Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 13
Effects of Plant-Based Diets on Outcomes Related to Glucose Metabolism: A Systematic Review
Authors Johannesen CO , Dale HF , Jensen C , Lied GA
Received 3 June 2020
Accepted for publication 11 July 2020
Published 7 August 2020 Volume 2020:13 Pages 2811—2822
DOI https://doi.org/10.2147/DMSO.S265982
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Antonio Brunetti
Christina Osland Johannesen,1 Hanna Fjeldheim Dale,1– 3 Caroline Jensen,1 Gülen Arslan Lied1,3
1Centre for Nutrition, Department of Clinical Medicine, University of Bergen, Bergen, Norway; 2Section of Gastroenterology, Department of Medicine, Haukeland University Hospital, Bergen, Norway; 3National Centre of Functional Gastrointestinal Disorders, Haukeland University Hospital, Bergen, Norway
Correspondence: Hanna Fjeldheim Dale
Centre for Nutrition, Department of Clinical Medicine, University of Bergen, 15 Haukelandsbakken, Bergen 5009, Norway
Tel +47 98-088-495
Email [email protected]
Abstract: According to the rising prevalence of obesity and metabolic disorders leading to impaired glucose metabolism, effective strategies to prevent and/or delay the onset of disease are of great need. A plant-based diet has been suggested as an effective lifestyle change that may reduce the degree of obesity and improve outcomes related to glucose metabolism. This systematic review aimed to evaluate the effect of a plant-based diet on outcomes related to glucose metabolism. A literature search was conducted in the database PubMed until January 30, 2020. Randomized controlled trials investigating the effect of a plant-based dietary intervention on outcomes related to glucose metabolism in human subjects compared to an omnivorous diet were eligible for inclusion. Of 65 publications identified, nine trials on subjects with overweight/obesity, type 2 diabetes mellitus, or cardiovascular disease were included. Five studies reported that the plant-based intervention significantly improved markers of glycemic control from baseline to end point, of which four revealed a significant improvement in the intervention group compared to the control intervention. The remaining four studies did not observe a significant effect of a plant-based intervention on outcomes related to glucose metabolism. Our findings suggest that a shift to a plant-based diet may lead to favorable effects on glycemic control in individuals diagnosed with type 2 diabetes mellitus and/or obesity. The data were however somewhat conflicting, and the included trials reported results based on different intervention diets and study populations. Overall, no clear conclusions regarding effects of different plant-based diets can be drawn based on the current findings alone.
Keywords: glycemic control, plant-based diet, vegan, vegetarian, glucose metabolism, dietary pattern
Introduction
The term “plant-based diet” is used for a wide range of dietary patterns, and comprise all diets based mainly on food derived from plants. “Plant food” typically refers to vegetables, fruit, grains, seeds, legumes, pulses, fungi, and nuts, and a similarity among the different plant-based diets is the limited consumption of foods of animal origin.1,2 Due to variations in the degree of this limitation among diets, many plant-based diets exist, differing in the amount and type of animal foods included and excluded.3 Like other diets, a plant-based one can vary in nutritional content and proportion of the different food groups. As a natural consequence of the elimination of red meat and dairy, a plant-based diet is often low in fat, especially saturated fat.4 Furthermore, it is often characterized as carbohydrate-rich, with a high amount of fiber and starch, due to the high proportion of plant food. As such, plant-based diets usually turn out to be fat-reduced and carbohydrate-rich when compared to an omnivore diet, whether this is a conscious decision or not.4
On a global level, a large number of individuals follow a plant-based diet, with varying prevalence around the world. In most countries, individuals following a plant-based diet comprise only a small minority of the population. In recent years, there has been increased interest in plant-based diets, with more people following these types of diets in several Western countries.5 Contradictorily, several developing countries that until recently had a low consumption of meat face the opposite trend, with increased meat consumption. Overall, a large part of the world’s population is today eating more meat than recommended.5,6
Since 1975, the prevalence of obesity has nearly tripled worldwide, and it has been estimated that more than 1.9 billion adults were overweight in 2016, of whom over 650 million were obese.7 Increased body weight is considered a major risk factor for a number of chronic diseases, including type 2 diabetes mellitus (T2DM).8,9 Genetics explain only a small part of the obesity epidemic,10 and a sedentary lifestyle with excessive intake of food according to energy requirements is the main contributing factor. Given the rising prevalence of obesity and metabolic disorders leading to impaired glucose metabolism, effective strategies to prevent and/or delay the onset of disease are of great need.
