Back to Journals » Clinical Epidemiology » Volume 14
Effectiveness and Safety of Reduced and Standard Daily Doses of Direct Oral Anticoagulants in Patients with Nonvalvular Atrial Fibrillation: A Cohort Study Using National Database Representing the Japanese Population
Received 1 February 2022
Accepted for publication 25 April 2022
Published 29 April 2022 Volume 2022:14 Pages 623—639
DOI https://doi.org/10.2147/CLEP.S358277
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Eyal Cohen
Kiyoshi Kubota,1,2 Nobuhiro Ooba2
1NPO Drug Safety Research Unit Japan, Tokyo, Japan; 2Department of Clinical Pharmacy, Nihon University School of Pharmacy, Funabashi, Chiba, Japan
Correspondence: Kiyoshi Kubota, NPO Drug Safety Research Unit Japan, 6-2-9-2F Soto-Kanda, Chiyoda-ku, Tokyo, 101-0021, Japan, Tel +81-3-6284-4206, Fax +81-3-6284-4207, Email [email protected]
Purpose: To compare the effectiveness and safety of reduced or standard daily doses of direct oral anticoagulants (DOACs) with warfarin in Japanese patients with nonvalvular atrial fibrillation (NVAF). We used post-hoc analyses to identify patient groups that could benefit from reduced-dose DOACs.
Patients and Methods: Using the National Database of Health Insurance Claims and Specific Health Checkups of Japan, we identified 944,776 patients with NVAF who had started an oral anticoagulant after at least one year of non-use between April 2011 and March 2016. We matched patients taking any, reduced, or standard doses of DOACs 1:1 with those taking warfarin. We measured treatment effectiveness based on admission due to stroke or systemic embolism (S/SE) and safety based on admission due to any bleeding (defined as major bleeding, MB). We compared both outcomes between DOACs and warfarin using the Cox proportional hazards model. We used post-hoc analysis to match patients receiving reduced-dose DOACs to those receiving standard-dose DOACs and compared treatment effectiveness and safety.
Results: More than half of patients receiving DOACs used a reduced dose. The occurrences of S/SE and MB in patients receiving any, reduced, or standard doses of DOACs were equal to or lower than those receiving warfarin. In the post-hoc analysis, the risk of S/SE and MB was similar between reduced and standard doses of DOACs except for those with a history of cerebral infarction and CHA2DS2-VASc score ≥ 3, where the risk of S/SE was lower for reduced doses of any and individual DOACs.
Conclusion: Findings from the current study are consistent with recent Asian and global studies but different from most studies conducted in North America and Europe, where patients receiving a reduced dose of DOACs had an increased risk of S/SE. Future studies should test the reproducibility of results from the current study.
Keywords: atrial fibrillation, oral anticoagulant, database, propensity score, CHA2DS2-VASc score, pharmacoepidemiology
Introduction
Anticoagulant therapy is widely used to prevent stroke and systemic embolism in patients with atrial fibrillation.1–3 The advent of direct oral anticoagulants (DOACs) has facilitated anticoagulant therapy for patients with nonvalvular atrial fibrillation (NVAF) because it does not require frequent laboratory monitoring, and randomized trials have shown that the efficacy and safety of DOACs are similar or superior to treatment with warfarin.4–7 However, individualizing the daily dose of DOACs to maximize the benefit of preventing stroke or systemic embolism while minimizing the risk of bleeding is essential because laboratory monitoring is not available to optimize dosing.
The criteria used for a reduced daily dose differ among DOAC types; the criteria also differ among country guidelines, even for the same DOAC (Table S1).1–3 Standard and reduced daily doses of rivaroxaban also vary among countries. In Japan, standard and reduced doses are 15 and 10 mg/day, respectively, based on a study of rivaroxaban pharmacokinetics in Japanese subjects.8 Yet, standard and reduced daily doses of rivaroxaban are 20 and 15 mg/day, respectively, in many other countries.
The use of reduced-dose DOACs which do not conform to current guidelines/regulations is common, particularly in Asia.9–13 Reports on the effectiveness and safety of reduced-dose DOACs showed conflicting results.14–55 In the current study, we investigated the distribution of daily DOAC doses and the effectiveness and safety of reduced- and standard-dose DOACs compared to warfarin using a national Japanese claims database. In post-hoc analysis, we assessed patient groups that could benefit from reduced- versus standard-dose DOACs.
Materials and Methods
Dataset and Patient Selection
We used claims data for patients who received an oral anticoagulant such as warfarin, dabigatran, rivaroxaban, apixaban, or edoxaban, between April 1, 2010, and March 31, 2016, extracted from the National Database of Health Insurance Claims and Specific Health Checkups of Japan (NDB Japan). We identified 3,389,507 patients assuming that pairs of two identifiers (ID1 and ID2) represented the same patient if one of these two was identical between pairs.56 All subjects had ID1 and ID2; ID1 was created by encrypting the combination of health card number issued by the workplace, date of birth, and sex, while ID2 was created by encrypting the combination of family and given names, date of birth, and sex.56 Two identifiers are used in NDB Japan because ID1 may change when a subject gets a new job, and ID2 may change when the family name changes (eg, due to marriage). We selected patients who were at least 20 years old and had started a single oral anticoagulant after a diagnosis of atrial fibrillation, not specified as “suspected” or “valvular” (defined as NVAF in the current study), who had at least one year of no anticoagulant use (Figure 1). We excluded patients if they had a diagnosis code other than NVAF indicating use of an oral anticoagulant (defined as “non-AF indication”, Table S2) except when the first non-AF indication appeared after the patient with NVAF had started an oral anticoagulant (Figure S1). We also excluded patients if they had received edoxaban before October 2014 when NVAF became an indication for this medication or had died in the month after starting an oral anticoagulant because only the year and month of death were available from Japanese claims data; thus we were not able to confirm whether a patient had access to the drug.
 |
Figure 1 Flow chart for selection of new users of DOAC and warfarin with NVAF. aFigure S1 diagrammatically shows the exclusion process. Abbreviations: DOAC, direct oral anticoagulant; OAC, oral anticoagulant; AF, atrial fibrillation; NVAF, non-valvular atrial fibrillation. |
Of the remaining 944,776 eligible patients, 727,866 had a diagnosis code of NVAF only during the observation period, while 216,910 had a diagnosis code of NVAF followed by a non-AF indication after starting an oral anticoagulant. New users of an oral anticoagulant included 373,956 who received warfarin and 570,820 who received DOACs as follows: dabigatran (n=191,441), rivaroxaban (n=207,496), apixaban (n=150,143), and edoxaban (n=21,740).
Daily Dose of DOAC
We defined the daily dose of DOAC as the most frequently prescribed dose in one or more DOAC prescriptions before a study subject was censored (see details of censoring under Statistical Analysis). We classified the daily dose as a reduced dose if the most frequent daily dose was 220 mg/day dabigatran, 10 mg/day rivaroxaban, 5 mg/day apixaban, and 30 mg/day edoxaban. The daily dose was classified as a standard dose if the dose was 300 mg/day dabigatran, 15 mg/day rivaroxaban, 10 mg/day apixaban, and 60 mg/day edoxaban.
