Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 15
Effectiveness and Economic Evaluation of Hospital-Outreach Pulmonary Rehabilitation for Patients with Chronic Obstructive Pulmonary Disease
Authors Zhang A, Wang L, Long L, Yan J, Liu C, Zhu S, Wang X
Received 18 February 2020
Accepted for publication 27 March 2020
Published 15 May 2020 Volume 2020:15 Pages 1071—1083
DOI https://doi.org/10.2147/COPD.S239841
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Chunxue Bai
Aidi Zhang,1 Lianhong Wang,2 Lu Long,1 Jin Yan,1,3 Chun Liu,4 Sucui Zhu,1 Xiaowan Wang5
1Nursing Department, Third Xiangya Hospital of Central South University, Changsha 410013, People’s Republic of China; 2The First Affiliated Hospital of Zunyi Medical University, Zunyi 563003, People’s Republic of China; 3Xiang Ya Nursing School of Central South University, Changsha 410013, People’s Republic of China; 4Respiratory Department, Third Xiangya Hospital of Central South University, Changsha 410013, People’s Republic of China; 5Center for Health Policy and Management, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100730, People’s Republic of China
Correspondence: Jin Yan Email [email protected]
Objective: Hospital-outreach pulmonary rehabilitation (PR) can improve health status and reduce health-care utilization by patients with chronic obstructive pulmonary disease (COPD). However, its long-term effects and costs versus benefits are still not clear. This study was conducted to develop, deliver, and evaluate the effects and monetary savings of a hospital-outreach PR program for patients with COPD.
Methods: A randomized controlled trial was conducted. Patients with COPD (n=208) were randomly assigned to the hospital-outreach PR program (treatment) or treatment as usual (control). The treatment group received a 3-month intensive intervention, including supervised physical exercise, smoking cessation, self-management education, and psychosocial support, followed by long-term access to a nurse through telephone follow-up and home visits up to 24 months. The control group received routine care, including discharge education and a self-management education brochure. Main outcomes were collected at 3, 6, 12, and 24 -months postrandomization. Primary outcomes included health-care utilization (ie, readmission rates, times, and days, and emergency department visits) and medical costs. Secondary outcomes included lung function (ie, FEV1, FEV1% predicted, FVC), dyspnea (mMCR), exercise capacity (6MWD), impact on quality of life (CAT), and self-management (CSMS).
Results: At the end of 24 months, 85 (81.7%) in the treatment group and 89 (85.6%) in the control group had completed the whole program. Compared with the control group, patients in the treatment group had lower readmission rates, times, and days at 6 and 12 months and during 12– 24 months. Regarding costs during the 2 years, the program achieved CN¥ 3,655.94 medical savings per patient per year, and every ¥ 1 spent on the program led to ¥ 3.29 insavings. Patients in the treatment group achieved improvements in FEV1, FEV1% predicted, exercise capacity, and self-management. It also achieved relief of dyspnea symptoms and improvement in COPD’s impact on quality of life.
Conclusion: The hospital-outreach PR program for patients with COPD achieved reductions in health-care utilization, monetary savings, and improvements in patient health outcomes. The effects of the program were sustained for at least 2 years.
Trial Registration: This trial was registered at the Chinese Clinical Trial Registry (ChiCTR-TRC-14005108).
Keywords: chronic obstructive pulmonary disease, savings, effects, hospital-outreach intervention, pulmonary rehabilitation
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive and debilitating respiratory condition that leads to significant burden. It is the only chronic disease with continuously increasing morbidity and mortality rates.1 The World Health Organization predicts COPD to be the third-leading cause of death worldwide by 2030.2 China has the largest population of patients with COPD in the world: around 99 million people, with prevalence of 8.6%. It accounts for >0.9 million death every year.3,4
Prevention of readmission is critical for patients with COPD. Around one in five patients with COPD discharged from hospital are rehospitalized within 30 days5–7 and around a third readmitted within 90 days after discharge. Admission costs are major drivers of medical costs, accounting for 40%–70% of the total.8 In China, the median annual direct cost of patients with COPD accounts for about a third of annual income.9,10 Readmission of a patient means exacerbation of his/her COPD, which is a signal of the beginning of the terminal phase of illness and is associated with a significant decline in quality of life and chances of survival.11
Hospital-outreach intervention is an effective approach to prevent readmission of patients with chronic diseases.12–14 It is the outreach of health-care services from hospital to community and family, with the formation of integration among hospital, community, and family making services continuous among different health-care settings and keeping consistent with the patient’s needs.15,16 Outreach services take various and flexible approaches, such as telephone follow-up, and home visits shortly after discharge,17,18 health education,16,19 support for self-management,20,21 training in exacerbation monitoring and recognition,19 and improvement in access to health-care services.12,22–24 It has been found that hospital-outreach intervention achieves chronic symptom relief, improvement in self-management, and decreased readmissions and emergency department (ED) visits.
