Back to Journals » HIV/AIDS - Research and Palliative Care » Volume 13
Effect of the Test and Treat Strategy on Mortality Among HIV-Positive Adult Clients on Antiretroviral Treatment in Public Hospitals of Addis Ababa, Ethiopia
Authors Tesfaye B, Ermias D , Moges S , Astatkie A
Received 27 January 2021
Accepted for publication 19 March 2021
Published 30 March 2021 Volume 2021:13 Pages 349—360
DOI https://doi.org/10.2147/HIV.S303557
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Bassel Sawaya
Bereket Tesfaye,1 Dejene Ermias,2 Sisay Moges,3 Ayalew Astatkie4
1USAID Family-Focused HIV Prevention Care and Support Program Integrated Services for Health and Development Organization, Addis Ababa, Ethiopia; 2Public Health Department, College of Medicine & Health Sciences, Wachemo University, Hosanna, Ethiopia; 3Department of Health Informatics, Hosanna College of Health Sciences, Hosanna, Ethiopia; 4School of Public Health, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
Correspondence: Dejene Ermias Email [email protected]
Background: The primary goal of antiretroviral therapy is to prevent human immune deficiency virus (HIV)-related morbidity and mortality. Deferring antiretroviral therapy (ART) until CD4 counts decline puts individuals with HIV at risk of HIV-related morbidity and mortality.
Objective: This study aims to assess the effect of the test and treat strategy on mortality among HIV-positive clients on ART in public hospitals in Addis Ababa.
Methods: A retrospective cohort study was conducted at five selected public hospitals in Addis Ababa. A cohort of 216 ART clients taken as an exposed group (test and treat” strategy) from 2017 to 2019 and 216 ART clients as an unexposed group taken from 2014 to 2017; totally, 432 clients were included in the study. Multivariate Cox regression was used to estimate the effect of the test and treat strategy on the survival of ART clients adjusting for other covariates.
Results: The 432 clients contributed to a total of 1025.17 person-years follow-up. Ninety-one (21.06%) of them died, 14.3% were unexposed and 6.7% were exposed (test and treat). The incidence of death was 92.4 and 81.8/1000 person-years in the unexposed group and exposed group, respectively, with an overall mortality rate of 88.8/1000 person-years. Besides, test and treat strategy (AHR: 0.31; 95% CI: 0.19, 0.52), baseline CD4 counts > 350 cells/mm3 (AHR 0.40; 95%: CI: 0.20, 0.80), bedridden functional status (AHR 2.46; 95% CI: 1.41, 4.27), poor adherence (AHR 3.25; 95% CI: 1.410– 7.51), moderate malnutrition on last visit (AHR 2.56; 95% CI: 1.30– 5.04) and staying on original regimen (AHR 4.68; 95% CI 2.72, 8.07) were independent predictors of mortality.
Conclusion: Mortality among HIV patients on treatment decreased significantly since the start of the test and treat strategy. Therefore, test and treat strategy should be strengthened in all public and private facilities throughout the country.
