Back to Journals » Clinical Interventions in Aging » Volume 13
Effects of age on effect-site concentration of remifentanil for suppressing anesthetic emergence cough in male patients undergoing laparoscopic cholecystectomy
Authors Kim HY, Lee SY, Kang S, Kim B, Moon YR , Kim JE
Received 23 February 2018
Accepted for publication 18 April 2018
Published 30 May 2018 Volume 2018:13 Pages 1053—1060
DOI https://doi.org/10.2147/CIA.S166423
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Ha Yeon Kim,1 Sook Young Lee,1 Seyoon Kang,1 Bora Kim,1 Yeo Rae Moon,2 Ji Eun Kim1
1Department of Anesthesiology and Pain Medicine, Ajou University School of Medicine, Suwon, Republic of Korea; 2Department of Biostatistics, Ajou University School of Medicine, Suwon, Republic of Korea
Background: Remifentanil infusion during emergence lowers cough. Effect-site concentration (Ce) of remifentanil using target-controlled infusion (TCI) has been evaluated in previous studies. Recent studies revealed the existence of sex-related differences in remifentanil Ce in young and elderly patients. Thus, there was the need to re-evaluate the effect of age in single sex. We investigated the remifentanil Ce for suppressing emergence cough in young and elderly male patients and evaluated the age-related differences.
Patients and methods: In total, 25 young (ages between 20 and 50 years) and 24 elderly (ages between 65 and 75 years) male patients undergoing laparoscopic cholecystectomy were enrolled. Anesthesia was implemented with remifentanil using TCI and sevoflurane. The remifentanil Ce for suppressing emergence cough was estimated for each group using Dixon’s up-and-down method and isotonic regression method with a bootstrapping approach.
Results: The remifentanil Ce for suppressing emergence cough in 50% (EC50) and 95% (EC95) of the patients was comparable between the young and elderly patients. Isotonic regression demonstrated that the EC50 (83% confidence interval [CI]) of remifentanil was 2.56 (2.39−2.75) ng/mL in the young patients and 2.15 (1.92−2.5) ng/mL in the elderly patients. The EC95 (95% CI) of remifentanil was 3.33 (2.94−3.46) ng/mL in the young patients and 3.41 (3.18−3.48) ng/mL in the elderly patients. Dixon’s up-and-down method also demonstrated that the EC50 was comparable between the two groups (2.69±0.32 ng/mL vs 2.39±0.38 ng/mL, P=0.132).
Conclusion: The remifentanil Ce for suppressing emergence cough following extubation during general anesthesia was comparable between young and elderly male patients. It indicates that age-related differences in remifentanil requirement for suppressing emergence cough did not exist in male sex.
Keywords: age difference, cough, extubation, male patients, remifentanil
Introduction
Cough has been an important issue during the perioperative period. Cough during emergence from general anesthesia is caused by anesthetic gas, secretion, or primarily stimulation from the endotracheal tube.1 Coughing that follows extubation on emergence may lead to a number of potentially dangerous effects, including laryngospasm, increased intraocular and intracranial pressures, wound disruption, and detrimental hemodynamic changes such as tachycardia, myocardial ischemia, and arrhythmia.
