Back to Journals » Neuropsychiatric Disease and Treatment » Volume 12
Effects of escitalopram with a Chinese traditional compound Jiuweizhenxin-keli on mismatch negativity and P50 in patients with major depressive disorders
Authors Kuang W, Tian L, Yue L, Li J
Received 13 January 2016
Accepted for publication 29 February 2016
Published 3 August 2016 Volume 2016:12 Pages 1935—1941
DOI https://doi.org/10.2147/NDT.S104020
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Wai Kwong Tang
Weihong Kuang,1,* Liantian Tian,2,* Lili Yue,1 Jin Li1
1Department of Psychiatry and Mental Health Center, West China Hospital, Sichuan University, Chengdu, People’s Republic of China; 2Occupational Respiratory Disease Research Center, No 4 West China Hospital/West China School of Public Health, Sichuan University, Chengdu, People’s Republic of China
*These authors contributed equally to this work
Objective: The objective of this study was to investigate the therapeutic effects of escitalopram in conjunction with Jiuweizhenxin-keli on neuroelectrophysiology in patients with major depressive disorders (MDD).
Patients and methods: Patients with depressive episode of MDD according to the criteria of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, were randomly assigned to Esc group (30 patients) receiving escitalopram treatment and JK group (30 patients) treated with a combination of escitalopram and Jiuweizhenxin-keli. The healthy control (HC) group (30 persons with normal health condition) served as control. All groups were subject to examination of 24-item Hamilton Depression Rating Scale and Hamilton Anxiety Scale, mismatch negativity (MMN), and sensory gating potential P50 (SG-P50) of event-related potentials. Data were collected at three different time points: baseline (before treatment) and week 2 and week 6 post treatment.
Results: At baseline, all electrophysiological parameters of patients with MDD were significantly higher than those of HCs. After treatment, in the Esc group, MMN latency, S2-P50 amplitude, and S2-P50/S1-P50 amplitude ratio decreased; however, the decrements were not statistically significant compared to either baseline or the HC group. Also, no significant changes were observed in the percentage of individuals whose S2-P50/S1-P50 ≥0.5 in the Esc group. On the other hand, in the JK group after a 6-week treatment, MMN latency (206.35±32.14 ms) was significantly shorter than that of the Esc group (219.57±36.51 ms), S2-P50 amplitude (7.27±4.85 µV) reduced significantly compared with the baseline level (10.21±4.10 µV), the percentage of individuals whose S2-P50/S1-P50 ≥0.5 in the JK group greatly decreased and this was not significantly different compared to that of the HC group (P≥0.05).
Conclusion: Neuroplasticity of patients with MDD is apparently disturbed, characterized by aberrant MMN latency and SG-P50-related event-related potential parameters. A combination of escitalopram and Jiuweizhenxin-keli treatment can markedly restore these neuroelectrophysiological features, and thus, could be a novel therapeutic solution for improving the impaired neuroplasticity of MDD patients.
Keywords: major depressive disorder, Jiuweizhenxin-keli, escitalopram, MMN, P50, neuroplasticity
Introduction
Major depressive disorder (MDD) is a psychiatric disorder characterized by persistent, pervasive feelings of sadness and anhedonia. It is associated with high morbidity and mortality as well as disability and disease burden with lifetime prevalence estimated as 13%–16% in adults.1–3 The important pathological processes in the onset, progress, and prognosis of the disease include disruption of neuroplasticity, reduction in neuropil, dysfunction of brain structures related to emotional feedback loop, and reductions in the total volume and atrophy and loss of neurons in the hippocampus.4,5 Among these, neuroplasticity is a fundamental process by which human brain acquires information and makes adaptive responses to changes in both inner and outer environments. Neuroplasticity plays a critical role in brain function such as neural development, learning and memory, and recovery after brain injury. The key molecules such as brain-derived neurotrophic factor (BDNF) have critical roles in stabilizing synaptic change and neuroplasticity in depression.6 Dysfunction of neuroplasticity could contribute to the pathophysiology of mood disorders, and induction of appropriate plasticity of the brain could exert therapeutic effect on the diseases.7–9 Antidepressant treatment may block or reverse disruption of neuroplasticity by chronic stress, enhance patients’ cognitive function, and even reverse functional defection.10
