Back to Journals » Neuropsychiatric Disease and Treatment » Volume 14
Effects of cognitive behavioral therapy for depression on improving insomnia and quality of life in Chinese women with breast cancer: results of a randomized, controlled, multicenter trial
Authors Qiu H, Ren W, Yang Y, Zhu X, Mao G, Mao S, Lin Y, Shen S, Li C, Shi H, Jiang S, He J, Zhao K, Fu Y , Hu X, Gu Y, Wang K, Guo X , He J
Received 16 April 2018
Accepted for publication 24 July 2018
Published 10 October 2018 Volume 2018:14 Pages 2665—2673
DOI https://doi.org/10.2147/NDT.S171297
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Huihua Qiu,1 Wenwei Ren,1 Yanjie Yang,2 Xiongzhao Zhu,3 Guangyun Mao,4 Shanping Mao,5 Yan Lin,6 Shanshan Shen,7 Changjin Li,8 Hongying Shi,4 Suo Jiang,8 Jingjing He,9 Ke Zhao,8 Ye Fu,10 Xiaoqu Hu,11 Yingying Gu,1 Kai Wang,12 Xiuchan Guo,13 Jincai He1,8
1Department of Neurology, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, People’s Republic of China; 2Department of Medical Psychology, Public Health Institute of Harbin Medical University, Harbin, People’s Republic of China; 3Medical Psychological Institute, Second Xiangya Hospital, Central South University, Changsha, People’s Republic of China; 4Department of Preventive Medicine, Wenzhou Medical University, Wenzhou, People’s Republic of China; 5Department of Neurology, RenMin Hospital of Wuhan University, Wuhan, People’s Republic of China; 6Department of Neurology, The Second Affiliated Hospital of Wenzhou Medical University, Wenzhou, People’s Republic of China; 7Department of Geriatrics, Zhejiang Hospital, Hangzhou, People’s Republic of China; 8Department of Psychology, Wenzhou Medical University, Wenzhou, People’s Republic of China; 9Department of Psychiatry, Tongde Hospital of Zhejiang Province, Hangzhou, People’s Republic of China; 10Yinzhou Hospital Affiliated To Medical School of Ningbo University, Ningbo, People’s Republic of China; 11Department of Oncology, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, People’s Republic of China; 12Department of Psychiatry, The First Affiliated Hospital of Anhui Medical University, Hefei, People’s Republic of China; 13Key Laboratory of Laboratory Medicine, School of Laboratory Medicine and Life Science, Wenzhou Medical University, Wenzhou, People’s Republic of China
Purpose: Cognitive behavioral therapy (CBT) for depression had been found to be effective in reducing depressive and anxiety symptoms in breast cancer survivors. It is not known whether CBT for depression would also improve insomnia and quality of life (QOL). The aim of this study was to investigate whether CBT for depression would improve insomnia and QOL in a randomized controlled multicenter trial.
Patients and methods: In this study, breast cancer survivors (n=392) were randomly allocated to the following three groups: CBT (n=98), self-care management (SCM, n=98), and usual care (UC, n=196) in a ratio of 1:1:2. CBT and SCM received a series of nine sessions for 12 weeks, whereas UC received UC only. Insomnia and QOL were evaluated using Athens Insomnia Scale (AIS) and Functional Assessment of Cancer Therapy-Breast (FACT-B) questionnaire at baseline, 4, 12, and 24 weeks.
Results: There was a significant intergroup difference in AIS and FACT-B scores (both P<0.01). CBT showed less insomnia problems and better overall QOL compared with those in SCM and UC (both P<0.01). No significant differences were found between SCM and UC in insomnia problems and overall QOL. Moreover, the effects of CBT on insomnia and QOL were maintained during the follow-up period.
Conclusion: CBT for depression can be effective in improving insomnia problems and QOL in the Chinese breast cancer survivors.
