Back to Journals » Clinical Interventions in Aging » Volume 13
Effect of starting oral intake on weekends on the clinical course of patients with aspiration pneumonia
Authors Kenzaka T , Kumabe A, Kosami K, Ueda Y, Takahashi T, Yamamoto Y , Hayashi Y, Kitao A, Okayama M
Received 6 January 2018
Accepted for publication 22 March 2018
Published 9 May 2018 Volume 2018:13 Pages 895—901
DOI https://doi.org/10.2147/CIA.S161786
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Tsuneaki Kenzaka,1,2 Ayako Kumabe,2 Koki Kosami,2 Yuki Ueda,2 Takeshi Takahashi,3 Yuya Yamamoto,4 Yurika Hayashi,4 Akihito Kitao,4 Masanobu Okayama5
1Division of Community Medicine and Career Development, Kobe University Graduate School of Medicine, Kobe, Japan; 2Division of General Medicine, Center for Community Medicine, Jichi Medical University School of Medicine, Shimotsuke, Japan; 3Department of Community and Family Medicine, Yuzawa Community Medical Center, Yuzawa, Japan; 4Department of General Medicine, Toyooka Public Hospital, Toyooka, Japan; 5Division of Community Medicine and Medical Education, Kobe University Graduate School of Medicine, Kobe, Japan
Purpose: The aim of this study was to investigate whether the day of starting oral intake affects the clinical course of patients with aspiration pneumonia.
Patients and methods: We conducted a retrospective cohort study of 392 patients who were hospitalized for aspiration pneumonia but tolerated oral intake. Patients were divided into two groups according to the day of starting oral intake: Monday to Friday (midweek group) and Saturday or Sunday (weekend group). Underlying diseases, severity of pneumonia, time to oral intake, hospital duration, discontinuation of oral intake, and death during hospitalization were compared between the groups. Multivariate analysis was performed using hospital duration and discontinuation of oral intake due to aspiration as the dependent variables.
Results: The cohort comprised 244 men and 148 women with a mean age of 79.3 ± 13.1 years. The weekend (n = 98) and midweek (n = 294) groups exhibited similar age, sex, and underlying diseases. There were no significant differences in pneumonia-related factors, such as CURB-65 score, A-DROP score, extent of shadow on chest radiograph, incidence of bacteremia, and ventilator use. The weekend group exhibited a significantly shorter time to oral intake and hospital duration, as well as a significantly lower incidence of discontinuation of oral intake than the midweek group. Multivariate analysis revealed that starting oral intake on the weekend was independently associated with a lower incidence of discontinuation of oral intake due to aspiration.
Conclusion: The weekend group exhibited a shorter total hospital duration and a lower incidence of discontinuation of oral intake due to aspiration.
Keywords: discontinuation of oral intake, hospital duration, health economics, weekend
Introduction
The number of deaths caused by pneumonia in Japan is increasing due to the aging Japanese population. Recent statistics indicate that, after malignant neoplasms and heart disease, pneumonia is the third most frequent cause of death in Japan and is more common than cerebrovascular disease.1 In total, >120,000 people die from pneumonia each year, corresponding to approximately 100 deaths per 100,000 population, and these rates are expected to increase. Aspiration pneumonia is especially frequent among elderly individuals, accounting for approximately 33.0%, 50.0%, and 80.1% of pneumonia-related hospitalizations among individuals aged 50–59, 60–69, and >70 years, respectively.2 Furthermore, aspiration pneumonia is the strongest risk factor for death within 30 days of hospitalization among patients with pneumonia.3 Thus, treating and preventing aspiration pneumonia are important considerations when treating patients with pneumonia.
In the Japanese medical system, only a small number of doctors, nurses, and caregivers work on the weekend. Furthermore, our previous study4 revealed that ~80.0% of clinicians started oral intake on a weekday for patients with aspiration pneumonia. Thus, it appears that Japanese medical professionals are hesitant to start oral intake on the weekend after its prohibition in patients with aspiration pneumonia. However, it is unclear whether this hesitation has any effect on the clinical course.
Therefore, the aim of the current study was to investigate whether the day of starting oral intake affects the clinical course of patients with aspiration pneumonia.
