Back to Journals » International Journal of Women's Health » Volume 14
Effect of Surgical Findings on Prediction of Postoperative Ovarian Reserve in Patients with Ovarian Endometrioma
Received 2 May 2022
Accepted for publication 10 August 2022
Published 20 August 2022 Volume 2022:14 Pages 1127—1136
DOI https://doi.org/10.2147/IJWH.S373135
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Jisun Lee, Juyeon Kang, Hyun Jung Lee
Department of Obstetrics and Gynecology, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, Republic of Korea
Correspondence: Hyun Jung Lee, Department of Obstetrics and Gynecology, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, 130, Dongdeok-ro, Jung-gu, Daegu, 41944, Republic of Korea, Tel +821035328741, Fax +82534237905, Email [email protected]
Objective: Revised American Society for Reproductive Medicine (rASRM) classification for endometriosis is considered to have limited ability to predict fertility after surgery. This study evaluated the effect of surgical findings described by the rASRM classification on postoperative change in serum Anti-Müllerian hormone (AMH) in endometriosis.
Study Design: We retrospectively analyzed 112 patients with endometrioma who underwent laparoscopic ovarian cystectomy. The ovarian score was defined as the sum of the endometrioma score from the size and depth of endometrioma and the adhesion score from the extent and types of ovarian adhesion described in the rASRM classification. The ovarian score was correlated with the AMH levels before surgery (AMH0), 3 (AMH3), and 6 months (AMH6) after surgery. To design a model for predicting AMH6, using ovarian score and AMH0, we calculated the unstandardized predictive value of AMH6/AMH0 (UPV) by linear regression analysis. The predicted AMH6 (pAMH6) could be calculated by multiplying the UPV by AMH0. When AMH6 is less than 1.0 ng/mL, it was defined as a poor ovarian reserve group (PORG), and the accuracy of the predictive model was validated.
Results: The level of AMH declined more in rASRM stage IV compared to stage III after surgery. The ovarian score had a significant variable in the linear regression analysis with the ratio of AMH6/AMH0 (p = 0.001). The UPV was correlated with ovarian score negatively. The pAMH6 correlated with AMH6 positively and with age negatively. The pAMH6 showed sensitivity 0.564, specificity 0.909, positive predictive rate 0.786, and negative predictive rate 0.800 in the prediction of PORG (p < 0.001).
Conclusion: The pAMH6 predicted the PORG at 6 months after surgery. Based on the results of our study, the surgical findings, including the size and depth of the endometrioma and extent and types of adhesion could be useful indicators for ovarian reserve after surgery.
Keywords: endometrioma, anti-Müllerian hormone, ovarian reserve, cystectomy, revised American Society for Reproductive Medicine (rASRM) classification
Introduction
Endometriosis is defined as the presence of ectopic endometrial tissue outside the uterus that triggers a chronic inflammatory response, resulting in pain and infertility as major problems.1 Among them, ovarian endometriosis is closely related to infertility. The goals of treatment of ovarian endometriomas are to relieve endometriosis-related pain, exclude malignancy, and improve subfertility, while preserving ovarian function. Among surgical treatment option, performing cystectomy is recommended instead of cyst drainage and coagulation, as cystectomy reduces recurrence of endometrioma, and endometriosis associated pain.2,3 Although ovarian cystectomy is regarded as the treatment of choice for ovarian endometrioma, there are concerns that it may reduce ovarian reserve due to damage to surrounding healthy ovarian tissue during surgery. Ovarian reserve is determined by the quantity and quality of the remaining ovarian follicle pool that can grow in the presence of gonadotropins. Although no ideal standard single marker can predict the functional ovarian reserve in women of reproductive age, serum anti-Müllerian hormone (AMH) is considered a relatively good marker.4 As AMH is secreted by granulocytes in preantral and antral follicles, but not in primordial follicles, the ovarian invasion of endometriosis or ovarian damage during ovarian cystectomy and adhesiolysis around the ovary may be closely related to AMH reduction.5 The most widely used staging system for endometriosis is the revised American Society of Reproductive Medicine (rASRM) classification based on morphological descriptions.6,7 However, Vercellini et al8 observed no association between the endometriosis stage or lesion type and lesion site and the cumulative probability of pregnancy. As a tentative conclusion, this staging method has been considered to have a limited ability to predict future fertility after surgery in patients with endometrioma.9 Therefore, the rASRM classification needs a supplemental approach that can enhance the prediction of long-term prognosis such as ovarian reserve. We hypothesized that there was a relationship between surgical findings and the decrease of AMH after surgery. Among items described in the rASRM classification, we analyzed the correlation between ovarian factors, such as the size and depth of ovarian endometrioma and extent and types of ovarian adhesions, and the ovarian reserve after surgery. In this study, we aimed to evaluate the effect of surgical findings on serum AMH changes after surgery in patients with endometrioma, as a marker for predicting ovarian functional reserve.