Pulmonary rehabilitation (PR) is recommended for most patients with COPD. It benefits patients with different COPD severity, especially those with moderate–severe COPD.11 PR comes under the concept of integrated care, constructed and implemented by multidisciplinary team members, and highlights the importance of behavior changes.22,25 A PR program includes exercise as a key component, and includes patient assessments, education, psychological support, and nutritional counseling.23,24 PR has robust effectiveness in improving health-related quality of life and enhancing exercise capacity.25,26
Although China has a large population of patients with COPD, patients receive health care mostly in the hospital, but with a lack of follow-up services after discharge. Currently existing hospital-outreach intervention typically includes telephone follow-up and home visits.27,28 Most program focus only on medication taking, nutrition management, and health education. It is of great necessity to develop and implement a hospital-outreach model and content.
In addition, despite the strong recommendation of hospital-outreach and PR programs, there are still issues that need to be resolved. First, previous studies have not offered much economic evaluation of hospital-outreach intervention or PR. Second, most studies have focused on the effects of short-term programs (eg, 6–8 weeks or 3 months), and the long-term effects of programs remain unclear. The objectives of this study were to develop, deliver, and evaluate of effects and medical monetary savings of a hospital-outreach PR program among patients with COPD after discharge from hospital to home.
Methods
Study Design and Setting
A randomized controlled trial was conducted. Participants (n=208) were recruited from a tertiary hospital in Zunyi, China. This hospital has a capacity >3,000 beds. It provides medical services to >6 million people residing in urban and rural areas.
Participants
Inclusion and Exclusion Criteria
Inclusion criteria were age ≥40 years old, diagnosis of COPD according to GOLD guideline (FEV1/FVC <0.7 after use of bronchodilator), including COPD stage 2 (moderate, FEV1 ≤50%–80% predicted), 3 (severe, FEV1 ≤30%–<50% predicted), or 4 (very severe, FEV1 <30% predicted),hospitalized at least once due to COPD exacerbation during the last 12 months, and not intending to move to another city within the next 2 years. Exclusion criteria were unable to provide accurate information or follow instructions, unable to walk even during periods of COPD, and currently involved in another program.
Recruitment
Patients were recruited between August 2014 and January 2016. Potentially eligible patients were identified through review of electronic medical records in the hospital information system. Physicians in the respiratory ward were also asked to identify COPD patients. All potentially eligible patients were then asked about their willingness to take part. Thereafter, the program’s aims, interventions, and significance were explained to patients who had expressed interest in participating. Once patient had been identified as fulfilling the inclusion criteria, written informed consent was signed and baseline data collected.
Randomization and Masking
Block randomization was used. Subjects were randomized after consent and collection of baseline data. Every two patients with the same level of COPD severity were allocated into one block according to their admission dates. In each block, the two patients were further allocated into treatment and control groups randomly based on allocation sequence. The sequence was generated by the statistical staff and released to the interventionist on a case-by-case basis, so recruitment staff had no access to the randomization. Patients were informed of the results of randomization in person or by phone after discharge. The intervention schedule was explained to patients and any additional questions answered.
This was a single-blind trial. Given the nature of the intervention, blinding the subjects was not feasible, and the interventionist would also know that those contacted were in the intervention arm. The statistician was blinded to individual results during the trial, and the allocation-to-trial-arm coding was not revealed until the data set had been sealed. For outcome assessment, the assessor was also blinded to subject allocation. The study was approved by the Institutional Review Board of the Third Xiangya Hospital of Central South University (2014/S159) and the Affiliated Hospital of Zunyi Medical College (2014/s14). This trial was conducted in accordance with the Declaration of Helsinki.
Sample Size
Sample size was calculated by power analysis with NCSS PASS software. One intervention group and one control group of equal size and two-tailed hypothesis testing was assumed. The power was set >0.8, with α=0.05. According to the literature review, self-reported health status is independently associated with COPD hospitalizations.29 Patient’s self-reported health status as fair/poor had deleterious effect (OR 1.57, 95% CI 1.10–2.23). For patients with no hospitalization in the previous 12 months, the proportion reporting health status as fair/poor was 10.8%, and for patients with at least one hospitalization, the proportion reporting health status as fair/poor was 26.7%.29 The calculated sample size was 92 for each group. Considering an attrition rate of 20%, the final sample size decided upon was 220.