The infusion of opioids during emergence may provide a smooth emergence by reducing coughing, agitation, and deleterious hemodynamic changes.2 However, opioids can also lead to the depression of ventilation and delayed awakening. Remifentanil, as an ultrashort-acting opioid, has been recommended to supplement the emergence process due to its short half time and easy controllability.3 Remifentanil provides a rapid awakening from anesthesia even after a prolonged infusion during surgery, and its cough suppression enables smooth extubation alongside less complications.4,5 Furthermore, it is affected minimally by the excessive age or hepatic or renal dysfunction. Since a low-dose manually controlled infusion of remifentanil was reported to reduce the emergence cough,6 target-controlled infusion (TCI) was introduced to reach a defined target concentration without a rapid change in drug levels or an increase beyond the intended range.7
A number of studies have determined the optimal effect-site concentration (Ce) of remifentanil for suppressing emergence cough following extubation.8–17 However, the optimal remifentanil Ce for suppressing emergence cough can vary according to the characteristics of anesthesia and surgery. In addition, the effect of opioid shows differences both in quality and quantity according to age and sex.18,19 In 2014, the existence of sex-related differences regarding the remifentanil Ce for emergence cough suppression was demonstrated in young patients (ages 20–46 years).15 In 2018, it was revealed in elderly patients (ages 60–75 years).17 Recently, Yoo et al reported no difference between adult patients (ages 20–60 years) and elderly patients (ages 65–80 years) in the remifentanil Ce for suppressing emergence cough.16 However, they did not consider the sex-related differences of opioid and enrolled both male and female subjects.16
The purpose of this study was to compare the emergence cough in 50% (EC50) and 95% (EC95) of remifentanil in effect-site TCI for suppressing emergence cough following extubation in young male patients and elderly male patients and to evaluate the existence of age-related differences. We hypothesized that young male patients may require a higher concentration of remifentanil for preventing cough during anesthetic emergence than elderly male patients.
Patients and methods
Patients
After approval by the Ajou University Hospital Institutional Review Board (protocol number: AJIRB-MED-OBS-16-146, 1st June 2016) and registration at http://cris.nih.go.kr (registration number: KCT0002353), data were collected from June 2016 to December 2017. Twenty-five young male patients (ages between 20 and 50 years) and 24 elderly male patients (ages between 65 and 75 years) with an American Society of Anesthesiologists (ASA) physical status I–II, who were scheduled for laparoscopic cholecystectomy, were enrolled in this study. Patients were excluded if the following criteria were present; recent upper respiratory infection, history of difficult intubation, Mallampati class 3 or 4, uncontrolled hypertension and diabetes mellitus, current smoker, coronary artery disease, and a body mass index of more than 30 kg/m2. Written informed consent was acquired from all patients.
Anesthesia
None of the patients were administered any pre-medication. Upon arrival at the operating room, monitoring such as electrocardiography, pulse oximetry, automatic noninvasive arterial pressure measurement, end-tidal carbon dioxide (EtCO2), and bispectral index (BIS™ Quatro Sensor; Covidien, Boulder, CO, USA) were performed. Anesthesia was induced with 1.5–2.5 mg/kg of intravenous (IV) propofol and 1–5 ng/mL target concentration of remifentanil (Ultiva; GlaxoSmithKline, Brentford, UK) using TCI, via a commercial anesthesia infusion pump (Orchestra® Base Primea; Fresenius Vial, Brezins, France) based on Minto’s pharmacokinetic model.20 After consciousness loss, 0.8 mg/kg of IV rocuronium was administered. Oral tracheal intubation was conducted using a tracheal tube with an internal diameter of 7.5 mm. Cuff pressure was adjusted to 20–25 mmHg using a hand pressure gauge.
Anesthesia was maintained with a sevoflurane vol% of 1.5–2.5 and a remifentanil Ce of 1–5 ng/mL in order to target a BIS value of 40–55 and heart rate (HR) and mean arterial pressure (MAP) that were within 20% of baseline. Rocuronium was continuously infused to maintain 1 or 2 of train-of-four count using nerve stimulator. Ventilation was maintained mechanically with an air/oxygen mixture of FiO2 0.5 and 3 L/min gas flow, targeting EtCO2 at 35–40 mmHg.
Approximately 15 minutes prior to the end of surgery, sevoflurane was modulated to a BIS level of approximately 60, and the remifentanil Ce was set at the pre-determined Ce. At the end of surgery, sevoflurane was stopped, and fresh gas flow was changed to 5 L/min. After confirming the train-of-four count >2, 3 mg/kg of IV Bridion® (sugammadex) was administered to reverse a neuromuscular block, which was re-checked as more than 90% response of train-of-four ratio. Thirty mg of IV ketorolac and 0.3 mg of ramosetron were administered for postoperative analgesics and antiemetics. Mechanical ventilation was then switched to manual ventilation while maintaining EtCO2 of 35–40 mmHg. After the patients opened the eyes, and the spontaneous ventilation with an adequate respiratory frequency and tidal volume was confirmed, the trachea was extubated. Immediately after extubation, remifentanil infusion was stopped and 100% oxygen was supplied by a facemask. After observation for 5 minutes, patients were transferred to the post-anesthesia care unit (PACU).