Materials and Methods
Subjects
We retrospectively analyzed 112 patients with ovarian endometrioma who underwent ovarian cystectomy between May 2013 and June 2020 at the Department of Obstetrics and Gynecology, Kyungpook National University Hospital (KNUH), Kyungpook National University Chilgok Hospital, Daegu, Korea. The retrospective data collection and analysis were approved by the institutional review board of KNUH. The need for informed consent was waived because of the retrospective design of the study. Patients who had a history of adnexal surgery, other endocrine disorders, evidence of malignancies, or received hormone therapy within 6 months before the study were excluded. All patients were histologically confirmed to have ovarian endometrioma.
All patients received laparoscopic ovarian cystectomy. Initially, we examined the pelvis and abdomen to assess the extent of the endometriosis and identify any abnormalities or distortions of the pelvic organs. After mobilization by dissecting adhesions around the ovary, we made an incision on the antimesenteric border of the ovary with a monopolar hook. After the identification of the cleavage plane between the cyst capsule and the adjacent normal ovarian tissue, the cyst wall was stripped using two atraumatic grasping forceps. Residual ovarian tissue was sutured in two layers using a 2–0 V-LocTM (Medtronic, Covidien) for hemostasis rather than bipolar coagulation for minimizing tissue trauma. We recorded the surgical findings based on the rASRM classification (Figure 1). The stage of endometriosis and the score of each item described at rASRM classification were obtained. The size of the endometriomas was divided into three categories: <1cm, 1~3cm, and >3cm. The endometrioma depth of endometrioma was classified as deep and superficial. Deep endometrioma was defined as the complete coverage with normal ovarian tissue. The endometrioma score was defined as the sum of the scores for the size and depth of ovarian endometrioma. The adhesion score was defined as the sum of the scores for the extent and types of ovarian adhesions. The sum of the endometrioma score and adhesion score was defined as the ovarian score. After surgery, the dienogest was administered to all patients. The total operative time was defined as the time from skin incision to skin closure. Estimated blood loss (EBL) was calculated by the anesthesiology as the difference between the total amounts of suction and irrigation. Hemoglobin loss was defined as the difference in hemoglobin levels before and the first day after surgery. All patients were followed until 6 months after surgery.
Hormonal Measurements
The serum AMH level was measured using an enzyme-linked immunosorbent assay (ELISA) kit according to the manufacturer’s instructions (AMH Gen II ELISA, Immuno-tech). The intra- and inter-assay coefficients of variation for the AMH assay were both <10%. The lowest amount of AMH in a sample that could be detected with a 95% probability was 0.08 ng/mL. The serum AMH levels were tested in each patient before surgery (AMH0) and 3 (AMH3) and 6 months (AMH6) after surgery. The ratios of AMH3 over AMH0, AMH3 over AMH6, and AMH6 over AMH0 were calculated.
Statistical Analyses
Continuous variables were compared using paired t-test, and Student’s unpaired t-test was used if the data were normally distributed, as assessed using the Kolmogorov–Smirnov test. The correlations between factors and the ratios of AMH levels in all patients, including those in the unilateral or bilateral groups, rASRM III or IV groups, and AMH6 <1.0 ng/mL and AMH6 ≥1.0 ng/mL groups, were analyzed via bivariate correlation analysis and expressed as Pearson or Spearman correlation coefficients, as appropriate. Multiple linear regression analysis models were used to estimate the independent contributions of variables to AMH levels.