Procedures
Hospital-Outreach Pulmonary Rehabilitation
The program was developed under the combination framework of PR and hospital-outreach intervention. Firstly, a literature review was conducted according to the rationale of GOLD 2013, other guidelines, and related clinical trials,30–36 and four main elements of the program were exercise, smoking cessation, self-management training, and psychosocial support. Secondly, an expert panel (13 professionals, including nurses with hospital-outreach intervention experience, respiratory physicians, rehabilitation physicians, and nutritionists) consultation was conducted for details of the protocol. Delivery of the program included two phases, as follows.
Firstly, a 3-month intensive intervention was conducted at the rehabilitation center in the hospital. This consisted of four main components. Details of the intervention (content, frequency, and interventionist) are presented in Table 1. The first comprised supervised physical exercise, including upper-limb strength training, lower-limb endurance training, and modified six-form tai chi. The modified tai chi was simplified from the traditional 24-form tai chi. The six-form version not only retains the essence of “breathing control” of traditional tai chi but also fully exercised balance and flexibility of the body. It is also simple and suitable for patients to grasp and exercise at home. Effects of this modified tai chi among patients with COPD have been proved.37 Exercise was supervised by a physiotherapist, tai chi mentor, and respiratory nurse, and included training in using equipment, grasping tai chi, and safety monitoring. During each exercise, participants' heart rate, SpO2, and symptoms of dyspnea were monitored. Oxygen supplementation was provided if SpO2 went <90%, and exercise would be stopped immediately if there were any chest pain, cardiac arrhythmia, dizziness, or nausea. The second component was smoking-cessation intervention for current smokers. To assess the degree of tobacco dependence of smokers, the Fagerström Test for Nicotine Dependence was used. Interventions combined group sessions of cessation education with individualized counseling. Motivation interviews and smoking-cessation drug-use guidance were used for individualized counseling for patients with strong tobacco dependence. The third component comprised self-management education, implemented by multidisciplinary professionals with group sessions and individualized counseling, and the fourth psychosocial support sessions, with group activities to promote peer communication, and coping strategies.
 |
Table 1 Contents of the 3-Month Intensive Intervention |
After the intensive intervention, long-term follow-up was provided by a respiratory nurse. Its rationale was based on hospital-outreach intervention programs that aim at realization of continuous care among hospital, community, and home. Each patient received an individualized home-exercise prescription. Although home exercise was not supervised by professionals, each patient got an exercise diary to record daily exercise, including patterns, length of time, and symptoms during exercise. Periodical telephone follow-up (once every 1–2 weeks) and home visits (once every 1–3 months) was provided. During every telephone or home-visit follow-up, home-exercise adherence, symptom changes, medication adherence, and smoking adherence were recorded by the nurse. Instructions were given to the patient based on the diaries and records, and reminders of necessary outpatient follow-up were given to patients who may suffer deterioration of COPD or need medication prescription. For follow-up frequency, previous studies and health status were taken into consideration. If telephone follow-up showed the patient’s exercise or medication adherence was not ideal or his/her health status was not good, home-visiting frequency would be increased. Follow-up was aimed at permanent access to a nurse. For this study, program completion was defined as completion of the 3-month intensive intervention and completing follow-up for 24 months after allocation.
Treatment as Usual
Patients in the control group received usual care: discharge education about self-management, exercise training, medication, and seeking health care when necessary. Each patient in this group got a pamphlet addressing self-management of COPD, including symptom recognization, smoking cessation, physical exercise, medication use, oxygen therapy, and nutrition. Contact information was printed in the pamphlet for a health-counseling service. Besides the intervention and usual care, both groups received prescriptions from physicians according to individual disease status.
Outcome Measures
Outcome measures included patient health-care utilization, medical costs, and health outcomes. Participants were assessed at five time points: baseline (before randomization) and at 3, 6, 12, 24 months postrandomization. The primary outcomes was health-care utilization, costs which were collected through the hospital information system, follow-up records, and patients’ reports. Records and recipients were used for verification. Although this may not be the perfect method, we did our best to ensure cost information was accurate. Health-care utilization included readmission rates, times, and days and ED-visit times. For economic evaluations, medical costs, including patients' out-of-pocket costs and those paid by health-service reimbursement, were assessed as accumulation of inpatient costs, ED-visit costs, and outpatient costs (ie, outpatient visitcosts and medication costs). Chinese yuan were converted into US dollars for better comparison with other studies. Collection of medical costs was from 2014 to 2018, so the currency exchange rate was based on the average exchange rate of those 5 years.38 The rates were from the National Bureau of Statistics of China . (US$1 = CN¥6.48) Program intervention costs included intensive intervention costs and follow-up costs. Details of intervention-cost elements and unit costs are displayed in Table 2.