Measurements
Remifentanil Ce was measured by up-and-down sequential allocation design. The initial Ce of remifentanil was 2 ng/mL for the first patient of each group; and the pre-determined Ce of the next patient was determined by the cough response of the previous patient. If the patient did not cough during emergence, the extubation was defined as smooth extubation (success), and the pre-determined concentration for the next patient was reduced by 0.5 ng/mL. If the patient coughed anytime, it was considered as failed smooth extubation (failure), and the pre-determined Ce was increased by 0.5 ng/mL.
Hemodynamic data, which include HR and MAP, during perioperative period were recorded at 5 time points – before induction, at the end of operation, before, immediately after, and 3 minutes after extubation. In all, 0.5 mg of IV atropine and 4 mg ephedrine were administered for bradycardia of HR <40 beats/min and hypotension of MAP <60 mmHg. Cough was defined as the strong and sudden cough developed during 5 minutes after extubation. The time to extubation was defined as the time from discontinuing sevoflurane until extubation. The sevoflurane concentration at eye opening was recorded. Complications including bradypnea of respiratory rate <8 bpm, laryngospasm, and desaturation of SpO2 below 95% despite oxygen supplementation were recorded. The sedation and overall pain scores were assessed for each patient upon arrival at the PACU. In the PACU, sedation was scored using the Ramsay Sedation Scale (six levels; 1, Anxious and agitated or restless or both; 6, No response to a light glabellar tap or loud auditory stimulus), and pain was scored by an 11-point numerical rating scale (NRS; 0, no pain; 10, worst pain). In all, 0.5 μg/kg of IV fentanyl was given for an NRS score of 5 or greater.
Statistics
For estimating EC50 and EC95 of remifentanil, which were the primary outcomes, Dixon’s up-and-down method and isotonic regression method were used. Referring previous study,17 EC50 by the Dixon’s up-and-down method needs at least 6 pairs of success-failure and at least 20 patients to get stable estimates.21 In this study, 25 young and 24 elderly patients in each group were enrolled based on Dixon’s method. The EC50 of remifentanil was defined as the mean at the mid-point of the crossover concentration for each group (ie, success-failure). They were compared using independent t-tests. The remifentanil Ce also was analyzed by isotonic regression method using a pooled-adjacent-violators algorithm in order to interpolate the EC50 (83%) and the EC95 (95%) of remifentanil alongside the confidence intervals (CIs). The CI was calculated through a bootstrapping approach.21 If the EC50 and EC95 estimates did not overlap at the 83% CI and 95% CI, each, the hypothesis was rejected at an α-value of 0.05.21,22
Among the secondary outcomes, categorical variables were analyzed using the chi-squared test or Fisher’s exact test. Continuous variables were tested for normality using Kolmogorov-Smirnov test. Then, the variables showing normality were analyzed using Student’s t-test and the variables not showing normality were analyzed using Mann-Whitney test. The repeated measured variables were analyzed using a linear mixed model.
Data were presented as mean ± standard deviation (SD), median (range), or number. Statistical significance was defined as a P-value of less than 0.05. The SPSS package (version 23.0, IBM Corporation, Armonk, NY, USA) including R (version 3.2.5, The R foundation for Statistical Computing; https://www.r-project.org) was used for statistical analyses.
