Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 9
Effectiveness of topical peppermint oil on symptomatic treatment of chronic pruritus
Authors Elsaie LT, El Mohsen AM, Ibrahim IM, Mohey-Eddin MH, Elsaie ML
Received 11 July 2016
Accepted for publication 19 August 2016
Published 11 October 2016 Volume 2016:9 Pages 333—338
DOI https://doi.org/10.2147/CCID.S116995
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Lotfy T Elsaie,1,† Abdelraouf M El Mohsen,1 Ibrahim M Ibrahim,1 Mahmoud H Mohey-Eddin,1 Mohamed L Elsaie2
1Department of Dermatology, Al Azhar University, 2Department of Dermatology, National Research Centre, Cairo, Egypt
†Dr Lotfy T Elsaie passed away on December 17, 2014
Background: Pruritus is one of the commonest skin complaints. Peppermint oil can be effective in reducing the severity of such a condition.
Aim: The aim of this study was to assess the efficacy of topically applied peppermint oil in the treatment of chronic pruritus.
Subjects and methods: Fifty selected subjects diagnosed with chronic pruritus due to hepatic, renal, or diabetic cause were studied and divided into two groups of 25 patients each. Group I patients were instructed to hydrate the skin and then apply topical peppermint oil, while Group II patients applied petrolatum topically by hand; this application was done on the areas of pruritus, twice daily for 2 weeks. The severity of the itch was assessed and compared before and after the study by the 5-D itch scale (5D-IS). The results were analyzed by SPSS software. Statistical methods such as descriptive analysis, independent samples t-test, paired samples t-test, and chi-square test were employed.
Results: There was a significant improvement regarding all studied individual parameters (5-D IS) for the peppermint oil users with no significance among petrolatum users. A comparison of total score of 5-D IS between patients of Group I and patients of Group II favored the improvement following the use of peppermint oil than using placebo (P-value <0.05).
Conclusion: The topical treatment of chronic pruritus with peppermint oil is effective, easy to use, safe, cheap, and more acceptable for those whose topical and systemic treatments tend to be irritating, contraindicated, or less well tolerated.
Keywords: pruritus, peppermint oil, itch
Introduction
Chronic pruritus is defined as an itch persisting for >6 weeks, which can be severe enough to interfere with lifestyle activities.1 Pruritus can be a hallmark of many skin diseases as well as other noncutaneous diseases. Neuropathic, psychogenic, systemic, and dermatologic disorders constitute the majority of causes of pruritus.2
Peppermint (Mentha piperita, of the Labiatae or Lamiaceae family), a native herb of Mediterranean Europe that is cultivated in many parts of the world, is a well-known plant that can be used in many forms (ie, oil, leaf, leaf extract, and leaf water).3 Peppermint oil is a hybrid of spearmint (Mentha spicata) and water mint (Mentha aquatica) and is synonymous with Mentha oil, M. piperita oil, and oil of peppermint.4
Records from ancient Egypt, Greece, and Rome show that peppermint has been used medicinally for centuries for gastrointestinal disorders, including irritable bowel syndrome, indigestion, and nausea, as well as cold, headache, and cramps.5
Recently, topical application of peppermint oil has also received much attention. A little has been published on peppermints effect on pruritus or other conditions other than irritable bowel syndrome, for which its use is still controversial.6
The present pilot study aimed to evaluate application of peppermint oil for the treatment of chronic pruritus of renal, hepatic, and diabetic origins.
Subjects and methods
This study was conducted on 50 patients (of both sexes and different ages) attending the outpatient clinic of dermatology, venereology, and andrology in Al-Hussein University Hospital, Cairo, Egypt, and suffering from chronic pruritus, ie, hepatic, renal, and diabetic pruritus, during the period from June 2014 to June 2015. The study was initially approved by the ethical committee of Al-Azhar University. Written informed consent was obtained from all participants before enrollment (Table 1).
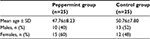  | Table 1 Age and sex in the studied groups Abbreviation: SD, standard deviation. |
Exclusion criteria
The following patients were excluded from the study:
- patients with dermatological diseases that cause pruritus, eg, psoriasis and contact dermatitis;
- patients who suffered from acute pruritus (<6 weeks); and
- patients with chronic pruritus due to systemic disease other than chronic renal disease, hepatic disease, or diabetes mellitus.
The studied population was divided into two groups: Group I with 25 patients applied 5% of topical crude peppermint oil, while Group II of 25 patients applied topical petrolatum.
Materials
The materials required for this study were as follows:
- 5% crude peppermint oil in petrolatum for Group I patients and
- petrolatum base used alone for Group II patients.
