Back to Journals » Clinical Ophthalmology » Volume 9
Effect of selective laser trabeculoplasty on macular thickness
Authors Koc M, Durukan I, Koban Y, Ceran B , Ayar O, Ekinci M, Yilmazbas P
Received 25 May 2015
Accepted for publication 7 August 2015
Published 15 December 2015 Volume 2015:9 Pages 2335—2338
DOI https://doi.org/10.2147/OPTH.S89221
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mustafa Koc,1 Irfan Durukan,2 Yaran Koban,3 Basak Bastanci Ceran,1 Orhan Ayar,4 Metin Ekinci,3 Pelin Yilmazbas1
1Department of Ophthalmology, Ulucanlar Eye Training and Research Hospital, Ankara, 2Ophthalmology Clinic, Kayserigoz Hospital Kayseri, 3Department of Ophthalmology, Faculty of Medicine, Kafkas University, Kars, 4Department of Ophthalmology, Faculty of Medicine, Bulent Ecevit University, Zonguldak, Turkey
Background: To investigate the effects of selective laser trabeculoplasty (SLT) on macular thickness change.
Methods: Forty eyes of 40 consecutive patients with uncontrolled primary open-angle glaucoma with medical treatment were included in this prospective study. SLT was performed to the inferior 180°, and macular thickness was measured. Data were collected before SLT, and 1 week and 1 month after SLT. Macular thickness evaluation was performed in five quadrants, the central 1 mm quadrant (fovea = F), the nasal 3 mm quadrant surrounding F (NQ), temporal quadrant, superior quadrant (SQ), and inferior quadrant (IQ). The preoperative and postoperative thicknesses were compared.
Results: There was an increase in macular thickness in the NQ, IQ, and SQ on the first week after SLT compared to preoperative measurements. On the other hand, there was no significant increase in the F and temporal quadrant. On the first month after SLT, thickness in the NQ, IQ, and SQ was back to preoperative measurements, and there was no significant change between the preoperative measurements in any quadrant.
Conclusion: There was no significant increase in macular thickness shortly after SLT in our study.
Keywords: complication, glaucoma, laser treatment, macula, optical coherence tomography
Introduction
Glaucoma is an important optic neuropathy that can lead to blindness. Meanwhile, lowering intraocular pressure (IOP) seems to be the main treatment option for slowing down the progression of glaucoma.1 There are a few options for lowering IOP: medical treatment, laser therapy, and surgery.2 Generally, a step-by-step approach is preferred for glaucoma treatment. If target IOP could not be obtained with medical treatment, or the patient has a poor compliance for the drops, laser trabeculoplasty is an option for the ophthalmologist. Moreover, if the target IOP could still not be obtained, surgery will be the final option.3
Laser trabeculoplasty is an efficient method in primary open-angle glaucoma (POAG) treatment.4 It decreases IOP by increasing trabecular outflow.5 Wise and Witter were the first to show that argon laser trabeculoplasty (ALT) lowered IOP.6 Afterward, krypton and diode lasers were used for trabeculoplasty, and similar results were obtained.7,8 On the other hand, histologic studies showed that these treatment modalities caused coagulation damage in trabecular meshwork, scarring, and synechiae formation, which lead to unsuccessful results when treatment needs to be repeated. In order to prevent these undesirable consequences, frequency-doubled, Q-switched neodymium:yttrium–aluminum–garnet (Nd:YAG) laser was used in 1995 instead. It was observed that this selectively affected the pigmented cells in trabecular meshwork and did not destruct nonpigmented cells and surrounding tissues. In this method, which was later named as selective laser trabeculoplasty (SLT), a lesser energy was applied compared to ALT and in short sequences as 3 seconds.9,10 Although the exact mechanism is not known, it is assumed that secretion of cytokines, induction of matrix metalloproteinase, formation of new cell populations, and activation of macrophage may play a key role in increasing the trabecular outflow.11 When compared to ALT, IOP lowering effects are similar, yet side effects are less and it is a safer method. Moreover, it can be repeated so that it can be applied as the first-line therapy or in addition to medical treatment of POAG.12,13
Although SLT is a safe and effective treatment of glaucoma, with greater cost-effectiveness than its pharmacological and surgical alternatives, cystoid macular edema (CME) has been reported after SLT treatment as case reports in the literature.14–16 Even not proven by some studies,17,18 Nd:YAG laser capsulotomy may also lead to CME.19,20 Although the target tissues for SLT and Nd:YAG laser capsulotomy are different, total amount of energy transferred to the eye is close to each other in these applications. Even though CME formation after capsulotomy was reported in previous studies, number of cases reported after SLT treatment is limited.