Results
A total of 50 patients were enrolled, but 1 patient was eliminated from the data collection due to an incorrect pre-determined Ce of remifentanil (Figure 1). Ultimately, 25 young and 24 elderly male patients completed the study. Patient and operative characteristics are presented in Table 1. The mean age of the young patients was lower than that of the elderly patients (39±7 vs 70±4 years). Because of the age-related difference, height and weight were significantly higher among the young patients; however, the body mass index was not significantly different.
  | Figure 1 Consort flow diagram. |
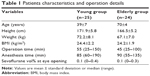  | Table 1 Patients characteristics and operation details |
The sequence of smooth emergence (success) and failed smooth emergence (failure) is provided in Figure 2, and the isotonic regression curve of the probability of no cough is displayed in Figure 3. The EC50 and EC95 values of the remifentanil Ce for abolishing cough during emergence calculated by Dixon’s method or isotonic regression are shown in Table 2. By Dixon’s method, the EC50 of remifentanil Ce was comparable as 2.69±0.32 ng/mL in the young patients and 2.39±0.38 ng/mL in the elderly patients (P=0.132). By isotonic regression, the EC50 of remifentanil Ce was 2.56 (83% CI, 2.39-2.75) ng/mL in the young patients and 2.15 (83% CI, 1.92-2.50) ng/mL in the elderly patients. The EC95 of remifentanil Ce was 3.33 (95% CI, 2.94-3.46) ng/mL in the young patients and 3.41 (95% CI, 3.18-3.48) ng/mL in the elderly patients. Since both EC50 and EC95 values overlapped at the each CI level, the Ce of remifentanil for suppressing cough during emergence was comparable between the two groups.
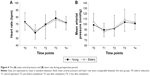
The emergence and recovery outcomes are shown in Table 3. During anesthetic emergence, bradypnea occurred in 1 young patient with 3 ng/mL of remifentanil Ce and in 2 elderly patients with 2 ng/mL and 3 ng/mL of remifentanil Ce. As shown in Figure 4, the MAP and HR were comparable between the two groups throughout perioperative period.
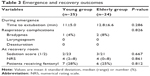  | Table 3 Emergence and recovery outcomes |
Discussion
This study demonstrated that the required concentration of remifentanil for suppressing emergence cough associated with extubation is comparable between young and elderly male patients. The EC50 values of remifentanil Ce for suppressing emergence cough following extubation were 2.56 ng/mL in the young male patients and 2.25 ng/mL in the elderly male patients.
The cough reflex is associated with opioid action.23 Opioids block the peripheral C-fiber as a nociceptor to reduce the amount of coughing, and act at the brain stem to reduce a reflexive cough.23 Remifentanil, as an opioid most commonly used for anesthesia,24 is known to lead to faster recovery and lower respiratory depression than other short-acting opioids.25 Since a low-dose infusion of remifentanil, compared to a bolus dose, reduced the emergence cough from general anesthesia,6,26 remifentanil infusion with the use of TCI demonstrated reduced incidence and severity of anesthetic emergence cough.9–11,14 The optimal Ce of remifentanil for suppressing emergence cough was evaluated in various anesthetic conditions.8,13,16 However, a great part of these studies has overlooked sex- or age-related differences when using opioid.
A literature in 2016 revealed that age-related difference did not appear in the remifentanil Ce for suppressing emergence cough.16 However, the sex-related differences were not considered and both sexes were enrolled simultaneously. The existence of sex-related differences regarding the remifentanil Ce for suppressing emergence cough were determined both in young and elderly patients.15,17 Therefore, there was a need to confirm the effect of age on the remifentanil concentration for suppressing emergence cough when being investigated in single male sex. Consequently, in this study, age did not affect the remifentanil requirement for smooth extubation during emergence and age-related differences in male patients were confirmed not to exist.