Patients and methods
Study setting and population
Consecutive patients with aspiration pneumonia were identified at three study sites (ICD code, J69): Division of General Internal Medicine, Jichi Medical University Hospital (Tochigi, Japan; 2007–2013); Department of General Medicine, Toyooka Public Hospital (Hyogo, Japan; 2011–2013); and Department of Community and Family Medicine, Yuzawa Community Medical Center (Niigata, Japan; 2010–2012).
Based on consensus guidelines adopted by the Japanese Respiratory Society,5,6 aspiration pneumonia was defined as pneumonia that occurred in patients with dysphagia or aspiration and/or patients who were strongly suspected of having dysphagia or aspiration based on their clinical course. The exclusion criteria were as follows: patients who died or who had not restarted oral intake during hospitalization. The baseline data were comparable to those reported in our previous study.7 This study was approved by the ethics committee for epidemiologic study at Jichi Medical University (Shimotsuke, Japan). The requirement for informed consent was waived owing to the retrospective observational study design. According to the ethical guidelines concerning the medical system study for people in Japan, we conducted this study in individual hospitals (number: Ekigaku 12–34; approved on November 22, 2012). We also kept confirmation of patient data confidentiality or anonymized data.
Measurements
The patients’ medical records were used to collect data on age, sex, underlying diseases (a history of head and neck tumors, gastroesophageal surgery, cerebral nerve disease, chronic lower respiratory disease, and diabetes mellitus), the day of admission, and the day of restarting oral intake. In addition, the following information was obtained on admission: consciousness score (Glasgow Coma Scale),8 blood oxygen saturation level, extent of shadow on chest radiograph, white blood cell count, albumin level, C-reactive protein level, Eastern Cooperative Oncology Group performance status, and the presence of bacteremia. The severity of pneumonia was assessed using the A-DROP scoring system,9 which provides a severity score for community-acquired pneumonia that was proposed by the Japanese Respiratory Society based on the CURB-65 score,10 which was also assessed. The A-DROP score was calculated using age (score added for men aged ≥70 years or women aged ≥75 years), dehydration, respiratory failure, disturbance of orientation, and low blood pressure. The CURB-65 score was calculated using confusion, blood urea nitrogen levels, respiratory rate, blood pressure, and age >65 years. The A-DROP and CURB-65 scores were calculated retrospectively. Data were also collected regarding the following variables during hospitalization: respirator use, time to starting oral intake, hospital duration, discontinuation of oral intake due to aspiration (a temporal interruption, not a permanent discontinuation that lasted until discharge), and death during hospitalization.
Only one or two speech therapists were present at each participating hospital for this study. This number was not sufficient to effectively carry out swallow function tests in all patients. Therefore, if the physician believed that the patient had nearly normal swallowing function, then swallowing function was not assessed by a speech therapist. In addition, oral ingestion began in stages. In these cases, physicians relied on information from the patients’ families and on dysphagia screenings by well-trained nurses. However, if the physician suspected that a patient had poor swallowing function, then swallowing function was assessed by a speech therapist. According to the advice of a speech therapist, oral intake began in stages or was postponed while undergoing swallowing function training.
Statistical analyses
Patients were grouped according to the day of the week that they started oral intake after its prohibition. Hospital duration, time to starting oral intake, discontinuation of oral intake due to aspiration, and death for each day of the week in each group were recorded. Patients were divided into two groups according to the day of starting oral intake: Monday to Friday (midweek group) and Saturday or Sunday (weekend group). Continuous variables were compared between the groups using the Student’s t-test; categorical variables were compared using the Chi-square test. Multivariate regression analysis was performed using hospital duration and discontinuation of oral intake due to aspiration as the dependent variables. Variables with a P-value of <0.05 and those that were previously reported to be associated with aspiration pneumonia were included in the multivariate analysis. All statistical analyses were conducted using Statistical Package for the Social Sciences for Windows (version 22.0; IBM Corporation, Armonk, NY, USA). A P-value of <0.05 was considered statistically significant.
