Back to Journals » Cancer Management and Research » Volume 10
Effects of controlled ovarian stimulation on toxicity of TAC chemotherapy in early breast cancer patients
Authors de Groot S, Louwé LA, Ramautar AIE, Portielje JEA, Ogilvie AC, Batman E, Fiocco M, Kroep JR
Received 17 September 2017
Accepted for publication 23 April 2018
Published 26 September 2018 Volume 2018:10 Pages 3931—3935
DOI https://doi.org/10.2147/CMAR.S151905
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Stefanie de Groot,1 Leoni A Louwé,2 Ashna IE Ramautar,1 Johanneke EA Portielje,1,3 Aernout C Ogilvie,4 Erdogan Batman,5 Marta Fiocco,6,7 Judith R Kroep1
1Department of Medical Oncology, Leiden University Medical Center, Leiden, the Netherlands; 2Department of Gynecology, Leiden University Medical Center, Leiden, the Netherlands; 3Department of Medical Oncology, Haga Hospital, Den Haag, the Netherlands; 4Department of Medical Oncology, OLVG Hospital, Amsterdam, the Netherlands; 5Department of Medical Oncology, Alrijne Hospital, Leiden, the Netherlands; 6Department of Medical Statistics and Bioinformatics, Leiden University Medical Center, Leiden, the Netherlands; 7Mathematical Institute, Leiden University, Leiden, the Netherlands
Background: Oocyte and embryo cryopreservation, using controlled ovarian stimulation (COS), are common fertility preservation methodologies in breast cancer patients receiving gonadotoxic neo (adjuvant) chemotherapy (CT). The effects of COS and peak estradiol levels on CT-induced side effects are unknown.
Patients and methods: Eighteen patients with stage II and III breast cancer underwent oocyte or embryo cryopreservation at Leiden University Medical Center before receiving docetaxel, adriamycin, and cyclophosphamide (TAC) CT (COS group). A control group (N=18) was retrospectively selected from breast cancer patients, aged between 18 and 40, who underwent TAC CT without fertility preservation. CT -induced toxicity in the 2 groups was compared using χ2 analysis. Associations between peak estradiol levels and distinct stimulation protocols and side effects in the COS group were investigated by using regression analysis.
Results: Patient characteristics between both groups were similar, except for a lower age in the COS group vs the control group (30.5 vs 35.2 years, P=0.005). No differences were seen in grade III/IV side effects between both groups. In the COS group, an increase in thrombopenia grade I/II was seen, while grade I/II stomatitis and constipation were significantly lower in the COS group as compared with the control group (P=0.006 and P=0.008, respectively). In the COS group, no association was found between the peak estradiol levels and distinct stimulation protocols and side effects of CT.
Conclusion: COS prior to TAC CT was not associated with an increase in grade III/IV side effects. Interestingly, COS may have a protective effect on mucositis and constipation. Moreover, the peak estradiol levels and distinct stimulation protocols had no effect on grade III/IV side effects in our study.
Keywords: chemotherapy, toxicity, fertility preservation, controlled ovarian hyperstimulation
Introduction
Premenopausal breast cancer patients who receive chemotherapy (CT) have a risk of decreased ovarian reserve, premature ovarian failure, and infertility after treatment.1–3 Therefore, discussion of and referral for fertility preservation in patients who wish to have a child in the future is an essential part of the treatment plan.4–7 As mortality rates have declined over time in this patient group and patients often postpone their first pregnancy,2,8 oocyte and embryo cryopreservation are commonly used fertility preservation options.9 Both approaches require controlled ovarian stimulation (COS) for ~2 weeks. Conventional ovarian stimulation protocols cause high serum levels of estradiol.10,11 To block or to decrease estradiol during COS, new protocols with tamoxifen and aromatase inhibitors in combination with low levels of follicle-stimulating hormone (FSH) are developed.10,12 Studies have shown that COS for fertility preservation with tamoxifen or aromatase inhibitors in patients with breast cancer are unlikely to increase recurrence risk.13–16 The effects of COS and the additional hormonal alterations on toxicity of CT have not been studied. Preclinical evidence shows that sex hormones may interfere with side effects of CT.17,18 Therefore, we conducted a retrospective case–control study of the effects of COS on CT-induced toxicity in early breast cancer patients undergoing oocyte and embryo cryopreservation for fertility preservation prior to neo (adjuvant) docetaxel, adriamycin, and cyclophosphamide (TAC) CT.