Effect of aging on cough reflex remains controversial.27–31 Cough reflexes to inhaled ammonia or distilled water gas were reduced in elderly subjects compared to younger subjects.27,28 On the other hand, the cough reflex threshold to citric acid was not reduced with advanced aging.29 Recently, in human brain imaging, the cortex was revealed to have a primarily critical role in controlling cough,32 which the sensory cortex becomes prone to aging; motor cortex is relatively resistant to aging.30 In 2011, Ebihara et al investigated the effect of aging on the cognitive aspect of cough reflex,31 wherein the elderly had a reduced cognition to urge-to-cough compared with the younger, but the cough reflex threshold was similar in both. It means that the sensory regions are degenerated by aging, and the net performance of the cough reflex is compensated in the elderly.31
Effect of aging on the pharmacokinetics of opioids also remains controversial. A simulation study demonstrated that elimination half-time, volume distribution and clearance were significantly higher in the elderly, which suggested that the time required for a decrease in remifentanil Ce would be more variable in the elderly.33 In a pharmacodynamic research by Xu et al, there was no age-related difference in 405 Chinese patients who were less than 65 years old.34 In a research by Yang et al, the remifentanil Ce required at loss of response for a standard noxious painful stimulus was similar between the younger and the elderly.35 These findings are consistent with the results of this study, where the young male patients needed similar concentration of remifentanil for suppressing emergence cough compared with the elderly male patients (2.56 and 2.15 ng/mL in young and elderly patients, respectively).
The main result of this study is the disappearance of age-related difference in male patients. Several possibilities may explain this. First, a factor affecting pharmacokinetics with increased age is the reduction in the volumes of distribution for drugs. It results from the changes of body composition following age; for example, a decrease in water content or an increase in fat content, and alterations in terms of protein binding.36 In general, these changes lead to higher initial plasma levels after opioid administration. However, considering a previous study, in which age-related increases in maximum plasma concentrations were shown not for a single dose but only after multiple repeat doses,37 remifentanil seems to be closer to single dosing administration despite infusion in the elderly patients, due to no in vivo accumulative characteristics and short context sensitive half-time (approximately 3 min). Second, although the relationship between perioperative pain and aging remains controversial,36 a study of approximately 500 cancer patients found that the elderly had similar pain levels to the younger.38 The elderly tended to choose lower pain scores and request less opioid analgesia compared to the younger.39 Moreover, the sensitivity to mechanical pain increased with age, mostly for men.40 The densities of opioid receptor decrease with aging, but the affinity between opioid and opioid receptor increases with aging, although the final effects regarding opioid analgesia is controversial yet.36 Third, TCI for remifentanil infusion was performed using the Minto model, which accounts for some co-variables such as height, weight, and age.33 Minto et al identified age as an influencing factor on the pharmacokinetics of remifentanil, postulating that this results from a reduction of central volume of distribution in the elderly.20
There are some limitations. First, because the in-room outcome assessor was not blinded to pre-determined remifentanil Ce, the in-room outcome measurement might have been biased. Second, biological aging often does not correlate with actual age. It results in considerable physiological, pharmacodynamic, and pharmacokinetic differences, which may contribute to large variations in responses. Third, only patients with an ASA physical status I–II were chosen as part of the elderly group; thus, results may be limited in generalizability for patients with poor ASA status due to coexisting diseases. Fourth, females differ from males in basal pain perception or opioid sensitivity, and the gonadal hormone influences the opioid sensitivity. The results may have a possibility to change if females were enrolled. Finally, although the remifentanil Ce for abolishing emergence cough did not show significant difference, there was the tendency of higher remifentanil concentration in young patients, and the results may be altered when a large volume study is performed.
Conclusion
The Ce of remifentanil for suppressing emergence cough following extubation from general anesthesia was comparable between young and elderly male patients, which indicates no existence of age-related differences in the Ce of remifentanil. Therefore, the clinicians do not need to consider age when adjusting the Ce of remifentanil to suppress anesthetic emergence cough in male patients.
Disclosure
The authors report no conflicts of interest in this work.