Neuroplasticity involves coordination of both Long-Term Potentiation (LTP) and Long-Term Depression.9 Previous investigations show that characteristics of brain LTP and long-term depression can be evaluated using auditory-evoked potential-related mismatch negativity (MMN) and sensory gating (SG) potential.11 In the human body, neuroplasticity of the central nervous system (CNS) can be indirectly represented by the characteristics of cerebral cortex excitatory and inhibitory functions. In the level of neuroelectrophysiology, through the measurement of single pulse and pair pulse stimuli, we can determine intracortical facilitation/inhibition and evaluate neuroplasticity of the CNS.12 As postsynaptic potential, MMN reflects automatic processing of information gathered from outer environment and implies precognitive processing.13,14 MMN is a negative wave obtained using event-related potentials induced by low probability event (deviant stimuli) to minus event-related potentials induced by high probability event (standard stimuli) when brain is not under active attention. It is widely recognized that MMN is one of the most important functional indexes reflecting early process of information by cerebral cortex15 and involves neural mechanism of LTP during learning and memory.16 MMN latency period reflects information processing speed of the brain. On the other hand, SG-P50 belongs to SG mechanism of the CNS and reflects individual’s ability to selectively filter complex sensory information and inhibit nonrelevant information of the cerebral context. Abnormal SG function is related to aberrant pathophysiological function of patients with mental disorders.17,18 SG status can be evaluated using auditory-evoked potential P50 paradigm measurement, which is a positive phase wave appearing between 30 ms and 90 ms after condition (S1)–test (S2) stimulation. In normal individual, S2-P50 decreases at least 50% compared to S1-P50. Therefore, these electrophysiological parameters were measured to characterize neuroplasticity of MDD patients in this study.
Jiuweizhenxin-keli is a commercially available traditional Chinese compound commonly used to treat general anxiety disorder. Owing to its therapeutic effects on anxiolytic symptoms and advantages in drug tolerance and drug safety, Jiuweizhenxin-keli can be applied in adjuvant or potentiation therapeutic regimen of depressive patients.19 The active ingredients of Jiuweizhenxin-keli include a variety of phytochemicals such as ginsenosides, Rehmannia-related polysaccharides, jujube seed alcohol, poria sugar, and deoxyschizandrin. In vitro studies have shown that these compounds can regulate intracellular Ca2+ concentration, enhance glutamatergic pathway in hippocampal neurons, decrease free radical level,20,21 reduce stress-related apoptosis of neural cells in rats, increase gene expression of nerve growth factor (NGF) and c-fos in rat brain, and improve function of cholinergic system and levels of glutamate/γ-aminobutyric acid in the CNS.22 Ginsenosides upregulate the mRNA level of BDNF after chronic stress and downregulate the level of excitement in the rat hypothalamo-pituitary-adrenal axis of the depression model of chronic stress.22 Rehmannia-related polysaccharides inhibit glutamate level and decrease N-methyl-D-aspartate receptor expression.23 Jujube seed alcohol downregulates calmodulin expression, inhibits intracellular calcium overload, and protects neurons from apoptosis.24 Taken together, it is suggested that Jiuweizhenxin-keli can potentially improve neuroplasticity of the CNS. To test this hypothesis, we utilized neuroelectrophysiology measurements described earlier as indirect indicators of patients’ neural plasticity and investigated effects of Jiuweizhenxin-keli on neuroelectrophysiology function in patients with MDD.
Patients and methods
Patients
Sixty patients (18–60 years of age) were recruited at Mental Health Center, West China Hospital, Sichuan University, from January 2010 to August 2011. They were patients with either the first onset of MDD or the relapse of MDD after discontinuing treatment with antidepressants for at least 3 months. All patients were in accordance with the diagnostic criteria of depressive episodes in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision.25 They all had 24-item Hamilton Depression Rating Scale (HAMD-24) ≥20 points and Hamilton Anxiety Scale (HAMA) ≤14 points. In order to eliminate potential influences from comorbidity of depressive disorder and anxiolytic disorder, we adopted HAMA threshold value of ≤14, which is the critical value used to determine whether there is anxiety in the Chinese norm.26 Patients with one or more of the following criteria were excluded from the study: patients with severe disease such as heart, liver, or kidney disease; women in gestation or who are breastfeeding; and patients who had received repetitive transcranial magnetic stimulation or electroconvulsive treatment within 1 year. The patients were then randomly assigned into two treatment groups: Esc group (30 patients) receiving only escitalopram treatment (a serotonin selective reuptake inhibitor [SSRI]) and JK group (30 patients) who were treated with a combination of escitalopram and Jiuweizhenxin-keli. The healthy control (HC) group included 30 volunteers without any neuropsychiatric diseases, with HAMD-24 scores ≤8 points and HAMA scores ≤7 points. All patients were right handed with normal hearing and verbal communication capabilities and provided their written informed consent before being enrolled in the study.