Keywords: test and treat, mortality, HIV/AIDS, Addis Ababa, Ethiopia
Introduction
Acquired immunodeficiency syndrome (AIDS) is an advanced stage of human immune deficiency virus (HIV) infection that takes years after the introduction of HIV to the human body and characterized by the development of certain cancers, serious infections, and other severe clinical manifestations.1
It is important for people living with HIV to initiate ART as soon as possible. This reduces the time between HIV diagnosis and ART initiation, thereby decreasing HIV-related morbidity and mortality, and reduces the forward transmission of HIV, including MTCT. In 2017, three out of four HIV-positive people know their status, which is the first step towards meditation. Besides, 21.7 million patients are on recovery with a net rise of 2.3 million people compared to 2016.2,3
In Ethiopia, an estimated 738,976 people are currently living with HIV and all of them require antiretroviral therapy (ART). Besides, 94,240 clients are receiving ART in Addis Ababa. Various programs have been undertaken to increase the health quality of HIV-positive patients, the quality of life, and to prolong the period of HIV-infection/AIDS-diagnosis to death; however, around 11,000 people in Ethiopia are dying from HIV-related disease.4–6 With free HIV testing and ART service, there should be no HIV-related death; however, death from HIV-related causes in the world, especially in developing countries such as Ethiopia is still being reported. Ethiopia has adopted the test and treat recommendation since February 2017 and since then all HIV-positive clients are eligible to start ART right away.7–9
The scale-up of access to treatment should not be taken for granted. HAART regimens commonly require changes that often involve switches of multiple medications simultaneously. As a result, treatment changes have become a common phenomenon, and hence limitation of treatment options has turned out major concern for the future of HAART and HIV/AIDS patients.10,11
Early diagnosis is key for tracing of HIV-positive people and leads to early initiation of ART, and hence might significantly reduce the rate of HIV-related mortality. The test and treat strategy is aimed to markedly decrease mortality related to HIV/AIDS.2 Ethiopia has changed the eligibility criteria of HIV-positive people for ART utilization. Recently Ethiopia adopted the WHO test and treat strategy and started the implementation on pilot bases in some health facilities then expanded to all health facilities in the country. Ever since there are no eligibility criteria to start on ART other than having HIV-positive results.12
Even though few studies are carried out to understand the impact of the HIV-related mortality and life expectancy test and treatment plan of people living with HIV globally, published study in Ethiopia is scarce. The findings will greatly assist health institutions in monitoring improvements to their clients’ survival as a result of the application of a plan for testing and treatment, will have a great impact in terms of evaluating the effectiveness or failure of the strategy for the Federal Health Minister and the Federal HIV/AIDS Prevention and Control Organization (HAPCO). The results
Therefore, this study is aimed to assess the effect of the test and treat strategy on mortality among HIV-positive adult clients who are on ART in public hospitals of Addis Ababa city, Ethiopia.
Methods
A hospital-based retrospective cohort study was conducted on HIV-positive clients on ART in five general hospitals (Menilik, Gandhi, Zewditu Memorial, Ras Desta, and Yekatit12) in Addis Ababa city, June 2020. All adult HIV-positive people who were enrolled in HIV care and treatment service at public hospitals in Addis Ababa city comprised the source population. Selected HIV-positive people who started ART in five selected General Hospitals (Menilik, Gandhi, Zewditu, Ras Desta, and Yekatit 12) constituted the study population. The study hospitals have already been chosen by the Federal Minister of Ethiopia as pilot hospitals for the implementation of the latest HIV-positive patients care plan, called the test and treatment strategy. The study population consists of two groups: a group of HIV-Positive clients who were not exposed to the test and treat strategy (unexposed), specifically clients who started ART two years before the start of the test and treat strategy (between July 2014 and January 2017), and a group of HIV-positive clients exposed to the test and treat strategy(exposed), specifically clients who started ART between February 2017 and July 2019.
Adult clients age greater than or equal to 15 years old enrolled in care and treatment and who started ART at least six months before the study were included in the study sample. On the other hand, clients who were diagnosed and started ART at the same hospital and transferred out (TO) and patients who started ART before July 2014 and After July 2019 were excluded from the study to ensure that our study clients have to be at least 6 months on ART.
The sample size is calculated using Epi info version 7. The following assumptions are considered; 95% confidence level, 80% power, the proportion of outcome in an unexposed group (9%) (i.e. death rate among HIV-positive clients before the test and treat strategy), and AHR=2.1713 taken from the previous study done in Ethiopia; and the ratio of exposed to an unexposed group of 1:1. A sample of 392 was obtained. Considering 10% incomplete documents, the final sample 432 (216 from exposed and 216 from non-exposed) study participants were included in the study.
Based on their proportion of clients, the samples were assigned to the 5 hospitals for their preliminary assessment. Accordingly, Gandi contributed 12% (52) clients, Zewditu contributed 33% (144) clients, Ras Desta 17% (75) clients, Minilik 18% (79) clients, and Yekatit 19% (82) clients. The sample was divided into exposed and unexposed categories in selected hospitals and client records are extracted from an electronic database with a systematic random sample.
