Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 11
Effects of ABCB1 rs1045642 polymorphisms on the efficacy and safety of amlodipine therapy in Caucasian patients with stage I–II hypertension
Authors Sychev D, Shikh N, Morozova T, Grishina E, Ryzhikova K, Malova E
Received 29 November 2017
Accepted for publication 10 July 2018
Published 20 September 2018 Volume 2018:11 Pages 157—165
DOI https://doi.org/10.2147/PGPM.S158401
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Dmitry Sychev,1 Nadezhda Shikh,2 Tatiana Morozova,2 Elena Grishina,3 Kristina Ryzhikova,3 Elena Malova1
1Department of Clinical Pharmacology and Therapy, Russian Medical Academy of Continuous Professional Education, Ministry of Healthcare, Moscow, Russia; 2Department of Clinical Pharmacology and Pharmacotherapy, Institute of Professional Education, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia, Moscow, Russia; 3Research Center, Russian Medical Academy of Continuous Professional Education, Ministry of Healthcare, Moscow, Russia
Purpose: The aim of this study was to determine the impact of ABCB1 (MDR1) rs1045642 polymorphisms on the efficacy and safety of amlodipine in Caucasian patients.
Patients and methods: The 12-week study included 100 patients. Patients with the newly diagnosed stage I–II hypertension (HT) were recruited to complete genotyping of the rs1045642 single-nucleotide polymorphism (SNP). The study design did not include a control group. Before treatment, all patients either did not undergo antihypertensive treatment at all or did not receive regular antihypertensive therapy. The initial dose was 5 mg/day. Four office blood pressure measurements, two 24-hour noninvasive ambulatory blood pressure measurements, and questionnaires of Tsvetov were used to evaluate the efficacy and safety of amlodipine.
Results and conclusion: The highest antihypertensive effect in combination with the lowest incidence of adverse reactions was observed in the TT group, while patients with the CC genotype showed a low antihypertensive effect and the highest incidence of adverse effects. Patients with the CC genotype presented with adverse effects predominantly in the form of edema. A total of 33 patients reached the target blood pressure (SBP <140 mmHg; DBP <90 mmHg): two patients with the CC genotype (12%); 18 patients with the CT genotype (34%); and 13 patients with the TT genotype (43%). The intergroup differences were: CC vs CT, P=0.02; CC vs TT, P=0.02; and CT vs TT, P=0.05. The results of this study indicate the potential of pharmacogenetic testing for rs1045642 SNP when prescribing amlodipine for the first time in Caucasian patients with stage I–II arterial HT.
Keywords: pharmacodynamics, rs1045642, personalized, side effects, CYP3A5, single-nucleotide polymorphism, SNP, P-glycoprotein
Introduction
Arterial HT is one of the risk factors for cardiovascular disease and its complications. Currently, the drugs of choice for the long-term management of HT are diuretics, beta-blockers, angiotensin receptor blockers II, angiotensin-converting enzyme inhibitors, and calcium antagonists (CCBs).1–3 Despite the wide range of innovative drugs with high antihypertensive efficacy, organoprotective properties, and an influence on cardiovascular prognosis, BP control often remains insufficient. Every year, the number of people with uncontrolled BP rises.4
Calcium antagonists are one of the most commonly prescribed drug classes for a variety of cardiovascular disorders and are widely used in Russia.5 Two chemical groups of calcium antagonists are used in the clinical setting: non-dihydropyridines (verapamil, diltiazem) and dihydropyridines (amlodipine). Over the past 10 years, amlodipine has been included in the list of vital and essential medicines (Decree of the Russian Federation from December 29, 2005, 2343 pp.).