 |
Table 2 Unit Cost Schema for Hospital-Outreach PR Intervention |
Secondary outcomes were as follows. Lung-function indicators — forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), and predicted percentage of FEV1 — were calculated. Indicators were measured by spirometry.39,40 Symptoms of dyspnea were measured with the modified Medical Research Council (mMRC) dyspnea scale.41 This has a range of 0–4, with higher scores representing worse symptoms. Exercise capacity was assessed by 6-minute walking distance. This test measures the distance a patient can walk quickly on a flat, hard surface in 6 minutes. Participants were given two chances at each assessment, and the longer distance was recorded. Quality of life was measured with the COPD Assessment Test.42 This has a range of 0–40, with higher scores indicating more negative well-being. Self-management was measured with the COPD Self-Management Scale developed by Zhang et al.43 This comprises five dimensions: symptom management, daily life management, emotion management, information management, and self-efficacy. It has a range of 51–255, with higher scores indicating higher levels of self-management.
Statistical Analysis
For description of demographic characteristics, means ± SD/medians (IQR), frequencies, and percentages were used. For equivalence between two groups at baseline, Student’s t-test, Wilcoxon’s rank-sum test, or ANOVA were used for continuous variables and χ2 for categorical variables. To examine differences in health-care utilization, medical costs, and health outcomes between the groups for readmission rates, χ2 was used. For other results, a generalized estimated equation was used for comparisons between the groups at different time points and periods. p<0.05 was considered statistically significant. Net benefits like medical monetary savings, reductions in health-care utilization, can be expressed thus: γit=β0+β1I+β2T+β3IT+ε, where γ is net benefit and I intervention: I=0 means without intervention and I=1 with intervention. T stands for before/after intervention: T=0 means before intervention and T=1 after intervention. Net benefit (β3: interaction coefficient of group and time in the generalized estimated equation) is calculated in Table 3.
 |
Table 3 Calculation of the net benefits |
Results
Participants
At the end of the second year, among the 208 participants, 85 (81.7%) participants in the treatment group and 89 (85.6%) in the control group had completed the program (Figure 1). Participants’ mean age was 65.93±7.31 years, with mean length of COPD diagnosis 7.21±4.65 years. Baseline characteristics of the two groups are presented in Table 4 (health-care utilization and costs stand for accumulative utilization and costs during the last 12 months before randomization). All group characteristics, except for ED visit costs, reached equivalence. Medication taking for both groups at baseline are displayed in Table 5. No significant differences were found between the groups. During the intensive intervention period, participant attendance for exercise was 20.72±8.07 and mean completion of education sessions 3.78±1.61. Time of telephone follow-up was 21.06±2.78 and that of home visits 4.64±3.04.
 |
Table 4 Baseline Characteristics of Participants (n=174) |
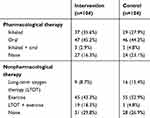 |
Table 5 Medication-Taking Comparisons Between the Groups |
 |
Figure 1 Participant flowchart. |
Effects on Health-Care Utilization
Compared with the control group, lower admission rates were found in the treatment group at 6 (36.5% vs 53.9%, p=0.021), 12 (55.3% vs 80.9%, p<0.001), and 12–24 months (51.8% vs 77.5%, p<0.001; Table 6). No significant group differences were found at 3 months (11.8% vs 20.2%, p=0.129). For readmission times and days, similar trends were found, with lower times and days at 6, 12, and 12–24 months, with no statistical difference at 3 months (Table 6). Table 8 shows reductions in health-care utilization between the groups during different periods. During the first year, compared with the control group, reduction in readmission time was 0.61 (95% CI −1.03 to −0.18), reduction in readmission days 7.21 (95% CI −11.5 to −2.92), and reduction in ED-visit time 0.81 (95% CI −1.33 to −0.28). During the second year, reductions in these three indicators were 0.65 (95% CI −1.07 to −0.23), 6.56 (95% CI −11.20 to −1.93), and 0.55 (95% CI −1.15 to 0.04), respectively. During the first 2 years, reductions in the three indicators per patient per year were 0.63 (95% CI −0.97 to −0.28), 6.97 (95% CI −10.61 to −0.28), and 0.68 (95% CI −1.17 to −0.19), respectively.
 |
Table 6 Health-Care Utilization of Patients Participating in Hospital-Outreach PR Versus Usual Care (n=174) |
 |
Table 7 Costs of Different Groups at Different Times (n=174) |
 |
Table 8 Changes to Health-Care Utilization and Costs in Hospital-Outreach PR Program Compared with Control Group (n=174) |
Monetary Savings of Hospital-Outreach PR Program
Table 7 shows that total medical costs of the treatment group were lower than the control group: first year — ¥10,370.00/$1,601.17 (IQR ¥2,354.70–¥27,410.50/$363.58–$4,232.30) vs ¥14,736.51/$2,275.38 (IQR ¥10,837.20–¥27,410.50/$1,673.31–$4,232.30), p=0.001; second year — ¥8,049.00/$1,242.80 (IQR ¥2,669.00–¥16,595.00/$412.11–$2,562.34) vs ¥12,941.00/$1,998.15 (IQR ¥8,159.95–¥17,834.92/$1,259.93–$2,753.79), p=0.020.