Keywords: cancer, psychotherapy, sleep, prognosis
Introduction
Cognitive behavioral therapy (CBT) has been demonstrated to be effective in reducing depressive and anxiety symptoms.1,2 In the People’s Republic of China, non-pharmacological treatments such as the psychotherapy are still not widely available, partly owing to the differences in culture and socioeconomic structures.3 Although the effectiveness of CBT for depression on depression symptoms and anxiety symptoms had been found,4,5 few studies have been conducted to explore the effectiveness of CBT for depression on insomnia and quality of life (QOL). Therefore, this study sought to examine the effects of CBT for depression on insomnia and QOL.
Insomnia is one of the most common symptoms associated with cancer.6 Moreover, insomnia is particularly frequent in breast cancer survivors relative to other cancer types, affecting 42%–69% of breast cancer survivors.7 The consequences of insomnia can cause psychological and physical functioning impairments,8,9 as well as increased burden of health care system.10 However, insomnia is often overlooked by the patients and caregivers compared with the consequences of cancer itself.11,12
Furthermore, insomnia often co-occurs with depressive symptoms as well as anxiety symptoms,13,14 and the relationships between insomnia and depressive symptoms and insomnia and anxiety symptoms seem to be reciprocal. For example, insomnia increases the risk of depressive symptoms and anxiety symptoms,15,16 and conversely depressive symptoms and anxiety symptoms contribute to the development of insomnia.17 The bidirectionality of the abovementioned relationships suggests that improvement in depressive symptoms and anxiety symptoms might also improve insomnia.
Meanwhile, QOL is negatively associated with depressive symptoms and anxiety symptoms.18,19 Individuals with depressive symptoms or anxiety symptoms had poorer QOL compared with those without these symptoms.20 Besides, as reported in previous research studies, compared with American women with breast cancer, Chinese women are diagnosed with breast cancer at younger ages and undergo more aggressive surgical treatment,21,22 which may exert more severe psychosocial impacts on Chinese women and lead to poorer QOL. According to a multicenter study, both depressive disorder and anxiety disorder had a negative effect on various dimensions of QOL.23 Therefore, QOL is a significant measurement to evaluate the effect of an intervention beyond the improvements in these symptoms. Based on all these, we aim to investigate whether CBT for depression would also be effective in improving insomnia problems as well as QOL among Chinese breast cancer survivors.
Patients and methods
Participants
Participants were screened by direct physician referrals during follow-up appointments between December 26, 2010, and July 24, 2012, from six research centers of breast or oncology clinics across the People’s Republic of China, including: 1) The First Affiliated Hospital of Wenzhou Medical University (n=74); 2) The Second Xiangya Hospital of Central South University (n=64); 3) The First Affiliated Hospital of Anhui Medical University (n=64); 4) The Second Affiliated Hospital of Wenzhou Medical University (n=40); 5) RenMin Hospital of Wuhan University (n=56); and 6) Harbin Medical University (n=94). Demographic data and clinical characteristics were abstracted from the medical records, surgical records as well as the participants’ self-reports. Women were recruited if they: 1) were diagnosed with breast cancer; 2) were aged 20–65 years; 3) had undergone a radical mastectomy within 1 year before the study; 4) had the ability and willingness to give informed consent; 5) had depressive symptoms or anxiety symptoms, defined as Hamilton Depression Rating Scale (HAMD)24 score ≥8, and/or Hamilton Anxiety Scale (HAMA)25 score ≥8. The exclusion criteria was as follows: 1) serious medical illnesses including cardiovascular, liver, or kidney dysfunctions; 2) severe visual or auditory impairments; 3) patients with excessive alcohol drinking or drug abuse; 4) a history of mental disorder or bipolar disorder; 5) patients who had accepted antidepressants or antipsychotics recently or participated in any psychological treatment or clinical trials; and 6) patients with severe depression or suicidal tendencies.
The study was conducted based on the principles of the Declaration of Helsinki and approved by the Human Research and Ethics Committee of the First Affiliated Hospital of Wenzhou Medical University. Besides, this study was registered with ClinicalTrials.gov, number NCT01256008. The researchers obtained the informed consent from the participants after a detailed description of the study.
Intervention
The participants were randomly assigned to the following three groups: CBT (n=98), self-care management (SCM, n=98), and usual care (UC, n=196) by choosing an envelope that contained random number concerning the group assignment. The primary investigators and evaluators were blind to assignment. The participants would not know the group assignments until the first meeting.