It is now well established from a variety of studies, such as the ALLHAT,6 VALUE,7 and ACCOMPLISH trials,8 that amlodipine is highly effective. While antihypertensive efficacy is high, the possible adverse effects of amlodipine are also well known. Approximately 20% of patients stop taking amlodipine because of its adverse effects. The most common are ankle and tibial edema. In some cases, because of vasodilation, the hands may also become swollen.9 Dihydropyridine CCBs produce other adverse reactions such as redness of the face and upper extremities, which are related to systemic vasodilation.10
The reasons for inadequate control of HT and the development of adverse effects vary. Age, comorbidities and polypharmacy play a significant role. There is a growing body of literature that recognizes the genetic characteristics of patients among the important factors determining differences in drug response. Genetic factors can account for up to 50% of patient variability.11
Much uncertainty still exists about the relationship between the safety of amlodipine therapy and ethnic differences in drug response. To the best of our knowledge, very few studies have addressed the issue of amlodipine pharmacogenetics and they have not identified any convincing correlations.
P-gp-mediated transcellular transport is of great importance in the metabolism of amlodipine.13 The P-gp drug efflux pump, encoded by the gene ABCB1 (MDR1), is the most widely studied component in multidrug resistance. An SNP has been identified within ABCB1, rs1045642 (C3435T), which may alter P-gp substrate specificity and have an impact on the effectiveness of treatment.14
Pharmacogenetic testing may enable physicians to understand why patients react differently to various drugs and to make better decisions about therapy. Ultimately, this understanding may shift the medical paradigm to highly individualized therapeutic regimens.15,16
Goals
This study aimed to evaluate the effects of ABCB1 rs1045642 polymorphisms on the efficacy and safety of amlodipine therapy in Caucasian patients with stage I–II HT.
Materials and methods
The Ethics Committee of the Sechenov First Moscow State Medical University, Moscow, Russia, approved the study (Act. No. 02-15 from February 18, 2015). Written informed consent was obtained from all subjects.
This open uncontrolled 12-week study included 100 patients. Each patient was required to make four visits during the study: one pretreatment visit and follow-up visits at 2, 4, and 12 weeks of treatment. Only Caucasian patients were included in the study.
We assessed the clinical safety and effectiveness of treatment using OBPM, 24-hour noninvasive ABPM, electrocardiograms, and common clinical methods (analysis of complaints; obtaining medical history including HT duration; risk factors; comorbidities; physical examination; anthropometric measurements; lung, heart, and major blood vessel auscultation; an assessment of peripheral pulse; and palpation of the abdomen). The complaint analysis, results of the physical examination, and questionnaires of Tsvetov were used to evaluate drug tolerability.12 The rs1045642 polymorphism of the ABCB1 gene was studied.
The inclusion criteria for the study were stage I–II HT, and men and women over the age of 18 years. Patients were excluded from the study if they had stage III HT, uncontrolled HT, resistant HT, unstable angina, acute myocardial infarction, an acute cerebrovascular accident <6 months prior to the study, hypotension, decompensated heart failure of classes III–IV, exacerbation of illnesses requiring additional therapy, active liver disease, decompensation of diabetes, stage IV–V chronic renal failure, chronic alcoholism, drug addiction and mental illness that could affect compliance, contraindications for amlodipine or amlodipine intolerance, concomitant use of drugs that are metabolized by CYP3A4, pregnancy, and lactation. Before treatment, all patients either did not use antihypertensive therapy at all or did not receive regular antihypertensive therapy. The initial dose was 5 mg/day. As no clinical response was apparent during the first 2 weeks, the dose was increased twice (10 mg/day). If BP levels were <140/90, the dosage remained at 5 mg/day.