The methods were designed in accordance with the approved guidelines. The methods and protocol were approved by the West China Hospital Clinical Trials and Biomedical Ethics Committee of Sichuan University (File No 93 of 2011).
Methods
Therapeutic regimen
The patients diagnosed with MDD received treatment for 6 weeks. In the Esc group, the patients received escitalopram (5–20 mg/d). In the JK group, the patients received combination therapy with escitalopram (5–20 mg/d) and Jiuweizhenxin-keli (6–12 g/d). Initially, each patient was given a lower dose of medicine, and then, psychiatrists participating in this study made adjustment to reach the therapeutic dose within the first week of treatment according to the clinical conditions of patients. When a patient suffered from insomnia, a small dose of alprazolam was prescribed temporarily to relieve the symptoms.
Clinical evaluation
Examinations through HAMD-24 scales, HAMA scales, and brain-evoked potentials were employed in this study. For HC group, all examinations were performed only once upon admission into the study (ie, baseline). For two treatment groups, examinations were carried out at three time points: baseline and after a 2-week or 6-week treatment.
Examination of brain-evoked potentials
Electromyography/evoked potential system (MEB-9200; Nihon Kohden, Tokyo, Japan) was employed to record MMN and P50. MMN electrode placement was carried out according to the 10–20 International System of electroencephalogram. Recording electrodes were placed on central zero (Cz) and frontal zero (Fz), reference electrodes were placed in parallel on the mastoid bones of both left and right sides of the skull, and the grounding electrode was placed on Frontal Polar site. Using auditory oddball mode, we randomly gave each subject a series of deviant stimuli (2,000 Hz audio frequency, 80 dB) at a low frequency (20%) mixed with a series of standard stimuli (1,000 Hz audio frequency, 60 dB) at a high frequency (80%). The characteristics of stimuli were as follows: stimulation rate 1 Hz, analysis time 100 ms/div, sensitivity 20 μV/div, record passband 0.1–100 Hz, and deviant stimuli superposition 40 times. The patients were not required to react to any stimulus during the examination. Negative wave was obtained by using waveform induced by deviant stimuli to minus waveform induced by standard stimuli. The biggest negative wave obtained was defined as MMN. The MMN latency of Cz lead was determined with reference to the MMN waveform of Fz lead. P50 was examined using condition (S1)–test (S2) paired acoustic stimulation with short wavelength and sound pressure set at 105 dB. The interval between the two stimuli S1 and S2 was 500 ms, and the interval between two paired stimuli was 10 seconds. The rest of the parameters were as follows: analysis time 30 ms/div, sensitivity 10 μV/div, filter passband 0.1–1,000 Hz, and S1 and S2 stimuli superposition 16 times. The patients were not required to react to any stimulus during the examination. The S1-P50 amplitude, S2-P50 amplitude, S2-P50/S1-P50 amplitude ratio, and percentage of aberrant P50 inhibition (S2-P50/S1-P50 ≥0.5) of Cz lead were recorded during the examination. Previous investigation showed that MMN latency is consistent for healthy people over time.27 Thus, we only measured it once for the HC group at baseline and at all three time points for the Esc and JK groups.
Statistical analysis
SPSS software 12.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The calculation index was expressed as mean value ± standard deviation (SD). One-way analysis of variance and repeated measures analysis of variance were employed when data complied with normal distribution and homogeneity of variance. Nonparametric test was used when data did not conform to normal distribution and homogeneity of variance. P<0.05 was considered as statistically significant.
Results
Characteristics of patients and clinical outcomes
A total number of three groups were included in this study (refer the “Methods” section): HC group consisting of HC participants, Esc group of 30 MDD patients who received treatment of only escitalopram, and JK group of 30 MDD patients who were treated with a combination of escitalopram and Jiuweizhenxin-keli. There are no significant differences in sex composition, age, and education background among the HC, Esc, and JK groups (P>0.05). No significant differences were detected in clinical features such as course and severity of disease between the Esc and JK groups (P>0.05).