Patients and methods
Study population
Eligible patients with early breast cancer stage, Ic, II and III, and underwent oocyte or embryo cryopreservation at the gynecology department of the Leiden University Medical Center (LUMC) between 2009 and 2015. All patients received TAC CT (docetaxel 75 mg/m2 IV, adriamycin 50 mg/m2 IV, and cyclophosphamide 500 mg/m2 IV, day 1, q3 weeks) and were treated in 6 hospitals in the Netherlands. The control group was selected from all patients in the LUMC who underwent TAC CT between 2009 and 2015 without oocyte or embryo cryopreservation and with the age at diagnosis between 18 and 40 years. The retrospective study was conducted according with the Declaration of Helsinki and the Dutch “Code of Good Conduct,” and was approved by the Ethics Committee of the LUMC. Patient consent was assumed as per the no-objection rule of the “Code of Good Conduct” (https://www.federa.org/codes-conduct).
Stimulation protocols
The following stimulation protocols were used: 1) COS protocol with FSH, tamoxifen, and gonadotropin-releasing hormone (GnRH) antagonist; 2) protocol with FSH and a GnRH antagonist alone; and 3) protocol with FSH and a GnRH agonist. Patient received the distinct COS protocols depending on hormone receptor status of the tumor and timing of start in the follicular or luteal phase of the menstrual cycle. Typically, patients received COS on the second or third day of the menstrual bleeding with an average dose of 150 U of FSH subcutaneously with or without 60 mg tamoxifen daily. Until E2 >250 pg/mL and/or the largest ovarian follicles reach 17–18 mm in diameter by ultrasound examination, the stimulation was followed by an human chorionic gonadotropin (HCG) injection (subcutaneous ovitrelle 0.25 mg/d). The oocyte retrieval was performed 36 hours later.
Toxicity
Side effects and hematological toxicity were graded according to the Common Terminology Criteria for Adverse Events version 4.03. Each side effect, documented by the physician, was scored once per patient at maximum during the course, and the highest grade of occurrence was scored.
Blood sampling and assay methods
During the monitoring phase of the COS, venous blood samples were drawn in a serum-separating tube with intervals of 1–4 days. Serum estradiol levels were analyzed by electrochemiluminescence immunoassay (Modular Analytics E 170 Roche Diagnostics, Basel, Switzerland). All samples were analyzed by the accredited clinical laboratory of the LUMC.
Statistical analysis
For the primary endpoint, toxicity due to CT was compared between both groups using chi-square and logistic regression analysis. For the secondary endpoints, peak estradiol serum levels and distinct stimulation protocols were associated with grade III/IV toxicity in the COS group by using regression analysis. Univariate and multivariate odds ratios along with their 95% confidence intervals were estimated. All tests were 2-tailed, and P-values <0.05 were considered significant. All data were analyzed using Statistical Package for Social Sciences software™ 20.0 (IBM Corporation, Armonk, NY, USA).
Results
Patient characteristics
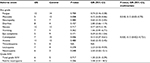
Eighteen patients received COS prior to neo (adjuvant) CT. Ten patients received a COS protocol with tamoxifen and GnRH antagonist, four patients a protocol with a GnRH antagonist alone, and four patients a protocol with a GnRH agonist alone. Eight patients in the COS group received 2 subsequent cycles of COS, whereas 10 patients received 1 cycle of COS. The control group (N=18) consisted of patients who received neo (adjuvant) TAC CT between 2009 and 2016 and were between 18 and 40 years old. Patient characteristics between both groups were similar, except for a lower age in the COS group vs the control group (30.5 vs 35.2 years, P=0.005). Two patients did not receive all 6 cycles of TAC in the COS group. One patient switched after one TAC cycle due to neutropenic enterocolitis (typhlitis) to 3 3-weekly cycles AC followed by 9 weekly cycles of paclitaxel, and 1 patient chose to stop after 4 cycles of TAC without a medical necessity to discontinue the CT. Patient characteristics at diagnosis are summarized in Table 1.
  | Table 1 Patient characteristics Abbreviations: CT, chemotherapy; ER, estrogen receptor; GnRH, gonadotropin-releasing hormone; HR, hormone receptor; OS, ovarian stimulation; PR, progesterone receptor. |
Toxicity
The observed grade III/IV side effects were neutropenic fever, neutropenic enterocolitis, fatigue, and pneumonia. No difference were seen in grade III/IV side effects between both groups. The incidence of side effects that occurred in both groups is given in Table 2. In the COS group an increase in thrombopenia grade I/II was seen; 4 patients had a grade I and 1 patient had a grade II thrombopenia. Grade I/II stomatitis and constipation occurrence was significantly lower in the COS group as compared to the control group (P=0.008 and P=0.006, respectively). These results remained significant in multivariate analysis when adjusting for age (P=0.018 and P=0.020, respectively). No grade V toxicity occurred during the CT in either group.
