting the need for subsequent studies to investigate whether a high level of PD-L1 expression is indicative of the efficacy of RT plus immunotherapy.
Conclusion
RT plus immunotherapy resulted in significantly longer OS and PFS when compared with immunotherapy alone in patients with stage II or higher esophageal cancer. Predictive models that include NLR, RT, and tumor differentiation can guide personalized treatment or monitor prognosis.
Abbreviations
RT, radiation therapy; Non-RT, no radiation therapy; NLR, neutrophil-to-lymphocyte ratio; ROC, receiver operating characteristic; PFS, progression-free survival; AUC, area under the ROC curve; OS, overall survival; ESCC, esophageal cell squamous carcinoma; SCEC, small cell esophageal carcinoma; NET, neuroendocrine tumor; HGIN, high-grade intraepithelial neoplasia; LGIEN, low-grade intraepithelial neoplasia; EAC, esophageal adenocarcinoma; HR, hazard ratio; CI, confidence interval.
Ethics Statement
The study protocol was approved by the Ethics Committee of Provincial Hospital affiliated to Shandong University (LCYJ: No.2019-090) and conformed to the guidelines of the Declaration of Helsinki. All data were anonymized, and each included patient provided written informed consent.
Patient Consent
All participants in this study were informed of its purpose and provided both written and verbal informed consent. The collected data were checked for completeness. A copy of the written consent form is available for review by the Editor-in-Chief of this journal upon request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Beijing Xisike Clinical Oncology Research Foundation (grant number Y-2019AZMS-0522); the Natural Science Foundation of Shandong Province (grant number ZR2020MH229) and the Xisike - 2019 Qilu Oncology Research Fund Project (grant number Y-QL2019-0149).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ajani JA, D’Amico TA, Bentrem DJ, et al. Esophageal and esophagogastric junction cancers, version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17(7):855–883. doi:10.6004/jnccn.2019.0033
2. Zhang Z, Yu X, Guo Y, Song W, Yu D, Zhang X. Genetic variant in CASP3 affects promoter activity and risk of esophageal squamous cell carcinoma. Cancer Sci. 2012;103(3):555–560. doi:10.1111/j.1349-7006.2011.02173.x
3. Gupta B, Kumar N. Worldwide incidence, mortality and time trends for cancer of the oesophagus. Eur J Cancer Prev. 2017;26(2):107–118. doi:10.1097/CEJ.0000000000000249
4. Kato H, Nakajima M. Treatments for esophageal cancer: a review. Gen Thorac Cardiovasc Surg. 2013;61(6):330–335. doi:10.1007/s11748-013-0246-0
5. Uhlenhopp DJ, Then EO, Sunkara T, Gaduputi V. Epidemiology of esophageal cancer: update in global trends, etiology and risk factors. Clin J Gastroenterol. 2020;13(6):1010–1021. doi:10.1007/s12328-020-01237-x
6. Oh SJ, Han S, Lee W, Lockhart AC. Emerging immunotherapy for the treatment of esophageal cancer. Expert Opin Investig Drugs. 2016;25(6):667–677. doi:10.1517/13543784.2016.1163336
7. Kato K, Shah MA, Enzinger P, et al. KEYNOTE-590: phase III study of first-line chemotherapy with or without pembrolizumab for advanced esophageal cancer. Future Oncol. 2019;15(10):1057–1066. doi:10.2217/fon-2018-0609
8. Chen XX, Zhong Q, Liu Y, et al. Genomic comparison of esophageal squamous cell carcinoma and its precursor lesions by multi-region whole-exome sequencing. Nat Commun. 2017;8(1):524. doi:10.1038/s41467-017-00650-0
9. Noman MZ, Parpal S, Van Moer K, et al. Inhibition of Vps34 reprograms cold into hot inflamed tumors and improves anti-PD-1/PD-L1 immunotherapy. Sci Adv. 2020;6(18):eaax7881. doi:10.1126/sciadv.aax7881
10. Zhang W, Yan C, Gao X, et al. Safety and feasibility of radiotherapy plus camrelizumab for locally advanced esophageal squamous cell carcinoma. Oncologist. 2021;26(7):e1110–e1124. doi:10.1002/onco.13797
11. Sun JM, Shen L, Shah MA, et al.; for KEYNOTE-590 Investigators. Pembrolizumab plus chemotherapy versus chemotherapy alone for first-line treatment of advanced oesophageal cancer (KEYNOTE-590): a randomised, placebo-controlled, phase 3 study. Lancet. 2021;398(10302):759–771. doi:10.1016/S0140-6736(21)01234-4