The purpose of this clinical study was to investigate the effects of SLT on macular thickness change.
Materials and methods
This prospective randomized clinical trial was conducted on 40 eyes of 40 consecutive patients with POAG who were examined between October and December 2012 at Kayserigoz Hospital. Either one of the eyes was chosen randomly if the patients had received bilateral treatment. Patients having a glaucoma type other than POAG, history of ocular surgery or trauma, macular disease, hypertension, or diabetes mellitus were excluded. Indications for SLT treatment were insufficient IOP control, allergy or discomfort to topical antiglaucoma medication, or noncompliance to topical treatment. Target IOP was determined using the Collaborative Initial Glaucoma Treatment Study formula.21 After getting signed informed consent from the patients, all patients received a full ophthalmic examination.
Baseline IOP was defined as the IOP measured immediately before performing SLT using a Goldmann applanation tonometer (Model AT 900, Haag-Streit USA, Mason, OH, USA). The macular thickness measurement was performed with optical coherence tomography (OCT, Model 3000; Carl Zeiss Meditec AG, Jena, Germany) after pupillary dilatation. Pupils were dilated with 1% tropicamide and 2.5% phenylephrine and then underwent OCT examination after waiting for 15 minutes. This study was approved by the Kafkas University Human Ethics Committee, Kars, Turkey, and adheres to the tenets of the Declaration of Helsinki.
We waited 1 day for the pupil to turn back to the miotic state. Next day, half an hour before SLT, eyes received one drop of brimonidine tartrate 0.15% (Alphagan P; Allergan Inc., Irvine, CA, USA). Topical anesthesia was obtained by proparacaine 0.5% (Alcaine; Alcon Laboratories, Inc., Fort Worth, TX, USA) eyedrops. Goniolens filled with 1% methylcellulose was placed in the eyes. SLT was performed to the inferior 180° with Selecta II (Lumenis, Palo Alto, CA, USA) device. Spot radius was 400 μm. Spot energy was adjusted, starting from 0.8 mJ and increasing by 0.1 mJ steps until the cavitation bubble was observed. Besides the medical treatment that was already started, fluorometholone (FML®; Allergan, Inc.) eyedrops were prescribed for everyday for 3 days. On the first day after treatment, anterior segment examination and IOP measurement were performed. On the first week and first month, besides ophthalmic examination, macular thickness of the patients were measured with OCT. Macular thickness evaluation was performed in five quadrants, the central 1 mm quadrant (fovea = F), the nasal 3 mm quadrant surrounding F (NQ), temporal quadrant, superior quadrant (SQ), and inferior quadrant (IQ) as described in the “Early Treatment Diabetic Retinopathy Study”.
Statistical analyses
The normal distribution of the data was checked using the Kolmogorov–Smirnov test.
For statistical analysis, SPSS 16.0 software for Windows (IBM Corporation, Armonk, NY, USA) was used to analyze outcomes. P-values <0.05 were considered to be statistically significant. The paired samples t-test was used for comparison of the parameters studied before and after SLT treatment.
Results
Sixteen of the total patients were male (40%), and 24 were female (60%). Eighteen right eyes (45%) and 22 left eyes (55%) were included for the analysis. The subjects were aged 53–75 years. Mean age of the group was 68.3±12.4 years.
Forty eyes of 40 patients with POAG were used for statistical analyses. Pretreatment and posttreatment LogMAR values were 0.45 (range, 0.20–0.95) and 0.50 (range, 0.30–1.00), respectively. The difference in visual acuity before and after IVB treatment was not significant (P=0.39).
The mean prestudy IOP was 16.3±3.4 mmHg on 2.2±0.8 eyedrops. The number of medications was significantly reduced at all time intervals following SLT when compared to the pretreatment level (P<0.0001). After laser treatment, the mean IOP was 12.2±2.2 mmHg while on 1.1±0.9 eyedrops.
Average spot size was 68.3±12.4 μm, and mean number of spots was 57±8 μm. The mean trabecular meshwork pigmentation was 1.48 (range, 0–3). There were no complications of any kind during and after the treatments. Anterior chamber reaction disappeared within 24 hours.