The primary outcome variable is death (mortality) which is defined as the death of a client while on ART due to any cause except accidental death and occurred in hospitals and any setting confirmed by the hospitals. Hospitals, however, have methods to monitor their clients exclusively as hospitals have already been chosen by the Federal Minister of Ethiopia as pilot hospitals for the implementation of the latest HIV-positive patients care plan, called the test and treatment strategy. Hospitals thus closely follow, track and confirm when their clients have missed or died through a registered patient address since these hospitals are under close oversight by the Minister of Health. The mortality rate is measured by using person-time at risk starting from the time of ART initiation until each patient dies or is censored. Besides, the main exposure variable was test and treat strategy, which is defined as ART initiation immediately or within one week of diagnosis of HIV positive and linkage to care and treatment unit. Other independent variables included are functional status at baseline that was retrieved from the patient registry has three categories, working, ambulatory, and bedridden; it is classified according to national and WHO standards. The patient is listed as ambulatory if the client cannot work but is active; weight at baseline, clinical factors (baseline CD4, baseline WHO stage, anemia), sociodemographic factors (age, gender, educational level), treatment adherence retrieved from the hospital registry, and was identified using the WHO adherence appraisal process, and follow-up laboratories result like High viral load and low CD4 count.
To maintain the quality of data, appropriate training was given for data collectors. Incomplete data were excluded from the study and daily supervision was made at each facility throughout the data collection process.
Data were entered into EpiData then exported to STATA 14.2 for analysis. Descriptive statistics such as median with IQR, and mean with SD were computed to describe the characteristics of the cohort. Person-years of follow-up were calculated by assessing the date of enrollment for ART and the date of death or censoring. The Kaplan–Meier method was used to compare survival probabilities of the exposed and unexposed groups. The Log rank test, and Breslow, and Tarone test were used to determine if the survival probabilities in the exposed and unexposed groups were significantly different. Cox regression was employed to identify the effect of test and treat strategy on mortality of ART clients adjusted for other independent variables. Both Crude Hazard ratios (CHR) and Adjusted Hazard Ratio(AHR) with 95% confidence intervals were used as effect measures.
Since the unexposed group and the exposed group were not followed for an equal period, We conducted the Cox regression model again after excluding unexposed participants who were followed more than the maximum follow-up period of the exposed group (test and treat). Therefore, variables with p < 0.25 in the bivariate cox regression model and predefined variable (treatment modality) were included in the multivariate cox regression model to adjust for covariates. However, all variables included in the earlier cox regression model were also included in the Cox regression model conducted a second time after excluding participants in the exposure group who had a longer follow-up duration. The assumptions of proportionality of the Cox regression model were tested using the global test in STATA version 14.2 and satisfied (Proportionality Schoenfeld residual test (phtest) of (8) =7.91, P = 0.442).
Result
The study was carried out in five selected public hospitals in Addis Ababa City with a sample of 432 adult clients who began ART between July 1, 2014, and July 31, 2019. Half of them (216) started ART before the implementation of the test and treat strategy (unexposed group) based on other eligibility criteria. And the other half (216) started ART as per the test and treat strategy in which the criteria to start ART is having HIV-positive result and client readiness to start (exposed group).
Socio-Demographic Characteristics
The two arms of the cohort had no statistically significant difference in terms of basic sociodemographic characteristics. In the category of tests and treat, 56.5% were women, while 61.1% were women in the unexposed group. The median age of the clients was 39 years with an interquartile range (IQR) of 13.0 years. In the group of test and treat (exposed group), 91.2% of clients were between 16 and 50 years of age, while in the non-exposed group, 90.7% were in the age group indicated. Regarding educational status, clients in both groups have comparable educational status in the respective categories of education. Regarding the client’s employment status, in the test and treat cohort, 50.5% of clients were employed whereas 46.7%, in the control group (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Clients on ART, Addis Ababa, 2014–2019 |
Baseline Clinical Characteristics of the Cohort
Baseline CD4 count was done for 58.8% of clients in the unexposed group and 80% of clients in the test and treat group. Most (78.7%) of the study subjects had working functional status in the test and treat group and 69% had in the unexposed group. Half (48.6%) of the test and treat group clients had baseline WHO stage I while 40.3% in the unexposed group WHO stage I disease (Table 2).
