Back to Journals » Cancer Management and Research » Volume 14
Effects of Breast-Conserving Surgery Combined with Immediate Autologous Fat Grafting on Oncologic Safety, Satisfaction and Psychology in Patients with Breast Cancer: A Retrospective Cohort Study
Authors Gong F , Zhou X , Niu Z , Mao Y, Wang Y, Lv M, Gao X , Liu W , Wang H
Received 10 December 2021
Accepted for publication 23 February 2022
Published 10 March 2022 Volume 2022:14 Pages 1113—1124
DOI https://doi.org/10.2147/CMAR.S353370
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Antonella D'Anneo
Fang-xue Gong,1 Xin Zhou,2 Zhao-he Niu,1 Yan Mao,1 Yong-mei Wang,1 Meng Lv,1 Xue-qiang Gao,1 Wen-jing Liu,1 Hai-bo Wang1
1Department of Breast Disease Center, The Affiliated Hospital of Qingdao University, Qingdao, Shandong Province, People’s Republic of China; 2Qingdao Medical College of Qingdao University, Qingdao, Shandong Province, People’s Republic of China
Correspondence: Hai-bo Wang, Department of Breast Disease Center, The Affiliated Hospital of Qingdao University, No. 59 Haier Road, Laoshan District, Qingdao City, Shandong Province, People’s Republic of China, Tel +86 18661805787, Email [email protected]
Purpose: Autologous fat grafting (AFG) is a technique that can improve the appearance of breasts in surgical patients. There are currently few studies on breast-conserving surgery (BCS) combined with immediate AFG, although we believe that it could achieve satisfactory effects. Therefore, the purpose of this study is to observe the effects of BCS combined with immediate AFG on oncologic safety, satisfaction and psychology of breast cancer patients.
Patients and Methods: We retrospectively collected the data of 85 breast cancer patients from February 2018 to October 2018. After screening, 40 patients in AFG group (AG, BCS combined with immediate AFG) and 40 patients in control group (CG, BCS alone) were finally included in the study. The primary outcomes were the survival, tumor recurrence and metastasis, and BREAST-Q score of patients. The secondary outcomes were short and long-term complications, degree of depression and anxiety of patients.
Results: A total of 80 patients were included in the analysis. There was no significant difference in the clinicopathological data between the two groups (P> 0.05). The average follow-up time of the two groups was 40.58± 2.630 and 40.28± 2.679 months. In the analysis of oncologic safety, no patients died in AG and 1 patient died in CG. In addition, there was no significant difference between the two groups in terms of the overall recurrence rate and the distribution of recurrence types (P> 0.05). As for satisfaction, the BREAST-Q score of AG was significantly higher than that of CG (57.85± 4.833 vs 51.93± 5.045, P< 0.001). In the secondary outcomes, there was no short-term complication specified in the study; in the long-term complications, the incidence of calcification in AG was not significantly higher than that in CG (P=0.065). In the analysis of depression and anxiety, there was no significant difference between the two groups (P> 0.05).
Conclusion: BCS combined with immediate AFG can significantly improve patients’ satisfaction without increasing the risk of death and tumor recurrence. However, it does not seem to play a role in improving the conditions of depression and anxiety.
Keywords: breast cancer, breast-conserving surgery, autologous fat grafting, oncologic safety, BREAST-Q, psychology
Introduction
Burden of Breast Cancer
Breast cancer is one of the most common cancers in women. In 2020, breast cancer surpassed lung cancer to become the highest morbidity cancer in the world, accounting for about 11.7% of all malignant tumors and nearly a quarter of the female population.1 In Asia, the incidence of breast cancer is also rising rapidly. A series of factors have contributed to the occurrence of breast cancer.2,3 On the one hand, as people’s awareness of prevention and health care has increased, the detection rate of breast cancer has risen accordingly; on the other hand, it is also related to people’s lifestyle, delayed delivery, and overweight. In addition, breast cancer has also brought a huge burden to personal finances and medical insurance.4,5 With the improvement of medical standards, health awareness, and economic conditions, the 5-year survival rate of female breast cancer has reached 73%, and the 10-year survival rate has reached 61%.6 In areas where the above-mentioned conditions are developed, this rate will be even higher. Therefore, patients’ expectations for treatment have also been greatly improved compared to the past. Not only must the treatment effect be satisfied, but also the quality of life and labor ability must not be affected as much as possible.7 Especially for young women, the aesthetic requirements are relatively higher. Therefore, this puts forward higher requirements for surgical treatment.