Estimation of Propensity Scores and 1:1 Matching
We estimated the propensity score (PS) using the age at which a patient started an oral anticoagulant (as a continuous variable), sex, and 28 diagnosis codes and 34 drug codes potentially relevant to the use of an anticoagulant or occurrence of outcomes as covariates (Table S3). The confounding status was positive if we found a corresponding diagnosis code or drug in any claims issued within one year before the patient started an oral anticoagulant. Using logistic regression, we estimated three separate PSs for any, reduced, or standard doses of any DOAC compared to warfarin. We also estimated PSs for any, reduced, or standard doses of individual DOACs (dabigatran, rivaroxaban, apixaban, or edoxaban) compared to warfarin. Since clinical practice for the selection of an anticoagulant (DOAC versus warfarin) for patients with specific characteristics (eg, age or comorbidities) may have changed during the observation period, we divided the 60 months between April 2011 and March 2016 into ten six-month periods and estimated PSs in each of ten groups of patients who started an oral anticoagulant in the corresponding six-month period.
We matched a patient receiving warfarin to a patient receiving a DOAC by PS (1:1 matching) in each of ten six-month periods using Parsons’ 5-to-2 digit matching algorithm.57 We used sex, age group (<55, 55–64, 65–74, or >74 years old), and previous history of outcomes (diagnosis code of cerebral infarction, systemic embolism, intracranial bleeding, gastrointestinal (GI) bleeding, other bleeding, and myocardial infarction in any outpatient/inpatient claim before starting an oral anticoagulant) as additional matching variables.
Outcomes
The main outcome for treatment effectiveness was hospital admission due to stroke or systemic embolism (S/SE), and the main outcome for safety was major bleeding (MB), defined as admission due to any bleeding (Table S4A). We also examined individual outcomes for effectiveness (cerebral infarction, cerebral bleeding, and systemic embolism) and safety (intracranial bleeding, GI bleeding, and other bleeding), hospital admissions due to myocardial infarction, and deaths due to any cause. In the current analysis, cerebral bleeding was included as an outcome to evaluate effectiveness (stroke) and safety (intracranial bleeding) as in the RE-LY randomized trial.4
The current study used a conservative definition of outcomes (Table S4B); the first admission after starting an oral anticoagulant when it was the admission to a diagnosis procedure combination (DPC) hospital in which S/SE or MB was one of three major DPC diagnoses (main condition, trigger-for-hospitalization condition, and greatest-resource condition),58 or the admission to a non-DPC hospital in which the diagnosis was followed by outcome-specific treatment specified in Table S4C. Throughout this study we used this outcome definition because some outcomes had not yet been validated. However, in the sensitivity analysis (detailed in Statistical Analysis) we used less strict definitions that included any admission with a diagnosis code of S/SE or MB.
Main and individual outcomes (and myocardial infarction) were estimated separately in patients with and without a history of the corresponding outcomes before starting an anticoagulant (Figure S2). To avoid complexity, we considered patients with a diagnosis of any intracranial bleeding before starting an anticoagulant to have a history of intracranial bleeding (a component of the main outcome for MB) and a history of cerebral bleeding (a component of the main outcome for S/SE) even if the patient had a history of intracranial bleeding other than cerebral bleeding (eg, subarachnoid bleeding).
In previous studies, the code for “dead” in inpatient or outpatient claims had a high positive predictive value (PPV) (95.6%).59 The PPV for acute myocardial infarction in DPC claims was 78.7% to 93.8%,58,60 and the PPV for cerebrovascular diseases, including hemorrhagic and ischemic stroke, in DPC claims was 85.7% to 89.9%.60,61
In this study, we followed patients until the occurrence of an outcome of interest, death (“dead” indicated on an inpatient or outpatient monthly claim), first diagnosis of a non-AF indication, anticoagulant discontinuation (defined as a gap between prescriptions with 30 days of grace period), change to a different anticoagulant (including change from one type of DOAC to another), or March 31, 2016, whichever came first. Information on “day” was available in the claims data for treatment and outcome occurrences, while we defined the date of death for this study as day 15 of the month when the patient died.
Statistical Analyses
We estimated frequencies and percentages for categorical variables and means and standard deviations for continuous variables to summarize patient characteristics. We assessed covariate balance in patients with DOAC versus warfarin using the absolute standardized difference (aSD), in which a value of 0.1 or more was considered important.62
After 1:1 matching, we compared the occurrence of outcomes between DOAC and warfarin by estimating rate ratios (RRs) and hazard ratios (HRs) using Cox proportional hazards models with 95% confidence intervals (CIs). We regarded death as a competing event to the outcome of interest when estimating HRs and generating the cumulative incidence function.63,64 In the primary analyses, we compared the main outcome for effectiveness (S/SE) and safety (MB) between patients receiving DOAC and those receiving warfarin with and without a history of S/SE and any bleeding, respectively, for any, reduced, or standard doses of any DOAC. In the secondary analyses, we repeated the estimation from the primary analyses for each DOAC along with individual outcomes for effectiveness and safety, myocardial infarction, and all-cause mortality.
We conducted several sensitivity analyses. First, we repeated the primary and secondary analyses using a less strict definition of first admission to any hospital with a condition code for each outcome. Second, we conducted stratified analyses by sex and age group (<55 versus ≥55, <65 versus ≥65, and <75 versus ≥75 years old). Third, we analyzed data for the main outcomes using grace periods of 15, 60, and 90 days. Fourth, we conducted weighting analyses using the PSs used for 1:1 matching after excluding subjects with preference scores <0.3 or >0.7 in each of ten six-month periods.65 In the weighting analyses, we estimated HRs and 95% CIs using the robust variance by inverse probability of treatment weighting (IPTW),66 matching weight (MW),67 overlapping weight (OW),68 and fine stratum weighting (FSW).69 In FSW, we stratified patients into 100 fine strata in each of ten six-month periods. When stratified by the history of outcome of interest, sex, and age group, we estimated the distribution of all covariates in each stratum. Covariates with aSD>0.1 in any stratum were included in the model when HR was estimated using the Cox proportional hazards model.70 We did not present HRs and CIs when the number of outcomes was smaller than five times the number of explanatory variables (an exposure variable plus covariates with aSD>0.1).71
For additional analyses, we divided patients selected by 1:1 matching divided into six subgroups for CHA2DS2-VASc scores (0 or 1, 2, 3, 4, 5, and >5),72 five subgroups for HAS-BLED scores (0 or 1, 2, 3, 4, and >4),73 and seven subgroups for Charlson Comorbidity Index (CCI) scores (0, 1, 2, 3, 4, 5, and >5) in each six-month period. We estimated the CCI score according to a previous study in which risk factors were defined by the International Classification of Diseases, Tenth Revision (ICD-10) codes.74 We defined the risk factors for the CHA2DS2-VASc and HAS-BLED scores in Tables S5A and B by references to a prior study on mapping ICD-9 clinical modification (CM) codes (ICD-9 CM) to ICD-10 CM codes regarding those scores.75 We estimated RRs and HRs to evaluate the occurrence of S/SE in patients on DOACs compared with warfarin in subgroups classified using CHA2DS2-VASc scores, the occurrence of MB in subgroups using HAS-BLED scores, and all-cause mortality in subgroups using CCI scores. We stratified all patients by these scores irrespective of whether they had a history of the outcomes of interest because they were used to estimate the scores (eg, prior stroke and bleeding). In the Cox proportional hazards model, PS was included as an explanatory variable while using six-month periods in which PS was estimated as strata because the matching was ignored when we stratified subjects according to these scores.