 |
Table 2 Baseline Characteristics of Clients on ART, Addis Ababa, 2014–2019 |
Other Variables of the Cohort
In the test and treat (exposed group), 80% of the clients had disclosed their status to their families and friends while in the unexposed group 79.6% of clients had disclosed their results. The comparable number of clients in test and treat and unexposed groups had opportunistic infection (OI) treatment other than TB at least once throughout their follow-up. Regarding the TB coinfection status of the clients, no difference was observed between the two cohorts. And 67.6% of clients had good adherence for their medication in the exposed group and 65.7% had unexposed. A significant difference was shown in clients with mild malnutrition between the two groups. Thus, 46.3% of clients in the exposed group stayed on their original first-line regimen but, 56% of the HIV patients in the unexposed group remained on their original regimen (Table 3).
 |
Table 3 Other Variables of HIV-Positive Clients on ART, Addis Ababa, 2014–2019 |
Survival Analysis
From a total of 432 clients, 270 (62.5%) were active (alive on ART) at the end of the follow-up, 71 (16.4%) were lost to follow up and 91 (21.1%) died. Ninety-one (21.06%) of the clients died from the unexposed group. And 29 (6.7%) died from the exposed group. The study participants contributed a total of 1025.17 person-years of follow-up. The unexposed group was followed longer [mean (±standard deviations [SD]): 3.1 (±1.8) years] than the exposed group [mean (± SD): 1.6 (±0.8) years]. The person-year incidence of death was 92.4 per 1000 person-years in the unexposed group and 81.8 per 1000 person-years in the test and treatment group (exposed group), with an overall mortality rate of 88.7 per 1000 person-years.
The cumulative survival probability at year 1, 2, 3, 4, 5, for the group of clients who started before the implementation of the test and treat (unexposed group), was 0.84, 0.77, 0.75, 0.71, and 0.67, respectively, and for the group of clients who started ART based on test and treat strategy (exposed group) at year 1, 2, 3 was 0.93, 0.83 and 0.79, respectively.
The Kaplan–Meier survival curve shows the test-and-treat group had a higher survival probability than the unexposed group throughout the follow-up period (Figure 1). Though the Log rank test indicates the two categories have no significant difference in survival (p-value =0.65), the Breslow and Tarone tests show that there is a significant difference in survival of the two groups (p-values: 0.021 and 0.036, respectively).
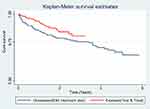 |
Figure 1 Kaplan–Meier survival estimate between unexposed group (previous treatment strategy) and exposed (test and treat strategy) among HIV infected patients on ART, Addis Ababa, 2014–2019. |
Effect of the Test and Treat Strategy and Other Covariates on Mortality
In crude analysis, test and treat strategy has no significant effect on mortality but baseline CD4 count, baseline functional status, baseline WHO stage, treatment adherence, last nutritional status, other comorbidities, and regimen change have a significant effect on mortality, and all of these variables were selected for multivariate analysis. Even though the test and treat strategy showed no significance, it was among the selected variables because it is our main variable of interest.
After controlling the effect of other co-varieties, the test and treat strategy has no significant effect on mortality (adjusted hazard ratio [AHR] =0.783; 95% CI=0.486 −1.263). Other covariates, which had a significant effect on mortality among ART clients, were baseline CD4 count, baseline functional status, adherence to medication, last nutritional status, other comorbidities, and regimen change. Clients whose baseline CD4 count was >350 cells/mm3 had a 40% lesser hazard of death as compared to those whose baseline CD4 count was less than 200 cells/mm3 (AHR= 0.40; 95% CI: 0.205–0.805). Bedridden patients had more than 2 times the higher hazard of mortality as compared to patients with working functional status (AHR= 2.46; 95% CI: 1.419–4.271) and ambulatory patients had about 1.5 times the higher hazard of mortality relative to working patients (AHR= 2.43; 95% CI: 1.38–4.27). Clients with poor medication adherence had more than 3 times the higher hazard of death compared to clients with good adherence (AHR= 3.25; 95% CI: 1.410–7.51). Clients diagnosed with moderate malnutrition on their last visit had more than 2.5 times more hazard of death compared to clients with normal nutritional status (AHR= 2.56; 95% CI: 1.30–5.04). Taking the original drug regimen increases the risk of mortality as compared to clients who changed their regimen (AHR= 4.68; 95% CI: 2.72–8.07) (Table 4).