ABPM
All the enrolled patients underwent ABPM for 24 hours before the administration of amlodipine and again after 3 months of treatment. Repeated investigations were performed on a comparable (work) day using the same equipment every time throughout the study. The 24-hour noninvasive ABPM was performed using a SCHILLER BR-102 portable BP recorder, which uses both auscultatoric and oscillometric methods. The recorder was set to take one measurement every 15 minutes during the day and every 30 minutes at night. Daytime and nighttime periods were defined individually for each patient. To confirm the reliability of the nighttime readings, we compared them with the patients’ logs. Logs of activities, wake and sleep times, time of medication administration, meals, and any occurrence of symptoms were obtained from each patient. When the quality of the ambulatory tracing was not sufficient (valid measures <85%), the patients underwent repeat monitoring on the following day. Reading and editing of the data were performed using a computerized program. Mean values of 24-hour BP (mean arterial, systolic, and diastolic) and HRs were recorded. BP measurements obtained during the daytime and nighttime periods were considered in subsequent analysis together with the nocturnal reduction in BP percentage (<10% or >10%) that was calculated using the formula: ([diurnal value − nocturnal value]/diurnal value)×100%. Uncontrolled BP values, as assessed using ABPM, were 24-hour SBP ≥130 mmHg and/or 24-hour DBP ≥80 mmHg. Moreover, for diurnal and nocturnal BPs, increased values were considered to be ≥135/85 and ≥120/70 mmHg, respectively.17
OBPM
All the enrolled patients underwent OBPM on each visit. The first OBPM was performed before the administration of amlodipine. On the follow-up visits, to achieve maximum accuracy and estimate the trough effect, BP was measured before the next dose of amlodipine.18–20 Patients were asked to avoid food intake, strenuous exercise (which can lower BP), smoking, and the ingestion of caffeine 30 minutes prior to evaluation.21 Cuff sizes were chosen in accordance with the American Heart Association recommendations regarding the appropriate cuff size for a designated arm circumference.22
The BP measurement was performed in a quiet and warm examination room with the patient in a seated position with their back supported and legs uncrossed after 10 minutes of rest. The arm was supported at the level of the heart.23,24 Two or more readings separated by 2 minutes were averaged. If the first two readings of SBP differed by >5 mmHg, additional readings were obtained until stabilization had occurred, with a difference between the two readings of <5 mmHg. BP was checked simultaneously in both arms, at least once. BP was recorded in the arm with the higher pressure.25
Genotyping for the ABCB1 rs1045642 polymorphism
A total of 100 µL of venous blood was collected in VACUETTE® vacuum tubes (Greiner Bio-One, Kremsmünster, Austria) on the first day of amlodipine therapy. The standard proteinase K/phenol DNA isolation method was used. Genomic DNA was isolated from peripheral blood leukocytes using the DNK-Extran-1 kit (Syntol, Moscow, Russia).
All PCRs were performed with a negative control (no genomic DNA) to ensure that there was no contamination of reagents. Amplicon containing rs1045642 was amplified from genomic DNA using the following primers: CCACCGTCTGCCCACTCTGC (forward) and GGCCATCTATCCACCTATCTAA (reverse). The primers were designed using PrimerSelect 4.05©1993–2000 DNASTAR Inc. software and synthesized by Syntol. The carriership of ABCB1 rs1045642 was determined using real-time PCR with the SNP-Screen kit from CJSC Syntol. The program included preliminary denaturation at 95°C, which lasted for 3 minutes, 40 cycles of denaturation at 95°C for 15 seconds per cycle, and then annealing at 60°C for 40 seconds.26 Genotype polymorphisms were detected using Real-Time CFX96 Touch (Bio-Rad Laboratories Inc., Hercules, CA, USA).
The criteria for antihypertensive efficacy included the percentage of patients with normalization of BP (reduction in SBP <140 mmHg and DBP <90 mmHg) and a reduction in SBP ≥20 mmHg.15 The criteria for tolerability were as follows: excellent, no side effects; good, adverse reactions that did not require dose correction; satisfactory, adverse reactions that required dose correction; and unsatisfactory, discontinuation of amlodipine because of adverse reactions.
A statistical analysis of the results was performed with nonparametric methods using “Statistica v.10.0” software (StatSoft; Dell Statistica, Tulsa, OK, USA). To determine the significance of intergroup differences, the Mann–Whitney U-test was used for quantitative variables. To compare the three independent groups of quantitative data, a Kruskal–Wallis one-dimensional (single-factor) ANOVA with Bonferroni correction was used. To assess the reliability of the difference in the mean for two groups, Student’s t-test was used. Differences were regarded as significant at P<0.05. A comparison of qualitative signs was performed using the Fisher’s exact test or chi-squared test.