To evaluate patient’s severity of depression and level of recovery, HAMD-24 scales were recorded and analyzed for each patient in the Esc and JK groups before and after treatment. The mean (±SD) HAMD-24 scores at admission were 30.09±9.03 and 31.54±8.96 for Esc and JK groups, respectively, which were both markedly elevated compared to the HAMD-24 score of the HC group. After treatment, Hamilton Depression Scale (HAMD) scores decreased in week 2 of treatment and further decreased after 6 weeks of treatment.
Clinical improvement was also observed with HAMA scores before and after treatment. The mean ± SD HAMA scores at admission were 17.48±5.89 and 17.63±6.08 for Esc and JK groups, respectively, which were greatly increased compared to the mean ± SD HAMA score of the HC group. After treatment, HAMD scores decreased in week 2 of treatment and further decreased after 6 weeks of treatment (Table 1).
Mismatch negativity analysis
Having established that both Esc and combination therapy lead to distinguished clinical improvements, we further examined MMN latency to study individual’s brain neuroplasticity. A previous investigation showed that MMN latency is consistent for healthy people over time,27 so we only measured it once for the HC group at baseline. The mean (±SD) values of MMN latency at baseline were significantly prolonged in both the Esc and JK groups compared with the HC group. After 2 weeks of treatment, MMN latency in both the Esc and JK groups decreased. It was still significantly longer than that of the HC group and was not significantly decreased compared with baseline of each group. However, after 6 weeks of treatment, MMN latency further decreased for the Esc and JK groups and was significantly shorter than that of the HC group (Table 2).
Analysis of P50 and related index
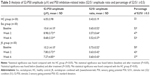
The mean (±SD) values of S2-P50 amplitude were 6.05±3.98, 10.61±4.10, and 10.21±4.10 at baseline for the HC, Esc, and JK groups, respectively. Significant increases were found in both the Esc and JK groups compared with the HC group. After 2 weeks of treatment, reductions in S2-P50 amplitude were found in both treatment groups, though the decrements were not statistically significant compared with the baseline value of each group. Further reductions were observed in both treatment groups after week 6 of treatment. The decrement in the JK group was statistically significant compared with the baseline value, while it was not statistically significant for the Esc group (Table 3).
The mean (±SD) values of P50 inhibition (S2 amplitude/S1 amplitude) at baseline were 0.43±0.19, 0.65±0.52, and 0.73±0.52 for the HC, Esc, and JK groups, respectively. Significant increases were found in both the Esc and JK groups compared with the HC group. After treatment, there were continuous reductions in both treatment groups. The mean (±SD) values decreased to 0.57±0.64 and 0.52±0.37 in week 2 and week 6, respectively, for the Esc group after treatment and were 0.63±0.42 and 0.60±0.43 for the JK group in week 2 and week 6, respectively, of treatment. However, P50 inhibition after treatment still remained significantly higher in both treatment groups than that in the HC group.
Percentages of individuals with P50 inhibition ≥0.5 were 33%, 53%, and 50% for HC, Esc, and JK groups, respectively, at baseline. In the Esc group, percentages of P50 inhibition ≥0.5 decreased to 47% in week 2 and rebounced to 53% in week 6 of treatment. No significant changes were detected in this group after treatment. On the other hand, in the JK group, there were continuous decreases in percentage of P50 inhibition ≥0.5 after treatment. Percentages of individuals with P50 inhibition ≥0.5 decreased to 43% in week 2 of treatment, which was still statistically significant compared to that of the HC group. Furthermore, in week 6 of treatment, percentage of individuals with P50 inhibition ≥0.5 recovered to 37%, which was comparable to that of the HC group (Table 3).