12. Azad A, Yin Lim S, D’Costa Z, et al. PD-L1 blockade enhances response of pancreatic ductal adenocarcinoma to radiotherapy. EMBO Mol Med. 2017;9(2):167–180. doi:10.15252/emmm.201606674
13. Luke JJ, Lemons JM, Karrison TG, et al. Safety and clinical activity of pembrolizumab and multisite stereotactic body radiotherapy in patients with advanced solid tumors. J Clin Oncol. 2018;36(16):1611–1618. doi:10.1200/JCO.2017.76.2229
14. Doi T, Piha-Paul SA, Jalal SI, et al. Safety and antitumor activity of the anti-programmed death-1 antibody pembrolizumab in patients with advanced esophageal carcinoma. J Clin Oncol. 2018;36(1):61–67. doi:10.1200/JCO.2017.74.9846
15. Gooden MJM, de Bock GH, Leffers N, Daemen T, Nijman HW. The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with meta-analysis. Br J Cancer. 2011;105(1):93–103. doi:10.1038/bjc.2011.189
16. Huang SH, Waldron JN, Milosevic M, et al. Prognostic value of pretreatment circulating neutrophils, monocytes, and lymphocytes in oropharyngeal cancer stratified by human papillomavirus status. Cancer. 2015;121(4):545–555. doi:10.1002/cncr.29100
17. Bruix J, Cheng AL, Meinhardt G, Nakajima K, De Sanctis Y, Llovet J. Prognostic Factors and predictors of sorafenib benefit in patients with hepatocellular carcinoma: analysis of two phase III studies[J Hepatol 67 (2017) 999–1008]. J Hepatol. 2018;69(4):990–991. doi:10.1016/j.jhep.2018.07.015
18. Li Y, Wang C, Xu M, et al. Preoperative NLR for predicting survival rate after radical resection combined with adjuvant immunotherapy with CIK and postoperative chemotherapy in gastric cancer. J Cancer Res Clin Oncol. 2017;143(5):861–871. doi:10.1007/s00432-016-2330-1
19. Qiu MJ, Yang SL, Wang MM, et al. Prognostic evaluation of esophageal cancer patients with stages I-III. Aging. 2020;12(14):14736–14753. doi:10.18632/aging.103532
20. Lin SH, Wang L, Myles B, et al. Propensity score-based comparison of long-term outcomes with 3-dimensional conformal radiotherapy vs intensity-modulated radiotherapy for esophageal cancer. Int J Radiat Oncol Biol Phys. 2012;84(5):1078–1085. doi:10.1016/j.ijrobp.2012.02.015
21. Wu VW, Sham JS, Kwong DL. Inverse planning in three-dimensional conformal and intensity-modulated radiotherapy of mid-thoracic oesophageal cancer. Br J Radiol. 2004;77(919):568–572. doi:10.1259/bjr/19972578
22. Patel RP, Parikh R, Gunturu KS, et al. Cardiotoxicity of immune checkpoint inhibitors. Curr Oncol Rep. 2021;23(7):79. doi:10.1007/s11912-021-01070-6
23. Mahmood SS, Fradley MG, Cohen JV, et al. Myocarditis in patients treated with immune checkpoint inhibitors. J Am Coll Cardiol. 2018;71(16):1755–1764. doi:10.1016/j.jacc.2018.02.037
24. Sise ME, Seethapathy H, Reynolds KL. Diagnosis and management of immune checkpoint inhibitor-associated renal toxicity: illustrative case and review. Oncologist. 2019;24(6):735–742. doi:10.1634/theoncologist.2018-0764
25. Gupta S, Short SAP, Sise ME, et al.; for the ICPi-AKI Consortium Investigators. Acute kidney injury in patients treated with immune checkpoint inhibitors. J Immunother Cancer. 2021;9(10):e003467. doi:10.1136/jitc-2021-003467
26. Kumar V, Chaudhary N, Garg M, Floudas CS, Soni P, Chandra AB. Current diagnosis and management of immune related adverse events (irAEs) induced by immune checkpoint inhibitor therapy. Front Pharmacol. 2017;8:49. doi:10.3389/fphar.2017.00049
27. Zhang H, Ren P, Ma M, et al. Prognostic significance of the preoperative albumin/fibrinogen ratio in patients with esophageal squamous cell carcinoma after surgical resection. J Cancer. 2021;12(16):5025–5034. doi:10.7150/jca.58022
28. Austin PC, Stuart EA. Optimal full matching for survival outcomes: a method that merits more widespread use. Stat Med. 2015;34(30):3949–3967. doi:10.1002/sim.6602
29. D’Agostino RB Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17(19):2265–2281. doi:10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b
30. Zhu X, Chen D, Li S, et al. Albumin-to-alkaline phosphatase ratio as a novel and promising prognostic biomarker in patients undergoing esophagectomy for carcinoma: a propensity score matching study. Front Oncol. 2021;11:764076. doi:10.3389/fonc.2021.764076