 |
Table 4 Effect of Test and Treat Strategy and Other Covariates on Mortality Among HIV-Positive Clients on ART, Addis Ababa, 2014–2019 |
However, the unexposed group and exposed group were not followed for an equal period. The maximum follow-up period for the unexposed group was 5.85 years and for test and treat, it was 3.24 years. We conducted the analysis again after excluding participants in unexposed who were followed more than the maximum follow-up period of the test and treat category (3.24 years). Accordingly, HIV patients treated with the test and treat strategy had 69% less likely to die than those treated as per the previous strategy (AHR= 0.31; 95% CI 0.19–0.52), which makes the test and treat strategy a significant predictor of mortality. Baseline CD4, baseline functional status, adherence to medication, and regimen change also remained to be significantly associated with mortality in the re-analysis (Table 5).
Discussion
This study aimed to assess the effect of the test and treat strategy on mortality in comparison with the other strategy, which was implemented before the start of the test and treat, of adult clients who were on ART at five selected public hospitals of Addis Ababa town.
In this study, the overall mortality among the total of 432 clients was 21%. Incidence of death in the era of test and treat was reduced significantly (13.4%) as compared to the unexposed group (28.7%). When the entire data was analyzed, the test and treat strategy has no significant effect on survival. However, after we made the follow-up period of the two cohorts equal by excluding those in the unexposed group followed for a longer period than the maximum follows up period of the test and treat cohort, the test and treat group had significantly lower mortality both on Log rank test and Cox regression. In addition to the test and treat strategy, baseline CD4, baseline functional status, medication adherence, last nutritional status, other comorbidities, and regimen change have a significant effect on the mortality of clients.
The overall mortality was high (21%) as compared to the studies done in different parts of Ethiopia, and it was comparable with a study done in Nepal 20%.14 In a study conducted at Gurage, it was 9.6%,5 in Aksum, 8.8%7 and Tigray 7.5%.15 This difference might be explained by the documentation of the final status of clients at Addis Ababa might be better as compared to other small cities due to the use of well-organized communication between adherence supporters at all hospitals with urban health extension workers and the update of clients address in each visit was being practiced since the last two year in facilities at Addis Ababa which helps to trace the clients. When we compare the two cohorts the mortality among the test and treat cohort was lower than the unexposed group. It might be since during the time before the test and treat the clients were not eligible for treatment until they have advanced disease and low CD4, so that they may have not responded well to treatment which results in the death of many clients due to immune reconstitution syndrome IRIS.16,17
The effect of the test and treat strategy found by this study is in line with the studies done in the Gurage zone in Ethiopia18 and South Africa,1 but in a study done in Nigeria, the mortality rate after implementation of test and treat was 2%,17 which was much less than our finding 13.4%. This may happen despite the implementation of the test and treat strategy because clients are still presenting for care and treatment late as evidenced by 22% of clients in the test and treat cohort who presented with CD4 lower than 200cells/cubic mm and 28% who presented with WHO stages III and IV at baseline.
In our study, the Log rank test showed test and treat strategy has no significant effect on mortality when we analyze the whole data. This is due to the Log rank test emphasizes events that happened late in the follow-up period. And the maximum follow-up period for the two cohorts was not equal. The control group was followed for 5.85 years of maximum period, and the maximum follow-up period for test and treat clients were 3.24 years. The Breslow and Tarone tests (which emphasize the events that happened early and in the middle of the follow-up period, respectively) showed that test and treat has a significant effect on mortality.19,20
After excluding clients in the unexposed group who were followed for more than the maximum follow-up period of the test and treat group the test and treat strategy significantly affects mortality, and the mortality of clients decreased by 30%. The cumulative survival at years 2 and 3 is also higher in clients on the test and treat group and it agrees with the results found in Gurage Ethiopia and Nigeria.17,18
Unlike many other studies gender, educational status, and opportunistic infections have no significant effect on the survival of clients.7,15 And the magnitude of other factors that significantly contribute to the difference in survival rate is in line with other studies in Ethiopia and other African countries.
In this study having a baseline CD4 of less than 200cells/cubic mm is a significant predictor of mortality. This may be because these clients are highly immune-compromised and prone to other opportunistic infections, and this is in line with the studies done in Uganda, central Tigray, and Debre Markos.15,16,21 However, clients without CD4 count records were considerably different between the two groups, variation has not been noted in sensitivity analysis after excluding cases with missing CD4 count. Thus, the result we have reported is robust. Therefore, the detail of the sensitivity analysis in the study is not mentioned.