Before the research, all the assessors and therapists had received a rigorous unified training and comply with the Standard Operation Procedure (SOP) to ensure the quality of this research. There were 3-day training sessions for all therapists and assessors. The treatment manuals were explained and practiced in role plays. Besides, they discussed the treatment modalities and integrated the existing views. Two prime monitors were delegated by the principal investigator (PI) to check the case report form, progress of research, and operation procedure in each sub-center, and issues were fed back to the PI, who then contacted with the sub-center PI to deal with the issues. In each sub-center, there were two trained therapists who were assigned to conduct the CBT or SCM separately. The therapists, who were kept blinded to outcomes and study hypotheses, would offer the treatment conditions to avoid contamination. To ensure protocol adherence, we would record sessions and script, and we would randomly choose and assess the fidelity of 20% of the recordings and give feedback to the therapists. Power analyses based on the sample size showed that the study retained 90% power to identify the effect sizes, with an α of 0.05.
The participants in CBT received nine sessions based on the manual codified by Aaron T Beck,26 which were specifically designed on the basis of the psychological characteristics of breast cancer patients and took 12 weeks to complete. The 1–5 sessions were carried out once a week and 6–9 sessions every 2 weeks. The intervention combined behavioral, cognitive, and educational strategies. Participants were taught how to identify and restructure any unhelpful thoughts. They were also taught behavioral strategies and some psychological techniques to cope with psychological distress. Meanwhile, they were guided to review the process of emotion change and related physical symptoms, which helped them to feel interaction between psychological and physical symptoms. In the final session, the therapist would encourage all the participants to give a review and summary of what they had learned in the intervention and to share maintenance plan. Participants would be followed up at intervals of 12 weeks after final session. In addition, the participants in the CBT group also received usual medical care throughout the intervention.
Most previous CBT studies used UC or wait-list controls, but we used SCM as an attention control because treatment expectations and potential effects of interacting with the therapist might improve symptoms and function of the participants. The protocol was modified according to the one used by the National Institute of Mental Health Treatment of Depression Collaborative Research Program27 and the University of Pittsburgh’s late-life depression studies.28 As an attention control, SCM also consisted of nine sessions and took 12 weeks to complete. The therapist did not teach participants CBT techniques such as cognitive restructuring and behavior activation. The therapist also avoided some topics about the patient’s behaviors, feelings, or interpersonal issues that may be psychotherapeutic. The therapist focused on the structured protocol including introduction of information about cancer treatments, diet after radical mastectomy, the rehabilitation exercise, and methods for dealing with the complications of breast cancer. Moreover, the therapist would ask general questions about how things were going about the participant’s complications. Participants would also be followed up at intervals of 12 weeks after final session. In addition, the participants also received usual medical care during the study.
In UC, which was designed to assess the efficacy of CBT and SCM, the participants received usual medical care provided by nurses who were professionally trained.
Measures
Before the study, a questionnaire was completed by the participants including demographic and clinical characteristics.
The 17-item Hamilton Depression Scale (HAMD-17)24 and 14-item Hamilton Anxiety Scale (HAMA-14),25 administered by trained psychiatrists, were applied to assess baseline depressive and anxiety symptoms of participants, respectively. Participants with a score of ≥8 were considered to have depressive or anxiety symptoms.
Severity of sleep problems was measured at baseline, 4, 12, and 24 weeks using Athens Insomnia Scale (AIS),29 which is a self-report measure of sleep quality. Each item is measured on a 4-point Likert scale that reflects the insomnia criteria of the 10th edition of the ICD-10. The total score ranges from 0 (absence of any sleep-related problem) to 24 (severe insomnia). Scores of 6 or higher are recognized as insomnia.30
QOL was assessed at baseline, 4, 12, and 24 weeks using Functional Assessment of Cancer Therapy-Breast (FACT-B) questionnaire,31,32 which is a self-report instrument designed to evaluate multidimensional QOL in breast cancer survivors. The FACT-B consisted of five subscales including social well-being (SWB), physical well-being (PWB), functional well-being (FWB), emotional well-being (EWB), as well as breast cancer-specific concerns (BCS), with higher scores indicating better QOL. The psychometric properties, brevity, as well as relevance to patients’ values make FACT-B suitable for the assessment of QOL.