Table 8 shows medical monetary savings during different periods between the groups. During the first year, compared with the control group, the treatment group achieved savings of ¥4,927.94/$760.90 (95% CI −9,265.93 to −589.95) per patient per year. During the second year, savings were ¥1,418.05/$218.95 (95% CI −5,297.64, to 2,936.11). For the first 2 years, the program achieved ¥3,655.94/$564.49 (95% CI −7,462.39 to 150.50) savings per patient per year.
The ratios are based on savings/reductions in health-care utilization and intervention costs, savings for every ¥1 spent on the program, and the amount of money spent on the program to a achieve one-unit decrease inhealth-care utilization. Individualized intervention costs during the first year were ¥1,820.65/$281.12 (95% CI ¥1,745.45–¥1,895.84) per patient per year, and every ¥1 spent on the program achieved ¥2.71/$0.42 savings. Intervention costs during the second year were ¥398.60/$61.55 (95% CI ¥346.34–¥450.87), and every ¥1 spent on the program led to ¥3.56 savings. During the first 2 years, intervention costs were ¥1,109.63/$171.33 (95% CI ¥992.53–¥1,226.72) per patient per year, and every ¥1 spent on the program achieved ¥3.29 savings. Every ¥1,775.40/$237.98 spent on the program achieved one admission prevention.
Effects on Health Outcomes of the Program
Table 9 shows the measure scores for health outcomes of the groups. Table 10 shows net benefits of health-outcome indicators. Except for FVC, all outcomes showed improvements in the treatment group compared with the control group at the four time points (all p<0.05). Outcomes for the mMRC scale, COPD Assessment Test, and self-management achieved continuous improvements in the treatment group during the first 6 months, and slight reductions were found afterward. The lung-function indicators FEV1 and FEV1% predicted achieved continuous improvements during the first 12 months, and slight reductions were found during the second year.
 |
Table 9 Health-Outcome Scores of the Two Groups (n=174) |
 |
Table 10 Changes in Health Outcomes in Hospital-Outreach PR Program Compared with Usual Care (n=174) |
Discussion
The findings of the study showed that our hospital-outreach PR program for patients with COPD led to reductions in patient readmissions and ED visits, lower medical costs, and improvements in health outcomes. The program achieved a net saving of ¥3,655.94/$564.49 per patient per year during the first 2 years, and every ¥1 spent on the program achieved a saving of ¥3.29. Effects of the program on health-care utilization were significant at 6 months and other time intervals, but group differences were not statistically significant at 3 months, when the intensive intervention had just been completed. Previous studies with 8- to 12-week PR programs also showed no significant reductions in admission44,45 or hospital days46 immediately after intervention. This indicates that although short-term effects of PR programs can be found in health outcomes, such as improvements in exercise capacity and self-management, effects on health-care utilization may not become significant until several months later.
This hospital-outreach PR program also achieved monetary savings. The main element contributing to the savings came from decreased inpatient costs. Economic evaluation results have differed among previous studies. Differences in health-care systems among different countries and differing interventions (with or without maintenance program), duration (6–8 weeks, 3 months, 12 months, or 24 months), and doses (exercise frequency, length of time per session) bring difficulties for comparisons, and findings also indicate that further studies may need to explore content and doses of similar programs. Our program was associated with greater outpatient costs than usual care: an increase of ¥1,124.08/$173.56 per patient per year during the 2 years. A possible explanation for this increase may be increased use of inhaled medications for symptom control. This suggests that patient awareness of and adherence to medication taking improved. However, this should be viewed with caution, since we only got this from follow-up records of patients' general medication adherence. More details on prescribed medications and doses may be needed in future studies.