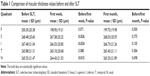
Table 1 demonstrates macular thickness before and on week 1 and month 1 after SLT in each quadrant and the comparison and P-values of macular thickness before SLT and 1 week and 1 month after SLT. According to this, there was an increase in macular thickness in the NQ, IQ, and SQ on the first week after SLT compared to preoperative measurements. On the other hand, there was no significant increase in the F and temporal quadrant. Even in the areas of quadrants where increase was observed, cystoid changes were not seen. On the first month after SLT, thickness in the NQ, IQ, and SQ was back to preoperative measurements, and there was no significant change between the preoperative measurements in any quadrant.
Discussion
SLT is accepted as a successful treatment modality for management of POAG; however, its order in treatment algorithm and role in different glaucoma types are not clearly displayed.22 Various amounts of IOP decrease were published according to the glaucoma type, usage of glaucoma drops, pigmentation of trabecular meshwork, and area where laser was applied (90°–360°). A meta-analysis recently published stated a 6.9%–35.9% decrease in IOP, which was similar to the results of ALT.23 But as mentioned earlier, since SLT causes less destruction on trabecular meshwork compared to ALT, it is tolerated better and can be reapplied.24
Complication rate of SLT is reported to be very low in the existing literature. Anterior chamber reaction, a temporary increase in IOP,13 hyphema,25 temporary or permanent corneal edema, haze, thinning,26 endothelial changes,27 choroidal effusion,28 and CME14–16 were the complications reported in a minority of patients.
Mechanism of CME formation is not fully understood. Blood–retina barrier is destructed, which leads to fluid accumulation between retinal layers. Branch and root vein occlusion, diabetic retinopathy, cataract surgery, and intraocular inflammation may induce CME formation.12 Wechsler and Wechsler observed CME after SLT in an eye with a history of complicated cataract surgery and a posterior chamber lens implant lacking the posterior capsule.14 SLT was applied to the inferior 180°, and a total of 40 mJ energy was applied. No inflammatory reaction was observed in the follow-up period. The CME was treated with nonsteroidal anti-inflammatory eyedrops and healed after 3 weeks of treatment. Similarly, Ha et al reported CME in a diabetic patient after SLT treatment.16
The purpose of our study was to investigate the effect of SLT on macular thickness. For this reason, we evaluated the change in macular thickness after SLT in six of the nine quadrants described by Early Treatment Diabetic Retinopathy Study. As a result, we observed an increase in NQ, SQ, and IQ in the postoperative first week. This result was not in harmony with the only existing literature, investigating the macular thickness change after SLT treatment published by Klamann et al.12 In their study, SLT was performed in 360°, and no anti-inflammatory drops were prescribed in the postoperative period. Macular thickness was evaluated in all nine quadrants in their study, and the follow-up period was 3 months. Klamann et al did not observe any significant increase during the follow-up period. There was no information regarding the patients’ medical history in their study. Having said that, we assume our patient cohort who had not had cataract surgery and who did not have any systemic diseases such as diabetes might have affected our results. Since some of the cases with CME after SLT in the existing literature had cataract surgery and had a history of diabetes, we may raise the question whether our patient cohort was different, we would have disparate results.
Conclusion
In conclusion, SLT is a safe and effective first-line or adjuvant treatment option, which can be repeated in POAG. Even though there are case reports presenting undesirable complications, side effects of this treatment modality are limited. We have observed a limited and temporary change in macular thickness after SLT treatment; however, prospective studies with larger patient groups, especially ones with a history of cataract surgery or systemic diseases, such as diabetes mellitus, are needed for further investigation of this matter.
Disclosure
The authors report that they have no competing interests in this work. The authors alone are responsible for the content and writing of the paper.