We used post-hoc exploratory analyses to compare patients receiving reduced-dose DOACs to those receiving standard-dose DOACs to find patient groups that might benefit from the reduced-dose treatment. We estimated PSs and matched a reduced-dose DOAC user to a standard-dose DOAC user in each of ten six-month periods similarly to the matching of a DOAC user to a warfarin user, except that we used the molecular entity of DOAC (dabigatran, rivaroxaban, apixaban, and edoxaban) as a matching variable in addition to sex, age group, and history of each outcome. We estimated effectiveness and safety in those patients on a DOAC selected by 1:1 matching. Specifically for S/SE and cerebral infarction, we estimated RRs and HRs for individual DOACs. As additional post-hoc exploratory analyses, we subclassified patients selected by 1:1 matching by CHA2DS2-VASc scores or HAS-BLED scores and evaluated effectiveness and safety in each subgroup. Specifically for S/SE and cerebral infarction, we divided patients into those with CHA2DS2-VASc score <3 and those with CHA2DS2-VASc score ≥3 and estimated RRs and HRs for individual DOACs. Furthermore, we subdivided patients taking a DOAC selected by 1:1 matching by three additional factors and evaluated S/SE and cerebral infarction. First, we stratified them by the number of days (0–7, 8–14, 15–30, and 31 or more days) between the last day of admission due to S/SE or cerebral infarction, before starting DOAC treatment, and the day when they initiated DOAC treatment. Second, we stratified patients by the type of NVAF diagnosis before starting a DOAC; NVAF as one of three major DPC diagnoses, another in-hospital diagnosis, or an outpatient diagnosis only. Third, we stratified patients by the number of days delay (0–30, 31–90, 91–365, and 366 days or longer) between the earliest day when any claim recorded the NVAF diagnosis and the day of starting a DOAC. In the Cox proportional hazards model used in additional post-hoc analyses to stratify patients by CHA2DS2-VASc scores, HAS-BLED scores, and three additional factors, we used PS as an explanatory variable while using six-month periods in which we estimated PS as strata because we ignored 1:1 matching in those additional analyses.
All statistical analyses were conducted by using SAS 9.4.
Ethics
This study was approved by the ethics committee of the Nihon University School of Pharmacy which waived the need of obtaining patient consent (16-008) and registered to the UMIN Clinical Trials Registry (UMIN000027974) even though this was an observational study. All data accessed complied with data protection and privacy regulations given in relevant guidelines and laws.
Results
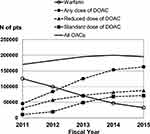
Table 1 shows that the age, sex, and other characteristics of patients who used warfarin were similar to those who used any, reduced, and standard doses of any DOAC after 1:1 matching (aSD<0.1 for all covariates). These characteristics were also similar for matched patients who used warfarin and any, reduced, and standard doses of individual DOACs (aSD<0.1 for all covariates) (data not shown). In the pre-matched population, patients who used warfarin had a mean age of 60.2 years, and 57.9% were male; patients who used reduced-dose DOACs were slightly older (62.0 years old) and had slightly fewer males (54.5%), and those who used standard-dose DOACs were considerably younger (51.5 years old) and more often male (73.6%) (Table S6A). The annual number of new users of any oral anticoagulant (warfarin or DOAC) gradually increased from 170,596 in fiscal year (FY; April to March of the following year) 2011 to 200,114 in FY 2014 but decreased slightly to 195,344 in FY 2015. However, new warfarin users declined 74% from FY 2011 to FY 2015, while users of any DOAC increased by 6.8-fold (Figure 2). In FY 2011, 45,485 (26.7%) of the 170,596 new oral anticoagulant users were using DOACs, while in FY 2015, 162,898 (83.4%) of the 195,349 new anticoagulant users used DOACs. In pre-matching, new warfarin users had more frequently anemia, hypertension, heart failure, peptic ulcer, vascular disease, pulmonary disease, and renal disease; furthermore, they used drugs more frequently including aspirin, angiotensin-converting-enzyme inhibitor/angiotensin receptor blocker, carvedilol, and proton pump inhibitor, to treat those conditions than new users of any, reduced, or standard doses of DOACs. The proportion of patients with a history of S/SE was higher in reduced-dose DOAC users but lower in standard-dose DOAC users than warfarin users. Similarly, the proportion of patients with a history of any bleeding was higher in users of reduced-dose DOACs but lower in standard-dose DOAC users than warfarin users (Table S6A).
 |
 |
 |
Table 1 Distribution of Covariates in New Users with Any, Reduced, and Standard Doses of Direct Oral Anticoagulant (DOAC) Compared with New Users of Warfarin Selected by 1:1 Matching |
Table 2 shows the distribution of new users’ most frequent daily DOAC dose, demonstrating that most (>89%) patients used either reduced or standard doses. Dabigatran and edoxaban had around 70% reduced-dose users, while rivaroxaban and apixaban had slightly over 50% reduced-dose users. The proportion of reduced-dose users of any DOAC was 67% in FY 2011 but decreased to 57% in FY 2013 and 54% in FY 2015. This decrease was mainly due to the shift in frequently used DOACs from dabigatran in FY 2011 and FY 2012 to rivaroxaban and apixaban in FY 2013 to FY 2015 (Table S6B). The daily DOAC dose did not change for most users; reduced-dose DOAC users were on the same daily dose for 97.7–99.1% of the observation periods, and standard-dose DOAC users were on the same daily dose for 96.1–98.1% of the observation periods (Table S7A and B). The proportion of patients with a history of S/SE and any bleeding was higher in reduced-dose users than in standard-dose users for all four DOACs, as seen in Table 2.