Research has indicates that a reduction in the intake of animal products and an increase in plant-based foods have several positive health outcomes.1,4,11,12 Due to the high intake of dietary fibre, antioxidants, unsaturated fatty acids, and phytochemicals in combination with reduced intake of cholesterol and saturated fatty acids, a plant-based diet is associated with a number of health benefits.13–15 This, as well as the exclusion of foods of animal origin, has been shown to reduce the risk of obesity and T2DM, as well as cardiovascular disease (CVD), hypertension, and some cancers.13,14,16 Irrespective of sex or age, some studies have reported that the prevalence of obesity is much lower in both vegetarians and vegans, and that individuals following a plant-based diet are leaner overall than omnivores.12 In addition, several studies have reported that a plant-based diet is highly effective for weight loss and weight management.17–19 Overall, a plant-based diet has been suggested as an effective lifestyle change that may reduce the degree of obesity and improve outcomes related to glucose metabolism.11,12
Several studies have shown that a plant-based diet improves glycemic control and leads to increased insulin sensitivity, hence suggesting that a plant-based diet offers an advantage compared to an omnivorous diet with respect to both prevention and management of T2DM.13,16 The aim of this systematic review was to evaluate the effect of a plant-based diet on outcomes related to glucose metabolism by a thorough evaluation of publications reporting on interventions with different plant-based diets on relevant outcomes related to glucose metabolism. A systematic review was conducted in order to summarize the different findings from relevant randomized controlled trials (RCTs) with plant-based diets as intervention. The primary outcome was change in parameters related to glucose metabolism, after excluding animal foods from the diet.
Methods
The checklist and flowchart of the PRISMA (Preferred Reporting for Systematic Reviews and Meta-Analyses) guidelines were followed for this systematic review.
Search Strategy
Relevant literature was retrieved from the database PubMed (Medline). The different search terms used were divided into two categories, intervention and outcome, and are presented in Table 1.
 |
Table 1 Search Terms and MeSH Tags for the Literature Search |
Inclusion and Exclusion Criteria
Criteria for inclusion and exclusion of published literature are presented in Table 2. All RCTs published after 2010 looking at changes in glucose metabolism in a human population consuming a plant-based diet for >4 weeks were included based on the given inclusion and exclusion criteria. This comprised all studies collecting data linked to the metabolism of glucose at baseline and at the end of the intervention. Relevant outcomes of interest related to glucose metabolism included fasting plasma-glucose concentrations, HbA1c levels, C-peptide concentrations, and Homeostasis Model Assessment of Insulin Resistance (HOMA-IR) index values. No specific definition or subgroup of plant-based diet was favored by the inclusion criteria. Trials with physical activity as part of the intervention were excluded. Exclusion also applied to studies for which the full text was not available and those basing their results on the same data set as another included study. There were no limitations regarding sex, age, population size, nationality, or comorbidity.
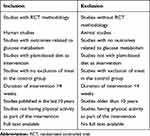 |
Table 2 Inclusion and Exclusion Criteria for this Literature Review |
Literature Search
A literature search based on the search combination listed in Table 1 was conducted in the database PubMed (Medline) on January 30th, 2020. The search filters “randomized controlled trials“ and “humans“ were used. The search identified in total 65 studies, of which 38 were excluded based on abstracts. The full-text versions of the remaining studies were assessed for eligibility.
Results
Included Studies
As a result of the search conducted in PubMed, and according to criteria for inclusion and exclusion, nine publications were included in the systematic review. The process of selection is shown in Figure 1. Study characteristics of the included studies are summarized in Table 3.
 |
Table 3 Overview of Studies Included in the Systematic Review |
 |
Figure 1 Flowchart depicting the inclusion of relevant publications in the current systematic literature review. |
Comparison of Included Studies
Among the nine studies included in this review, there were great variations in dietary patterns, intervention diets, study populations, and criteria for exclusion and inclusion. In addition, primary and secondary outcomes differed among the studies. Differences in inclusion and exclusion criteria caused variations in study populations. Some studies required participants to be clinically healthy, while others included only subjects previously diagnosed with a certain disease. Three studies were conducted in individuals diagnosed with T2DM,20–22 while one was conducted in subjects with CVD.23 Participants in the remaining five studies differed in characteristics, though obesity or overweight was represented among all the included subjects, specified with a BMI range of 25–40 kg/m2. In addition, comorbidity in the form of T2DM, ischemic heart disease, hypertension, or hypercholesterolemia were criteria for inclusion in two of these five studies.8,9 The plant-based diets chosen as intervention varied among the studies. Six of nine studies had vegan diets as intervention,9,–20-24 and four of these studies specified that the diet should be low in fat.9,21,22,24 Two of the three remaining studies implemented a lacto-ovo-vegetarian diet,25,26 of which one was a calorie-restricted diet. The last study administrated a low-fat plant-based diet, not otherwise specified.8
Of the nine studies included in this review, five evaluated the effect of a plant-based intervention compared to a conventional omnivorous diet,8,9,21,24,26 whereas three studies compared the effect of the intervention to a diet based on national health recommendations.20,22,23 The dietary patterns based on national guidelines were the American Heart Association (AHA) recommended diet,23 a conventional diet recommended by the Korean Diabetes Association 2011 (KDA)20 and a diet based on the 2003 American Diabetes Association (ADA) dietary recommendations.22 The rest of the studies implemented the Mediterranean diet as the control diet.25
The size of study populations varied between 45 and 291 individuals, and the duration of intervention varied from 4 to 24 weeks. Additionally, glycemic markers used for evaluation of improvement in glycemic control varied. The majority of the studies assessed changes in HbA1c levels, while others reported changes in fasting plasma-glucose concentrations, fasting insulin concentrations, concentrations of C-peptide, or used measuring tools, such as the HOMA-IR index.