Statistical analyses
Baseline characteristics were compared using the chi-squared test, one-way ANOVA, and the Kruskal–Wallis test, as appropriate. When ANOVA showed significant differences among three groups, the post hoc Tukey test was applied to assess differences in two-group comparisons. Bonferroni corrections were used to adjust for multiple testing. Based on the intention-to-treat principle, full analysis set (FAS, including all the participants) was established to be emphatically analyzed, the result of which proved to be consistent with the Per Protocol Set (PPS, excluding the withdrawal participants). Missing data were dealt by the last-observation-carried-forward (LOCF) approach.
The changes in AIS and QOL scores during the 24 weeks were analyzed using the repeated measures ANOVA (RM-ANOVA). Effect sizes were estimated by partial eta (ηp2), with 0.01–0.06, 0.06–0.14, as well as 0.14 or higher corresponding to small, moderate, as well as large effect sizes.33
Statistical analyses were performed using IBM SPSS Statistics 19.0 (IBM Corporation, Armonk, NY, USA). All P-values were two-tailed, and the significance level was set at 0.05.
Results
Enrollment and participant characteristics
Figure 1 shows the flow of participants through the course of the study. A total of 493 individuals were screened; of whom, 392 were finally enrolled and signed informed consent. Furthermore, the 392 participants enrolled in this study were randomly allocated to CBT, SCM, and UC. The demographic and baseline clinical variables of participants are shown in Table 1. No intergroup difference was found in baseline characteristics except the baseline HAMD, HAMA (P<0.01), and BCS (P<0.05) scores, for which they were included as the covariates in the following RM-ANOVA. Furthermore, in the study population (n=392), 239 participants (61.0%) reported clinical levels of insomnia (defined as an AIS score of ≥6). At baseline, the average levels of insomnia in each group approached the cutoff (an AIS score of 6), indicating clinical insomnia, respectively (Table 1).
  | Figure 1 Flow chart of the participants through the randomized trial. |
Effect of CBT for depression and SCM on insomnia
All three groups showed a downward trend over time in the AIS scores, but the reduction in AIS scores in CBT was much greater than that in SCM and UC (Figure 2). Meanwhile, the effect of CBT was maintained after its termination (12 weeks). As demonstrated in Table 2, a significant intergroup difference in AIS scores was found (P<0.001), with a moderate effect size (ηp2=0.115). In two-group comparisons, the AIS scores in CBT were significantly lower compared with those in SCM and UC (both P<0.01). However, the difference in the AIS scores was not significant between SCM and UC.
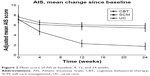  | Figure 2 Mean score of AIS at baseline, 4, 12, and 24 weeks. |
Furthermore, a significant main effect of time for change in the AIS scores was found (P<0.001), with a large effect size (ηp2=0.385). The group by time interaction was also significant for the AIS scores (P<0.001), with a moderate effect size (ηp2=0.109).
Effect of CBT for depression and SCM on QOL
All three groups showed an upward trend over time in the scores of total FACT-B (overall QOL), but the improvement in CBT was much greater than that in SCM and UC (Figure 3). Furthermore, the effect of CBT was maintained after its termination (12 weeks). Besides, as Table 2 demonstrates, a significant intergroup difference in the scores of overall QOL was found (P<0.001), with a large effect size (ηp2=0.198). Meanwhile, a significant intergroup difference in the scores of five subscales was also found (all P<0.01). In two-group comparisons, results show that CBT reported higher levels of overall QOL, PWB, SWB, EWB, FWB, and BCS (all P<0.01) than SCM and UC. SCM had a higher level of FWB (P<0.05) than UC.
Moreover, a significant main effect of time for change in the score of overall QOL was found, with a large effect size (ηp2=0.564). The group by time interaction was significant for the score of overall QOL as well, with a moderate effect size (ηp2=0.137). In addition, a significant main effect of time for change in the scores of the five subscales was also found (all P<0.001). The group by time interaction was also significant for the scores of the five subscales (all P<0.001).