 |
Table 2 Most Frequent Daily Dose of DOAC and Patients with Reduced and Standard Daily Doses with a History of S/SE and Any Bleeding |
Table 3 shows crude incidence rates, RRs, and HRs of S/SE and MB in 222,030, 184,837, and 96,302 users of any, reduced, or standard DOAC doses, respectively, and the same number of warfarin users selected by 1:1 matching. The data were further stratified into patients with and without a history of each outcome before starting an oral anticoagulant. For example, 222,030 pairs of users of any dose of DOAC and warfarin were divided into 133,332 pairs without and 88,698 pairs with a history of S/SE. During the observation period, the incidence rate of S/SE was 17.6 to 21.8 per 1000 patient-years in warfarin users without a history of S/SE and 5.7 to 7.1 times higher in those with a history of S/SE. The incidence rate of MB was 17.2 to 21.5 per 1000 patient-years in warfarin users without a history of bleeding and 1.8 to 1.9 times higher in those with a history of bleeding. Both RRs and HRs of any, reduced, and standard doses of DOACs compared with warfarin were lower than 1.0 for both S/SE and MB in those with and without a history of these outcomes. Figure S3A shows the cumulative incidence functions of S/SE in patients receiving any dose of DOAC of any type or warfarin with or without a history of S/SE. The cumulative incidence increased rapidly once patients started oral anticoagulant treatment, particularly among those with a history of S/SE, in which approximately 5% of patients developed S/SE and required hospitalization within approximately 50 days after starting warfarin or DOACs. The cumulative incidence of MB also increased shortly after starting an oral anticoagulant, but the initial rise was modest relative to S/SE (Figure S3B). RRs and HRs for effectiveness and safety, myocardial infarction, and all-cause mortality are shown in Table S8. RRs and HRs were <1.0 for most individual outcomes with or without a history of the outcome but were approximately 1.0 for GI bleeding in patients treated with any, reduced, or standard doses of DOAC, irrespective of whether they had a history of GI bleeding. RRs and HRs were also about 1.0 for cerebral infarction, cerebral bleeding, and intracranial bleeding in patients receiving standard-dose DOACs who had a history of those outcomes. Figure 3, Table 3, and Table S8 show the HRs and 95% CIs estimated using the Cox proportional hazards model for main and individual outcomes. Figure S4A–D show HRs for main and individual outcomes following treatment with individual DOACs, which were similar to those following treatment with any DOAC (Figure 3).
 |
Table 3 Association of Any, Reduced, and Standard Doses of Any DOAC with Main Outcomes for Effectiveness and Safety Compared to Warfarin |
Figure S5 shows HRs and 95% CIs for less strictly defined outcomes in patients receiving any, reduced, or standard doses of any DOAC compared to warfarin. The HRs’ point estimates for less strictly defined outcomes were similar to those for strictly defined outcomes shown in Figure 3. However, the 95% CIs were narrower because with strictly defined outcomes, 45–57% of patients had cerebral infarction, cerebral bleeding, and intracranial bleeding, 26–39% had GI bleeding and other bleeding, and 9–19% had myocardial infarction and systemic embolism compared to those with less strict definition (Table S9). Figure S6A–H show that HRs stratified by sex or age were similar to those in the primary analysis. The only exception was patients ≥65 years old, whose MB HR was close to 1.0 with or without a history of the outcome (Figure S6F). In patients ≥75 years old, only 658 users of standard-dose DOACs were matched to warfarin users, and HRs were not shown for many individual outcomes because the number of patients with those outcomes was <5 times the number of explanatory variables (an exposure variable plus covariates with aSD>0.1) (Figure S6H). The analyses for grace periods of 15, 60, and 90 days were similar to the primary analysis using the grace period of 30 days (Figure S7). Figure S8A and B show the main outcomes calculated using four weighting methods, and the individual outcomes calculated by MW, respectively. The HRs estimated using four weighting methods were similar and generally consistent with the 1:1 matching results from the primary analyses (Figure 3). After excluding subjects with preference scores <0.3 and >0.7, 86.9% and 87.8% of users were included when warfarin use was compared to use of any and reduced doses of DOAC, respectively (Table S10). However, only 46.9% of patients were included when comparing use of warfarin to the standard dose of DOAC, indicating that the distribution of baseline characteristics in patients using the standard dose of DOAC were substantially different from those using warfarin.
Table S11 and Figure S9 show the incidence rates, RRs, and HRs of outcomes for S/SE when stratified by CHA2DS2-VASc scores. The incidence rate of S/SE for a CHA2DS2-VASc score>5 was more than ten times higher than for a CHA2DS2-VASc score of 0 or 1 in both warfarin and DOAC users. RRs and HRs were <1.0 for lower CHA2DS2-VASc scores but increased and approached 1.0 with increasing CHA2DS2-VASc scores, particularly for standard-dose DOAC users. The incidence rate of MB for a HAS-BLED score>4 was 5 to 7.5 times greater than the rate of MB for a HAS-BLED score of 0 or 1 in both warfarin and DOAC users (Table S12 and Figure S10). RRs and HRs for MB were < 1.0 for lower HAS-BLED scores but approached 1.0 with increasing HAS-BLED scores. The all-cause mortality for a CCI score >5 was more than 11 times higher than for a CCI score of 0 (Table S13 and Figure S11). RRs and HRs were approximately 0.7 regardless of the CCI score for patients receiving any, reduced, or standard doses of DOAC compared to those receiving warfarin.
Table S14A and Figure S12 show main and individual outcomes in 96,170 reduced-dose DOAC users that were directly matched to the same number of standard-dose DOAC users. After 1:1 matching, the mean patient age was 55.0 years, and 69.2% were males, for those receiving either reduced- or standard-dose DOACs (aSD<0.1 for all covariates). In patients without a history of S/SE or MB, HRs of reduced- compared to standard-dose DOACs for effectiveness and safety were slightly less than 1.0. However, for those with a history of S/SE or cerebral infarction, reduced-dose DOACs were clearly better than standard-dose DOACs (HR=0.66, 95% CI: 0.63–0.69 and HR=0.65, 95% CI: 0.62–0.68, respectively). However, in those with a history of any bleeding, the MB HR was about 1.0. The findings were similar after stratification by sex and age group (Figure S13). As for any DOAC (Table S14A and Figure S12), for individual DOACs reduced-dose was better than standard-dose for patients with a history of S/SE (HR; 0.61–0.73, Table S14B) and cerebral infarction (HR; 0.60–0.72, Table S14C), although estimates were unstable for edoxaban due to a small sample size.