Estradiol levels and toxicity
In the COS group, no association was found between the peak estradiol levels and distinct stimulation protocols and grade III/IV side effects of CT. The mean peak estradiol serum levels in the protocol with tamoxifen was 8,046 pmol/L (N=10) and in the protocol without tamoxifen 5,717 pmol/L (N=8); the peak estradiol levels per protocol are given in Table 3. The peak estradiol levels were not significantly different (P=0.351).
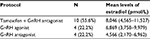  | Table 3 The peak estradiol levels of distinct stimulation protocols Abbreviation: GnRH, gonadotropin-releasing hormone. |
Discussion
This study shows that COS prior to TAC CT is not associated with an increase or decrease in grade III/IV side effects in breast cancer patients treated with neo (adjuvant) TAC CT. To the best knowledge of the authors, this is the first study on effects of COS on CT -induced side effects.
COS for fertility preservation prior to TAC CT appears to be safe in terms of toxicity in breast cancer patients, as it did not increase grade III/IV side effects. However, we found a significant increase in grade I/II thrombopenia in the COS group. Because thrombocytopenia grade II (<75.0×109/L blood platelets) might require delay and/or dose reduction of the CT, these results need to be validated in a larger study.
Interestingly, COS had a protective effect on mucositis and constipation. The protective effect of COS on occurrence of mucositis during CT treatment may be due to the hormonal alterations caused by COS. Analogously, estrogen treatment had a beneficial effect on recurrent aphthous mouth ulcers in premenopausal healthy women19 and on oral discomfort in postmenopausal women.20 Additionally, the estrogen receptor has been detected in the oral mucosa.21,22 Thus, decrease in occurrence of mucositis in the COS group may be due to a transient increase of estradiol levels due to COS and its effects on the oral mucosa. The beneficial effect on constipation may be caused by the hormonal alternations as well. Researchers found a beneficial effect of estrogen on stool consistency and ease of passage in healthy postmenopausal women.23 However, this effect might also be due to variable antiemetics protocols used in the different hospitals, as antiemetics can cause constipation.24
As an alternative for COS, ovarian tissue cryopreservation is an option for breast cancer patients under the age of 35 years with CT resulting in >50% loss of ovarian reserve.25 Although, it does not require COS and can be performed without delaying the start of CT, ovarian tissue cryopreservation requires surgery and is still in the experimental stage. The success rate for pregnancy has been estimated between 11% and 30%;26 however, presumably, the success rate cannot be accurately determined yet.27 Our study results support the usage of COS prior to CT because of the absence of a significant effect on grade III/IV side effects during CT. Moreover, patients with a mutation of BRCA1/2 might choose preimplantation genetic diagnosis, which requires COS and an in vitro fertilization procedure.28
It seems important to emphasize that the sample size of our study was small. Therefore, the results need to be validated in a larger cohort. Another limitation of our study was the significant difference in age between the COS and control group. We cannot rule out that this difference might be related to our results, although we used the same inclusion criteria for age in both groups. Moreover, in this retrospective study, the estradiol levels of the patients in the control group were unknown, and these levels may be valuable for the comparison between both groups in a future study.
Conclusion
In conclusion, COS prior to TAC CT is not associated with an increase in grade III/IV side effects. COS may increase grade I/II thrombocytopenia and may have a protective effect on mucositis and constipation.
Acknowledgment
The authors gratefully acknowledge the physicians R Oosterkamp (Medisch Centrum Haaglanden), M Bos (Reinier de Graaf Hospital), G Jonkers (Alrijne Hospital), and MM Geenen (Sint Lukas Andreas Hospital); PC de Jong (St. Antonius Hospital); G Sonke (Anthoni van Leeuwenhoek Hospital); and AH Jonkoop (Isala).
Disclosure
The authors report no conflicts of interest in this work.