The correlation between the surgical findings, such as the size and location of the endometrioma, the extent and types of ovarian adhesions, and AMH0 and AMH6 was evaluated. Based on the regression analysis between the ovarian score based on the rASRM classification and the ratio of AMH6/AMH0, the unstandardized predictive value of AMH6/AMH0 (UPV) by linear regression analysis was calculated. The formula is y=−0.007x+0.693 (x=ovarian score based on rASRM classification, y=unstandardized predictive value of AMH6/AMH0). The predicted AMH6 (pAMH6) was obtained by multiplying the UPV by AMH0. This formula was validated by comparison pAMH6 with the actual AMH6 (R2=0.701, p < 0.001). When the AMH6 was <1.0 ng/mL, it was defined as a PORG. The statistical analysis, including the logistic regression analysis, was performed using a commercial software package (SPSS for Windows, v13.0; SPSS, Chicago, IL). P < 0.05 was considered statistically significant.
Results
All the women had regular menstrual cycles, and their ages ranged from 18 to 43 years (29.78 ± 5.86, mean ± standard deviation). Compared with stage III based on the rASRM classification, AMH0 and the ratio of AMH6 over AMH3 (AMH6/AM3) did not show significant differences in stage IV. However, AMH3, AMH6, the ratio of AMH3 over AMH0 (AMH3/AMH0), and the ratio of AMH6 over AMH0 (AMH6/AMH0) were significantly lower in stage IV (Table 1). The AMH3 was decreased compared with AMH0 (p < 0.001), but AMH6 was not significantly decreased (p = 0.886) compared with AMH3. The AMH6/AMH0 ratio of the bilateral group was lower than that of the unilateral group. A significant primary effect of rASRM stage (F = 6.159, p < 0.001) (Figure 2A) and bilaterality (F = 26.375, p < 0.001) (Figure 2B) on AMH, respectively, was observed. There is no significant interaction between bilaterality and ASRM stage on AMH (F = 0.469, p = 0.494). AMH6 showed a negative correlation with age and more decrease in rASRM stage IV compared to stage III (Figure 3A). AMH6 showed a linear relationship with AMH0 and was significantly lower in stage IV compared to stage III (Figure 3B). Thirty-seven patients were included in the PORG, and the remaining 75 patients had an AMH6 level of 1.0 ng/mL or higher. In the comparison between the two groups, the endometrioma score and adhesion score were significantly higher in PORG. Also, bilateral endometrioma and rASRM stage IV were more frequently observed in PORG (Table 2). The PORG not only was older but also presented with low AMH0, AMH3, and AMH6 levels and AMH6/AMH0 ratios (Table 3). The ovarian score had a significant variable in the linear regression analysis with AMH6/AMH0 ratio (R2 = 0.119, p = 0.001) (Figure 4A). The UPV showed a negative correlation with the ovarian scores (Figure 4B). The pAMH6 correlated with age negatively (Figure 5A), and showed a linear relationship with AMH6 (Figure 5B). Both pAMH6 and AMH6 were lower in the PORG.
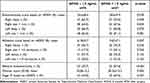 |
Table 2 Comparison of Items Defined on the rASRM Classification Between 6 Months AMH After Surgery (AMH6) ≥ 1.0 Ng/mL Group and AMH6 < 1.0 Ng/mL Group |
 |
Table 3 Comparison of Serum Anti-Müllerian Hormone (AMH) Levels Between 6 Months AMH After Surgery (AMH6) ≥1.0 Ng/mL Group and AMH6 < 1.0 Ng/mL Group |
In the receiver operating characteristic (ROC) curve estimation, pAMH6 showed a high predictive ability compared to age, AMH0, and ovarian score based on rASRM classification (Figure 6). The ovarian score based on rASRM classification showed a sensitivity of 0.658, specificity of 0.554, positive predictive rate of 0.431, negative predictive rate of 0.759, and accuracy of 0.589 in predicting the PORG (p = 0.046). The pAMH6 showed a sensitivity of 0.564, specificity of 0.909, positive predictive rate of 0.786, and negative predictive rate of 0.800 in the prediction of the PORG (P < 0.001) (Table 4).