Table S15A and Figure S14 show HRs and CIs for S/SE, and Table S15B shows HRs and CIs for cerebral bleeding in patients who used reduced- compared to standard-dose DOACs stratified by CHA2DS2-VASc scores. The risks of S/SE and cerebral infarction were similar between reduced- and standard-dose DOACs when the CHA2DS2-VASc score was 0 or 1, but reduced-dose DOACs were better than standard-dose DOACs (HR<1.0) when the CHA2DS2-VASc score was ≥3. Table S15C and D show HRs and CIs for S/SE and cerebral infarction in patients who used reduced- compared to standard-dose of individual DOACs divided into two groups; one with CHA2DS2-VASc score<3 and the other with CHA2DS2-VASc score≥3. The reduced-dose was better than the standard-dose regarding both S/SE (HR; 0.52–0.76) and cerebral infarction (HR; 0.52–0.76) for all individual DOACs when the CHA2DS2-VASc score was ≥3. Table S16 and Figure S15 show the HRs and CIs for the main outcome of MB in patients receiving reduced-dose DOACs compared to standard-dose DOACs stratified by HAS-BLED scores. HRs for MB were stable and about 1.0 regardless of the HAS-BLED score. Table S17A and B show the results of the first additional post-hoc study, in which the incidence rates of S/SE and cerebral infarction were highest when DOACs were started 15 to 30 days after S/SE and cerebral infarction admissions, respectively. HRs were about 0.8 and similar regardless of when DOACs were started after the last S/SE or cerebral infarction admission. Table S18A and B show the results of the second post-hoc study where the incidence rates of S/SE and cerebral infarction were similar between the three diagnosis types of NVAF with and without history of S/SE and cerebral infarction, respectively. With a history of S/SE and cerebral infarction, HRs were approximately 0.7 for all diagnosis types. Table S19A and B show the results of the third post-hoc study. The incidence rates of S/SE and cerebral infarction were of similar magnitude irrespective of the delay between the first diagnosis of NVAF and the day of starting DOACs with and without a history of S/SE and cerebral infarction, respectively. With a history of S/SE and cerebral infarction, HRs were approximately 0.7 irrespective of whether the delay was ≤30 days, 31–90 days, 91–365 days or ≥366 days.
Discussion
More than half of patients with NVAF who started DOACs in Japan between FY 2011 and FY 2015 used reduced doses. Users of standard-dose DOACs were approximately 10 years younger and more often male than users of reduced-dose DOACs or warfarin. After 1:1 matching, both reduced- and standard-dose DOAC users had decreased risks of S/SE and MB than warfarin users. These findings were consistent for individual DOACs and after stratification by sex and age group except for GI bleeding and MB in individuals ≥65 years of age. When stratified by CHA2DS2-VASc and HAS-BLED scores, RRs and HRs for both S/SE and MB were <1.0 in patients with low scores but HRs approached 1.0 for those with high CHA2DS2-VASc and HAS-BLED scores. After stratification by CCI scores, the HR of all-cause mortality was stable and about 0.7 regardless of CCI score in users of any, reduced, or standard doses of DOACs compared to users of warfarin. This was potentially the result of residual confounding because in pre-matching, the proportion of warfarin users with conditions like anemia, heart failure, and renal diseases was higher than that for reduced- and standard-dose DOAC users, and the confounding control may have been insufficient for all-cause mortality (Table S6A). Exploratory analyses suggested that the effect of reduced- and standard-dose DOACs was not substantially different except for those with a history of S/SE (particularly cerebral infarction) and CHA2DS2-VASc score ≥3, in which the effect of reduced-dose DOACs was better than standard-dose DOACs for any DOAC (Tables S14A, S15A and B) and individual DOACs (Tables S14B, S14C, S15C and D). The finding that reduced-dose DOACs were more beneficial than standard-dose DOACs in patients with a history of S/SE and cerebral infarction was consistent across individual DOACs and in stratified analysis by the period between the last day of admission due to S/SE or cerebral infarction and the day of starting DOACs (Table S17A and B); type of NVAF diagnosis (Table S18A and B); and magnitude of the delay between the first NVAF diagnosis and the day of starting DOACs (Table S19A and B).
In the current study, the proportion of patients using reduced dose DOACs who met the criteria for receiving a reduced dose was unknown because creatinine clearance and body weight values were not available in the claims data (Table S1). However, it is likely that a considerable fraction of reduced-dose DOAC users (accounting for more than half of all users) did not meet the criteria because the proportion of patients with renal disorders was <10%, and the average age of reduced-dose DOAC users was 62 years before 1:1 matching (Table S6A).
Our findings differed from those in studies from the United States (US),14–16 Europe,17–21 Israel,22 and Asia23–28 reporting the association between reduced-dose DOACs and the increased risk of S/SE. Some systematic reviews have also reported that use of reduced-dose DOACs produced less favorable outcomes than standard-dose DOACs.17,29–32 However, several reports, mainly from Asia33–46 but also from the US47–50 and Israel,51 as well as international/global studies,52,53 show that reduced-dose DOACs were not associated with an increased risk of S/SE; in some of these studies, investigators specified reduced-dose as “inappropriately reduced-dose” or “off-label underdose”.39,47–49,51,53 In a recent systematic review, Choi et al reported that reduced-dose DOACs were not associated with an increased risk of S/SE in Asians,54 and Shen et al reported the same conclusion in a systematic review that included a diverse population.55
In the current study, a direct comparison of patients receiving reduced- and standard-dose DOACs suggests that the use of reduced-dose DOACs may be beneficial to patients with a history of cerebral infarction and high CHA2DS2-VASc score (≥3), but whether this finding, obtained in post-hoc analyses is reproducible should be tested in the future. Currently, trial-approved DOAC doses or those recommended by respective country guidelines/regulations may be used as indicated in recent consensus recommendations issued by experts in Asia-Pacific regions.76,77
A strength of this study is the large number of patients extracted from the NDB Japan database. This allowed for analyses in subgroups stratified by individual DOAC, sex, and age group with and without a history of the outcome of interest and subgroups divided by CHA2DS2-VASc, HAS-BLED, and CCI scores.
Our study has several limitations. First, we have not validated the definition of NVAF used in the current study, and thus its accuracy remains unknown. The definition of NVAF based on ICD-10 codes and anticoagulants provided 94.1% of the PPV in a study conducted using a claims database in Korea.78 The PPV in the current study may be similar because the ICD-10 codes for AF and oral anticoagulant use were also included in the definition of NVAF. We used the diagnosis code for a non-AF diagnosis before starting an anticoagulant as an additional exclusion criterion (Figure 1 and Figure S1), which might improve the specificity and PPV of the NVAF definition. Similarly, we have not validated the definitions of the outcomes except for cerebrovascular disorders, myocardial infarction, and death.58–61 As a result, conservative (strict) outcome definitions (Table S4B) were used that were likely to be more specific. Another limitation of this study was that creatinine clearance and body weight information was not available; therefore, we could not identify patients who met the criteria for reduced-dose DOAC treatment. Furthermore, there was a short observation period, and the average time period obtained by dividing person-years (PY) by the number of patients (N) in Table 3 was slightly more than a year for those without a history of outcomes and less than a year for those with a history of outcomes. Lastly, this is an observational study, not a clinical trial, therefore, we cannot exclude the possibility that our findings were due to residual confounding. Future studies should determine whether the finding that reduced-dose DOACs are beneficial to patients with a history of S/SE (particularly cerebral infarction) or high CHA2DS2-VASc scores can be reproduced, using data sources that include creatinine clearance and body weight. If other studies replicate our findings, randomized clinical trials may confirm or negate the possible beneficial effect of reduced-dose DOACs, particularly in the Asian population with a history of S/SE and high CHA2DS2-VASc scores.