Surgical Treatment and AFG
The surgical treatment of breast cancer has developed over more than one hundred years. From simple tumor resection to classic modified radical mastectomy, to breast-conserving surgery (BCS), etc. This long process reflects the shift in the focus of treatment by doctors, and the improvement of patients’ demand for treatment. That is, “a longer but better life for breast cancer patients”. The necessary condition for the optimization of these treatments is the guarantee of safety. After decades of research and amelioration, BCS, combined with adjuvant radiotherapy and chemotherapy, can achieve the ideal comprehensive therapeutic effect. However, there are still some problems with this surgery. Simple BCS will leave partial collapse of the breast area, bilateral asymmetry, etc.,8 and local radiotherapy will also affect the cosmetic effect, so this does not satisfy the patient’s demand. As one of the important adjunct of breast reconstruction, autologous fat grafting (AFG) has gained popularity recently for improving breast contour, beautifying symmetry, trimming volume, and reducing scar contracture and hardening.9,10 In addition, AFG can also alleviate patients’ depression and anxiety about appearance, thereby regulating mental health and improving quality of life.11 Although many recent literatures have demonstrated the oncologic safety of AFG following BCS,12–14 there are still controversial reports on the risk of cancer recurrence with AFG. Particularly, few studies have been focused on the immediate AFG combined with BCS in breast cancer patients. Therefore, more researches are needed to investigate oncologic safety of immediate AFG, such as survival rate, local recurrence rate, so that this procedure with great potential can be widely used in clinic. In keeping with this purpose, the present study aimed to summarize and analyze the short- and long-term clinical outcomes of breast cancer patients after BCS combined with immediate AFG.
Patients and Methods
Data Source
This is a retrospective cohort study. Data was gathered from the hospital information system or paper medical records. It was carried out at the Department of Breast Disease Center, the Affiliated Hospital of Qingdao University, between February 1, 2018 and October 31, 2018. A total of 85 patients were initially collected. After screening, 80 patients met the criteria and were divided into 2 groups. 40 patients who underwent BCS combined with immediately AFG were in AFG group (AG) and 40 patients who underwent BCS alone were control group (CG). The study was approved by the ethics committee of the Affiliated Hospital of Qingdao University. The ethic approval number is QYFYWZLL26704. This study was conducted in accordance with the Declaration of Helsinki. And informed consents have been obtained from all patients included in this study.
Inclusion and Exclusion Criteria
The inclusion and exclusion criteria were as follows. Inclusion criteria: 1. Female patients with invasive breast cancer who underwent breast-conserving surgery; 2.30–65 years old; 3. With conditions for long-term follow-up (main urban areas; neighboring districts and counties). Exclusion criteria: 1. T stage III or IV (AJCC-American Joint Committee on Cancer, 8th Edition Cancer Staging); 2. Received chest radiotherapy or neoadjuvant chemotherapy; 3. Preoperative distant metastasis; 4. Bilateral breast cancer; 5. Personal or family history of breast cancer; 6. Tumors in the nipple and areola area; 7. American Society of Anesthesiologists (ASA) grade>3.