During the second year, the effects of the program were maintained, which means that its effects lasted for at least 24 months. Most previous studies evaluated short-term or medium-term effects of PR of 3–12 months. This study adds evidence of PR’s long-term effects. The maintenance approach after intensive intervention may play an important role in achieving long-term effects. Another study evaluated effects of an 8-week PR program followed by a maintenance phase with home exercise, evaluated by a chest physician or nurse every 2–3 months, lasting 52 weeks, and reductions were found in exacerbations and hospitalization times and days during the year after PR.47 However, for programs without a maintenance schedule, there were disparities in PR’s effects on hospitalization.48,49
The effects of the program on health outcomes were similar to previous studies,25,50 with improvements in exercise tolerance, dyspnea, and self-management. There were also interesting findings for FEV1 and FEV1%, two important lung-function indicators where improvements were found. COPD is usually characterized as a progressive decline in lung function.25,51 Many interventional studies for COPD patients have not included lung-function indicators. In this study, tai chi was used as an important part of the exercise. In previous systematic reviews of traditional Chinese exercise, including tai chi and qigong, for patients with COPD, improvements were found in FEV1 and FEV1% predicted.52–54 Tai chi exercise requires coordination of breathing and movement, strengthens respiratory muscles, and reduces pulmonary residual volume.55 In our program, traditional 24-form tai chi was modified to a simple six-form version, keeping the essence of breathing control, taking patient exercise capacity into consideration, and maintaing training in balance and flexibility. This simplified tai chi is easy to grasp and adhere to. Its effects among patients with COPD have been proved in our previous study.37 This indicates that lung function should be involved among outcomes of PR programs and be further proved.
Above all, these findings indicate that hospital-outreach PR is a double-win program that achieves reductions in health-care utilization, leads to medical monetary savings, and improves health outcomes. Our findings provide evidence for policy-makers in the health-care system to increase accessibility of hospital-outreach PR, improve referral mechanisms for PR in hospitals, and to optimize health insurance and financial compensation policies for the program. There are still limitations to this study. First, it was a single-center randomized controlled trial, and further multiple-center trials are necessary to enhance the evidence. Second, the effects of the program on health outcomes and health-care utilization and costs were dramatically improved for the first year of the program. Although the improvements still existed at the end of the second year, there were declines in exercise capacity (6-minute walking distance) and increased dyspnea (mMRC scale) and ED visits during the second year compared with the first year. This indicates that another intensive intervention may be needed at the start of the second year to sustain the benefits of the program. Third, although single-blind design was followed because of the nature of the intervention, unblinding participants and interventionists may cause potential bias, such as higherer expectations for the treatment group.
Conclusion
In this study, we developed a hospital-outreach PR program for patients with COPD after dischargfrom hospital to home. The program not only helped in reducing readmissions and length of stay in hospital and improve health outcomes but also achieved monetary savings. It also provided evidence for long-term effects of hospital-outreach PR intervention. The program also has implications for providing evidence to policy- makers, promoting decision-making for policy optimization to improve accessibility, affordability, and sustainability of such programs and maintain their benefits for patients.
Abbreviations
PR, pulmonary rehabilitation; COPD, chronic obstructive pulmonary disease; GOLD, Global Initiative for Chronic Obstructive Lung Disease; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; mMRC, modified Medical Research Council (dyspnea scale); CAT, COPD Assessment Test; 6MWD, 6-minute walking distance; CSMS, COPD Self-Management Scale.
Data-Sharing Statement
Individual participant data that underlie the results reported in this article (test, tables, and figures) are available after deidentification for 36 months after publication from the corresponding author on reasonable request, and researchers should provide a methodologically sound proposal.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosures
The authors report no conflicts of interest in this work.
Funding
This study was supported by the China Medical Board (12-115) and the National Key Research and Development Program of China (2018YFC1313600).
References
1. COPD Gene. Information on COPD; [
2. Mathers CD, Loncar D, Samet J. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi:10.1371/journal.pmed.0030442
3. Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387(10015):251–272. doi:10.1016/S0140-6736(15)00551-6
4. Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391(10131):1706–1717. doi:10.1016/S0140-6736(18)30841-9
5. Canadian Institute for Health Information. The Canadian Institute for Health Information Top 10 Reasons for Hospitalization in Canada; 2011.
6. Press VG, Au DH, Bourbeau J, et al. Reducing chronic obstructive pulmonary disease hospital readmissions. an official American Thoracic Society workshop report. Ann Am Thorac Soc. 2019;16(2):161–170. doi:10.1513/AnnalsATS.201811-755WS
7. Goto T, Faridi MK, Gibo K, et al. Trends in 30-day readmission rates after COPD hospitalization, 2006–2012. Respir Med. 2017;130:92–97. doi:10.1016/j.rmed.2017.07.058
8. Price LC, Lowe D, Hosker H, Anstey K, Pearson M, Roberts CM. UK national COPD audit 2003: impact of hospital resources and organisation of care on patient outcome following admission for acute COPD exacerbation. Thorax. 2006;61(10):837–842. doi:10.1136/thx.2005.049940
9. Chen X, Wang N, Chen Y, Xiao T, Fu C, Xu B. Costs of chronic obstructive pulmonary disease in urban areas of China: a cross-sectional study in four cities. Int J Chron Obstruct Pulmon Dis. 2016;11:2625. doi:10.2147/COPD.S118523
10. Lou P, Zhu Y, Chen P, et al. Vulnerability, beliefs, treatments and economic burden of chronic obstructive pulmonary disease in rural areas in China: a cross-sectional study. BMC Public Health. 2012;12(1):287. doi:10.1186/1471-2458-12-287
11. Global Initiative for Chronic Obstructive Lung Disease. 2018 global strategy for prevention, diagnosis and management of COPD; [
12. Yang F, Xiong Z-F, Yang C, et al. Continuity of care to prevent readmissions for patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. COPD J Chron Obstruct Pulmon Dis. 2017;14(2):251–261. doi:10.1080/15412555.2016.1256384
13. Lawlor M, Kealy S, Agnew M, et al. Early discharge care with ongoing follow-up support may reduce hospital readmissions in COPD. Int J Chron Obstruct Pulmon Dis. 2009;4:55.
14. Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675–684. doi:10.1111/j.1532-5415.2004.52202.x
15. Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The importance of transitional care in achieving health reform. Health Aff. 2011;30(4):746–754. doi:10.1377/hlthaff.2011.0041
16. Uijen AA, Schers HJ, Schellevis FG, van den Bosch WJ. How unique is continuity of care? A review of continuity and related concepts. Fam Pract. 2011;29(3):264–271. doi:10.1093/fampra/cmr104
17. Deseda J, Frank M, Bhogal N, Harris M. Single center post-discharge outreach intervention to reduce COPD readmissions. Chest. 2017;152(4):A814. doi:10.1016/j.chest.2017.08.845
18. Rodgers J, Stanton M, Jackson J. Providing care to COPD patients using in-home visits by nurse practitioners. J Nurs Care Qual. 2018;33(3):208–212. doi:10.1097/NCQ.0000000000000295
19. Benzo R, Vickers K, Novotny PJ, et al. Health coaching and chronic obstructive pulmonary disease rehospitalization. A randomized study. Am J Respir Crit Care Med. 2016;194(6):672–680. doi:10.1164/rccm.201512-2503OC
20. Aboumatar H, Naqibuddin M, Chung S, et al. Better Respiratory Education and Treatment Help Empower (BREATHE) study: methodology and baseline characteristics of a randomized controlled trial testing a transitional care program to improve patient-centered care delivery among chronic obstructive pulmonary disease patients. Contemp Clin Trials. 2017;62:159–167. doi:10.1016/j.cct.2017.08.018
21. Aboumatar H, Naqibuddin M, Chung S, et al. Effect of a program combining transitional care and long-term self-management support on outcomes of hospitalized patients with chronic obstructive pulmonary disease: a randomized clinical trial. JAMA. 2018;320(22):2335–2343. doi:10.1001/jama.2018.17933
22. Clini E, Holland AE, Pitta F, Troosters T. Textbook of Pulmonary Rehabilitation. Springer; 2018.
23. Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–e64. doi:10.1164/rccm.201309-1634ST
24. Wagg K. Unravelling Self-Management for COPD: What Next? London: SAGE Publications Sage UK; 2012.
25. McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;2.
26. Lacasse Y, Cates CJ, McCarthy B, Welsh EJ. This cochrane review is closed: deciding what constitutes enough research and where next for pulmonary rehabilitation in COPD. Cochrane Database Syst Rev. 2015;11.
27. Chen G, Wu S, Luo X, Li Q, Wu Q, Wang Y. The effects of Wechat on outreach management among chronic obstructive pulmonary disease. Chongqing Med. 2017;46(29):4132–4134.
28. Hu B, Miao X, Zhu X, Xiu L, Zhao J. The study of patients’ adherence with COPD therapy by home visit. Chin J Gen Pract. 2013;11(2):175–176.
29. Benzo RP, Chang -C-CH, Farrell MH, et al. Physical activity, health status and risk of hospitalization in patients with severe chronic obstructive pulmonary disease. Respiration. 2010;80(1):10–18. doi:10.1159/000296504
30. Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi:10.1164/rccm.201204-0596PP
31. Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. doi:10.1164/rccm.200703-456SO
32. Jenkins S, Hill K, Cecins NM. State of the art: how to set up a pulmonary rehabilitation program. Respirology. 2010;15(8):1157–1173. doi:10.1111/j.1440-1843.2010.01849.x
33. Downs CA, Appel SJ. Chronic obstructive pulmonary disease: diagnosis and management. J Am Acad Nurse Pract. 2007;19(3):126–132. doi:10.1111/j.1745-7599.2006.00207.x
34. Qaseem A, Wilt TJ, Weinberger SE, et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179–191. doi:10.7326/0003-4819-155-3-201108020-00008
35. Ergün P, Kaymaz D, Günay E, et al. Comprehensive out-patient pulmonary rehabilitation: treatment outcomes in early and late stages of chronic obstructive pulmonary disease. Ann Thorac Med. 2011;6(2):70. doi:10.4103/1817-1737.78420
36. Coultas D, McKinley J. Update on pulmonary rehabilitation for COPD. Clin Pulm Med. 2009;16(4):183–188. doi:10.1097/CPM.0b013e3181ac9a11
37. Zhu S, Shi K, Yan J, et al. A modified 6-form Tai Chi for patients with COPD. Complement Ther Med. 2018;39:36–42. doi:10.1016/j.ctim.2018.05.007