Conclusion
Between FY 2011 and FY 2015, the proportion of patients with NVAF who started DOACs, among all NVAF patients starting oral anticoagulants, increased from 27% to 83%. More than half of new DOAC users used reduced-dose DOACs. These patients were older and included a higher proportion of females than those using standard-dose DOACs. The effectiveness (S/SE) and safety (MB) of reduced- and standard-dose DOACs were at least as strong as for warfarin use. This is not consistent with studies conducted mainly in the US and Europe, where reduced DOAC doses were associated with an increased incidence of S/SE,14–32 but consistent with some recent studies in Asia, other countries, and international/global studies.33–55 Exploratory post-hoc analyses suggested that reduced-dose DOACs may be better than standard-dose DOACs for patients with a history of S/SE or cerebral infarction and high CHA2DS2-VASc scores (≥3). However, it may be prudent to respect recent consensus recommendations by experts in Asia-Pacific regions76,77 that trial-approved doses of DOACs or doses recommended by specific country guidelines/regulations should be used until more results become available. Physician recommendations for individual patients are also important.
Data Sharing Statement
In the guidelines for the use of NDB Japan, it is strictly prohibited to share any data except for tables and figures in published papers.
Acknowledgments
The authors would like to thank Boehringer Ingelheim for their contribution to the improvement of the study protocol prior to the data acquisition. Boehringer Ingelheim was not involved in the study for any other aspects including data analyses, interpretation of results, and manuscript preparation.
Funding
This work was supported by Boehringer Ingelheim.
Disclosure
The authors report no conflicts of interest in this work.
References
1. January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines and the heart rhythm society. Circulation. 2019;140:e125–e151. doi:10.1161/CIR.0000000000000665
2. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. doi:10.1093/eurheartj/ehaa612
3. Ono K, Iwasaki Y, Shimizu W, et al. JCS/JHRS 2020 guideline on pharmacotherapy of cardiac arrhythmias. Available from: https://www.j-circ.or.jp/cms/wp-content/uploads/2020/01/JCS2020_Ono.pdf.
4. Connolly SJ, Ezekowitz MD, Yusuf S, et al.; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. doi:10.1056/NEJMoa0905561
5. Patel MR, Mahaffey KW, Garg J, et al.; ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–891. doi:10.1056/NEJMoa1009638
6. Granger CB, Alexander JH, McMurray JJ, et al.; ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–992. doi:10.1056/NEJMoa1107039
7. Giugliano RP, Ruff CT, Braunwald E, et al.; ENGAGE AF-TIMI 48 Investigators. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–2104. doi:10.1056/NEJMoa1310907
8. Tanigawa T, Kaneko M, Hashizume K, et al. Model-based dose selection for Phase III rivaroxaban study in Japanese patients with non-valvular atrial fibrillation. Drug Metab Pharmacokinet. 2013;28(1):59–70. doi:10.2133/dmpk.dmpk-12-rg-034
9. Chao TF, Hong KS, Lee BC, et al. Factors associated with the dosing of edoxaban for stroke prevention in patients with atrial fibrillation from South Korea and Taiwan: 1-year data from the Global ETNA-AF program. J Chin Med Assoc. 2021;84:485–490. doi:10.1097/JCMA.0000000000000516
10. Shen NN, Zhang C, Hang Y, et al. Real-world prevalence of direct oral anticoagulant off-label doses in atrial fibrillation: an epidemiological meta-analysis. Front Pharmacol. 2021;12:581293. doi:10.3389/fphar.2021.581293
11. Stoll S, Macha K, Marsch A, et al. Ischemic stroke and dose adjustment of oral Factor Xa inhibitors in patients with atrial fibrillation. J Neurol. 2020;267:2007–2012. doi:10.1007/s00415-020-09795-3
12. Ueda A, Toki S, Kitayama C, Akazawa M. Reduction in the doses of direct oral anticoagulants and risk of ischemic stroke events: a hospital survey. Biol Pharm Bull. 2020;43:1135–1140. doi:10.1248/bpb.b19-00798
13. Eschler CM, Woitok BK, Func GC, et al. Oral anticoagulation in patients in the emergency department: high rates of off-label doses, no difference in bleeding rates. Am J Med. 2020;133:599–604. doi:10.1016/j.amjmed.2019.09.026
14. Graham DJ, Reichman ME, Wernecke M, et al. Cardiovascular, bleeding, and mortality risks in elderly Medicare patients treated with dabigatran or warfarin for nonvalvular atrial fibrillation. Circulation. 2015;131(2):157–164. doi:10.1161/CIRCULATIONAHA.114.012061
15. Yao X, Shah ND, Sangaralingham LR, Gersh BJ, Noseworthy PA. Non-vitamin K antagonist oral anticoagulant dosing in patients with atrial fibrillation and renal dysfunction. J Am Coll Cardiol. 2017;69(23):2779–2790. doi:10.1016/j.jacc.2017.03.600
16. Hernandez I, Zhang Y. Comparing stroke and bleeding with rivaroxaban and dabigatran in atrial fibrillation: analysis of the US medicare part D data. Am J Cardiovasc Drugs. 2017;17(1):37–47. doi:10.1007/s40256-016-0189-9
17. Beyer-Westendorf J, Fay M, Amara W. The importance of appropriate dosing of nonvitamin K antagonist oral anticoagulants for stroke prevention in patients with atrial fibrillation. TH Open. 2021;5(3):e353–e362. doi:10.1055/s-0041-1731777
18. Hecker J, Marten S, Keller L, et al. Effectiveness and safety of rivaroxaban therapy in daily-care patients with atrial fibrillation: results from the Dresden NOAC registry. Thromb Haemost. 2016;115(5):939–949. doi:10.1160/TH15-10-0840
19. Nielsen PB, Skjøth F, Søgaard M, Kjældgaard JN, Lip GYH, Larsen TB. Effectiveness and safety of reduced dose non-vitamin K antagonist oral anticoagulants and warfarin in patients with atrial fibrillation: propensity weighted nationwide cohort study. BMJ. 2017;356:j510. doi:10.1136/bmj.j510
20. Helmert S, Marten S, Mizera H, et al. Effectiveness and safety of apixaban therapy in daily-care patients with atrial fibrillation: results from the Dresden NOAC registry. J Thromb Thrombolysis. 2017;44(2):169–178. doi:10.1007/s11239-017-1519-8
21. Godino C, Bodega F, Melillo F, et al. Inappropriate dose of nonvitamin-K antagonist oral anticoagulants: prevalence and impact on clinical outcome in patients with nonvalvular atrial fibrillation. J Cardiovasc Med. 2020;21(10):751–758. doi:10.2459/JCM.0000000000001043