Surgery Procedure
Both groups underwent BCS (nipple and areola-sparing surgery) under general anesthesia with supine position. Axillary incisions can be used for tumors in the upper outer quadrant, and areola incisions can be used for tumors in the lower outer quadrant and near the center. Extensive segmental resection was performed to remove the tumor. During the operation, the margins were taken and sent for frozen tissue pathological examination. If the histopathological results of margins were positive, the corresponding periluminal tissues were enlarged resected until negative margins were obtained. Patients in the AG were immediately given AFG, harvested by low-pressure liposuction, and moderate centrifugation. The machine is the all-in-one liposuction transplantation machine produced by Yanshan Medical Equipment Co., Ltd. AFG follows the Coleman principle: minimally invasive fat harvesting; moderate centrifugation; multi-point, multi-level, and micro-injection. The specific method is as follows: 1. Abdominal liposuction is carried out by syringe suction method (20mL syringe, 2mm aperture liposuction needle). The upper abdomen is mostly selected for the suction site without changing the body position. The extracted fat and swelling suspension are placed in a centrifuge with a centrifugation radius of 20 cm and speed of 1000 r/min for 3 minutes to remove oil and liquid components; 2. Transfer the prepared fat granule graft to a 20 mL syringe and inject it evenly with a 1.4 mm blunt needle into the defect site. The level of fat grafting is the sub-pectoral, intra-pectoral, intra-glandular, and subcutaneous fat; 3. Disperse fat by local massage after injection to avoid fat accumulation.
It should be noted that we performed the BCS according to the indications formulated by the Chinese Anti-Cancer Association (CACA) Guidelines and Standards for Breast Cancer Diagnosis and Treatment 2018 Edition. In addition, we will introduce various breast reconstruction surgeries to the patients before surgery. After the patients fully understanding the process, risks and benefits of various breast reconstruction surgeries, we will decide whether to perform AFG according to the patients’ wishes. If the patient is a high-risk group of AFG (such as family history, BRCA-1 or BRCA-2 gene carrier) we do not recommend her for AFG treatment.
Outcomes
The primary outcomes of this study were as follows: 1. Results related to oncologic safety (survival, recurrence, metastasis rate, etc.). Tumor recurrence and metastasis were evaluated based on clinical evaluation, postoperative molybdenum target mammography, breast ultrasound, and MRI imaging results. Tumor recurrence was divided into local, regional or distant metastasis. The recurrence of breast tissue or skin was classified as local recurrence; the recurrence of ipsilateral armpit, subclavian and intramammary lymph nodes was classified as regional recurrence; distant metastasis referred to metastasis to other tissues and organs. An outpatient follow-up was conducted 2 months after the patient was discharged, and then a telephone follow-up was conducted every 6 months. 2. The patient’s satisfaction with the appearance of the postoperative breast. We conducted a questionnaire survey at the first postoperative follow-up and used BREAST-Q-BCT MODULE (POSTOPERATIVE) VERSION 2.0 SATISFACTION WITH BREAST to investigate. We used a table with 11 questions about breasts of patients as follows: (1) How you look in the mirror clothed. (2) The shape of your lumpectomy breast when you are wearing a bra. (3) How normal you feel in your clothes. (4) Being able to wear clothing that is more fitted. (5) How your lumpectomy breast sits/hangs. (6) How smoothly shaped your lumpectomy breast looks. (6) The contour (outline) of your lumpectomy breast. (7) The contour (outline) of your lumpectomy breast. (8) How equal in size your breasts are to each other. (9) How normal your lumpectomy breast looks. (10) How much your breasts look the same. (11) How you look in the mirror unclothed. The selection was divided into four levels: (1) Very Dissatisfied. (2) Somewhat Dissatisfied. (3) Somewhat Satisfied. (4) Very Satisfied. After calculating the sum score, the equivalent score transformed by CONVERSION TABLE was used for analysis.
The secondary outcomes were as follows: 1. Postoperative complications. The short-term complications include infection, bleeding, subcutaneous effusion, flap necrosis, upper limb edema. The long-term complications include calcification, cyst, fat liquefaction, necrosis. 2. Psychological related conditions include depression and anxiety. We used Self-Rating Depression Scale (SDS) to assess the depression status of patients. After the standard score was calculated, the divided degree of depression was taken as the evaluation result. We used Self-Rating Anxiety Scale (SAS) to assess patients’ anxiety. Similar to the SDS, it is also a scale with 20 items and 4 grades, which is used to evaluate the subjective feelings of anxiety patients. Finally, the divided anxiety degree was used as the evaluation result.