Main Findings
Effects of a Plant-Based Diet in Individuals with Overweight or Obesity
Five of the studies investigated the effects of different plant-based diets in subjects with overweight or obesity and different comorbidities, with conflicting overall results. Wright et al aimed to investigate the effectiveness of a low-fat plant-based diet on BMI and cholesterol levels in individuals with obesity or overweight, in addition to T2DM, ischemic heart disease, hypertension, or hypercholesterolemia.8 An RCT was conducted with 65 participants over 24 weeks. In relation to the metabolism of glucose, they reported changes in HbA1c. The between-group differences in HbA1c levels favored the intervention group, with a significant reduction of 3 mmol/mol from baseline to 24 weeks on the plant-based diet. An even greater reduction of 5 mmol/mol within the intervention group was reported on follow-up at 48 weeks. They reported a significant increase in HbA1c levels of 2 mmol/mol from baseline to end point at 24 weeks within the control group. Two participants in the intervention group previously diagnosed with DM no longer met the diagnostic criteria (HbA1c ≥50 mmol/mol) at the end of the intervention. Additionally, they reported that higher levels of HbA1c at intervention start correlated with larger subsequent reduction during the intervention.8
Mishra et al aimed to determine the effects of a plant-based dietary intervention on body weight, blood pressure, dietary intake, plasma-lipid concentrations, and HbA1c in participants with BMI >25 kg/m2 and/or T2DM.9 Participants were randomized to follow either a low-fat vegan diet (n=142) or a conventional omnivorous diet (n=149) for 18 weeks. HbA1c was measured at baseline and after 18 weeks only in participants diagnosed with T2DM (n=21 diet group, n=22 control group). Within the intervention and control groups, HbA1c levels had reduced by 0.6% and 0.08%, respectively. HbA1c levels differed significantly from baseline to end point at 18 weeks between the two diet groups. When limiting the analysis to participants with T2DM completing the assessment after 18 weeks (n=17 diet group, n=18 control group), a significant decrease in mean HbA1c within the intervention group of 0.7% compared to the control group (0.1%) was reported.9
Kahleova et al investigated the effect of a plant-based dietary intervention on β-cell function in healthy individuals with BMI 28–40 kg/m2 and no history of T2DM.24 They randomized participants to follow a low-fat vegan diet (n=38) for 16 weeks or to make no dietary changes (n=37). No significant improvements in HbA1c levels in either of the diet groups were observed in response to intervention, and levels of HbA1c did not differ between groups. However, the concentration of fasting plasma glucose, insulin, and C-peptide were all significantly reduced in the intervention group, with a significant difference between groups. The control group showed no significant changes in markers of glycemic control. In the intervention group, a notable increase in meal-stimulated secretion of insulin was observed compared with the control group.24
Sofi et al conducted an RCT investigating how low-calorie diets differing in presence of foods of animal origin affected total body weight, fat mass, and BMI.24 A total of 118 overweight omnivores with BMI >25 kg/m2 and a low–moderate cardiovascular risk profile were randomized to follow either a low-calorie lacto-ovo-vegetarian diet (n=60) or a low-calorie Mediterranean diet (n=58) for 12 weeks in a crossover manner. Primary outcomes were changes in fat mass, total body weight, and BMI from baseline, whereas secondary outcomes included changes in glycemic markers (plasma-glucose concentrations, insulin concentrations, and HOMA-IR index). No significant differences were reported in markers of glycemic control within either diet group or between the two diets.25
Li et al examined the influence of different protein sources and protein quantity on energy expenditure, cardiometabolic profile, and appetite regulation during energy restriction in overweight/obese subjects.25 In total, 47 participants were randomly assigned to follow either a lacto-ovo-vegetarian diet (n=25) or a conventional omnivorous diet (n=22), each diet containing one predominant source of protein: soy/legume in the lacto-ovo-vegetarian group and beef/pork in the omnivorous group. Throughout the intervention, participants consumed diets with different protein quantities (10%, 20%, or 30% of total energy intake) for 4 weeks each in a crossover manner. At the end of each 4-week period, fasting blood samples were collected. After completing all three intervention periods, Li et al reported that neither the source nor quantity of protein significantly affected concentrations of fasting insulin, fasting glucose, or HOMA-IR in any of the two dietary groups.26
Effects of a Plant-Based Diet in Individuals with T2DM
Three of the trials reported on the effects of a plant-based intervention in individuals with T2DM, with varying but overall promising results. Lee et al compared the effect of a vegan diet (n=46) and a KDA-recommended diet (n=47) on glycemic control among participants diagnosed with T2DM.20 The primary outcome was change in HbA1c over 12 weeks, and HbA1c levels were measured at weeks 0, 4, and 12. After intervention, both groups showed significant reductions in HbA1c levels. The reduction was greater in the vegan group than in the group following the KDA-recommended diet (0.5% and 0.2%, respectively). When considering only subjects with high compliance with their diet based on self-reported food records, the difference in HbA1c reduction between the two groups differed even more (0.9% vs 0.3%).20