References
Turan V, Oktay K. Sexual and fertility adverse effects associated with chemotherapy treatment in women. Expert Opin Drug Saf. 2014;13(6):775–783. | ||
Partridge AH, Winer EP. Long-term complications of adjuvant chemotherapy for early stage breast cancer. Breast Dis. 2004;21:55–64. | ||
Gadducci A, Cosio S, Genazzani AR. Ovarian function and childbearing issues in breast cancer survivors. Gynecol Endocrinol. 2007;23(11):625–631. | ||
Garvelink MM, Ter Kuile MM, Louwe LA, Hilders CG, Stiggelbout AM. A Delphi consensus study among patients and clinicians in the Netherlands on the procedure of informing young breast cancer patients about fertility preservation. Acta Oncol. 2012;51(8):1062–1069. | ||
Garvelink MM, ter Kuile MM, Fischer MJ, et al. Development of a decision aid about fertility preservation for women with breast cancer in the Netherlands. J Psychosom Obstet Gynaecol. 2013;34(4):170–178. | ||
Canada AL, Schover LR. The psychosocial impact of interrupted childbearing in long-term female cancer survivors. Psychooncology. 2012;21(2):134–143. | ||
Loren AW, Mangu PB, Beck LN, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31(19):2500–2510. | ||
Cossetti RJ, Tyldesley SK, Speers CH, Zheng Y, Gelmon KA. Comparison of breast cancer recurrence and outcome patterns between patients treated from 1986 to 1992 and from 2004 to 2008. J Clin Oncol. 2015; 33(1):65–73. | ||
Lobo RA. Potential options for preservation of fertility in women. N Engl J Med. 2005;353(1):64–73. | ||
Oktay K, Hourvitz A, Sahin G, et al. Letrozole reduces estrogen and gonadotropin exposure in women with breast cancer undergoing ovarian stimulation before chemotherapy. J Clin Endocrinol Metab. 2006; 91(10):3885–3890. | ||
Casper RF, Mitwally MF. Use of the aromatase inhibitor letrozole for ovulation induction in women with polycystic ovarian syndrome. Clin Obstet Gynecol. 2011;54(4):685–695. | ||
Jenninga E, Kroep JR, Hilders CG, Louwe LA, Verburg HJ, Nortier JW. [Fertility preservation in female oncology patients]. Ned Tijdschr Geneeskd. 2008;152(45):2437–2441. Dutch. | ||
Kim J, Turan V, Oktay K. Long-term safety of letrozole and gonadotropin stimulation for fertility preservation in women with breast cancer. J Clin Endocrinol Metab. 2016;101(4):1364–1371. | ||
Oktay K, Buyuk E, Libertella N, Akar M, Rosenwaks Z. Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol. 2005;23(19):4347–4353. | ||
Azim AA, Costantini-Ferrando M, Oktay K. Safety of fertility preservation by ovarian stimulation with letrozole and gonadotropins in patients with breast cancer: a prospective controlled study. J Clin Oncol. 2008;26(16):2630–2635. | ||
Turan V, Bedoschi G, Moy F, Oktay K. Safety and feasibility of performing two consecutive ovarian stimulation cycles with the use of letrozole-gonadotropin protocol for fertility preservation in breast cancer patients. Fertil Steril. 2013;100(6):1681–1685.e1. | ||
Altieri P, Barisione C, Lazzarini E, et al. Testosterone antagonizes doxorubicin-induced senescence of cardiomyocytes. J Am Heart Assoc. 2016;5(1):pii: 0022383. | ||
Imai A, Sugiyama M, Furui T, Tamaya T, Ohno T. Direct protection by a gonadotropin-releasing hormone analog from doxorubicin-induced granulosa cell damage. Gynecol Obstet Invest. 2007;63(2):102–106. | ||
Bishop PM, Harris PW, Trafford JA. Oestrogen treatment of recurrent aphthous mouth ulcers. Lancet. 1967;1(7504):1345–1347. | ||
Giuca MR, Carli E, Pasini M, Bonfigli D, Cappe MR. Evaluation of efficacy of estrogen and phytotherapy in oral cavity alterations of women in menopause. Minerva Ginecol. 2009;61(1):13–22. | ||
Valimaa H, Savolainen S, Soukka T, et al. Estrogen receptor-β is the predominant estrogen receptor subtype in human oral epithelium and salivary glands. J Endocrinol. 2004;180(1):55–62. | ||
Leimola-Virtanen R, Salo T, Toikkanen S, Pulkkinen J, Syrjanen S. Expression of estrogen receptor (ER) in oral mucosa and salivary glands. Maturitas. 2000;36(2):131–137. | ||
Gonenne J, Esfandyari T, Camilleri M, et al. Effect of female sex hormone supplementation and withdrawal on gastrointestinal and colonic transit in postmenopausal women. Neurogastroenterol Motil. 2006;18(10):911–918. | ||
Oncoline. [homepage on the Internet]. Cancer clinical practice guidelines “Nausea and vomiting” [updated June 16, 2014]. Available from: http://www.oncoline.nl/nausea-and-vomiting. Accessed July 1, 2017. | ||
Imbert R, Moffa F, Tsepelidis S, et al. Safety and usefulness of cryopreservation of ovarian tissue to preserve fertility: a 12-year retrospective analysis. Hum Reprod. 2014;29(9):1931–1940. | ||
Donnez J, Dolmans MM, Pellicer A, et al. Restoration of ovarian activity and pregnancy after transplantation of cryopreserved ovarian tissue: a review of 60 cases of reimplantation. Fertil Steril. 2013;99(6):1503–1513. | ||
Andersen CY. Success and challenges in fertility preservation after ovarian tissue grafting. Lancet. 2015;385(9981):1947–1948. | ||
Quinn GP, Vadaparampil ST, Jacobsen PB, et al. Frozen hope: fertility preservation for women with cancer. J Midwifery Womens Health. 2010;55(2):175–180. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.