Results
Pharmacogenetic testing showed that ABCB1 rs1045642 genotype distribution was as follows: wild-type genotype CC was found in 17 patients, CT genotype was found in 53 patients, and TT genotype was found in 30 patients. The distribution of these genotypes was in agreement with the Hardy–Weinberg equilibrium (P=0.62).
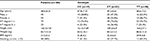
The mean age of the patients was 48.8±8.31 years (mean ± SD), and the patients had a mean body mass index of 31.5±5.2 kg/m2 (Table 1). A total of 45 men (45%) and 55 women (55%) participated in the study, and 75 participants presented with stage I HT and 25 with stage II HT. The initial OBPM values of the SBP were as follows: 146.9±8.39 mmHg for the CC genotype; 147.65±7.25 mmHg for CT; and 148.92±8.28 mmHg for TT (Table 2). The patients’ main demographic characteristics are presented in Table 1 according to their rs1045642 genotype. No relevant differences were found between the groups in terms of baseline characteristics.
  | Table 2 Results of office blood pressure measurements in patients with rs1045642 ABCB1 polymorphisms undergoing amlodipine therapy Note: Data are reported as mean ± SD. Abbreviation: HR, heart rate. |
At the 3-month evaluation, OBPM and ABPM demonstrated significant reductions in SBP and DBP across all genotypes and no significant HR changes.
OBPM
Table 2 shows the genotypes and the degree of BP reduction. The smallest BP reduction was in the CC group. SBP changed from 146.90±8.39 to 139.65±6.26 mmHg (–4.94±2.91∆%; P=0.04) and DBP from 89.51±7.94 to 83.04±6.38 mmHg (7.23±1.23∆%; P=0.02). The intermediate BP reduction was observed in the CT group: SBP changed from 147.65±7.25 to 139.00±5.36 mmHg (–5.86±2.12∆%; P=0.02) and DBP from 87.83±6.92 to 80.23±5.76 mmHg (–8.65±2.40∆%; P=0.04).
The largest change was observed in patients with the TT genotype: SBP reduced from 148.92±8.28 to 139.99±6.98 mmHg (–6.00±2.20∆%; P=0.02) and DBP from 85.22±7.35 to 76.85±6.06 mmHg (9.82±2.74∆%; P=0.04).
Significant differences in the SBP reduction, DBP reduction, and also in the ∆% were found between the CC and TT groups (P=0.04).
ABPM
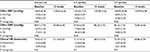
At the second ABPM recording, 24-hour SBP, 24-hour DBP, daytime SBP, daytime DBP, nighttime SBP, and nighttime DBP were significantly reduced across all genotype groups. HR did not change during the second ambulatory recording (Table 3).
Table 4 shows the genotypes and the BP variability. Patients with the TT genotype showed significantly decreased 24-hour SBP variability (P<0.05), 24-hour DBP variability (P<0.05), daytime SBP variability (P<0.01), and nighttime SBP variability (P<0.01). In the CT group, only the daytime SBP variability and the daytime DBP variability were significantly reduced (P<0.05).
  | Table 4 The effects of amlodipine on 24-hour, daytime and nighttime blood pressure variability in patients with rs1045642 ABCB1 polymorphisms Notes: Data are reported as mean ± SD. *P<0.05; **P<0.01. |
Significant differences in the BP reduction were found only between the CC and TT groups (Table 5).
  | Table 5 Intergroup differences in SBP and DBP reductions assessed using ambulatory blood pressure monitoring in patients with rs1045642 ABCB1 polymorphisms Note: Data are reported as mean ± SD. |
Efficacy and safety
Table 6 shows that 33 patients reached the target BP (SBP <140 mmHg and DBP <90 mmHg): two patients with the CC genotype (11%); 18 patients with the CT genotype (34%); and 13 patients with the TT genotype (43.3%). When using the Mann–Whitney U-test for pairwise comparisons between genotypes, we observed the significant intergroup differences: CC vs CT, P=0.02; CC vs TT, P=0.02; and CT vs TT, P=0.05.