References
Kim ES, Bishop MJ. Cough during emergence from isoflurane anesthesia. Anesth Analg. 1998;87(5):1170–1174. | ||
Tagaito Y, Isono S, Nishino T. Upper airway reflexes during a combination of propofol and fentanyl anesthesia. Anesthesiology. 1998;88(6):1459–1466. | ||
Beers R, Camporesi E. Remifentanil update: clinical science and utility. CNS Drugs. 2004;18(15):1085–1104. | ||
Twersky RS, Jamerson B, Warner DS, Fleisher LA, Hogue S. Hemodynamics and emergence profile of remifentanil versus fentanyl prospectively compared in a large population of surgical patients. J Clin Anesth. 2001;13(6):407–416. | ||
Mandel JE. Considerations for the use of short-acting opioids in general anesthesia. J Clin Anesth. 2014;26(1 Suppl):S1–S7. | ||
Aouad MT, Al-Alami AA, Nasr VG, Souki FG, Zbeidy RA, Siddik-Sayyid SM. The effect of low-dose remifentanil on responses to the endotracheal tube during emergence from general anesthesia. Anesth Analg. 2009;108(4):1157–1160. | ||
Albrecht S, Hering W, Schuttler J, Schwilden H. [New intravenous anesthetics. Remifentanil, S(+)-ketamine, eltanolone and target controlled infusion]. Anaesthesist. 1996;45(12):1129–1141. German [with English abstract]. | ||
Lee B, Lee JR, Na S. Targeting smooth emergence: the effect site concentration of remifentanil for preventing cough during emergence during propofol-remifentanil anaesthesia for thyroid surgery. Br J Anaesth. 2009;102(6):775–778. | ||
Chen J, Li W, Wang D, Hu X. The effect of remifentanil on cough suppression after endoscopic sinus surgery: a randomized study. Acta Anaesthesiol Scand. 2010;54(10):1197–1203. | ||
Jun NH, Lee JW, Song JW, Koh JC, Park WS, Shim YH. Optimal effect-site concentration of remifentanil for preventing cough during emergence from sevoflurane-remifentanil anaesthesia. Anaesthesia. 2010;65(9):930–935. | ||
Lim JH, Ryu SJ, Lim YS. The incidence of cough induced by remifentanil during anesthetic induction was decreased by graded escalation of the remifentanil concentration. Korean J Anesthesiol. 2010;58(2):117–121. | ||
Choi EM, Park WK, Choi SH, Soh S, Lee JR. Smooth emergence in men undergoing nasal surgery: the effect site concentration of remifentanil for preventing cough after sevoflurane-balanced anaesthesia. Acta Anaesthesiol Scand. 2012;56(4):498–503. | ||
Cho HB, Kim JY, Kim DH, Kim DW, Chae YJ. Comparison of the optimal effect-site concentrations of remifentanil for preventing cough during emergence from desflurane or sevoflurane anaesthesia. J Int Med Res. 2012;40(1):174–183. | ||
Chang CH, Lee JW, Choi JR, Shim YH. Effect-site concentration of remifentanil to prevent cough after laryngomicrosurgery. Laryngoscope. 2013;123(12):3105–3109. | ||
Soh S, Park WK, Kang SW, Lee BR, Lee JR. Sex differences in remifentanil requirements for preventing cough during anesthetic emergence. Yonsei Med J. 2014;55(3):807–814. | ||
Yoo JY, Kim JY, Kwak HJ, et al. Effect-site concentration of remifentanil for preventing cough during emergence in elderly patients undergoing nasal surgery: a comparison with adult patients. Clin Interv Aging. 2016;11:1247–1252. | ||
Lee SY, Jeong YY, Lee BH, Kim JE. Sex-related differences in effect-site concentration of remifentanil for preventing anesthetic emergence cough in elderly patients. Clin Interv Aging. 2018;13:81–89. | ||
Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL 3rd. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009;10(5):447–485. | ||
Niesters M, Dahan A, Kest B, et al. Do sex differences exist in opioid analgesia? A systematic review and meta-analysis of human experimental and clinical studies. Pain. 2010;151(1):61–68. | ||