Barnard et al hypothesized that a low-fat vegan diet would improve body weight, blood pressure, plasma-lipid concentrations, renal function, and glycemic control more effectively than a calorie-restricted omnivorous diet in individuals with T2DM.21 In sum, 45 participants were included in a 20-week parallel-group study. Both diets led to significant improvements in HbA1c within each group; however, the improvements did not differ between the two dietary patterns. In both groups at baseline, mean HbA1c values were <7% and were reduced similarly by an additional 0.4% in each group.21
Turner-McGrievy et al assessed the effect of changes in glycemic index (GI) and glycemic load (GL) on weight loss and HbA1c among individuals with T2DM adopting a low-fat vegan diet (n=49) or one based on the 2003 ADA recommendations (n=50).22 After intervention, they reported that the vegan-diet group showed reduced GI to a greater extent than the group following the ADA recommendations, whereas GL was reduced further in the ADA-diet compared to the vegan group. After controlling for weight loss, they found that GI was not a predictor of changes in HbA1c; however, weight loss was. No significant relationship between GL and changes in HbA1c was reported.22
Effects of a Plant-Based Diet in Individuals with Cardiovascular Disease
One study reported on the effect of a vegan diet in individuals with a CVD diagnosis. Shah et al aimed to determine the effects of a vegan diet (n=50) compared to an AHA-recommended diet (n=50) on markers for inflammation and high-sensitivity CRP) in participants diagnosed with CVD.23 The primary outcome was concentration of high-sensitivity CRP, while secondary outcomes included markers of glycemic control (blood-insulin concentration, fasting blood-glucose concentration, and HbA1c level), among others. Postintervention measures showed no significant differences in fasting glucose concentrations, HbA1c, or insulin concentrations between the groups.23
Summary
Among the nine studies included in this review, the main findings reported related to effects of a plant-based diet on outcomes related to glucose metabolism were inconsistent overall. Five of nine studies (56%) reported that the plant-based intervention significantly improved markers of glycemic control from baseline to end point.8,9,20,21,24 Only four studies (44%) reported a significant improvement in markers of glycemic control in the intervention group that differed from the control intervention: one of threeconducted on individuals with T2DM and three of five conducted on obese participants.8,9,20,24 The remaining four studies (44%) did not reveal any significant improvements of a plant-based intervention on outcomes related to glucose metabolism.22,23,25,26 Of note, none of the included studies reported a suggested negative effect of the intervention diet. The main findings of the nine studies included in this review are summarized in Table 4.
 |
Table 4 Main Findings Related to Glucose Metabolism in Studies Included |
Discussion
Main Findings
The overall aim of this systematic review was to evaluate the effect of a plant-based diet on outcomes related to glucose metabolism. The findings are overall inconclusive, with suggested beneficial effects attributed to a plant-based diet reported in four of the nine included studies. Previous studies have suggested that a diet with no food of animal origin offers an advantage with respect to both prevention and management of obesity and T2DM.13,16 Even after adjusting for BMI, several prospective studies reported that the prevalence of T2DM was 46%–76% lower in vegans and vegetarians compared to omnivores.27–29 Other studies have shown that a plant-based diet improved markers for glycemic control and led to increased insulin sensitivity.12,27 Several factors can explain the conflicting results and lack of effects in the trials included in the current review, and study population, study design, and adherence to intervention diet may be contributing factors.
Study Population
In five of the nine studies, change in body weight or BMI was the primary outcome. This was reflected in the participants, given that a majority of the studies had overweight or obesity as an inclusion criterion. Further, none of the nine studies examined the effect of a plant-based diet on glucose metabolism in healthy, normal-weight individuals. All included studies were conducted in participants with either overweight or obesity and/or at least one sequela related to excess body weight. The use of study populations with CVD, obesity, and/or T2DM may lead to a source of error, as these participants are usually more unconscious of their own health compared to the overall population.25 Studies evaluating the effects of a plant-based diet in healthy participants with BMI <25 kg/m2 were not identified in this systematic literature search.
The vast majority of the studies had a predominance of female participants. Several studies reported a remarkable underrepresentation of males, as men were difficult to recruit for dietary intervention or for reasons that were unclear. In fact, a predominance of female participants in clinical trials on interventions for behavioral change or dietary patterns is a well-known phenomenon.30 In all studies included in this review, with the exception of that by Shah et al, who had a skewed distribution in favour of men, women were strongly overrepresented among the participants. In the study by Kahleova et al, women accounted for as much as 89% of the total number of subjects.23 Only two of nine studies included analyses adjusted or stratified by sex.9,22 As such, one cannot exclude the possibility that the effect of a plant-based diet on glycemic control may differ according to sex.