Statistical Analysis
All statistical analysis was performed using SPSS 21.0. The level of significance for all statistical tests was set at 0.05 (α=0.05). Data are presented as means and standard deviations (Mean±SD) for continuous variables and as proportions for categorical variables. The continuous variables were assessed using Student’s t-test when Gaussian distribution is verified. Otherwise Wilcoxon rank sum test will be used alternatively. The association between categorical variables were assessed using Chi-squared test (χ2). The ordinal variables were assessed using Wilcoxon rank sum test. A two-tailed P value of <0.05 was regarded as statistically significant.
Results
Baseline Data
The flow diagram of this study was shown in Figure 1. The general characteristics of were shown in Table 1. The results of surgery, pathology and immunohistochemistry were shown in Table 2. As can be seen from the tables, there was no statistical difference between the 2 groups of patients in various clinicopathological data (P>0.05). That’s why we did not match the variables of patients. And it should be noted that the operations of all patients were performed by the same surgical team, including anesthesia and nursing staff. In addition, the postoperative treatment of all patients was carried out in accordance with the guidelines of the Chinese Society of Clinical Oncology (CSCO), including radiotherapy, chemotherapy, endocrine therapy, and targeted therapy.
 |
Table 1 General Characteristics of Patients (n=80) |
 |
Table 2 Surgery, Pathology and Immunohistochemistry Data (n=80) |
 |
Figure 1 Flow diagram. Abbreviations: ASA, American Society of Anesthesiologists; AG, autologous fat grafting group; CG, control group. |
Primary Outcomes
According to the data in Table 3, the average follow-up time of the two groups was about 40 months. During the follow-up, the number of tumor recurrences in AG and CG were 3 and 4 respectively, and there was no significant difference in the recurrence rate (P=0.692). Further comparing the distribution of recurrence types, there was still no significant difference (P=0.798). No patient in AG died during the follow-up; 1 patient in CG died 31 months after operation due to local tumor recurrence. In addition, in terms of patients’ satisfaction with breast surgery, the BREAST-Q scores in AG was statistically higher than CG (P<0.001) and detailed score (original score) was shown in Table 4. We did not perform statistical analysis on the original score of individual question because there was no separate equivalent score for single question in the CONVERSION TABLE provided by BREAST-Q.
 |
Table 3 Primary Outcomes (n=80) |
 |
Table 4 Detailed Score of BREAST-Q (n=80) |
Secondary Outcomes
According to the data in Table 5, there was no short-term complication occurred in both groups. As for long-term complications, calcification was found in 5 patients in AG, and there was no significant difference between two groups (P=0.065). In the comparison of the degree of depression and anxiety, there was no significant difference in the distribution of the two groups (P=0.260; P=0.459).
 |
Table 5 Secondary Outcomes (n=80) |
Discussion
Application of AFG and Oncologic Safety
With the increase of global incidence, breast cancer has become a malignant disease that seriously threatens women’s physical and mental health. However, it has become a cancer with great therapeutic effect due to the increasingly mature and standardized comprehensive treatment. It is precisely because of the significant improvement in survival rate that patients have an increasing demand for breast reconstruction, not just satisfied with BCS. Regarding breast reconstruction, the current mainstream methods include prosthesis implantation, autologous flap reconstruction, AFG, etc. Generally, we choose the reconstruction method according to the different surgical conditions of patients and their own needs. Since Professor Frenz Neuber first used AFG to treat facial defects in 1893, the AFG technique has a history of more than 100 years. In 1997, Professor Coleman adopted centrifugation and intraoperative non-invasive transfer methods to improve the AFG technique, which has now become one of the internationally recognized methods.15 The number of AFG is also increasing year by year. In 2018, more than 30,000 AFG operations were performed in the United States.16 Compared with other methods, AFG is relatively simple with less blood loss and easy access to fat, making it an ideal minimally invasive procedure to reconstruct soft tissue defects caused by BCS. However, there has been widespread concern that AFG increases the risk of breast cancer recurrence. In theory, adipocytes can release regulatory factors through multiple ways to create a microenvironment suitable for proliferation and invasion of breast cancer cell.17 The phenotype of adipocytes will also change under the influence of tumor cells,18 such as reduced differentiation potential and expression of cancer antigens.19 And these mutations will increase the tumorigenicity of adipose derived stem cells. In addition, cancer stem cells also secrete some factors that promote the growth and migration of cancer tissues, such as vascular endothelial growth factor (VEGF) and interleukin (IL-6).20 However, in clinical research, because there is still a lack of large samples of clinical data for verification, the safety of AFG cannot be determined.