Methods
All patients were subjected to an informed verbal consent after explanation of the problem and its medication.
All patients were subjected to the following.
Clinical assessment
The patients were subjected to history taking about their present illness, duration, degree, direction, and distribution of pruritus, in addition to disabilities resulting from pruritus (sleep disorder, social disorder, house work, and work problems); all of these constituted the items of pruritus scale estimation, according to the 5-D itch scale (5-D IS) of assessment of pruritus.7 The distribution domain included 16 items of itch locations (Figure 1):
  | Figure 1 The 5-D IS. Abbreviations: 5-D IS, 5-D itch scale; N/A, not applicable. |
- physical examination;
- general examination: for clinical evidence of renal or hepatic affection, as well as diabetes mellitus; and
- local examination: to exclude dermatological causes of pruritus and to determine the distribution of pruritus according to the 5-D IS.
Diagnosis of chronic pruritus
The diagnosis of chronic pruritus was done as follows:
- History: history of pruritus >6 weeks with history of chronic liver diseases, renal diseases, or diabetes.
- Clinically: by exclusion of dermatological causes of itching and the presence of involved systemic disease.
- Investigations: chosen patients were known hepatic, renal, or diabetic patients (proved by previous investigations of liver functions, kidney functions, and fasting blood glucose).
Patient instructions for drug application
The patients were instructed to hydrate the skin and then apply the preparations (peppermint or petrolatum) topically by hand; this application was done on the areas of pruritus, twice daily for 2 weeks.
Follow-up
Two weeks after the treatment, the patients were evaluated for improvement of itching and its severity, using the 5-D IS of assessment along with the possible recording of side effects such as irritation and burning sensation.
Statistical analysis
Statistical evaluation was done using the SPSS software, and methods such as descriptive analysis, independent samples t-test, paired samples t-test, and chi-square test were employed. The significance level was set at a P-value of <0.05.
Results
Fifty patients were included in this study (26 males and 24 females). According to the cause of chronic pruritus, there were 16 patients with renal diseases, 15 patients with hepatic diseases, and 19 patients with diabetic disease.
The patients were divided into two groups. Group I included 25 patients (10 males and 15 females). The mean age of patients was 47.76±8.23 years with minimum age 32 years and maximum age 66 years. They were subdivided according to the cause of pruritus into three subgroups:
- renal: eight patients;
- hepatic: seven patients; and
- diabetic: ten patients.
They were treated with 5% of topical peppermint oil for 2 weeks.
Group II included 25 patients (13 males and 12 females). The mean age of patients was 50.76±7.80 years with minimum age 29 years and maximum age 64 years. They were subdivided according to the cause of pruritus into three subgroups:
- renal: eight patients;
- hepatic: eight patients; and
- diabetic: nine patients.
They were treated with topical petrolatum as placebo for 2 weeks.
Results of Group I
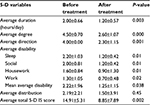
The average total score of 5-Ds for Group I before and after treatment was 15.18±3.55 and 7.94±3.28, respectively. There was a significant improvement regarding all studied individual parameters (5-D IS), including duration, degree, direction, disability, and distribution domains (P-value <0.05; Table 2).
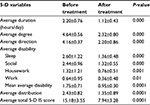  | Table 2 Effect of using peppermint oil before and after treatment (n=25) |
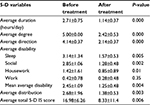
All the hepatic, renal, and diabetic patients showed a significant improvement regarding all studied individual parameters (5-D IS), including duration, degree, direction, disability, and distribution domains (P-value <0.05), except for the either “work” only or “work” and “housework” domains where there was no significant change before and after treatment (P-value >0.05; Tables 3–5).
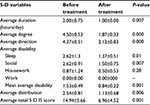  | Table 3 Improvement of patients with renal pruritus in Group I |
  | Table 4 Improvement of patients with hepatic pruritus in Group I |
  | Table 5 Improvement of patients with diabetic pruritus in Group I |
Comparison of total score of 5-D IS among Group I indicated that improvement among patients had no correlation with gender (P-value <0.05). However, when comparing between male and female patients regarding the total score of the 5-D IS before treatment, there was a small but a significant difference (P-value <0.05), same as with comparison after the treatment.
Results of Group II
The average total score of the 5-Ds for Group II before and after treatment was 14.54±2.09 and 13.47±3.73, respectively. There was no significant improvement in the duration, direction, disability, and distribution domains (P-value >0.05), while there was a significant improvement among the degree of itch and among the social and sleep items of the disability domain (Table 6).