We found that clients who had bedridden functional status at baseline were at increased risk of mortality as compared to those with working functional status. This can be explained by the fact that being bedridden indicates that the client is seriously sick and might have a lower CD4 count and advanced WHO stage. And this finding is consistent with many studies conducted in Ethiopia15,21,22 and Nigeria.17
The study also highlights having advanced baseline WHO stage (III & IV) also significantly increases the risk of mortality, as having advanced WHO stage is having more serious opportunistic infections. This was in line with findings of Eastern Ethiopia, Uganda, and Nigeria.16,17,22
The current study demonstrated poor adherence is also a significant predictor of mortality. Our result is consistent with the results of studies done in Debre Markos,21 in southwest Ethiopia23 and in Uganda15,16 which may be explained by the fact that clients who have poor adherence are at risk of developing resistance to medication and lastly treatment failure which can lead to mortality if it does not detect early.
Nutritional status also determines the mortality of clients significantly. Clients who had severe malnutrition on their last visit had 1.6 times the higher hazard of mortality. Similarly, nutritional status has been a predictor of mortality in many other studies.10,12 Our result is also in agreement with the study done in Somalia.24 The reason for this can be malnutrition elicits dysfunctions in the immune system and promotes increased vulnerability of the host to other serious infections that can lead to death.25
We demonstrated that the presence of comorbidities was significantly associated with the mortality of clients. However, this finding was contrary to the study conducted in southwest Ethiopia.23 The reason for high mortality among clients with other comorbidities could be the fact that comorbidities can be caused or exacerbated by HIV/AIDS and some comorbidities also worsen the HIV infection by affecting the immune system and become computing cause for mortality among HIV-positive clients.26,27
In this study, only four clients switched their medication to a second line, and all four of them were censored. However, the other scenario newly happening is a substitution of medication to a better and new first-line regimen. According to this study, clients who stayed on the old (original) first-line treatment had 4.6 times more risk of mortality as compared to clients who substituted their regimen with the new drug. This might be explained by better tolerability, the low discontinuation rate due to pill burden, and rapid viral suppuration of the new combination fixed-dose drug Tenofovir, lamivudine, and Deltogavir (TLD).28 Unlike our study, in most studies’ regimen change was considered as a change of treatment regime to second-line drug regimen but in a study conducted in Gurage regimen change, in general, was also indicated as a significant predictor of mortality.18
Even though the study was a retrospective cohort design done on secondary data, all the variables were available on an electronic database that made the data collection procedure less challenging in this pandemic time. However, a follow-up lab test (Viral load) was omitted from the study as the test was started recently as an evaluative test for treatment success in the era of test and treat. Thus, this variable could not be used as a covariate in the present study. Besides, due to the retrospective nature of the study, missing data was the main challenge of the study. Therefore, selection bias may be introduced.
Conclusion
There is high overall mortality in this study as compared to most of the studies conducted in Ethiopia and other countries. There is a significant decrease in mortality in the test and treat group in comparison with the unexposed group. Baseline variables (CD4 count, WHO stage, functional status, and weight), adherence to treatment, presence of co-morbidities and nutritional status were found to be significant predictors of mortality among HIV-positive clients on ART.
Test and treat might cover the second 95 of the three ’95s but without strengthening the first 95 (early detection) and the third 95 (optimal viral suppression), the expected result will not be achieved and mortality will not be decreased to a lower possible level. Test and treat strategy should be strengthened in all public and private facilities throughout the country and clients have to start treatment as early as possible after they know their status.
Paper Context
There has been a decline in AIDS-related death in the region from 2010 to 2018. Moreover, the progress is more rapid in recent years after the implementation of the fast track/test and treat strategy. Ethiopia adopted the WHO test and treat strategy and started the implementation on pilot basis in some health facilities then expanded to all health facilities in the country. However, there is a lack of evidence on the effect of the test and treat strategy on mortality among ART clients. In the present study, we demonstrated that mortality among HIV patients on treatment decreased significantly since the start of the test and treat as compared to the unexposed group. Controlling other predictors especially baseline clinical and laboratory characteristics of clients will make a significant reduction of HIV-related mortality in the era of test and treat.