Results
The study flowchart is shown in Figure 1. During the study period, 751 patients were hospitalized due to pneumonia, of whom 417 (55.5%) were diagnosed with aspiration pneumonia. However, 25 patients were discharged or had died without starting oral intake after its prohibition. Therefore, 392 patients were eligible for inclusion in this study. The study cohort comprised 244 men and 148 women with a mean age of 79.3 ± 13.1 (range: 22–102) years. The younger patients with aspiration pneumonia had underlying diseases, such as cerebral palsy and sequelae of cerebral hemorrhage.
  | Figure 1 Study flowchart. |
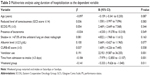
Measurements according to the day of the week are given in Table 1 and Figure 2. The number of hospital admissions tended to be higher on Mondays and Tuesdays. Significantly, fewer patients restarted oral intake on Sundays and Mondays. However, the time to restarting oral intake was shortest for Mondays, Saturdays, and Sundays (in that order). Furthermore, the rate of discontinuation of oral intake due to aspiration was lower for patients who restarted oral intake on Mondays, Saturdays, and Sundays (in that order). The rate of death during hospitalization was lower for patients who restarted oral intake on Mondays, Saturdays, and Thursdays (in that order). Conversely, the time from hospitalization to restarting oral intake was longest, and the rates of discontinuation of oral intake due to aspiration and death were highest for Fridays. In addition, the proportion of patients who restarted oral intake on Fridays was the second highest.
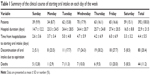  | Table 1 Summary of the clinical course of starting oral intake on each day of the week |
  | Figure 2 Histogram of the number of admissions per day according to the time from hospitalization to oral intake. |
Measurements for the weekend and midweek groups are summarized in Table 2. The weekend group included 98 patients, and the midweek group included 294 patients. The two groups exhibited similar age, sex, and underlying diseases. Coma was more common in the midweek group. However, there were no significant differences between the groups regarding pneumonia severity measures, such as A-DROP and CURB-65 scores, the extent of shadow on chest radiograph, the presence of bacteremia, and ventilator use. Compared to the midweek group, the weekend group exhibited a significantly shorter time to restarting oral intake and hospital duration as well as a significantly lower rate of discontinuation of oral intake due to aspiration. There was no significant difference in the death rate between the two groups.
The results of the multivariate analysis using hospital duration as the dependent variable are summarized in Table 3. Respirator use, a prolonged time to restarting oral intake, and restarting oral intake on a Monday to Friday were significantly associated with prolonged hospitalization. Therefore, the weekend group, who restarted oral intake on a Saturday or Sunday, had a shorter duration of hospitalization.
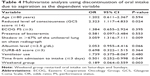
The results of the multivariate analysis using discontinuation of oral intake due to aspiration as the dependent variable are summarized in Table 4. A reduced level of consciousness, a large shadow on chest radiograph, a prolonged time to restarting oral intake, and restarting oral intake on a Monday to Friday were significant risk factors associated with the discontinuation of oral intake due to aspiration.
Discussion
This study evaluated the association between starting oral intake on specific days of the week and hospital duration and discontinuation of oral intake in patients with aspiration pneumonia. Our results suggest that starting oral intake on a Saturday or Sunday is associated with a significantly shorter hospital duration and a lower rate of discontinuation of oral intake due to aspiration. Interestingly, although the number of admissions tended to be higher on Mondays and Tuesdays, there were no significant differences in the number of admissions on the other days of the week. The weekend and midweek groups exhibited similar characteristics and severities of pneumonia. However, significantly fewer patients started oral intake on Sundays and Mondays, and the time to starting oral intake was significantly shorter in the weekend group than in the midweek group. Conversely, the time from hospitalization to starting oral intake was longest, and the rates of discontinuation of oral intake due to aspiration and death were highest for Fridays. In addition, the proportion of patients who started oral intake on Fridays was the second highest. This difference may be due to Japanese medical professionals being hesitant to start oral intake on weekends,4 due to having fewer medical resources and concerns regarding the need to perform medical procedures for aspiration and the recurrence of pneumonia. In other words, we assume that even for conditions where oral intake may be possible on weekends, clinicians are still hesitant in starting oral intake on weekends. Starting oral intake after the start of the week may extend the fasting period, which could lead to reduced swallowing function and extended durations of hospitalization. Meanwhile, on Fridays, there is the potential that even if the state of swallowing function is inadequate, oral intake may be started because physicians want to avoid starting oral intake on weekends. Starting oral intake despite inadequate swallowing function may lead to high rates of discontinuation of oral intake due to aspiration and high death rates.