22. Arbel R, Sergienko R, Hammerman A, et al. Effectiveness and safety of off-label dose-reduced direct oral anticoagulants in atrial fibrillation. Am J Med. 2019;132:847–855. doi:10.1016/j.amjmed.2019.01.025
23. Chan YH, Chao TF, Chen SW, et al. Off-label dosing of non-vitamin K antagonist oral anticoagulants and clinical outcomes in Asian patients with atrial fibrillation. Heart Rhythm. 2020;17:2102–2110. doi:10.1016/j.hrthm.2020.07.022.Yu
24. Lee KN, Choi JI, Boo KY, et al. Effectiveness and safety of off-label dosing of non-vitamin K antagonist anticoagulant for atrial fibrillation in Asian patients. Sci Rep. 2020;10:1801. doi:10.1038/s41598-020-58665-5
25. Cheng WH, Chao TF, Lin YJ, et al. Low-dose rivaroxaban and risks of adverse events in patients with atrial fibrillation. Stroke. 2019;50:2574–2577. doi:10.1161/STROKEAHA.119.025623
26. Ikeda T, Ogawa S, Kitazono T, et al. Outcomes associated with under‑dosing of rivaroxaban for management of non‑valvular atrial fibrillation in real‑world Japanese clinical settings. J Thromb Thrombolysis. 2019;48:653–660. doi:10.1007/s11239-019-01934-6
27. Shinoda N, Mori M, Tamura S, Korosue K, Kose S, Kohmura E. Risk of recurrent ischemic stroke with unintended low-dose oral anticoagulant therapy and optimal timing of review. J Stroke Cerebrovasc Dis. 2018;27:1546–1551. doi:10.1016/j.jstrokecerebrovasdis.2018.01.002
28. Lee SR, Choi EK, Park SH, et al. Off-label underdosed apixaban use in Asian patients with non-valvular atrial fibrillation. Eur Heart J Cardiovasc Pharmacother. 2021;7(5):415–423. doi:10.1093/ehjcvp/pvab004
29. Santos J, António N, Rocha M, Fortuna A. Impact of direct oral anticoagulant off-label doses on clinical outcomes of atrial fibrillation patients: a systematic review. Br J Clin Pharmacol. 2020;86:533–547. doi:10.1111/bcp.14127
30. Liu X, Huang M, Ye C, Xiao X, Yan C. Effect of non-recommended doses versus recommended doses of direct oral anticoagulants in atrial fibrillation patients: a meta-analysis. Clin Cardiol. 2021;44:472–480. doi:10.1002/clc.23586
31. Zhang XL, Zhang XW, Wang TY, et al. Off-label under- and overdosing of direct oral anticoagulants in patients with atrial fibrillation: a meta-analysis. Circ Cardiovasc Qual Outcomes. 2021;14(12):e007971. doi:10.1161/CIRCOUTCOMES.121.007971
32. Kido K, Shimizu M, Shiga T, Hashiguchi M. Meta-analysis comparing inappropriately low dose versus standard dose of direct oral anticoagulants in patients with atrial fibrillation. J Am Pharma Assoc. 2022;62:487–495. doi:10.1016/j.japh.2021.10.027
33. Umei M, Kishi M, Sato T, et al. Indications for suboptimal low-dose direct oral anticoagulants for non-valvular atrial fibrillation patients. J Arrhythm. 2017;33:475–482. doi:10.1016/j.joa.2017.05.008Citations:13
34. Yamaji H, Murakami T, Hina K, et al. Safety and efficacy of underdosing non-vitamin K antagonist oral anticoagulants in patients undergoing catheter ablation for atrial fibrillation. J Cardiovasc Pharmacol. 2017;69(2):118–126. doi:10.1097/FJC.0000000000000448
35. Sato T, Aizawa Y, Fuse K, et al. The comparison of inappropriate-low-doses use among 4 direct oral anticoagulants in patients with atrial fibrillation: from the database of a single-center registry. J Stroke Cerebrovasc Dis. 2018;27:3280–3288. doi:10.1016/j.jstrokecerebrovasdis.2018.07.028
36. Cho MS, Yun JE, Park JJ, et al. Pattern and impact of off-label underdosing of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation who are indicated for standard dosing. Am J Cardiol. 2020;125(9):1332–1338. doi:10.1016/j.amjcard.2020.01.044.Yu
37. Kato Y, Hayashi T, Tanahashi N, Takao M. The dose of direct oral anticoagulants and stroke severity in patients with acute ischemic stroke and nonvalvular atrial fibrillation. J Stroke Cerebrovasc Dis. 2018;27(6):1490–1496. doi:10.1016/j.jstrokecerebrovasdis.2017.12.038
38. Lin YC, Chien SC, Hsieh YC, et al. Effectiveness and safety of standard- and low-dose rivaroxaban in Asians with atrial fibrillation. J Am Coll Cardiol. 2018;72(5):477–485. doi:10.1016/j.jacc.2018.04.084
39. Murata N, Okumura Y, Yokoyama K, et al. Clinical outcomes of off-label dosing of direct oral anticoagulant therapy among Japanese patients with atrial fibrillation identified from the SAKURA AF Registry. Circ J. 2019;83(4):727–735. doi:10.1253/circj.CJ-18-0991
40. Suwa M, Morii I, Kino M, et al. Rivaroxaban or apixaban for non-valvular atrial fibrillation - efficacy and safety of off-label under-dosing: according to plasma concentration. Circ J. 2019;83:991–999. doi:10.1253/circj.CJ-18-1282
41. Yu HT, Yang PS, Jang E, et al. Label adherence of direct oral anticoagulants dosing and clinical outcomes in patients with atrial fibrillation. J Am Heart Assoc. 2020;9(12):e014177. doi:10.1161/JAHA.119.014177
42. Yagi N, Suzuki S, Arita T, et al. Creatinine clearance and inappropriate dose of rivaroxaban in Japanese patients with non‑valvular atrial fibrillation. Heart Vessels. 2020;35:110–117. doi:10.1007/s00380-019-01457-3
43. Chen IC, Chang WT, Hsu PC, et al. Off-label reduced-dose apixaban does not reduce hemorrhagic risk in Taiwanese patients with nonvalvular atrial fibrillation: a retrospective, observational study. Medicine. 2021;100(23):e26272. doi:10.1097/MD.0000000000026272
44. Kadosaka T, Nagai T, Suzuki S, et al. Association of low body weight with clinical outcomes in elderly atrial fibrillation patients receiving apixaban—J-ELD AF registry subanalysis. Cardiovasc Drugs Ther. 2021. doi:10.1007/s10557-021-07180-4
45. Kobayashi T, Sotomi Y, Hirata A, Sakata Y, Hirayama A, Higuchi Y. Impact of direct oral anticoagulant off-label reduced dose in combination with antiplatelet agents on clinical outcome - propensity score-matching analysis from the DIRECT real-world non-valvular atrial fibrillation registry. Circ Rep. 2020;2(6):289–296. doi:10.1253/circrep.CR-20-0026
46. Wakamatsu Y, Nagashima K, Watanabe R, et al. Clinical outcomes of off-label underdosing of direct oral anticoagulants after ablation for atrial fibrillation: subanalysis of the AF frontier ablation registry. Int Heart J. 2020;61:1165–1173. doi:10.1536/ihj.20-335
47. Steinberg BA, Peter Shrader P, Pieper K, et al. Frequency and outcomes of reduced dose non–vitamin K antagonist anticoagulants: results from ORBIT-AF II (the outcomes registry for better informed treatment of atrial fibrillation II). J Am Heart Assoc. 2018;7:e007633. doi:10.1161/JAHA.117.007633