Discussion
To the best of our knowledge, this is the first report in the People’s Republic of China evaluating the effect of CBT for depression on insomnia and QOL in breast cancer survivors. The results indicate that CBT for depression is effective for insomnia and QOL in breast cancer survivors. In this report, reduction in insomnia symptoms and improvement in QOL were significantly greater in CBT compared with those in SCM and UC.
Previous studies had shown the efficacy of CBT for insomnia in breast cancer survivors.34,35 Meanwhile, CBT for insomnia was also found to be effective in reducing depressive symptoms.36 However, only a few randomized controlled trials had been conducted on the efficacy of CBT for depression on insomnia.37 Before intervention, the average levels of insomnia in each group approached the cutoff (an AIS score of 6), indicating clinical insomnia. Our results indicated that CBT for depression showed a significant remission of insomnia compared with that in SCM and UC. Although we found reduction in insomnia symptoms over time in all three groups, the reduction in CBT was quicker and greater than SCM and UC. Moreover, we also observed that the adjusted mean AIS score was lower than 6 (the cutoff score used to define clinical insomnia30 in CBT at the 4-week evaluation), whereas the score was above this cutoff score in SCM and UC at the 4-week evaluation. Considering that an AIS score of 6 is used to distinguish clinical insomnia from normal sleep, this is a significant finding, which indicated that the reduction of insomnia problems was quicker in CBT than SCM and UC during the intervention. In addition, we found that the effect of CBT for depression on insomnia symptoms was maintained after the 12-week intervention. These results validated clinical usefulness of CBT for depression in the treatment of insomnia. CBT for depression might reduce insomnia problems via different mechanisms. On the one hand, the behavioral strategies and psychological techniques learned in CBT could also be applied to deal with unhelpful thoughts about sleep. On the other hand, CBT for depression might also reduce anxiety symptoms, which affect insomnia in that individuals with insomnia are overpowered by physiological hyperarousal, intrusive thoughts, and worrisome thinking.38
Another positive outcome associated with CBT was improvement in overall QOL. We observed that all three groups showed an upward trend in the overall QOL over time; however, the improvement was much greater in CBT compared with that in SCM and UC. This was consistent with previous studies supporting the effect of CBT for depression on improving QOL.39–41 In addition, this study also showed higher scores of five subscales in CBT than SCM and UC. Furthermore, we found that the treatment gain in CBT during the follow-up period on QOL was maintained. These results highlighted the effect of CBT for depression on improving QOL in breast cancer survivors. The effect of CBT on QOL in this study may attribute to reduction of depression symptoms as well as acquisition of behavioral strategies and psychological techniques to cope with psychological distress, which helped patients adopt a more helpful or realistic view of the existing circumstances and better adapt themselves to dissatisfying life circumstances.
In this study, SCM was designed as an attention control. Although SCM showed a higher level of FWB than UC, no differences were found between SCM and UC in the AIS scores and overall QOL, which indicated that additional clinical supervision and support provided to participants might not have an impact on participants’ insomnia and overall QOL. The superiority of CBT to SCM in improving participants’ insomnia and QOL in this study highlighted the efficacy of CBT.
Study limitations
However, this study still has some limitations. First, we did not collect other clinical variables that might have an influence on insomnia and QOL, such as lymphedema after surgery, as well as menopausal symptoms. Second, participants in CBT were more depressed or anxious compared with those in SCM as well as UC at baseline. Although the baseline HAMD and HAMA scores were controlled statistically, we could not exclude the possibility that breast cancer patients with more depressive or anxiety symptoms would respond better to intervention, thus impacting the results to some extent. Finally, polysomnography (PSG) was not conducted in this study, which may reflect the insomnia more objective.
Conclusion
In spite of these limitations, this 24-week study shows a significant effect of CBT for depression on insomnia and QOL for breast cancer survivors in the People’s Republic of China. Further investigation may focus on whether CBT for insomnia would also reduce depressive and anxiety symptoms in the breast cancer survivors and determine which intervention is more beneficial to patients.