Based on some retrospective studies, most of the conclusions are endorsement of the safety of AFG,21–23 there are also some studies with conflicting conclusions. For example, Petit et al found that the risk of AFG seems to be higher in patients with intraepithelial neoplasia.24 In our study, after an average of 40 months of follow-up, we found that there was no significant difference in tumor recurrence between the two groups. The observed recurrence types included local breast, metastasis of distant lymph node (cervical lymph node, axillary lymph node) and organ, and there was no significant difference in the distribution between the two groups. In addition, no death case was observed in AG; 1 patient in CG group died of tumor recurrence 31 months after surgery. Therefore, there was no statistical difference in all clinicopathological data between the two groups and AFG did not increase the risk of tumor recurrence and metastasis.
Improvement of Breast Appearance
For women, the breast is an organ integrating function and aesthetics, and it is a unique existence among secondary sexual characteristics. Although BCS can reduce the damage to the patient’s breast shape, the postoperative aesthetic outcomes are still unsatisfactory. Most patients will have problems such as nipple and areola asymmetry, partial deformation or bilateral asymmetry. AFG can play a certain role in correcting breast deformities. It can be directly repaired by the physical filling effect of fat, and it can also improve the skin affected by radiotherapy radiation through the fat regeneration effect of ADSC in fat grafts.25 And AFG is more suitable for patients with relatively small breasts for the shape and volume can be better restored. Therefore, the satisfaction and well-being of patients with breasts will be correspondingly improved23 and this was also confirmed in our study by comparing the BREAST-Q score. The comparison of the effects in two groups is shown in Figure 2. At present, there are a variety of aesthetic quantification and evaluation methods, but the expectations of different patients vary greatly. There are also many patients who believe that surviving from cancer is their greatest happiness and in contrast the requirements for aesthetic are not as high as when they are in health. So, the method based on patient self-assessment cannot eliminate the bias caused by subjective factors and there was no exception in this study. This inevitable error may be solved through machine deep learning and artificial intelligence evaluation in the future.
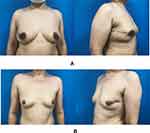 |
Figure 2 Comparison of aesthetic effect. (A) BCS combined with immediate AFG. (B) BCS. Through these two sets of pictures, we could see the advantages of AFG in protecting the appearance of breast. |
Psychological Problems of Breast Cancer Patients
The treatment of breast cancer patients is a good demonstration of the bio-psycho-social medicine model. Breast cancer patients who have undergone surgery suffer from multiple physical or psychological tortures, such as functional impairment, gender incompatibility, and fear of cancer recurrence.26,27 It is well known that poor breast appearance can lead to various psychological problems such as inferiority, anxiety, depression, etc.28,29 But in our study, AFG did not seem to reduce depression and anxiety correspondingly while improving the satisfaction of patients. This may be because the appearance is far less troublesome than the tumor itself such as the fear of cancer recurrence30 especially in the young, advanced tumor stage and low family income groups.31 However, based on the above-mentioned oncologic safety, it is believed that while solving the appearance problems as much as possible, it will also bring more comfort to patients’ mind, thereby alleviating the psychological burden of patients and improving their quality of life, although there may be no statistical difference. At the same time, we also appeal to the society to re-examine breast cancer. The emotional status, quality of life, and social function of breast cancer patients are poor, and their painful experience is significantly higher than that of healthy people.32 In addition, the patient’s work ability was significantly decreased during the treatment period, and the employment rate also decreased, which may be related to the cognitive, memory, and attention-related disorders caused by the comprehensive treatment.33,34 But an individual’s positive attitude towards pursuing life goals, combined with the support of families and all walks of life, can improve the quality of life of patients and even increase their survival rate.25,35 Good health education can help women stay away from the breast cancer problems originally, such as weight control, reducing alcohol consumption and increasing breastfeeding, etc.2 Personalized medical treatments will also bring more benefits to patients.36,37