Among patients who are prohibited from oral intake due to aspiration pneumonia, early evaluation of swallowing function and early training are effective for maintaining swallowing function when these steps are performed during dry swallowing.11 In addition, we believe that delaying oral intake will promote reduced swallowing function, especially among elderly patients. Therefore, delaying oral intake could lead to a higher rate of discontinuation of oral intake due to aspiration, which could prolong the duration of hospitalization. Furthermore, burdens are placed on the medical system by patients who experience delays in restarting oral intake, discontinuation of oral intake due to aspiration, and prolonged durations of hospitalization. Furthermore, a higher rate of discontinuation of oral intake due to aspiration and prolonged hospitalization due to reduced swallowing function negatively affects patient recovery and quality of life.
Our study has several limitations that warrant consideration. First, this study has a retrospective design, which is associated with various well-known limitations. Second, we only evaluated patients at three sites. Therefore, our findings may not be generalizable to other populations of Japanese patients with aspiration pneumonia. Third, the level of consciousness at admission tended to be lower in the midweek group than in the weekend group, although this was not significant. When the multivariate analysis was adjusted for the level of consciousness and the time to oral intake, we observed that starting oral intake on a weekend was independently associated with a shorter duration of hospitalization and a lower rate of discontinuation of oral intake due to aspiration. However, it is possible that a reduced level of consciousness prolonged the time to oral intake in the midweek group.
Conclusion
Japanese patients with aspiration pneumonia who started oral intake on a weekend (Saturday or Sunday) exhibited a shorter duration of hospitalization and a lower rate of discontinuation of oral intake due to aspiration than patients who restarted oral intake on a weekday (Monday to Friday).
Acknowledgments
We would like to thank Editage (www.editage.com) for English language editing. This study was supported by a Grant-in-Aid for scientific study from the Japan Society for the Promotion of Science (grant number: 25860507).
Author contributions
TK conceived the study concept and design, analyzed and interpreted the data, and coordinated and drafted the manuscript. A Kumabe, KK, YU, TT, YY, YH, and A Kitao participated in the acquisition of subjects and data. MO conceived the study concept and design, drafted the manuscript, and corrected and restructured the manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work. All the authors read and approved the final manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
Ministry of Health, Labour and Welfare [webpage on the Internet]. Vital Statistics. 3. Trends in Leading Causes of Death in Summary of Vital Statistics. Statistics and Information Department Minister’s Secretariat Ministry of Health, Labour and Welfare, JAPAN. Available from: http://www.mhlw.go.jp/english/database/db-hw/. Accessed January 31, 2016. | ||
Teramoto S, Fukuchi Y, Sasaki H, et al; Japanese Study Group on Aspiration Pulmonary Disease. High incidence of aspiration pneumonia in community- and hospital-acquired pneumonia in hospitalized patients: a multicenter, prospective study in Japan. J Am Geriatr Soc. 2008;56(3):577–579. | ||
Komiya K, Ishii H, Umeki K, et al. Impact of aspiration pneumonia in patients with community-acquired pneumonia and healthcare-associated pneumonia: a multicenter retrospective cohort study. Respirology. 2013;18(3):514–521. | ||
Kenzaka T, Kumabe A, Kosami K, et al. Physicians’ opinions regarding the criteria for resuming oral intake after aspiration pneumonia: a questionnaire survey and cluster analysis of hospitals across Japan. Geriatr Gerontol Int. 2017;17(5):810–818. | ||
Japanese Respiratory Society. Aspiration pneumonia. Respirology. 2009;14(Suppl 2):S59–S64. | ||
Kohno S, Imamura Y, Shindo Y, et al. Clinical practice guidelines for nursing- and healthcare-associated pneumonia (NHCAP) [complete translation]. Respir Investig. 2013;51(2):103–126. | ||
Kenzaka T, Takeshima T, Kosami K, et al. Factors involved in the discontinuation of oral intake in elderly patients with recurrent aspiration pneumonia: a multicenter study. Clin Interv Aging. 2017;12:283–291. | ||
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2(7872):81–84. | ||
Committee for the Japanese Respiratory Society Guidelines for the Management of Respiratory Infections. Guidelines for the management of community acquired pneumonia in adults, revised edition. Respirology. 2006;11(Suppl 3):S79–S133. | ||
Lim WS, van der Eerden MM, Laing R, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58(5):377–382. | ||
Yamamoto M. Effectiveness of dysphagia therapy in patients with disuse syndrome, and factors influencing its effectiveness. Jpn J Logop Phoniatr. 2008;49(1):7–13. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.