Study Design and Number of Participants
A criterion for inclusion was that the studies were followed an RCT methodology. However, study designs differed somewhat. Most studies followed an open, randomized, parallel design with no blinding of subjects in terms of the dietary interventions. Nonetheless, two studies had crossovers, which may give them stronger validity compared to the remaining studies.31
Considering that only a third of the studies reported having performed a power analysis prior to recruitment to ensure a sufficient number of subjects to achieve significant results, it is reasonable to assume that the results of the studies with the greatest number of participants have the most strength. Moreover, two of three studies that performed such a power analysis reported that the recruitment fell short of the sample size called for by the analysis. The studies with the largest number of participants were those conducted by Mishra et al and Sofi et al, with 211 and 107 completed participants, respectively.9,25 The latter study by Sofi et al stands out in the current review, due to the use of a clinically healthy European population, crossover design, and high number of participants.25
Adherence to Intervention Diet
In intervention studies, it is reasonable to expect low compliance with plant-based diets, as it may be difficult for individuals with a prior omnivorous diet to abstain from all foods of animal origin for several months. Lack of information and knowledge has beenidentified as the main barrier to adopting a whole-food plant-based diet in a survey.32 These findings suggest that proper education and adequate information prior to intervention will produce better compliance. Several of the studies included dietary education and follow-up by dieticians as part of the study program. This, together with a rapid initial weight loss, led to increased adherence to the prescribed diet, even in cases of plant-based diets.33,34 It is reasonable to assume that provision of groceries, compulsory measurement, and participation in group lessons would further increase the likelihood of high adherence. Four of the nine studies included weekly or biweekly meetings, counting cooking tutorials, discussion sessions, and instructions in food preparation and meal planning.8,9,21,22 One study provided both groups with groceries that supported the dietary recommendations on a weekly basis, whereas another initiated private weigh-ins before each meeting to make all participants aware of their body weight.21,23 Studies reporting low compliance among subjects used onlytelephone consultations, whereas a more intensive approach was implemented in the remaining trials. The high rate of completed participants in this review was presumably due to a higher level of motivation in the participants, which in turn underlines the importance of not attributing improvements in glycemic control solely to a plant-based diet.
Despite the fact that all the studies examined the effect of a plant-based dietary intervention in free-living individuals, different approaches were used to determine the food-consumption status of each participant. Li et al provided portioned quantities of selected foods to all participants throughout each 4-week period to encourage compliance with the prescribed diets.26 In addition, all subjects were counseled by a registered dietitian to achieve the desired intake of calories and macronutrients, and received a detailed grocery list based on daily menus with portion sizes for each food. However, this approach is not realistic outside a study context to a similar extent.
Nonetheless, most studies had a more realistic approach. Those where participants had to plan, buy, and prepare their own meals had the restriction that they could not completely monitor whether the participants were following the prescribed diets. Several studies used food records and telephone monitoring in an effort to minimize this problem. However, a food record once or twice a week is not necessarily representative of the total intervention period. Additionally, this requires reliance on self-reported dietary intake and recalls, which has well-known limitations.35 Participants may have underreported their intake, as well as potentially failed to report intake of animal foods, which could have introduced error.
Shah et al reported on an additional weakness regarding the use of self-reported data.23 They found that a participant in the comparison-diet group consuming no dairy or no animal protein would be considered adherent to the omnivorous diet according to the diet-adherence protocol used. This confirms that controlling the level of adherence to the diet through food questionnaires or records may not give a valid picture, and that results based on self-reported data should be interpreted with caution.
Effects of Different Plant-Based Diets
Several types of plant-based diets were implemented in the studies included in the current review, including a low-fat plant-based diet, a low-fat vegan diet, a vegan diet, a lacto-ovo-vegetarian diet, and a low-calorie lacto-ovo-vegetarian diet. Based on the overall findings, it is not possible to favor a specific plant-based diet according to effect on parameters related to glucose metabolism.
Weight loss initiated by a reduction in total energy intake is assumed to be the main mechanism behind improved glycemic control caused by various dietary interventions, including different plant-based diets.36 Therefore, a dietary approach aiming to initiate weight loss is likely to improve glycemic markers. None of the studies with caloric restriction reported a significant difference in glycemic markers between the intervention diet and the comparison diet.20,24 This suggests that the lack of difference between the control group and plant-based group may be seen as a result of the calorie restrictions in the comparison group.