Complications of AFG
Like other surgical procedures, AFG will also bring complications such as calcification, necrosis, hematoma, infection, etc. Although its incidence is low, and there is generally no need for re-surgical intervention, it may cause confusion of patients in the process of follow-up. Studies have shown an increased probability of biopsy after AFG, which may be due to the occurrence of fat calcification or cysts that make it difficult to distinguish recurrent nodules from breast cancer.38 Consistent with the previous reports, we found that abnormal imaging manifestation in some patients during the follow-up (Figure 3), but we did not perform biopsy to confirm the diagnosis. Because it is not too difficult to distinguish benign from malignant for a experienced radiologist. Therefore, the interference of imaging signs such as calcification and necrosis after AFG on the screening of cancer recurrence can be eliminated by the judgment of professional physicians.39
 |
Figure 3 Molybdenum target mammography. (A) MLO position. (B) CC position. As indicated by the red arrow is annular calcification. |
Limitations
There are some limitations in this study: (1) Breast cancer with different molecular types have differences in disease progression, treatment response, and prognosis. And young breast cancer patients are heterogeneous with elderly patients in etiology and biological manifestations.40 Therefore, we need to conduct special studies on the stratification of more and various breast cancer patients. (2) Technical differences in medical centers may lead to different results, either mastectomy or AFG. So, it is necessary to carry out a similar study with large sample in single center, which is also the focus of our research in the future. (3) We did not make a quantitative comparison of fat absorption rate. Combined with previous studies, the absorption rate of AFG reach the maximum half a year after AFG, which is about 50%. However, after our investigation, only a very small number of patients are willing to undergo AFG again. The reasons include the fear of reoperation, doubts about the effect of AFG, and economic factors. Therefore, in this study we only took into account the short-term effects of AFG in improving appearance. And considering the clinical value of measuring the absorption rate and the cost of patients, we ignored the concern of the absorption rate.
Conclusion
In summary, it was found that BCS combined with immediate AFG can improve the patient’s aesthetic effect on the basis of ensuring oncologic safety. But it was not confirmed by data in alleviating patients’ negative emotions and psychological pressure. Appearance may not be the shortest board of Cannikin Law in patients’ psychological problems. We speculate that in future studies with a larger sample size combined with a focus on psychology, different results may be obtained. At present, AFG has not yet entered the stage of large-scale implementation and more time is needed for research and development. Therefore, it is very important to manage the patients throughout the whole process and even life-long. Moreover, most of the patients receiving AFG are middle-aged women with acceptable tumor staging, so it is feasible and very meaningful to follow up for 10 years or even longer. To sum up, our findings provide evidence support for the promotion of clinical application of AFG and solve many doubts of doctors and patients.
Disclosure
The authors declare that they do not have any commercial, associative, or other conflicts of interest that represent a conflict of interest in connection with the work submitted.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi:10.3322/caac.21660
2. Heer E, Harper A, Escandor N, et al. Global burden and trends in premenopausal and postmenopausal breast cancer: a population-based study. Lancet Glob Health. 2020;8:e1027–e1037. doi:10.1016/S2214-109X(20)30215-1
3. Golubnitschaja O, Liskova A, Koklesova L, et al. Caution, “normal” BMI: health risks associated with potentially masked individual underweight-EPMA position paper 2021. EPMA J. 2021;4:1–22.