Acknowledgments
This research was supported by the National Key Technologies R&D program in the 11th 5-year plan from the Ministry of Science and Technology of the People’s Republic of China (grant number: 2009BAI77B06). Many thanks to Chunyan Zhu, Liuxiu Xu, Yiqun Yu, Xiaodan Xie, and Li Chen for their assistance in project management.
Author contributions
Jincai He, Changjin Li, and Suo Jiang designed the study and wrote the protocol. Xiongzhao Zhu, Yanjie Yang, Yan Lin, Shanshan Shen, Jingjing He, Ye Fu, Xiaoqu Hu, and Kai Wang conducted the trial. Huihua Qiu conducted literature searches and provided summaries of previous research studies. Guangyun Mao, Shanping Mao, Hongying Shi, Xiuchan Guo, Ke Zhao, and Yingying Gu conducted the statistical analyses. Huihua Qiu and Wenwei Ren wrote the first draft of the manuscript. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
de Jong M, Peeters F, Gard T, et al. A Randomized Controlled Pilot Study on Mindfulness-Based Cognitive Therapy for Unipolar Depression in Patients With Chronic Pain. J Clin Psychiatry. 2018;79(1):15m10160. | ||
Berardelli I, Bloise MC, Bologna M, et al. Cognitive behavioral group therapy versus psychoeducational intervention in Parkinson’s disease. Neuropsychiatr Dis Treat. 2018;14:399–405. | ||
Chen J. Seeking help for psychological distress in urban China. J Community Psychol. 2012;40(3):319–341. | ||
Shinmei I, Kobayashi K, Oe Y, et al. Cognitive behavioral therapy for depression in Japanese Parkinson’s disease patients: a pilot study. Neuropsychiatr Dis Treat. 2016;12:1319–1331. | ||
Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clin Psychol Rev. 2006;26(1):17–31. | ||
Mercier J, Savard J, Bernard P. Exercise interventions to improve sleep in cancer patients: A systematic review and meta-analysis. Sleep Med Rev. 2017;36:43–56. | ||
Savard J, Ivers H, Villa J, Caplette-Gingras A, Morin CM. Natural course of insomnia comorbid with cancer: an 18-month longitudinal study. J Clin Oncol. 2011;29(26):3580–3586. | ||
Otte JL, Carpenter JS, Theories CJS. Theories, models, and frameworks related to sleep-wake disturbances in the context of cancer. Cancer Nurs. 2009;32(2):90–104. quiz 105–106. | ||
Sateia MJ, Lang BJ. Sleep and cancer: recent developments. Curr Oncol Rep. 2008;10(4):309–318. | ||
Berger AM, Parker KP, Young-Mccaughan S, et al. Sleep wake disturbances in people with cancer and their caregivers: state of the science. Oncol Nurs Forum. 2005;32(6):E98–E126. | ||
Sateia MJ, Nowell PD. Insomnia. Lancet. 2004;364(9449):1959–1973. | ||
Savard J, Morin CM. Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol. 2001;19(3):895–908. | ||
Barlow DH. Unraveling the mysteries of anxiety and its disorders from the perspective of emotion theory. Am Psychol. 2000;55(11):1247–1263. | ||
Jansson-Fröjmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. 2008;64(4):443–449. | ||
Chen PJ, Huang CL, Weng SF, et al. Relapse insomnia increases greater risk of anxiety and depression: evidence from a population-based 4-year cohort study. Sleep Med. 2017;38:122–129. | ||
Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135(1–3):10–19. | ||
van Mill JG, Hoogendijk WJ, Vogelzangs N, van Dyck R, Penninx BW. Insomnia and sleep duration in a large cohort of patients with major depressive disorder and anxiety disorders. J Clin Psychiatry. 2010;71(3):239–246. | ||
Takahashi T, Higuchi Y, Komori Y, et al. Quality of life in individuals with attenuated psychotic symptoms: Possible role of anxiety, depressive symptoms, and socio-cognitive impairments. Psychiatry Res. 2017;257:431–437. | ||
Gold M, Dunn LB, Phoenix B, et al. Co-occurrence of anxiety and depressive symptoms following breast cancer surgery and its impact on quality of life. Eur J Oncol Nurs. 2016;20:97–105. | ||