Another important aspect regarding the different intervention diets is the consistent use of fat-reduced vegan diets in a majority of the studies. Observational studies have shown that both vegetarians and vegans in general have a lower consumption of fat and total energy compared to omnivores.37 In this regard, switching to a plant-based diet often results in reduced energy and fat content in the diet. As such, one can question whether it was necessary to impose such restrictions on the intervention diets. The frequent use of a low-fat vegan diet makes the interventions largely research-specific and requires that the results are interpreted with caution. Such intervention diets are not representative of a conventional plant-based diet and cannot tell whether a plant-based diet without nutritional restrictions actually leads to glycemic control.
It has to be acknowledged that the macronutrient ratio in a diet likely is an important reason contributing to why different plant-based diets exert different effects on glucose metabolism. Beneficial effects on glucose metabolism in response to a plant-based diet can in some cases most likely be attributed the macronutrient composition in the diet, rather than the plant-based diet alone. A recent study comparing a ketogenic plant-based diet to both a lacto-vegetarian ketogenic diet and an omnivorous ketogenic diet found that when the macronutrient and caloric intake of the three different diets were kept equal, glucose metabolism improved to the same degree, independently of the protein source in the diet being plant-based or not.38 This highlights the importance of taking the macronutrient composition of intervention diets into account when investigating plant-based diets compared to diets with animal foods.
The use of various diets as the comparator arm may also have affected the findings. Whether the studies in this review used a conventional omnivorous diet, one based on national health recommendations, or a diet otherwise specified as the comparison diet is a factor that should be taken into consideration. In addition to the five studies that used a conventional diet in the control group, three studies used a diet based on recommendations in cases of T2DM or CVD, whereas one used a low-calorie Mediterranean diet as the comparison diet. These diets are often designed for weight loss or DM control, and thus the participants in the control groups did not remain untreated. In cases of reducing risk factors associated with chronic degenerative diseases, the Mediterranean diet is widely reported to be one of the healthiest and most effective dietary patterns.37 A meta-analysis of 20 RCTs on various T2DM diet interventions reported the largest effect (reduction in HbA1c) with a Mediterranean diet.36 This underlines the fact that characteristics of the comparison diet are crucial to potential change in HbA1c levels, and that the use of a Mediterranean diet as comparison may lead to a reduction in effect size. In addition, the degree of similarity between the control diet and the original diet is decisive in whether one can conclude that a change in HbA1c is solely due to the plant-based diet or if it is seen as a result of a general change in eating pattern and dietary composition.
Strengths and Limitations
The present review has several strengths. All studies included followed an RCT design, considered the gold standard for dietary intervention studies. The fact that all participants in the studies were asked not to alter their exercise patterns or physical activity levels during the intervention period is an additional strength, as exercise is known to affect both energy metabolism and nutritional status.39 Also, the real-world nature of the studies and the fact that all subjects were responsible for their own food choices and living at home preparing their own meals makes the results applicable outside the research setting.
The fact that most of the participant groups had a high mean age — 50– 61 years — can be considered a limitation according to comparison to other population groups. In addition, all the studies were carried out in developed countries, and two-thirds of them were conducted on American populations. The results of an American study are not necessarily representative of other nationalities, and the overall conclusions may not be transferable to developing countries.
Future Directions
The studies in the current review reported on participants who were generally health-conscious and had higher health literacy than average. Therefore, it is reasonable to assume that they were willing to make substantial dietary changes and may not have been representative of the general population. Based on the current findings, future research should focus on larger and more representative study populations. This applies to both normal-weight and clinically healthy participants, as well as subjects with T2DM, with greater diversity and better demographic distribution. Further, future studies should aim for more even distribution according to sex, as well as a greater diversity in the age of the participants.
The study duration in those included varied from 4 to 24 weeks. Four weeks of intervention is a limited period that only only a suggestion of the possible interpretation of the results. However, to evaluate the long-term effects of a plant-based diet on glycemic control, a longer study is required. Plant-based intervention diets and omnivorous control diets should be unrestricted in both energy content and nutritional distribution, and be implemented in the everyday life of study participants over an extended period of time. The control diet should be similar to the participants’ original diet to avoid a major dietary adjustment in the comparison group, which may impact the effect size.
Considering the fact that most studies in this review used a low-fat vegan diet, it is difficult to draw a difference in effect on glycemic markers between different plant-based diets. More varied plant-based interventions should be conducted to acquire more knowledge about which plant-based dietary patterns are the most effective and potentially which patient groups or subgroups of the population benefit the most from such lifestyle change. Increased knowledge highlights several beneficial health effects in response to an increased consumption of plant-foods. Further research should aim to compare possible differences between a partly plant-based diet with a restricted intake of animal foods and a strict plant-based diet, as these differences have not been properly investigated to date. Future research might observe effects of less strict diets than those reported in the studies included in this review.
Implementing a plant-based diet in everyday life, as well as in clinical practice has been proposed as part of the prevention and treatment of overweight, obesity, and T2DM. Facilitated conditions, rapid initial weight loss, adequate education and information, and individualized counselling and support can contribute to a successful plant-based lifestyle and positive health effects.