Discussion
In this study, we found that compared to HC, baseline levels of MDD patients greatly increased in electrophysiological parameters such as MMN latency, S2-P50 amplitude, S2-P50/S1-P50 amplitude ratio, and percentage of individuals with S2-P50/S1-P50 ≥0.5, indicating impairment in neuroplasticity of MDD patients. Both monotherapy with escitalopram alone and combination therapy with escitalopram and Jiuweizhenxin-keli exhibited distinguished therapeutic effects from week 2 of treatment and lasted to week 6 after treatment. Monotherapy with escitalopram was able to partially restore patients’ neuroplasticity, by decreasing MMN latency, S2-P50 amplitude, and S2-P50/S1-P50 amplitude ratio. However, monotherapy treatment failed to lead to statistically significant improvement. In contrast, combining escitalopram with Jiuweizhenxin-keli showed distinct effects on MMN latency, S2-P50 amplitude, S2-P50/S1-P50 amplitude ratio, and percentage of individuals with S2-P50/S1-P50 ≥0.5. Downregulation of the parameters in patients was observed after a 2-week treatment, and further decrease was found after a 6-week treatment. Six-week treatment in the JK group resulted in significantly reduced MMN latency and S2-P50 amplitude compared to the baseline level, whereas the percentage of individuals with S2-P50/S1-P50 ≥0.5 were not statistically significant from the HC group. Taken together, these data suggested that combination therapy showed better effect in the reduction of MMN latency and enhancement of P50 inhibition and improved patients’ capability of processing and reaction to novel auditory stimuli, inhibition of interference of unrelated information, and enhancement of SG function. Therefore, compared to monotherapy of SSRI, combining SSRI with Jiuweizhenxin-keli could be a more beneficial solution for MDD patients, as demonstrated by the improvement.
Jiuweizhenxin-keli is a well-known traditional Chinese medicine with active ingredients such as ginsenosides, Rehmannia-related polysaccharides, and jujube seed alcohol. Previous investigations have shown that these active ingredients protect neurons from apoptosis24 and regulate several key molecules and pathways, for example, mRNA expression level of BDNF after chronic stress, level of excitement in the rat hypothalamo-pituitary-adrenal axis of depression model of chronic stress,22 gene expression level of NGF and c-fos, and glutamate level and N-methyl-D-aspartate receptor expression. Bioactivities of these individual components involve in stress and neuroplasticity of MDD, such as increase in BDNF and NGF levels, protection against neuronal apoptosis, regulation of excitatory amino acid level and function, and improvement in chronic stress-related neuroendocrine function10 and may be the underlying mechanisms of Jiuweizhenxin-keli’s therapeutic effects.
The study showed that HAMA and HAMD scores of patients evaluated before and after treatment have demonstrated the clinical improvement of MDD patients receiving escitalopram alone or in conjunction with Jiuweizhenxin-keli. Here, we report the impact of Jiuweizhenxin-keli treatment on electrophysiological features of MDD patients, but these parameters are indirectly linked with neuroplasticity. Therefore, it is of great importance to investigate correlation between electrophysiological data and molecular basis of these events, so as to assess key molecules, including BDNF and NGF, which are more direct indexes of neuroplasticity. Also, our future work will aim to investigate effects of Jiuweizhenxin-keli on clinical symptoms and other clinical parameters. Although treatment with Jiuweizhenxin-keli showed significant improvement in electrophysiological parameters of MDD patients, the study period of this work was relatively short; thus, it is difficult to predict its long-term effect. Studies with longer observation period could clarify this question.
Conclusion
Neuroplasticity of patients with MDD is apparently disturbed, characterized by aberrant electrophysiological measurements such as MMN latency and SG-P50-related event-related potential parameters. Compared with monotherapy with escitalopram alone, combination treatment with escitalopram and a traditional Chinese medicine Jiuweizhenxin-keli showed significant effects in restoring these neuroelectrophysiological features of MDD patients. Taken together, our study suggested that this combination therapy could be a novel therapeutic solution for improving the impaired neuroplasticity of MDD patients.
Disclosure
The authors report no conflicts of interest in this work.