48. Briasoulis A, Gao Y, Inampudi C, et al. Characteristics and outcomes in patients with atrial fibrillation receiving direct oral anticoagulants in off-label doses. BMC Cardiovasc Disord. 2020;20:42. doi:10.1186/s12872-020-01340-4
49. Ashraf H, Agasthi P, Shanbhag A, et al. Long-term clinical outcomes of underdosed direct oral anticoagulants in patients with atrial fibrillation and atrial flutter. Am J Med. 2021;134(6):788–796. doi:10.1016/j.amjmed.2020.12.022
50. Sugrue A, Sanborn D, Amin M, et al. Inappropriate dosing of direct oral anticoagulants in patients with atrial fibrillation. Am J Card. 2021;144:52–59. doi:10.1016/j.amjcard.2020.12.062
51. Salameh M, Gronich N, Stein N, et al. Stroke and bleeding risks in patients with atrial fibrillation treated with reduced apixaban dose: a real-life study. Clin Pharmacol Ther. 2020;108(6):1265–1273. doi:10.1002/cpt.1952
52. Amarenco P, Haas S, Hess S, et al. Outcomes associated with non-recommended dosing of rivaroxaban: results from the XANTUS study. Eur Heart J Cardiovasc Pharmacother. 2019;5(2):70–79. doi:10.1093/ehjcvp/pvy041
53. Camm AJ, Cools F, Virdone S, et al. Mortality in patients with atrial fibrillation receiving nonrecommended doses of direct oral anticoagulants. J Am Coll Cardiol. 2020;76(12):1425–1436. doi:10.1016/j.jacc.2020.07.045
54. Choi J, No JE, Lee JY, et al. Efficacy and safety of clinically driven low-dose treatment with direct oral anticoagulants in Asians with atrial fibrillation: asystematic review and meta-analysis. Cardiovasc Drugs Ther. 2021. doi:10.1007/s10557-021-07171-5
55. Shen NN, Zhang C, Wang N, Wang JL, Gu ZC, Han H. Effectiveness and safety of under or over-dosing of direct oral anticoagulants in atrial fibrillation: a systematic review and meta-analysis of 148909 patients from 10 real-world studies. Front Pharmacol. 2021;12:645479. doi:10.3389/fphar.2021.645479
56. Kubota K, Kamijima Y, Sato T, et al. Epidemiology of psoriasis and palmoplantar pustulosis: a nationwide study using the Japanese national claims database. BMJ Open. 2015;5(1):e006450. doi:10.1136/bmjopen-2014-006450
57. Parsons LS. Using SAS® software to perform a case-control match on propensity score in an observational study. Available from: https://support.sas.com/resources/papers/proceedings/proceedings/sugi25/25/po/25p225.pdf.
58. Ando T, Ooba N, Mochizuki M, et al. Positive predictive value of ICD-10 codes for acute myocardial infarction in Japan: a validation study at a single center. BMC Health Serv Res. 2018;18(1):895. doi:10.1186/s12913-018-3727-0
59. Ooba N, Setoguchi S, Ando T. Claims-based definition of death in Japanese claims database: validity and implications. PLoS One. 2013;8:e66116. doi:10.1371/journal.pone.0066116
60. Ono Y, Taneda Y, Takeshima T, Iwasaki K, Yasui A. Validity of claims diagnosis codes for cardiovascular diseases in diabetes patients in Japanese administrative database. Clin Epidemiol. 2020;12:367–375. doi:10.2147/CLEP.S245555
61. Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol. 2017;27(10):476–482. doi:10.1016/j.je.2016.09.009
62. Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38:1228–1234. doi:10.1080/03610910902859574
63. Gray RJ. A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat. 1988;16:1141–1154. doi:10.1214/aos/1176350951
64. Austin PC, Lee DS, Fine JP. Introduction to the analysis of survival data in the presence of competing risks. Circulation. 2016;133(6):601–609. doi:10.1161/CIRCULATIONAHA.115.017719
65. Walker A, Patrick A, Lauer M, et al. A tool for assessing the feasibility of comparative effectiveness research. Comparat Effective Res. 2013;3:11–20. doi:10.2147/CER.S40357
66. Hernán MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11:561–570. doi:10.1097/00001648-200009000-00012
67. Li L, Greene T. A weighting analogue to pair matching in propensity score analysis. Int J Biostat. 2013;9(2):215–234. doi:10.1515/ijb-2012-0030
68. Li F, Morgan KL, Zaslavsky AM. Balancing covariates via propensity score weighting. J Am Stat Assoc. 2018;113:3390–3400. doi:10.1080/01621459.2016.1260466
69. Desai RJ, Rothman KJ, Bateman BT, Hernandez-Diaz S, Huybrechts KH. A propensity-score-based fine stratification approach for confounding adjustment when exposure is infrequent. Epidemiology. 2017;28(2):249–257. doi:10.1097/EDE.0000000000000595
70. Lin KJ, Jin Y, Gagne J, et al. Longitudinal data discontinuity in electronic health records and consequences for medication effectiveness studies. Clin Pharmacol Ther. 2022;111:243–251. doi:10.1002/cpt.2400
71. Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165(6):710–718. doi:10.1093/aje/kwk052
72. Olsen JB, Torp-Pedersen C, Hansen ML, Lip GYH. The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0–1: a nationwide cohort study. Thromb Haemost. 2012;107(6):1172–1179. doi:10.1160/TH12-03-0175
73. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GYH. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093–1100. doi:10.1378/chest.10-0134
74. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–1294. doi:10.1016/j.jclinepi.2004.03.012
75. Webster-Clark M, Huang TY, Hou L, Toh S. Translating claims-based CHA 2 DS 2 -VaSc and HAS-BLED to ICD-10-CM: impacts of mapping strategies. Pharmacoepidemiol Drug Saf. 2020;29(4):409–418. doi:10.1002/pds.4973
76. Chiang CE, Okumura K, Zhang S, et al. 2017 consensus of the Asia Pacific Heart Rhythm Society on stroke prevention in atrial fibrillation. J Arrhythm. 2017;33:345–367. doi:10.1016/j.joa.2017.05.004
77. Chong DTT, Andreotti F, Andreotti P, et al. Direct oral anticoagulants in Asian patients with atrial fibrillation: consensus recommendations by the Asian Pacific society of cardiology on strategies for thrombotic and bleeding risk management. Eur Cardiol. 2021;16:e23. doi:10.15420/ecr.2020.43
78. Kim TH, Yang PS, Uhm JS, et al. CHA2DS2-VASc Score (congestive heart failure, hypertension, Age ≥75 (doubled), diabetes mellitus, prior stroke or transient ischemic attack (doubled), vascular disease, age 65–74, female) for stroke in Asian patients with atrial fibrillation: a Korean nationwide sample cohort study. Stroke. 2017;48(6):1524–1530. doi:10.1161/STROKEAHA.117.016926
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.