Conclusion
When comparing the results from the nine studies in this literature review, the findings were inconsistent. The overall tendency was that a plant-based diet had no or little potential to improve glycemic markers compared to implemented control diets. Nonetheless, 44% of the studies proposed that a dietary pattern excluding foods of animal origin is likely to have beneficial effects on glucose metabolism in individuals with T2DM and overweight/obesity; however specific changes in glycemic profile were not consistent among the studies. Improvement in glycemic control can presumably be explained by a reduction in excess body weight as a consequence of the reduced content of fat and energy in a plant-based diet compared to an omnivorous diet. The trials included reported results based on different intervention diets, control diets, and study populations. Overall, no clear conclusion regarding effects of different plant-based diets can be drawn based on the current findings alone.
Abbreviations
ADA, American Diabetes Association; AHA, American Heart Association; CVD, cardiovascular disease; HOMA-IR, Homeostasis Model Assessment of Insulin Resistance; KDA, Korean Diabetes Association; RCT, randomized controlled trial; T2DM, type 2 diabetes mellitus.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval to the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Rocha JP, Laster J, Parag B, Shah NU. Multiple health benefits and minimal risks associated with vegetarian diets. Curr Nutr Rep. 2019;8(4):374–381. doi:10.1007/s13668-019-00298-w
2. British Dietetic Association. Plant-Based Diet: Food Fact Sheet. [Internet]; 2020. Available from: https://www.bda.uk.com/resource/plant-based-diet.html.
3. Satija A, Hu FB. Plant-based diets and cardiovascular health. Trends Cardiovasc Med. 2018;28(7):437–441. doi:10.1016/j.tcm.2018.02.004
4. Key TJ, Appleby PN, Rosell MS. Health effects of vegetarian and vegan diets. Proc Nutr Soc. 2006;65(1):35–41. doi:10.1079/PNS2005481
5. Godfray HCJ, Aveyard P, Garnett T, et al. Meat consumption, health, and the environment. Science. 2018;361:6399. doi:10.1126/science.aam5324
6. Kim SR, Kim K, Lee SA, et al. Effect of red, processed, and white meat consumption on the risk of gastric cancer: an overall and dose⁻response meta-analysis. Nutrients. 2019;11:4.
7. World Health Organization. Obesity and overweight. [Internet]; 2020. Available from: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight.
8. Wright N, Wilson L, Smith M, Duncan B, McHugh P. The BROAD study: A randomised controlled trial using a whole food plant-based diet in the community for obesity, ischaemic heart disease or diabetes. Nutr Diab. 2017;7(3):e256–e256. doi:10.1038/nutd.2017.3
9. Mishra S, Xu J, Agarwal U, Gonzales J, Levin S, Barnard ND. A multicenter randomized controlled trial of a plant-based nutrition program to reduce body weight and cardiovascular risk in the corporate setting: the GEICO study. Eur J Clin Nutr. 2013;67(7):718–724. doi:10.1038/ejcn.2013.92
10. Skrypnik D, Mostowska A, Jagodziński PP, et al. Association of rs699947 (−2578 C/A) and rs2010963 (−634 G/C) single nucleotide polymorphisms of the VEGF Gene, VEGF-A and leptin serum level, and cardiovascular risk in patients with excess body mass: a case–control study. J Clin Med. 2020;9:469. doi:10.3390/jcm9020469
11. Appleby PN, Key TJ. The long-term health of vegetarians and vegans. Proc Nutr Soc. 2016;75(3):287–293. doi:10.1017/S0029665115004334
12. Grant JD. Time for change: benefits of a plant-based diet. Can Fam Physician. 2017;63(10):744–746.
13. Craig WJ. Health effects of vegan diets. Am J Clin Nutr. 2009;89(5):1627s–1633s. doi:10.3945/ajcn.2009.26736N
14. McEvoy CT, Temple N, Woodside JV. Vegetarian diets, low-meat diets and health: a review. Public Health Nutr. 2012;15(12):2287–2294. doi:10.1017/S1368980012000936
15. Corrin T, Papadopoulos A. Understanding the attitudes and perceptions of vegetarian and plant-based diets to shape future health promotion programs. Appetite. 2017;109:40–47. doi:10.1016/j.appet.2016.11.018
16. Pilis W, Stec K, Zych M, Pilis A. Health benefits and risk associated with adopting a vegetarian diet. Rocz Panstw Zakl Hig. 2014;65(1):9–14.