References
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. | ||
Nestler EJ, Barrot M, DiLeone RJ, Eisch AJ, Gold SJ, Monteggia LM. Neurobiology of depression. Neuron. 2002;34(1):13–25. | ||
Rizvi SJ, Kennedy SH. Emerging drugs for major depressive disorder: an update. Expert Opin Emerg Drugs. 2012;17(3):285–294. | ||
Stockmeier CA, Mahajan GJ, Konick LC, et al. Cellular changes in the postmortem hippocampus in major depression. Biol Psychiatry. 2004;56(9):640–650. | ||
Warner-Schmidt JL, Duman RS. Hippocampal neurogenesis: opposing effects of stress and antidepressant treatment. Hippocampus. 2006;16(3):239–249. | ||
Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature. 2008;455(7215):894–902. | ||
Duman RS. Pathophysiology of depression: the concept of synaptic plasticity. Eur Psychiatry. 2002;17(suppl 3):306–310. | ||
Duman RS, Malberg J, Thome J. Neural plasticity to stress and antidepressant treatment. Biol Psychiatry. 1999;46(9):1181–1191. | ||
Pascual-Leone A, Amedi A, Fregni F, Merabet LB. The plastic human brain cortex. Annu Rev Neurosci. 2005;28:377–401. | ||
Pittenger C, Duman RS. Stress, depression, and neuroplasticity: a convergence of mechanisms. Neuropsychopharmacology. 2008;33(1):88–109. | ||
Näätänen R. Attention and Brain Function. Hillsdale, NJ: Lawrence Erlbaum Associates; 1992. | ||
Classen J, Ziemann U. Mulation-induced plasticity in the human motor cortex. In: Boniface S, Ziemann U, editors. Plasticity in the Human Nervous System Investigation with Transcranial Magnetic Stimulation. Cambridge: Cambridge University Press; 2003:135–165. | ||
Näätänen R, Paavilainen P, Tiitinen H, Jiang D, Alho K. Attention and mismatch negativity. Psychophysiology. 1993;30(5):436–450. | ||
Näätänen R, Winkler I. The concept of auditory stimulus representation in cognitive neuroscience. Psychol Bull. 1999;125(6):826–859. | ||
Näätänen R, Sussman ES, Salisbury D, Shafer VL. Mismatch negativity (MMN) as an index of cognitive dysfunction. Brain Topogr. 2014;27(4):451–466. | ||
Zhang X, Chen X, Zhang M, Xiao Z, Zhao J. Experimental study of mismatch negativity in patients with depression. J Shanghai Jiaotong Univ Med Sci. 2006;26(4):351–353. | ||
Patterson JV, Hetrick WP, Boutros NN, et al. P50 sensory gating ratios in schizophrenics and controls: a review and data analysis. Psychiatry Res. 2008;158(2):226–247. | ||
Wang Y, Fang Y, Chen X, et al. Experimental study on sensory gating P50 with conditioning and testing stimulus paradigm in treatment-resistant depression. J Shanghai Jiaotong Univ Med Sci. 2008;28(12):1551–1553. | ||
Kuang W, Li J, Li J, et al. Randomized double-blind controlled trial on effectiveness and safety of Jiu Wei Lv Ping particle in the treatment of generalized anxiety disorder. Chin J Evid Based Med. 2004;4(8):523–527. | ||
An W, Zhang L, Li Y, Xu Y, Cao J, Li L. Effects of water extract from Poria cocos on mitochondrial impairment in hippocampal neurons induced by sodium azide. Zhongguo Yao Xue Za Zhi. 2001;36(7):450–453. | ||
Liu D, Zhang H, Gu W, Liu Y, Zhang M. Neuroprotective effects of ginsenoside Rb1 on high glucose-induced neurotoxicity in primary cultured rat hippocampal neurons. PLoS One. 2013;8(11):e79399. | ||
Zhu L, Chen D, Li Y, Zhang R. Study of the protection of cells apoptosis after rat serious cerebral trauma by ginsenoside and its mechanism. Chin Arch Tradit Chin Med. 2009;27(12):2554–2557. | ||
Zhu Y, Chang X. Pharmacological actions of Radix Rehmann Praeparata and its active components: research advances. Asia Pac Tradit Med. 2011;7(11):173–176. | ||
Zhang X, Ding C, Li H. Research progress on the chemical compositions and pharmacological effects of Semen ziziphi spinosae. Sci Technol Food Ind. 2009;(3):348–350. | ||
Association AP. Diagnostic and Statistical Manual of Mental Disorders. Arlington, VA: American Psychiatric Publishing; 2000. | ||
Ning G. A application of Hamilton anxiety scale in Chinese neurasthenia. Zhonghua Shen Jing Jing Shen Ke Za Zhi. 1986;32:342–344. | ||
Lindin M, Correa K, Zurron M, Diaz F. Mismatch negativity (MMN) amplitude as a biomarker of sensory memory deficit in amnestic mild cognitive impairment. Front Aging Neurosci. 2013;5:79. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.