Kasteenpohja T, Marttunen M, Aalto-Setälä T, Perälä J, Saarni SI, Suvisaari J. Outcome of depressive and anxiety disorders among young adults: Results from the Longitudinal Finnish Health 2011 Study. Nord J Psychiatry. 2018;72(3):1–9. | ||
Sivasubramaniam PG, Zhang BL, Zhang Q, et al. Breast Cancer Disparities: A Multicenter Comparison of Tumor Diagnosis, Characteristics, and Surgical Treatment in China and the U.S. Oncologist. 2015;20(9):1044–1050. | ||
Fan L, Strasser-Weippl K, Li JJ, et al. Breast cancer in China. Lancet Oncol. 2014;15(7):e279–e289. | ||
Shim EJ, Hahm BJ, Yu ES, et al. Prevalence, correlates, and impact of depressive and anxiety disorder in cancer: Findings from a multicenter study. Palliat Support Care. In press 2017. | ||
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. | ||
Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–55. | ||
Allen NB. Cognitive therapy of depression. In: John Rush A, Shaw Brian F, Emery Gary, editors. The Australian and New Zealand journal of psychiatry, Vol. 36(2). New York: Guilford Press; 1979–2002:275–278. | ||
Fawcett J, Epstein P, Fiester SJ, Elkin I, Autry JH. Clinical management – imipramine/placebo administration manual. NIMH Treatment of Depression Collaborative Research Program. Psychopharmacol Bull. 1987;23(2):309–324. | ||
MD M, BP P, III RC. Medication Clinic Training Procedures and Treatment Manual. PA: University of Pittsburgh; 1998. | ||
Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2000;48(6):555–560. | ||
Soldatos CR, Dikeos DG, Paparrigopoulos TJ. The diagnostic validity of the Athens Insomnia Scale. J Psychosom Res. 2003;55(3):263–267. | ||
Sander AP, Hajer NM, Hemenway K, Miller AC. Upper-extremity volume measurements in women with lymphedema: a comparison of measurements obtained via water displacement with geometrically determined volume. Phys Ther. 2002;82(12):1201–1212. | ||
Ng R, Lee CF, Wong NS, et al. Measurement properties of the English and Chinese versions of the Functional Assessment of Cancer Therapy-Breast (FACT-B) in Asian breast cancer patients. Breast Cancer Res Treat. 2012;131(2):619–625. | ||
Sockloff AL. Statistical power analysis for the behavioral sciences. In: Cohen Jacob, editor. Eval Program Plann, Vol. 1(3). New York: Academic Press; 1977–1978:249–250xv + 474 pp., $24.50 (revised edition). | ||
Savard J, Simard S, Ivers H, Morin CM. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part I: Sleep and psychological effects. J Clin Oncol. 2005;23(25):6083–6096. | ||
Zhou ES, Partridge AH, Recklitis CJ. A pilot trial of brief group cognitive-behavioral treatment for insomnia in an adult cancer survivorship program. Psychooncology. 2017;26(6):843–848. | ||
Ashworth DK, Sletten TL, Junge M, et al. A randomized controlled trial of cognitive behavioral therapy for insomnia: an effective treatment for comorbid insomnia and depression. J Couns Psychol. 2015;62(2):115–123. | ||
Mason E, Harvey A. Insomnia before and after treatment for anxiety and depression. J Affect Disord. 2014;168:415–421. | ||
Harvey AG. A cognitive model of insomnia. Behav Res Ther. 2002;40(8):869–893. | ||
Jeyanantham K, Kotecha D, Thanki D, Dekker R, Lane DA. Effects of cognitive behavioural therapy for depression in heart failure patients: a systematic review and meta-analysis. Heart Fail Rev. 2017;22(6):731–741. | ||
Hofmann SG, Curtiss J, Carpenter JK, Kind S. Effect of treatments for depression on quality of life: a meta-analysis. Cogn Behav Ther. 2017;46(4):265–286. | ||
Oei TP, Mcalinden NM. Changes in quality of life following group CBT for anxiety and depression in a psychiatric outpatient clinic. Psychiatry Res. 2014;220(3):1012–1018. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