17. Tuso PJ, Ismail MH, Ha BP, Bartolotto C. Nutritional update for physicians: plant-based diets. Perm J. 2013;17(2):61–66. doi:10.7812/TPP/12-085
18. Berkow SE, Barnard N. Vegetarian diets and weight status. Nutr Rev. 2006;64(4):175–188. doi:10.1111/j.1753-4887.2006.tb00200.x
19. Farmer B, Larson BT, Fulgoni VL
20. Lee Y-M, Kim S-A, Lee I-K, et al. Effect of a brown rice based vegan diet and conventional diabetic diet on glycemic control of patients with Type 2 diabetes: A 12-week randomized clinical trial. PLoS One. 2016;11(6):e0155918e0155918. doi:10.1371/journal.pone.0155918
21. Barnard ND, Levin SM, Gloede L, Flores R. Turning the waiting room into a classroom: weekly classes using a vegan or a portion-controlled eating plan improve diabetes control in a randomized translational study. J Acad Nutr Diet. 2018;118(6):1072–1079. doi:10.1016/j.jand.2017.11.017
22. Turner-McGrievy GM, Jenkins DJA, Barnard ND, Cohen J, Gloede L, Green AA. Decreases in dietary glycemic index are related to weight loss among individuals following therapeutic diets for type 2 diabetes. J Nutr. 2011;141(8):1469–1474. doi:10.3945/jn.111.140921
23. Shah B, Newman JD, Woolf K, et al. Anti-inflammatory effects of a vegan diet versus the american heart association-recommended diet in coronary artery disease trial. J Am Heart Assoc. 2018;7(23):e011367e011367. doi:10.1161/JAHA.118.011367
24. Kahleova H, Tura A, Hill M, Holubkov R, Barnard ND. A plant-based dietary intervention improves beta-cell function and insulin resistance in overweight adults: a 16-week randomized clinical trial. Nutrients. 2018;10(2):189. doi:10.3390/nu10020189
25. Sofi F, Dinu M, Pagliai G, et al. Low-calorie vegetarian versus mediterranean diets for reducing body weight and improving cardiovascular risk profile: CARDIVEG study (Cardiovascular Prevention With Vegetarian Diet). Circulation. 2018;137(11):1103–1113. doi:10.1161/CIRCULATIONAHA.117.030088
26. Li J, Armstrong CLH, Campbell WW. Effects of dietary protein source and quantity during weight loss on appetite, energy expenditure, and cardio-metabolic responses. Nutrients. 2016;8(2):63. doi:10.3390/nu8020063
27. Tonstad S, Butler T, Yan R, Fraser GE. Type of vegetarian diet, body weight, and prevalence of type 2 diabetes. Diab Care. 2009;32(5):791–796. doi:10.2337/dc08-1886
28. Snowdon DA, Phillips RL. Does a vegetarian diet reduce the occurrence of diabetes? Am J Public Health. 1985;75(5):507–512. doi:10.2105/AJPH.75.5.507
29. Vang A, Singh PN, Lee JW, Haddad EH, Brinegar CH. Meats, processed meats, obesity, weight gain and occurrence of diabetes among adults: findings from adventist health studies. Ann Nutr Metab. 2008;52(2):96–104. doi:10.1159/000121365
30. Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(4):406–441. doi:10.1161/CIR.0b013e3181e8edf1
31. Kaartinen K, Lammi K, Hypen M, Nenonen M, Hanninen O, Rauma AL. Vegan diet alleviates fibromyalgia symptoms. Scand J Rheumatol. 2000;29(5):308–313. doi:10.1080/030097400447697
32. Lea EJ, Crawford D, Worsley A. Public views of the benefits and barriers to the consumption of a plant-based diet. Eur J Clin Nutr. 2006;60(7):828–837. doi:10.1038/sj.ejcn.1602387
33. Ruby MB. Vegetarianism. A blossoming field of study. Appetite. 2012;58(1):141–150. doi:10.1016/j.appet.2011.09.019
34. Turner-McGrievy GM, Davidson CR, Wingard EE, Wilcox S, Frongillo EA. Comparative effectiveness of plant-based diets for weight loss: a randomized controlled trial of five different diets. Nutrition. 2015;31(2):350–358. doi:10.1016/j.nut.2014.09.002
35. Yuan C, Spiegelman D, Rimm EB, et al. Relative validity of nutrient intakes assessed by questionnaire, 24-hour recalls, and diet records as compared with urinary recovery and plasma concentration biomarkers: findings for women. Am J Epidemiol. 2018;187(5):1051–1063. doi:10.1093/aje/kwx328
36. Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr. 2013;97(3):505–516. doi:10.3945/ajcn.112.042457
37. Kennedy ET, Bowman SA, Spence JT, Freedman M, King J. Popular diets: correlation to health, nutrition, and obesity. J Am Diet Assoc. 2001;101(4):411–420. doi:10.1016/S0002-8223(01)00108-0
38. Basciani S, Camajani E, Contini S, et al. Very-low-calorie ketogenic diets with whey, vegetable or animal protein in patients with obesity: a randomized pilot study. J Clin Endocrinol Metab. 2020;105:dgaa336. doi:(10.1210/clinem/dgaa336)
39. Skrypnik D, Bogdański P, Skrypnik K, et al. Influence of endurance and endurance-strength training on mineral status in women with abdominal obesity: a randomized trial. Medicine. 2019;98(12):e14909. doi:10.1097/MD.0000000000014909
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