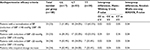  | Table 6 Antihypertensive efficacy of amlodipine in patients with rs1045642 ABCB1 polymorphisms Note: Data are reported as mean ± SD. Abbreviation: BP, blood pressure. |
The recommended dose for 66 patients was 5 mg/day, and 34 patients required a dosage increase up to 10 mg/day: nine patients (52.9%) with the CC genotype; 18 (34.05%) with the CT genotype; and seven (23.4%) with the TT genotype. Adverse events were observed in 16 patients during the 12-week study.
A total of 86 patients showed excellent tolerability, eight patients good tolerability and six patients satisfactory tolerability. The following side effects of varying severity were reported: leg and ankle swelling (peripheral edema) in eight patients, and redness of the face and upper extremities in six patients (Table 7).
  | Table 7 Adverse effects frequency in patients with rs1045642 ABCB1 gene polymorphisms undergoing amlodipine therapy |
An analysis of the incidence of adverse effects showed that 24.4% of patients with the CC genotype presented with adverse effects predominantly in the form of edema, and the TT genotype was associated with minimal adverse effects in 5.9% of patients (redness of the face and skin). The statistical significance of the intergroup differences was determined: CC vs TT, P=0.05; CC vs TT, P=0.05; CT vs TT, P=0.06; and ANOVA, P=0.05. A comprehensive assessment of the effects and tolerability of amlodipine therapy showed that the highest antihypertensive effect in combination with the lowest incidence of adverse reactions was in the TT group, while patients with the CC genotype showed a low antihypertensive effect and the highest incidence of adverse effects.
Discussion
Interindividual variability in drug efficacy and toxicity may result in unpredictable drug responses. This may be due to sequence variants in genes encoding drug metabolism enzymes, drug transporters, and/or drug targets.27 At least 105 variants have been identified for the ABCB1 gene, together with significant differences in their frequencies among different ethnic groups.28 Given the known interpopulation differences in drug response for amlodipine, it may be important to consider variability among ethnic groups by characterizing variability in genotypes, linkage disequilibrium, and recombination within and between ethnic populations.
Based on our data, we can infer that amlodipine pharmacokinetics is affected by the rs1045642 polymorphism of the ABCB1 gene. Patients with stage I–II HT and TT polymorphisms are expected to experience a greater antihypertensive effect and less adverse reactions from amlodipine therapy. In contrast, patients with CC polymorphisms have higher risks of adverse effects with lower doses of amlodipine. CT group patients may experience significant antihypertensive effects, but the incidence of adverse effects is slightly higher than in the TT polymorphisms group. Higher antihypertensive effects in the TT group can be explained by decreased expression of the ABCB1 gene and decreased P-gp synthesis. The effect of treatment is apparently much lower in the CC polymorphism group. On reviewing the literature, previous studies that could explain the association between CC polymorphisms and adverse effects were not found. To the best of our knowledge, the preexisting reports available in the literature are still controversial.29
The frequencies of ABCB1 rs1045642 CC, CT, and TT were 0.17, 0.53, and 30, respectively, which are similar to the report on Chinese hypertensive patients.30 The study by Guo et al included 60 patients and showed that the plasma concentration in the patients with ABCB1 rs1045642 TT genotype was lower compared to the patients with genotypes CC and CT (P<0.05), but the ABCB1 rs1045642 genotype had no impact on the antihypertensive efficacy of amlodipine (P>0.05). However, it is necessary to emphasize that the study by Guo et al was conducted in an Asian population, and the results with European patients may differ.