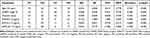 |
Table 4 Results of Multiple Linear Regression Analyses |
Discussion
Over the years, numerous ovarian reserve markers have been proposed including serum follicle-stimulating hormone (FSH) measured in early follicular phase with estradiol.10 The most recent markers, serum anti-Müllerian hormone (AMH) and antral follicle count (AFC) have shown to provide a direct and accurate management of ovarian follicle pool. AMH is produced only by granulosa cells in preantral and antral follicles, but not in primordial follicles.5 Thus, the AMH level indirectly represents the total number of follicles, as estimated by the number of early-growing-stage follicles. Compared to AFC, AMH has the advantage of a very little intra- and inter-cycle variability,11,12 is not affected by the use of gonadotropin-releasing hormone agonists or oral contraceptives,13 and is very sensitive to advancing age,14–16 it has been widely used in clinical practice for assessing ovarian reserve.17
It has been demonstrated that the serum AMH levels are decreased after the excision of an ovarian endometrioma18–20 and then can recover after the rearrangement of new growing AMH-secreting follicles.21 Therefore, after 6 months of surgery, AMH6 can be determined by the degree of the remaining primordial follicles according to the aging process, invasion by endometriosis, and adhesions that can damage the ovaries during surgery. The reduction of AMH related to aging and endometriosis infiltration was reflected in the AMH0. Age is a variable that has a close relationship with the AMH level before and after surgery. Therefore, the present study hypothesizes that the additional reduction of AMH by surgery was related to the rASRM score, including the size of the endometrioma and the degree of adhesion. In this study, we aimed to confirm our hypothesis by rejecting the null hypothesis that the AMH6/AMH0 ratio does not differ with increasing rASRM. We found that the surgical findings associated with ovarian endometrioma described at rASRM classification were associated with a decreased ratio of AMH6/AMH0 after surgery.
The staging of endometriosis requires the detailed observation and recording of the site, number, size, and depth of the endometriosis lesions, as well as the degree of adhesions. The original system was based on arbitrary scores and divided women into different stages: I (1–5 points), II (6–15 points), III (16–40 points), and IV (>40 points). The rASRM score is mainly used to assess the disease severity and develop a postoperative treatment plan. The diameter of endometrioma in the ovary plays a critical role in determining the rASRM score. One limitation in the evaluation of ovarian endometriosis is that it is difficult to compare the size of the endometrioma in the case of unilateral or bilateral involvement. For example, it is difficult to predict the prognosis by comparing a patient with an endometrioma with a size of 1 cm in the right ovary and 1 cm in the left ovary with a patient with an endometrioma with a size of 3 cm only in the right side. Moreover, we found that in the poor ovarian reserve group, the cyst score, adhesion score, and age were significantly higher and preoperative AMH was significantly lower (AMH6 <1 ng/mL). Furthermore, bilateral endometrioma and rASRM stage IV were more frequently observed in the poor ovarian reserve group. These results suggest that cystectomy and adhesiolysis for ovarian endometriomas affect the ovarian reserve, which correlates with the findings of other studies.24 In addition, among the factors associated with AMH decline after ovarian cystectomy, bilaterality and age are considered important factors.9,24 The rASRM score is calculated by adding up all the scores for the size, location, and degree of adhesion of each endometrioma affected in the left and right ovaries, but no additional score for bilaterality was given. In this study, sizes >3 cm were not associated with AMH. One of the reasons was that 86% of the endometriomas of the included patients had a size of >3 cm. The deep location of ovarian endometrioma is suspected to be associated with postoperative AMH decline. One of the proposed mechanisms that might be related to the postoperative reduction of ovarian reserve is the incidental removal of healthy ovarian tissue during cystectomy. Hemostatic efforts may also be associated with reduced ovarian reserve by damaging the vascularity of the remaining ovarian healthy tissue. Therefore, the removal of a deeply located endometrial cyst, where most of the cyst is surrounded by normal ovarian tissue, might lead to more loss of healthy ovarian tissue, which impairs ovarian reserve.22 However, there was no statistical significance between the ovarian deep location and poor ovarian reserve group in our cases. In this study, the adhesion score was significantly higher in the poor ovarian reserve group. One of the primary reasons for the reduction in ovarian reserve is the unintentional removal of the normal ovarian cortex containing follicles during adhesiolysis.22–24 When the size of the adhesions was large, the incidence of dense adhesion was high and the possibility of removal of healthy ovarian tissue during adhesiolysis was higher. However, some studies have reported no significant correlation between the number of follicles removed and the decline in AMH levels.25,26 In this study, we could predict 6 months of AMH after surgery using AMH before surgery and the ovarian score based on the rASRM classification. So, the surgeon could predict the ovarian reserve after surgery using the surgical findings, and it is expected to use for counseling with patients.