Abbreviations
AIDS, acquired immunodeficiency syndrome; ART, antiretroviral therapy; CPT, cotrimoxazole preventive therapy; EDHS, Ethiopian demographic health survey; HAART, highly active antiretroviral therapy; IPT, isoniazid preventive therapy; IRIS, immune reconstitution inflammatory syndrome; MTCT, mother to child transmission; OIs, opportunistic infections; PLHIV, people living with human immunodeficiency virus; PMTCT, prevention of mother to child transmission; SDG, sustainable development goal; T&T, test and treat; TB, tuberculosis; TLD, tenofovir, lamivudine; deltogavir; TO, transfer out.
Ethical Considerations
The study was approved by the Ethical Review Boards of Wachemo University (Ethiopia) and permission to collect data was also obtained from the Addis Ababa Health Bureau. Since the study was based on the review of medical records, patient consent was not obtained. However, the study does not harm any of the study participants. To maintain the confidentiality and privacy of the study participants, name of the participants and other personal information were not identified. Besides, training and instruction were given for data collectors regarding ethical aspect of the study. The ethical principles of the study are also in line with the Helsinki Declaration for medical sciences.
Acknowledgment
We would like to thank Wachemo University, Addis Ababa Health Bureau, and Yekatit 12 Hospital and Health Science College for their support during the study. We also appreciate supervisors, data collectors, and heads of selected hospitals.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
All Authors declare that they have no competing interests.
References
1. Bendavid E, Brandeau ML, Wood R, Owens DK. Comparative effectiveness of HIV testing and treatment in highly endemic regions. Arch Intern Med. 2010;170(15):1347–1354. doi:10.1001/archinternmed.2010.249
2. WHO. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection; 2016.
3. World Health O. Progress Report 2016: Prevent HIV, Test and Treat All: WHO Support for Country Impact. Geneva: World Health Organization; 2016:2016.
4. Office HPiERM-FHAPaC. HIV Prevention in EthiopiaNational Road Map 2018–2020; 2018.
5. Girum T, Wasie A, Worku A. Trend of HIV/AIDS for the last 26 years and predicting achievement of the 90-90-90 HIV prevention targets by 2020 in Ethiopia: a time series analysis. BMC Infect Dis. 2018;18(1):320. doi:10.1186/s12879-018-3214-6
6. Central Statistical Agency Addis Ababa E. Demographic and Health Survey 2016; 2016.
7. Tadesse K, Haile F, Hiruy N. FisahaHiruy, Neway. Predictors of mortality among patients enrolled on antiretroviral therapy in Aksum hospital, northern Ethiopia: a retrospective cohort study. PLoS One. 2014;9(1):e87392–e87392. doi:10.1371/journal.pone.0087392
8. FMOH. List of Hospitals in Addis Ababa Ethiopia; 2017.
9. Brinkhof MWG, Boulle A, Weigel R, et al. Mortality of HIV-infected patients starting antiretroviral therapy in sub-Saharan Africa: comparison with HIV-unrelated mortality. PLoS Med. 2009;6(4):e1000066–e1000066. doi:10.1371/journal.pmed.1000066
10. Hambisa MT, Ali A, Dessie Y. Determinants of mortality among HIV positives after initiating antiretroviral therapy in Western Ethiopia: a Hospital-Based Retrospective Cohort Study. ISRN AIDS. 2013;2013:491601. doi:10.1155/2013/491601
11. Kretzschmar ME, van der Loeff MF, Birrell PJ, De Angelis D, Coutinho RA. Prospects of elimination of HIV with test-and-treat strategy. Proc Natl Acad Sci U S A. 2013;110(39):15538–15543. doi:10.1073/pnas.1301801110
12. Walensky RP, David Paltiel A, Losina E, et al; Cepac Investigators. Test and treat DC: forecasting the impact of a comprehensive HIV strategy in Washington DC. Clin Infect Dis. 2010;51(4):392–400. doi:10.1086/655130