The results of Kim et al’s pharmacokinetic study are consistent with those of Guo et al’s study. The study included 26 Korean men.31 The frequencies of ABCB1 rs1045642 CC, CT, and TT were 0.35, 0.35, and 0.30, respectively. The results suggest that polymorphisms of the ABCB1 gene affect the disposition of amlodipine in humans. The authors stated that the polymorphic ABCB1 gene paradoxically reduced the plasma concentrations of amlodipine. Subjects with the mutant alleles (TT) of the ABCB1 gene, especially, showed an increase in the oral clearance of amlodipine with its lower plasma concentrations compared with those with the heterozygote (CT) or the wild-type (CC) genotype. Kim et al suggested that haplotype analysis rather than analysis of each genotype could be more crucial in determining the pharmacokinetic characteristics of amlodipine. The study also allowed us to rule out the potential role of gender difference because only male subjects were enrolled in this study.
Limitations
Lack of the control group had several consequences: we were unable to evaluate the placebo effect and possible confounding factors. Sample size of 100 patients and the power of study >80% were sufficient to determine only large effects. Further research with the greater number of participants, control group, and measurement of the pharmacokinetic parameters can find effects that this study failed to detect.
Further research on polymorphisms in other genes, in particular CYP3A5*3, is desirable to extend our knowledge of the pharmacogenetic characteristics of amlodipine.
Conclusion
The efficacy and safety of amlodipine were affected by the polymorphic ABCB1 gene in humans. These findings may provide a plausible explanation for interindividual variation in the amlodipine responses. The results of this study indicate the potential of pharmacogenetic testing for ABCB1 gene polymorphisms when prescribing amlodipine for the first time in Caucasian patients with stage I–II arterial HT.
Abbreviations
ABPM, ambulatory blood pressure measurement
BP, blood pressure
CCBs, calcium channel blockers
HR, heart rate
HT, hypertension
OBPM, office blood pressure measurement
P-gp, P-glycoprotein
SNP, single-nucleotide polymorphism
Acknowledgment
The authors thank Elena Kalle for genotyping assistance.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflict of interest in this work.
References
Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology. J Hypertens. 2013;(31):1281–1357. | ||
Cardioweb.ru [homepage on the internet]. Clinical guidelines “Diagnosis and Treatment of Arterial Hypertension”. Available from: https://www.cardioweb.ru/files/Klinicheskie_rekomendacii/Diagnostika_i_lechenie_arterialnoj_gipertonii.docx. Accessed March 26, 2014. Russian. | ||
Piepoli MF, Hoes AW, Agewall S, et al. European Guidelines on cardiovascular disease prevention in clinical practice. European Heart Journal. 2016;37(29):2315–2381. | ||
Chazova IE, Zhernakova JV, Oshhepkova EV, et al. Prevalence of cardiovascular risk factors in Russian patients with hypertension. Kardiologiya. 2014;10:4–12. | ||
Leonova M, Belousov Y, Shteynberg L, et al. Pharmacoepidemiology of arterial hypertension in Russia (Pyfagor III study. Farmateka. 2010;8:87–95. | ||
ALLHAT Collaborative Research Group. Major cardiovascular events in hypertensive patients randomized to doxazosin vs chlorthalidone: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA. 2002;288:1967–1975. | ||
Julius S, Kjeldsen SE, Weber M, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet. 2004;363(9426):2022–2031. | ||
Bakris GL, Sarafidis PA, Weir MR, et al. Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet. 2010;375(9721):1173–1181. | ||
Kukes VG, Sychev DA, Al’-Akhmad F, Dmitriyev VA. Влияние индивидуальных особенностей пациентов на риск развития нежелательных лекарственных реакций [Influence of individual characteristics of patients on the incidence of adverse reactions. Vestnik Roszdravnadzora. 2011;6:59–63. | ||