Nevertheless, our study has some limitations. First, this is a retrospective data collection and analysis, not a prospective randomized clinical trial. Therefore, many patients with serious conditions can be included in the surgical indication criteria. Second, the skill of the surgical technique of the surgeon who performed the laparoscopic ovarian cystectomy was not considered in the presented study. Third, the AMH level was the only marker for evaluating the ovarian reserve. The other factors are related to the ovarian reserve were not included.
Conclusions
The pAMH6 calculated using an ovarian score based on the rASRM classification in patients with ovarian endometrioma better predicted the poor ovarian reserve group at 6 months after surgery. Based on the results of our study, we concluded that the surgical findings related to ovarian endometrioma, including the size and depth of the endometrioma and extent and types of adhesions are expected to be useful indicators for ovarian reserve after surgery.
Abbreviations
AMH, anti-Müllerian hormone; rASRM, revised American Society for Reproductive Medicine; AMH0, anti-Müllerian hormone before surgery; AMH3, 3 months anti-Müllerian hormone after surgery; AMH6, 6 months anti-Müllerian hormone after surgery; pAMH6, predicted 6 months anti-Müllerian hormone after surgery; UPV, the unstandardized predictive value of AMH6/AMH0; PORG, poor ovarian reserve group.
Ethical Approval
Ethical approval was granted in November 2021 by institutional review board of Kyungpook National University Hospital (IRB file No. 2021-10-027-001). The date was anonymized and maintained with confidentiality. This study complies with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kennedy S, Bergqvist A, Chapron C, et al. ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod. 2005;20(10):2698–2704. doi:10.1093/humrep/dei135
2. Becker CM, Bokor A, Heikinheimo O, et al. ESHRE guideline: endometriosis. Hum Reprod Open. 2022;2022(2):hoac009.
3. Muzii L, Di Tucci C, Di Feliciantonio M, et al. Management of endometriosis from diagnosis to treatment: roadmap for the future. Minerva Ginecol. 2019;71(1):54–61.
4. Kwon SK, Kim SH, Yun SC, et al. Decline of serum antimullerian hormone levels after laparoscopic ovarian cystectomy in endometrioma and other benign cysts: a prospective cohort study. Fertil Steril. 2014;101(2):435–441.
5. Durlinger AL, Gruijters MJ, Kramer P, et al. Anti-Mullerian hormone inhibits initiation of primordial follicle growth in the mouse ovary. Endocrinology. 2002;143(3):1076–1084.
6. Canis M, Donnez JG, Guzick DS, et al. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67(5):817–821.
7. Adamson GD. Endometriosis classification: an update. Curr Opin Obstet Gynecol. 2011;23(4):213–220.
8. Vercellini P, Fedele L, Aimi G, De Giorgi O, Consonni D, Crosignani PG. Reproductive performance, pain recurrence and disease relapse after conservative surgical treatment for endometriosis: the predictive value of the current classification system. Hum Reprod. 2006;21(10):2679–2685.