4. Allaire BT, Ekwueme DU, Guy GP
5. Allaire BT, Ekwueme DU, Poehler D, et al. Breast cancer treatment costs in younger, privately insured women. Breast Cancer Res Treat. 2017;164:429–436. doi:10.1007/s10549-017-4249-x
6. Maajani K, Jalali A, Alipour S, et al. The global and regional survival rate of women with breast cancer: a systematic review and meta-analysis. Clin Breast Cancer. 2019;19:165–177. doi:10.1016/j.clbc.2019.01.006
7. Montazeri A. Health-related quality of life in breast cancer patients: a bibliographic review of the literature from 1974 to 2007. J Exp Clin Cancer Res. 2008;27:32. doi:10.1186/1756-9966-27-32
8. Hennigs A, Biehl H, Rauch G, et al. Change of patient-reported aesthetic outcome over time and identification of factors characterizing poor aesthetic outcome after breast-conserving therapy: long-term results of a prospective cohort study. Ann Surg Oncol. 2016;23:1744–1751. doi:10.1245/s10434-015-4943-z
9. van Turnhout AA, Fuchs S, Lisabeth-Brone K, et al. Surgical outcome and cosmetic results of autologous fat grafting after breast conserving surgery and radiotherapy for breast cancer: a retrospective cohort study of 222 fat grafting sessions in 109 patients. Aesthetic Plast Surg. 2017;41:1334–1341. doi:10.1007/s00266-017-0946-4
10. Bennett KG, Qi J, Kim HM, et al. Association of fat grafting with patient-reported outcomes in postmastectomy breast reconstruction. JAMA Surg. 2017;152:944–950. doi:10.1001/jamasurg.2017.1716
11. Patel AA, Martin SA, Cheesborough JE, et al. The safety and efficacy of autologous fat grafting during second stage breast reconstruction. J Plast Reconstr Aesthet Surg. 2021;74:792–799. doi:10.1016/j.bjps.2020.10.008
12. Hanson SE, Kapur SK, Garvey PB, et al. Oncologic safety and surveillance of autologous fat grafting following breast conservation therapy. Plast Reconstr Surg. 2020;146:215–225. doi:10.1097/PRS.0000000000006974
13. Tukiama R, Vieira RAC, Facina G, et al. Oncologic safety of autologous fat grafting after breast cancer surgical treatment: a matched cohort study. Plast Reconstr Surg. 2021;148:11–20. doi:10.1097/PRS.0000000000008037
14. Krastev T, van Turnhout A, Vriens E, et al. Long-term follow-up of autologous fat transfer vs conventional breast reconstruction and association with cancer relapse in patients with breast cancer. JAMA Surg. 2019;154:56–63. doi:10.1001/jamasurg.2018.3744
15. Coleman SR. Facial recontouring with lipostructure. Clin Plast Surg. 1997;24:347–367. doi:10.1016/S0094-1298(20)31069-5
16. Shamoun F, Asaad M, Hanson SE. Oncologic safety of autologous fat grafting in breast reconstruction. Clin Breast Cancer. 2021;21:271–277. doi:10.1016/j.clbc.2021.01.020
17. Li J, Han X. Adipocytokines and breast cancer. Curr Probl Cancer. 2018;42:208–214. doi:10.1016/j.currproblcancer.2018.01.004
18. Dirat B, Bochet L, Dabek M, et al. Cancer-associated adipocytes exhibit an activated phenotype and contribute to breast cancer invasion. Cancer Res. 2011;71:2455–2465. doi:10.1158/0008-5472.CAN-10-3323
19. Chandler EM, Seo BR, Califano JP, et al. Implanted adipose progenitor cells as physicochemical regulators of breast cancer. Proc Natl Acad Sci USA. 2012;109:9786–9791. doi:10.1073/pnas.1121160109
20. Choi J, Cha YJ, Koo JS. Adipocyte biology in breast cancer: from silent bystander to active facilitator. Prog Lipid Res. 2018;69:11–20. doi:10.1016/j.plipres.2017.11.002
21. Petit JY, Maisonneuve P, Rotmensz N, et al. Fat grafting after invasive breast cancer: a matched case-control study. Plast Reconstr Surg. 2017;139:1292–1296. doi:10.1097/PRS.0000000000003339
22. Stumpf CC, Zucatto AE, Cavalheiro JAC, et al. Oncologic safety of immediate autologous fat grafting for reconstruction in breast-conserving surgery. Breast Cancer Res Treat. 2020;180:301–309. doi:10.1007/s10549-020-05554-0