13. Mengesha S, Belayihun B, Kumie A. Predictors of survival in HIV-infected patient after initiation of HAART in Zewditu Memorial Hospital, Addis Ababa, Ethiopia. Int Sch Res Notices. 2014;2014:250913. doi:10.1155/2014/250913
14. Angdembe MR, Rai A, Bam K, Pandey SR, Maiga AI. Predictors of mortality in adult people living with HIV on antiretroviral therapy in Nepal: a retrospective cohort study, 2004–2013. PLoS One. 2019;14(4):e0215776. doi:10.1371/journal.pone.0215776
15. Belay H, Alemseged F, Angesom T, Hintsa S, Abay M. Effect of late HIV diagnosis on HIV-related mortality among adults in general hospitals of Central Zone Tigray, northern Ethiopia: a retrospective cohort study. HIV AIDS. 2017;9:187–192. doi:10.2147/HIV.S141895
16. Ingabire PM, Semitala F, Kamya MR, Nakanjako D. Delayed Antiretroviral Therapy (ART) initiation among hospitalized adults in a resource-limited settings: a challenge to the global target of ART for 90% of HIV-infected individuals. AIDS Res Treat. 2019;2019:1832152. doi:10.1155/2019/1832152
17. Stafford KA, Odafe SF, Lo J, et al. Evaluation of the clinical outcomes of the test and treat strategy to implement treat all in Nigeria: results from the Nigeria multi-center ART Study. PLoS One. 2019;14(7):e0218555. doi:10.1371/journal.pone.0218555
18. Girum TY, Yasin F, Wasie A, et al. The effect of “universal test and treat” program on HIV treatment outcomes and patient survival among a cohort of adults taking antiretroviral treatment (ART) in low income settings of Gurage zone, South Ethiopia. AIDS Res Ther. 2020;17(1):19. doi:10.1186/s12981-020-00274-3
19. Hazra A, Gogtay N. Biostatistics series module 9: survival analysis. Indian J Dermatol. 2017;62(3):251–257. doi:10.4103/ijd.IJD_85_17
20. Base K. How do the three methods compare to survival curves (log-rank, Mantel-Haenszel, Gehan-Breslow-Wilcoxon) differ? 2009; Available from: https://www.graphpad.com/support/faq/how-do-the-three-methods-compare-to-survival-curves-log-rank-mantel-haenszel-gehan-wilcoxon-differ/.
21. Abebe NA, Alemu K, Asfaw T, Abajobir AA. Survival status of HIV positive adults on antiretroviral treatment in Debre Markos Referral Hospital, Northwest Ethiopia: retrospective cohort study. Pan Afr Med J. 2014;17:88. doi:10.11604/pamj.2014.17.88.3262
22. Biadgilign S, Reda AA, Digaffe T. Predictors of mortality among HIV infected patients taking antiretroviral treatment in Ethiopia: a retrospective cohort study. AIDS Res Ther. 2012;9(1):15. doi:10.1186/1742-6405-9-15
23. Seyoum D, Degryse JM, Kifle YG, et al. Risk factors for mortality among adult HIV/AIDS patients following antiretroviral therapy in Southwestern Ethiopia: an assessment through survival models. Int J Environ Res Public Health. 2017;14(3):296. doi:10.3390/ijerph14030296
24. Damtew B, Mengistie B, Alemayehu T. Survival and determinants of mortality in adult HIV/Aids patients initiating antiretroviral therapy in Somali Region, Eastern Ethiopia. Pan Afr Med J. 2015;22:138. doi:10.11604/pamj.2015.22.138.4352
25. Duggal S, Chugh TD, Duggal AK. HIV and malnutrition: effects on immune system. Clin Dev Immunol. 2012;2012:784740. doi:10.1155/2012/784740
26. Albrecht S, Franzeck FC, Mapesi H, et al; Kiularco Study Group. Age-related comorbidities and mortality in people living with HIV in rural Tanzania. AIDS. 2019;33(6):1031–1041. doi:10.1097/QAD.0000000000002171
27. Lorenc A, Ananthavarathan P, Lorigan J, Jowata M, Brook G. The prevalence of comorbidities among people living with HIV in Brent: a diverse London Borough. London J Prim Care. 2014;6(4):84–90. doi:10.1080/17571472.2014.11493422
28. PEPFAR U, ICAP. Considerations for the Introduction of TLD in National Programs: PEPFAR Guidance on Developing Clinical and Programmatic Recommendations; 2018.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