9. Adamson GD, Pasta DJ. Endometriosis fertility index: the new, validated endometriosis staging system. Fertil Steril. 2010;94(5):1609–1615.
10. Grisendi V, Mastellari E, La marca A. Ovarian reserve markers to identify poor responders in the context of Poseidon classification. Front Endocrinol. 2019;10:281. doi:10.3389/fendo.2019.00281
11. La Marca A, Grisendi V, Griesinger G. How much does AMH really vary in normal women? Int J Endocrinol. 2013;2013:959487. doi:10.1155/2013/959487
12. La Marca A, Sighinolfi G, Radi D, et al. Anti-Mullerian hormone (AMH) as a predictive marker in assisted reproductive technology (ART). Hum Reprod Update. 2010;16(2):113–130. doi:10.1093/humupd/dmp036
13. Seifer DB, Maclaughlin DT. Mullerian Inhibiting Substance is an ovarian growth factor of emerging clinical significance. Fertil Steril. 2007;88(3):539–546. doi:10.1016/j.fertnstert.2007.02.014
14. van Rooij IAJ, Broekmans FJM, Scheffer GJ, et al. Serum antimüllerian hormone levels best reflect the reproductive decline with age in normal women with proven fertility: a longitudinal study. Fertil Steril. 2005;83(4):979–987. doi:10.1016/j.fertnstert.2004.11.029
15. Fanchin R. Serum anti-Mullerian hormone is more strongly related to ovarian follicular status than serum inhibin B, estradiol, FSH and LH on day 3. Human Reproduct. 2003;18(2):323–327. doi:10.1093/humrep/deg042
16. de Vet A, Laven JS, de Jong FH, Themmen AP, Fauser BC. Antimullerian hormone serum levels: a putative marker for ovarian aging. Fertil Steril. 2002;77(2):357–362.
17. Oh SR, Choe SY, Cho YJ. Clinical application of serum anti-Mullerian hormone in women. Clin Exp Reprod Med. 2019;46(2):50–59.
18. Maneschi F, Marasa L, Incandela S, Mazzarese M, Zupi E. Ovarian cortex surrounding benign neoplasms: a histologic study. Am J Obstet Gynecol. 1993;169(2 Pt 1):388–393.
19. Somigliana E, Ragni G, Benedetti F, Borroni R, Vegetti W, Crosignani PG. Does laparoscopic excision of endometriotic ovarian cysts significantly affect ovarian reserve? Insights from IVF cycles. Hum Reprod. 2003;18(11):2450–2453.
20. Raffi F, Metwally M, Amer S. The impact of excision of ovarian endometrioma on ovarian reserve: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2012;97(9):3146–3154.
21. Decanter C, Morschhauser F, Pigny P, Lefebvre C, Gallo C, Dewailly D. Anti-Mullerian hormone follow-up in young women treated by chemotherapy for lymphoma: preliminary results. Reprod Biomed Online. 2010;20(2):280–285.
22. Hachisuga T, Kawarabayashi T. Histopathological analysis of laparoscopically treated ovarian endometriotic cysts with special reference to loss of follicles. Hum Reprod. 2002;17(2):432–435.
23. Muzii L, Bianchi A, Croce C, Manci N, Panici PB. Laparoscopic excision of ovarian cysts: is the stripping technique a tissue-sparing procedure? Fertil Steril. 2002;77(3):609–614.
24. Roman H, Tarta O, Pura I, et al. Direct proportional relationship between endometrioma size and ovarian parenchyma inadvertently removed during cystectomy, and its implication on the management of enlarged endometriomas. Hum Reprod. 2010;25(6):1428–1432.
25. Hirokawa W, Iwase A, Goto M, et al. The post-operative decline in serum anti-Mullerian hormone correlates with the bilaterality and severity of endometriosis. Hum Reprod. 2011;26(4):904–910.
26. Celik HG, Dogan E, Okyay E, et al. Effect of laparoscopic excision of endometriomas on ovarian reserve: serial changes in the serum antimullerian hormone levels. Fertil Steril. 2012;97(6):1472–1478.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.