23. Cohen O, Lam G, Karp N, et al. Determining the oncologic safety of autologous fat grafting as a reconstructive modality: an institutional review of breast cancer recurrence rates and surgical outcomes. Plast Reconstr Surg. 2017;140:382e–392e. doi:10.1097/PRS.0000000000003576
24. Petit JY, Rietjens M, Botteri E, et al. Evaluation of fat grafting safety in patients with intraepithelial neoplasia: a matched-cohort study. Ann Oncol. 2013;24:1479–1484. doi:10.1093/annonc/mds660
25. Pinquart M, Duberstein PR. Associations of social networks with cancer mortality: a meta-analysis. Crit Rev Oncol Hematol. 2010;75:122–137. doi:10.1016/j.critrevonc.2009.06.003
26. Koch L, Bertram H, Eberle A, et al. Fear of recurrence in long-term breast cancer survivors-still an issue. Results on prevalence, determinants, and the association with quality of life and depression from the cancer survivorship–a multi-regional population-based study. Psychooncology. 2014;23:547–554. doi:10.1002/pon.3452
27. Williams F, Jeanetta SC. Lived experiences of breast cancer survivors after diagnosis, treatment and beyond: qualitative study. Health Expect. 2016;19:631–642. doi:10.1111/hex.12372
28. Avis NE, Levine B, Naughton MJ, et al. Explaining age-related differences in depression following breast cancer diagnosis and treatment. Breast Cancer Res Treat. 2012;136:581–591. doi:10.1007/s10549-012-2277-0
29. Howard-Anderson J, Ganz PA, Bower JE, et al. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104:386–405. doi:10.1093/jnci/djr541
30. Nahm SH, Blinman P, Butler S, et al. Factors associated with fear of cancer recurrence in breast and colorectal cancer survivors: a cross-sectional study of cancer survivors. Asia Pac J Clin Oncol. 2021;17:222–229. doi:10.1111/ajco.13434
31. Ohns SA, Stutz PV, Talib TL, et al. Acceptance and commitment therapy for breast cancer survivors with fear of cancer recurrence: a 3-arm pilot randomized controlled trial. Cancer. 2020;126:211–218. doi:10.1002/cncr.32518
32. Finck C, Barradas S, Zenger M, et al. Quality of life in breast cancer patients: associations with optimism and social support. Int J Clin Health Psychol. 2018;18:27–34. doi:10.1016/j.ijchp.2017.11.002
33. Lewis J, Mackenzie L, Black D. Workforce participation of Australian women with breast cancer. Psychooncology. 2020;29:1156–1164. doi:10.1002/pon.5392
34. Gregorowitsch ML, van den Bongard H, Couwenberg AM, et al. Self-reported work ability in breast cancer survivors; a prospective cohort study in the Netherlands. Breast. 2019;48:45–53. doi:10.1016/j.breast.2019.08.004
35. Teques AP, Carrera GB, Ribeiro JP, et al. The importance of emotional intelligence and meaning in life in psycho-oncology. Psychooncology. 2016;25:324–331. doi:10.1002/pon.3921
36. Bizzarri M, Fedeli V, Monti N, et al. Personalization of medical treatments in oncology: time for rethinking the disease concept to improve individual outcomes. EPMA J. 2021;56:1–14.
37. Bertele N, Karabatsiakis A, Buss C, et al. How biomarker patterns can be utilized to identify individuals with a high disease burden: a bioinformatics approach towards predictive, preventive, and personalized (3P) medicine. EPMA J. 2021;12:507–516. doi:10.1007/s13167-021-00255-0
38. Kling RE, Mehrara BJ, Pusic AL, et al. Trends in autologous fat grafting to the breast: a national survey of the American society of plastic surgeons. Plast Reconstr Surg. 2013;132:35–46. doi:10.1097/PRS.0b013e318290fad1
39. Groen JW, Negenborn VL, Twisk D, et al. Autologous fat grafting in onco-plastic breast reconstruction: a systematic review on oncological and radiological safety, complications, volume retention and patient/surgeon satisfaction. J Plast Reconstr Aesthet Surg. 2016;69:742–764. doi:10.1016/j.bjps.2016.03.019
40. Chollet-Hinton L, Anders CK, Tse CK, et al. Breast cancer biologic and etiologic heterogeneity by young age and menopausal status in the Carolina Breast Cancer Study: a case-control study. Breast Cancer Res. 2016;18:79. doi:10.1186/s13058-016-0736-y
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