Minto CF, Schnider TW, Egan TD, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997;86(1):10–23. | ||
Pace NL, Stylianou MP. Advances in and limitations of up-and-down methodology: a precis of clinical use, study design, and dose estimation in anesthesia research. Anesthesiology. 2007;107(1):144–152. | ||
Payton ME, Greenstone MH, Schenker N. Overlapping confidence intervals or standard error intervals: what do they mean in terms of statistical significance? J Insect Sci. 2003;3:34. | ||
Canning BJ, Chang AB, Bolser DC, Smith JA, Mazzone SB, McGarvey L; CHEST Expert Cough Panel. Anatomy and neurophysiology of cough: CHEST Guideline and Expert Panel report. Chest. 2014;146(6):1633–1648. | ||
Cho S, Han JI, Baik HJ, Kim DY, Chun EH. Monitored anesthesia care for great saphenous vein stripping surgery with target controlled infusion of propofol and remifentanil: a prospective study. Korean J Anesthesiol. 2016;69(2):155–160. | ||
Komatsu R, Turan AM, Orhan-Sungur M, McGuire J, Radke OC, Apfel CC. Remifentanil for general anaesthesia: a systematic review. Anaesthesia. 2007;62(12):1266–1280. | ||
Shajar MA, Thompson JP, Hall AP, Leslie NA, Fox AJ. Effect of a remifentanil bolus dose on the cardiovascular response to emergence from anaesthesia and tracheal extubation. Br J Anaesth. 1999;83(4):654–656. | ||
Pontoppidan H, Beecher HK. Progressive loss of protective reflexes in the airway with the advance of age. JAMA. 1960;174:2209–2213. | ||
Newnham DM, Hamilton SJ. Sensitivity of the cough reflex in young and elderly subjects. Age Ageing. 1997;26(3):185–188. | ||
Katsumata U, Sekizawa K, Ebihara T, Sasaki H. Aging effects on cough reflex. Chest. 1995;107(1):290–291. | ||
Ebihara S, Ebihara T, Kohzuki M. Effect of aging on cough and swallowing reflexes: implications for preventing aspiration pneumonia. Lung. 2012;190(1):29–33. | ||
Ebihara S, Ebihara T, Kanezaki M, et al. Aging deteriorated perception of urge-to-cough without changing cough reflex threshold to citric acid in female never-smokers. Cough. 2011;7(1):3. | ||
Widdicombe J, Eccles R, Fontana G. Supramedullary influences on cough. Respir Physiol Neurobiol. 2006;152(3):320–328. | ||
Minto CF, Schnider TW, Shafer SL. Pharmacokinetics and pharmacodynamics of remifentanil. II. Model application. Anesthesiology. 1997;86(1):24–33. | ||
Xu Z, Liu F, Yue Y, et al. The effect of gender and age on bispectral index and effective concentration 50 for propofol-remifentanil target-controlled infusion at two clinical end-points – a multi-center clinical research. Int J Anesth Resusc. 2006;27:144–148. | ||
Yang N, Zuo MZ, Yue Y, Wang Y, Shi Y, Zhang XN. Comparison of C50 for propofol-remifentanil target-controlled infusion and bispectral index at loss of consciousness and response to painful stimulus in elderly and young patients. Chin Med J (Engl). 2015;128(15):1994–1999. | ||
Wilder-Smith OH. Opioid use in the elderly. Eur J Pain. 2005;9(2):137–140. | ||
Davies KN, Castleden CM, McBurney A, Jagger C. The effect of ageing on the pharmacokinetics of dihydrocodeine. Eur J Clin Pharmacol. 1989;37(4):375–379. | ||
Loick G, Radbruch L, Sabatowski R, Siessegger M, Grond S, Lehmann KA. [Morphine dose and side effects: a comparison of older and younger patients with tumor pain]. Dtsch Med Wochenschr. 2000;125(41):1216–1221. German [with English abstract]. | ||
Gagliese L, Weizblit N, Ellis W, Chan VW. The measurement of postoperative pain: a comparison of intensity scales in younger and older surgical patients. Pain. 2005;117(3):412–420. | ||
Pickering G, Jourdan D, Eschalier A, Dubray C. Impact of age, gender and cognitive functioning on pain perception. Gerontology. 2002;48(2):112–118. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.