31. Li S, Wang H, Yang Z, et al. Naples prognostic score as a novel prognostic prediction tool in video-assisted thoracoscopic surgery for early-stage lung cancer: a propensity score matching study. Surg Endosc. 2021;35(7):3679–3697. doi:10.1007/s00464-020-07851-7
32. Austin PC. The performance of different propensity score methods for estimating marginal hazard ratios. Stat Med. 2013;32(16):2837–2849. doi:10.1002/sim.5705
33. Bando H, Kotani D, Tsushima T, et al. TENERGY: multicenter phase II study of atezolizumab monotherapy following definitive chemoradiotherapy with 5-FU plus cisplatin in patients with unresectable locally advanced esophageal squamous cell carcinoma. BMC Cancer. 2020;20(1):336. doi:10.1186/s12885-020-06716-5
34. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
35. Yang L, Liu Q, Zhang X, et al. DNA of neutrophil extracellular traps promotes cancer metastasis via CCDC25. Nature. 2020;583(7814):133–138. doi:10.1038/s41586-020-2394-6
36. Liang S, Li C, Gao Z, et al. A nomogram to predict short-term outcome of radiotherapy or chemoradiotherapy based on pre/post-treatment inflammatory biomarkers and their dynamic changes in esophageal squamous cell carcinoma. Int Immunopharmacol. 2021;90:107178. doi:10.1016/j.intimp.2020.107178
37. Cordeiro LAF, Silva TH, De Oliveira LC, Neto JFN. Systemic inflammation and nutritional status in patients on palliative cancer care: a systematic review of observational studies. Am J Hosp Palliat Care. 2020;37(7):565–571. doi:10.1177/1049909119886833
38. Arigami T, Okumura H, Matsumoto M, et al. Analysis of the fibrinogen and neutrophil-lymphocyte ratio in esophageal squamous cell carcinoma: a promising blood marker of tumor progression and prognosis. Medicine. 2015;94(42):e1702. doi:10.1097/MD.0000000000001702
39. Xie X, Luo KJ, Hu Y, Wang JY, Chen J. Prognostic value of preoperative platelet-lymphocyte and neutrophil-lymphocyte ratio in patients undergoing surgery for esophageal squamous cell cancer. Dis Esophagus. 2016;29(1):79–85. doi:10.1111/dote.12296
40. Freedman AN, Seminara D, Gail MH, et al. Cancer risk prediction models: a workshop on development, evaluation, and application. J Natl Cancer Inst. 2005;97(10):715–723. doi:10.1093/jnci/dji128
41. Kim SY, Yoon MJ, Park YI, Kim MJ, Nam BH, Park SR. Nomograms predicting survival of patients with unresectable or metastatic gastric cancer who receive combination cytotoxic chemotherapy as first-line treatment. Gastric Cancer. 2018;21(3):453–463. doi:10.1007/s10120-017-0756-z
42. Jeong SH, Kim RB, Park SY, et al. Nomogram for predicting gastric cancer recurrence using biomarker gene expression. Eur J Surg Oncol. 2020;46(1):195–201. doi:10.1016/j.ejso.2019.09.143
43. Huang YQ, Liang CH, He L, et al. Development and validation of a radiomics nomogram for preoperative prediction of lymph node metastasis in colorectal cancer. J Clin Oncol. 2016;34(18):2157–2164. doi:10.1200/JCO.2015.65.9128
44. Li J, Yu H, Peng L, et al. Novel nomogram predicting cancer-specific survival and overall survival in patients with primary esophageal small-cell carcinoma: a surveillance, epidemiology, and end results-based study. J Cancer Res Ther. 2021;17(3):630–637. doi:10.4103/jcrt.JCRT_1612_20
45. Van Calster B, Vickers AJ. Calibration of risk prediction models: impact on decision-analytic performance. Med Decis Making. 2015;35(2):162–169. doi:10.1177/0272989X14547233
46. Ruan R, Chen S, Tao Y, et al. Retrospective analysis of predictive factors for lymph node metastasis in superficial esophageal squamous cell carcinoma. Sci Rep. 2021;11(1):16544. doi:10.1038/s41598-021-96088-y
47. Templeton AJ, McNamara MG, Šeruga B, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124. doi:10.1093/jnci/dju124
48. Jain V, Berman AT. Radiation pneumonitis: old problem, new tricks. Cancers. 2018;10(7):222. doi:10.3390/cancers10070222
49. Rose J, Rodrigues G, Yaremko B, Lock M, D’Souza D. Systematic review of dose-volume parameters in the prediction of esophagitis in thoracic radiotherapy. Radiother Oncol. 2009;91(3):282–287. doi:10.1016/j.radonc.2008.09.010
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