38. China Foreign Exchange Trading Center. Available from: http://www.chinamoney.com.cn/fe/Channel/17383.
39. Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–968. doi:10.1183/09031936.05.00035205
40. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805
41. Bestall J, Paul E, Garrod R, Garnham R, Jones P, Wedzicha J. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. doi:10.1136/thx.54.7.581
42. Jones P, Harding G, Berry P, Wiklund I, Chen W, Leidy NK. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34(3):648–654. doi:10.1183/09031936.00102509
43. Zhang C, Wang W, Li J, et al. Development and validation of a chronic obstructive pulmonary disease self-management scale. Respir Care. 2013;58(11):1931–1936. doi:10.4187/respcare.02269
44. Boxall A-M, Barclay L, Sayers A, Caplan GA. Managing chronic obstructive pulmonary disease in the community: a randomized controlled trial of home-based pulmonary rehabilitation for elderly housebound patients. J Cardiopulm Rehabil Prev. 2005;25(6):378–385. doi:10.1097/00008483-200511000-00012
45. Man WD, Polkey MI, Donaldson N, Gray BJ, Moxham J. Community pulmonary rehabilitation after hospitalisation for acute exacerbations of chronic obstructive pulmonary disease: randomised controlled study. BMJ. 2004;329(7476):1209. doi:10.1136/bmj.38258.662720.3A
46. Eaton T, Young P, Fergusson W, et al. Does early pulmonary rehabilitation reduce acute health‐care utilization in COPD patients admitted with an exacerbation? A randomized controlled study. Respirology. 2009;14(2):230–238. doi:10.1111/j.1440-1843.2008.01418.x
47. Rubí M, Renom F, Ramis F, et al. Effectiveness of pulmonary rehabilitation in reducing health resources use in chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2010;91(3):364–368. doi:10.1016/j.apmr.2009.09.025
48. Ko FW, Dai DL, Ngai J, et al. Effect of early pulmonary rehabilitation on health care utilization and health status in patients hospitalized with acute exacerbations of COPD. Respirology. 2011;16(4):617–624. doi:10.1111/j.1440-1843.2010.01921.x
49. Rasekaba T, Williams E, Hsu-Hage B. Can a chronic disease management pulmonary rehabilitation program for COPD reduce acute rural hospital utilization? Chron Respir Dis. 2009;6(3):157–163. doi:10.1177/1479972309104419
50. Peytremann-Bridevaux I, Staeger P, Bridevaux P-O, Ghali WA, Burnand B. Effectiveness of chronic obstructive pulmonary disease-management programs: systematic review and meta-analysis. Am J Med. 2008;121(5):433–443. (). doi:10.1016/j.amjmed.2008.02.009
51. Decramer M, Janssens W. Chronic obstructive pulmonary disease and comorbidities. Lancet Respir Med. 2013;1(1):73–83. doi:10.1016/S2213-2600(12)70060-7
52. Tong H, Liu Y, Zhu Y, Zhang B, Hu J. The therapeutic effects of qigong in patients with chronic obstructive pulmonary disease in the stable stage: a meta-analysis. BMC Complement Altern Med. 2019;19(1):1–10. doi:10.1186/s12906-019-2639-9
53. Ding M, Zhang W, Li K, Chen X. Effectiveness of t’ai chi and qigong on chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Altern Complement Med. 2014;20(2):79–86. doi:10.1089/acm.2013.0087
54. Luo X, Zhang J, Castelberg R, et al. The effects of traditional Chinese exercise in patients with chronic obstructive pulmonary disease: a meta-analysis. PLoS One. 2016;11(9):e0161564. doi:10.1371/journal.pone.0161564
55. Ng BH, Tsang HW, Jones AY, So C, Mok TY. Functional and psychosocial effects of health qigong in patients with COPD: a randomized controlled trial. J Altern Complement Med. 2011;17(3):243–251. doi:10.1089/acm.2010.0215
56. Statistical Yearbook of Zunyi. Available from: http://www.zunyi.gov.cn/zwgk/jcxxgk/tjxx/tjnj/201711/t20171116_721918.html.
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