References
Leske MC, Heijl A, Hussein M, et al; Early Manifest Glaucoma Trial Group. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol. 2003;121:48–56. | ||
Ayala M, Chen E. Comparison of selective laser trabeculoplasty (SLT) in primary open angle glaucoma and pseudoexfoliation glaucoma. Clin Ophthalmol. 2011;5:1469–1473. | ||
McIlraith I, Strasfeld M, Colev G, Hutnik CM. Selective laser trabeculoplasty as initial and adjunctive treatment for open angle glaucoma. J Glaucoma. 2006;15:124–130. | ||
Samples JR, Singh K, Lin SC, et al. Laser trabeculoplasty for open-angle glaucoma: a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118:2296–2302. | ||
The Glaucoma Laser Trial Research Group. The glaucoma laser trial (GLT) and glaucoma laser trial follow up study: 7. Results. Am J Ophthamol. 1995;120:718–731. | ||
Wise JB, Witter SL. Argon laser therapy for open-angle glaucoma: a pilot study. Arch Ophthalmol. 1979;97:319–322. | ||
Spurny RC, Lederer CM. Krypton laser trabeculoplasty. A clinical report. Arch Ophthalmol. 1984;102:1626–1628. | ||
Chung PY, Schuman JS, Netland PA, Lloyd-Muhammad RA, Jacobs DS. Five-year results of a randomized, prospective, clinical trial of diode vs argon laser trabeculoplasty for open angle glaucoma. Am J Ophthalmol. 1998;126:185–190. | ||
Russo V, Barone A, Cosma A, Stella A, Delle Noci N. Selective laser trabeculoplasty versus argon laser trabeculoplasty in patients with uncontrolled open-angle glaucoma. Eur J Ophthalmol. 2009;19:429–434. | ||
Kramer TR, Noecker RJ. Comparison of the morphologic changes after selective laser trabeculoplasty and argon laser trabeculoplasty in human eye bank eyes. Ophthalmology. 2001;108:773–779. | ||
Kagan DB, Gorfinkel NS, Hutnik CM. Mechanisms of selective laser trabeculoplasty: a review. Clin Experiment Ophthalmol. 2014;42:675–681. | ||
Klamann MK, Maier AK, Gonnermann J, Ruokonen PC. Adverse effects and short-term results after selective laser trabeculoplasty (SLT). J Glaucoma. 2014;23:105–108. | ||
Realini T. Selective laser trabeculoplasty a review. J Glaucoma. 2008;17:497–502. | ||
Wechsler DZ, Wechsler IB. Cystoid macular edema after selective laser trabeculoplasty. Eye. 2010;24(6):1113. | ||
Wu ZQ, Huang J, Sadda S. Selective laser trabeculoplasty complicated by cystoid macular edema: report of two cases. Eye Sci. 2012;27(4):193–197. | ||
Ha JH, Bowling B, Chen SD. Cystoid macular oedema following selective laser trabeculoplasty in a diabetic patient. Clin Experiment Ophthalmol. 2014;42:200–201. | ||
Koucheki B, Hashemi H. Selective laser trabeculoplasty in the treatment of open angle glaucoma. J Glaucoma. 2012;21:65–70. | ||
Wong MO, Lee JW, Choy BN, Chan JC, Lai JS. Systematic review and meta-analysis on efficacy of selective laser trabeculoplasty in open-angle glaucoma. Surv Ophthalmol. 2015;60(1):6–50. | ||
Hong BK, Winer JC, Martone JF, Wand M, Altman B, Shields B. Repeat selective laser trabeculoplasty. J Glaucoma. 2009;18:180–183. | ||
Rhee D, Pasquale LR. Hyphema following selective laser trabeculoplasty. Ophthalmic Surg Lasers Imaging. 2009;40:493–494. | ||
Musch DC, Lichter PR, Standardi CL. The Collaborative Initial Glaucoma Treatment Study: study design, methods, and baseline characteristics of enrolled patients. Ophthalmology. 1999;106:653–662. | ||
Regina M, Bunya VY, Orlin SE, Ansari H. Corneal edema and haze after selective laser trabeculoplasty. J Glaucoma. 2011;20:327–329. | ||
Lee JW, Chan JC, Chang RT, et al. Corneal changes after a single session of selective laser trabeculoplasty for open-angle glaucoma. Eye. 2014;28:47–52. | ||
Kim DY, Singh A. Severe iritis and choroidal effusion following selective laser trabeculoplasty. Ophthalmic Surg Lasers Imaging. 2008;39:409–411. | ||
Giocanti-Aurégan A, Tilleul J, Rohart C, et al. OCT measurement of the impact of Nd:YAG laser capsulotomy on foveal thickness. J Fr Ophtalmol. 2011;34:641–646. | ||
Lewis H, Singer TR, Hanscom TA, Straatsma BR. A prospective study of cystoid macular oedema after neodymium:YAG laser posterior capsulotomy. Ophthalmology. 1987;94:478–482. | ||
Steinert RF, Puliafito CA, Kumar SR, Dudak SD, Patel S. Cystoid macular oedema, retinal detachment, and glaucoma after Nd:YAG laser posterior capsulotomy. Am J Ophthalmol. 1991;112:373–380. | ||
Billotte C, Berdeaux G. Adverse clinical consequences of neodymium:YAG laser treatment of posterior capsule opacification. J Cataract Refract Surg. 2004;30:2064–2071. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.