Dribnokhodova OP, Mironov KO, Dunayeva YA, Shipulin GA. Полиморфизмы генов, кодирующих транспортеры лекарственных средств ABCB1 и ABCG2, и исследование их методом пиросеквенирования [ABCB1 and ABCG2 polymorphisms encoding the drug carriers, and their study by pyrosequencing]. Eksperimentalnaya i klinicheskaya farmakologiya. 2012;75:29–36. | ||
Sychev DA, Muslimova OV, Gavrisyuk YV, Kosovskaya AV, Kukes VG. ФAрмAкогенеTичеCкие Tехнологии перCонAлизировAнной медицины: опTимизAция применения [Application of pharmacogenetic technologies in personalized medicine]. Terra Medica. 2011:124–129. | ||
Tsvetov VM. Monitoring of Adverse Drug Reactions in an Outpatient Clinic [dissertation]. Chelyabinsk: Chelyabinsk State Medical Academy; 2007. | ||
Finch A, Pillans P. P-glycoprotein and its role in drug-drug interactions. Aust Prescr. 2014;37(4):137–139. | ||
Drain S, Catherwood MA, Alexander HD, Denis Alexander H. Multidrug resistance in the chronic lymphoproliferative disorders. Leuk Lymphoma. 2010;51(10):1793–1804. | ||
Bodor M, Kelly EJ, Rj H. Characterization of the Human MDR1 Gene. AAPS J. 2005;7(1):E1–5. . | ||
Belle DJ, Singh H, Donna JB. Genetic factors in drug metabolism. Am Fam Physician. 2008;77(11):1553–1560. | ||
Committee for Medicinal Products for Human Use. Guideline on clinical investigation of medicinal products in the treatment of hypertension. European Medicines Agency. 2016:1–18. | ||
ESH/ESC Task Force for the Management of Arterial Hypertension. 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. 2013;31(10):1925–1938. | ||
Powers BJ, Olsen MK, Smith VA, et al. Measuring blood pressure for decision making and quality reporting: where and how many measures? Ann Intern Med. 2011;154(12):781. | ||
Myers MG. A proposed algorithm for diagnosing hypertension using automated office blood pressure measurement. J Hypertens. 2010;28(4):703–708. | ||
Sebo P, Pechère-Bertschi A, Herrmann FR, Haller DM, Bovier P. Blood pressure measurements are unreliable to diagnose hypertension in primary care. J Hypertens. 2014;32(3):509–517. | ||
Beevers G, Lip GY, O’Brien E. ABC of hypertension: Blood pressure measurement. Part II-conventional sphygmomanometry: technique of auscultatory blood pressure measurement. BMJ. 2001;322(7293):1043. | ||
Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697–716. | ||
Myers MG, Godwin M, Dawes M, et al. Conventional versus automated measurement of blood pressure in primary care patients with systolic hypertension: randomised parallel design controlled trial. BMJ. 2011;342:d286. | ||
O’Brien E, Asmar R, Beilin L, et al. Practice guidelines of the European Society of Hypertension for clinic, ambulatory and self blood pressure measurement. J Hypertens. 2005;23(4):697–701. | ||
Kryukov AV, Sychev DA, Andreev DA, et al. Influence of ABCB1 and CYP3A5 gene polymorphisms on pharmacokinetics of apixaban in patients with atrial fibrillation and acute stroke. Pharmgenomics Pers Med. 2018;11:43–49. | ||
Halperin AK, Cubeddu LX. The role of calcium channel blockers in the treatment of hypertension. Am Heart J. 1986;111(2):363–382. | ||
Zhao LM, He XJ, Qiu F, Sun YX, Li-Ling J, Xj H. Influence of ABCB1 gene polymorphisms on the pharmacokinetics of verapamil among healthy Chinese Han ethnic subjects. Br J Clin Pharmacol. 2009;68(3):395–401. | ||
Huang Y, Wen G, Lu Y, et al. CYP3A4*1G and CYP3A5*3 genetic polymorphisms alter the antihypertensive efficacy of amlodipine in patients with hypertension following renal transplantation . Int J Clin Pharmacol Ther. 2017;55(2):109–118. | ||
Guo C, Pei QI, Tan H, et al. Effects of genetic factors on the pharmacokinetics and pharmacodynamics of amlodipine in primary hypertensive patients. Biomed Rep. 2015;3(2):195–200. | ||
Kim KA, Park PW, Park JY. Effect of ABCB1 (MDR1) haplotypes derived from G2677T/C3435T on the pharmacokinetics of amlodipine in healthy subjects. Br J Clin Pharmacol. 2007;63(1):53–58. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.