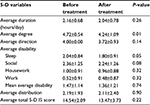  | Table 6 Effect of using petrolatum before and after treatment (n=25) |
All the hepatic, renal, and diabetic patients showed no significant improvement regarding all studied individual parameters (5-D IS) to all the studied individual parameters (5-D IS), including duration, degree, direction, disability, and distribution domains (P-value >0.05). Comparison of the total score of the 5-D IS with regard to gender among Group II indicated that the absence of improvement among patients had no correlation with gender (P-value >0.05); however, when comparing male and female patients regarding the total score of the 5-D IS before treatment, there was a small but a significant difference (P-value >0.05).
Discussion
A wide range of herbal remedies was proposed for use in pruritus. Tannins, chamomile, camphor, menthol, aloe vera, oatmeal, and others are traditionally considered of low risk and good value in treating pruritus, but there are no controlled studies to determine such effects.8
Peppermint is thought to alleviate the sensation of itch by activating A-delta fibers and k-opioid receptor.9 Previous research has shown that menthol in low concentrations is effective with no irritant effect.10 The long-term use of menthol for chronic itch has not been studied.6 In a letter to the editor of The Lancet in 1870, Dr A. Wright said that he had witnessed peppermint oil being used to treat “facial neuralgia” in the People’s Republic of China and that he had been able to repeat this success in his own practice.6
Only four patients who applied the oil in flexures (groin and axillae) complained of a burning sensation; otherwise, there were no reported side effects. Peppermint oil is generally recognized as safe according to the US Food and Drug Administration.11 However, the higher doses of peppermint oil used for medicinal purposes have not been extensively regulated, as peppermint oil is sold as a dietary supplement.
The efficacy of peppermint oil in combination with sesame oil was only studied once in female patients with pruritus gravidarum and has shown a consistent statistical significance in comparison to placebo.12 The patients used peppermint oil 0.5% in sesame oil and applied twice daily for 14 days. The severity of the itch was assessed and compared before and after the study by the visual analog system. The severity of the itch in the treated group with peppermint oil in comparison with the placebo group showed a significant statistical difference.10
In this study, the use of peppermint oil for pruritus of hepatic, renal, and diabetic origin showed a significant improvement regarding all studied individual parameters (5-D IS), including duration, degree, direction, disability, and distribution domains (P-value <0.05).
Conclusion
The topical treatment of chronic pruritus with peppermint is effective, easy to use, safe, cheap, has favorable odor, and is more acceptable for whom topical and systemic treatments tend to be irritating, contraindicated, or less well tolerated. This therapeutic option for chronic pruritus has excellent results and is free from toxic side effects.
Disclosure
The authors report no conflicts of interest in this work.
References
Reamy BV, Christopher W, Fletcher S. A diagnostic approach to pruritus. Am Fam Physician. 2011;84(2):195–202. | ||
Ständer S, Weisshaar E, Mettang T, et al. Clinical classification of itch: a position paper of the International Forum for the Study of Itch. Acta Derm Venereol. 2007;87(4):291–294. | ||
Nair B. Final report on the safety assessment of Mentha piperita (peppermint) oil, Mentha piperita (peppermint) leaf extract, Mentha piperita (peppermint) leaf, and Mentha piperita (peppermint) leaf water. Int J Toxicol. 2001;20(Suppl 3):61–73. | ||
Herro E, Jacob SE. Mentha piperita (peppermint). Dermatitis. 2010; | ||
Spirling LI, Daniels IR. Botanical perspectives on health peppermint: more than just an after-dinner mint. J R Soc Promot Health. 2001;121(1): | ||
Wright A. Oil of peppermint as a local anaesthetic. Lancet. 1870; | ||
Elman S, Hynan LS, Gabriel V, Mayo MJ. The 5-D itch scale: a new measure of pruritus. Br J Dermatol. 2010;162(3):587–593. | ||
Weisshaar E, Szepietowski JC, Darsow U, et al. European guideline on chronic pruritus. Acta Derm Venereol. 2012;92(5):563–581. | ||
Patel T, Ishiuji Y, Yosipovitch G. Menthol: a refreshing look at this ancient compound. J Am Acad Dermatol. 2007;57(5):873–878. | ||
Davies SJ, Harding LM, Baranowski AP. A novel treatment of postherpetic neuralgia using peppermint oil. Clin J Pain. 2002;18(3):200–202. | ||
Food and Drug Administration. Code of Federal Regulations. Title 21. Vol. 3. Silver Spring, MD: Food and Drug Administration; 2014. Part 182. Subpart A. Sec 182.20. | ||
Amjadi MA, Mojabb F, Kamranpoura SB. The effect of peppermint oil on symptomatic treatment of pruritus in pregnant women. Iran J Pharm Res. 2012;11(4):1073–1077. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
