Back to Journals » Patient Preference and Adherence » Volume 12
Effect of different methods for estimating persistence and adherence to new glucose-lowering drugs: results of an observational, inception cohort study in Portugal
Authors Torre C , Guerreiro J, Longo P, Raposo JF , Leufkens H, Martins AP
Received 10 April 2018
Accepted for publication 29 May 2018
Published 17 August 2018 Volume 2018:12 Pages 1471—1482
DOI https://doi.org/10.2147/PPA.S170134
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Carla Torre,1,2 José Guerreiro,1 Patrícia Longo,1 João Filipe Raposo,3,4 Hubert Leufkens,5 Ana Paula Martins2,6
1Centre for Health Evaluation & Research (CEFAR), National Association of Pharmacies, Lisboa, Portugal; 2Research Institute for Medicines (iMed.ULisboa), Faculty of Pharmacy, University of Lisbon, Lisboa, Portugal; 3Nova Medical School, New University of Lisbon, Lisboa, Portugal; 4Portuguese Diabetes Association (APDP), Lisboa, Portugal; 5Division of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, Utrecht University, Utrecht, the Netherlands; 6Faculty of Pharmacy, University of Lisbon, Lisboa, Portugal
Purpose: Several methods have been developed for assessing medication-taking behavior; understanding the determinants and variability in estimates obtained is crucial in interpreting results. We estimated persistence and adherence levels to new glucose-lowering drugs (GLDs) in type 2 diabetes mellitus (T2DM) patients using different methods: through the collection of pharmacy records and combining pharmacy records with self-reported data.
Methods: We conducted a prospective observational cohort study of T2DM patients initiating a new GLD. Data were collected at baseline through interviews (demographic and clinical data). Follow-up data included pharmacy records (refill dates and medication possession) and telephone questionnaires (self-declared monitored GLD refill in another pharmacy, reasons for drug withdrawal). The cohort was divided into incident and prevalent new users. Persistence and adherence (proportion of days covered) were estimated for patients using pharmacy records exclusively (Method 1) and ≥1 self-declared statement of being persistent (Method 2). Log-rank tests were used to compare Kaplan–Meier curves of time to nonpersistence.
Results: A total of 1,328 patients were recruited. When considering Method 1, 38.7% (95% confidence interval [95% CI]: 36.0–41.5) of patients were persistent, whereas combining with self-reported information, this estimate increased to 65.6% (95% CI: 62.9–68.2). Using Method 1, the risk of persistence failure was associated with using an oral GLD, living alone and living in a suburban/urban setting. Three hundred and twenty-seven (24.8%) patients stopped to use the inception GLD.
Conclusion: Regardless of the method used, results indicated low levels of persistence and adherence to a new GLD; however, when combining self-reported information, higher estimates were obtained. Considering pharmacy records exclusively, prevalent new users, who were more complex patients in terms of T2DM disease but more likely to be pharmacy-loyal patients, were significantly more adherent than the incident new users. Barriers and reasons leading to GLD withdrawal, namely adverse drug event management, should be addressed, since they represent half of the reasons for treatment switching or discontinuation.
Keywords: type 2 diabetes mellitus, medication use behavior, discontinuation, daily practice
Introduction
Type 2 diabetes mellitus (T2DM) is a serious illness, leading to severe complications1,2 and increased mortality.3 Considering the demographic trends, diabetes prevalence is expected to rise to >690 million people by 2,045, posing a major health concern to many countries worldwide.4 Portugal is no exception,5 and according to the International Diabetes Federation figures, is one of the countries with the highest prevalence of this condition in Europe.6
Achieving and maintaining glycemic control as a primary treatment goal is challenging. In general, T2DM treatment is carried out in a stepwise manner, initially with lifestyle modifications, followed by metformin, and subsequently by adding another glucose-lowering drug (GLD).7,8 Although it is recognized that persistence and adherence to medication is crucial to obtain optimal clinical outcomes,9,10 studies have shown that recommended glycemic goals are achieved by <50% of patients, suggesting poor levels of these metrics.11
Several new GLDs, such as dipeptidyl peptidase-4 inhibitor (DPP-4), glucagon-like peptide-1 (GLP-1) and sodium–glucose co-transporter 2 inhibitors, have recently been marketed, enabling physicians to tailor therapy through a range of combination strategies. In order to target these new agents to T2DM patients in actual clinical practice, it is essential to monitor and understand the use behavior outside of a clinical trial setting.12 This is especially relevant among treatment-experienced patients13 where information is scarce, as published studies usually come from treatment-naïve or selective T2DM patients’ groups with strict eligibility criteria, which represent only a small part of the real-life user population.14
Efforts to accurately measure and improve persistence and adherence have received increased attention from health systems. Several methods and measures have been proposed using different data sources and definitions analysis; hence, understanding the variability in obtained estimates is crucial in interpreting the results.15–17 Unlike much of the existing GLD persistence and adherence studies, which used secondary data known to be often poor in covariates, namely large claims databases,11,18,19 we used primary data originally collected for this research purpose, thus taking increased control over available information.20–23
We estimated persistence and adherence levels using two methods (the collection of pharmacy records and their combination with self-reported information on medication use behavior), within 6 months of initiating treatment with a new GLD. Additionally, we examined reasons for switching or discontinuation and identified potential factors associated with nonpersistence and nonadherence among different GLD user profiles. This study was conducted in Portugal, which is one of the European countries with the highest consumption rate of novel GLD,24 and where, unlike many other countries, pharmacy records are not centralized.
Methods
Study design, setting and population
An intensive monitoring design, defined as an observational, prospective cohort study of adult T2DM patients initiating one of the recently launched GLDs (inception cohort), recruited by community pharmacies, was conducted between November 15, 2014 and November 30, 2015. Invitation letters were sent to all pharmacies from the National Association of Pharmacies that satisfied the inclusion criteria (ie, required software, participation in at least one research study in the previous 4 years and had an average daily sale of ≥1 DPP-4/GLP-1 package) (n=1,979; 67.8% of all Portuguese pharmacies). The pharmacists who agreed to participate were invited to attend a training session in which the study was explained.
The eligible study population consisted of first users of the new GLD (defined as users who did not take the inception-monitored drug within the 6 months prior to recruitment, as self-reported by the patients) that were that were reimbursed in Portugal at the time of enrollment: DPP-4 (sitagliptin, vildagliptin, saxagliptin and linagliptin) alone or in fixed-dose combination with metformin, GLP-1 (liraglutide and exenatide) or SLGT-2 (dapagliflozin). In this context, the inception drug corresponded to the GLD within the monitored therapeutic classes (DPP-4, GLP-1 or SLGT-2) which the patient was identified with at cohort entry. As previously proposed by Suissa et al,13 our study cohort was divided into two subgroups on the basis of participants’ T2DM treatment experience: subgroup 1 – incident new users (patients who used one of the monitored drugs for the first time [inception drug] and had no prior experience with DPP-4, GLP-1 or SLGT-2) and subgroup 2 – prevalent new users (patients who had previously used at least one GLD of the monitored antidiabetic drug classes [DPP-4, GLP-1 or SLGT-2], but not the inception-monitored drug). For the eligible subjects who did not wish to participate, information regarding age group and gender was collected through a refusal log form.
Data collection
Data were collected through three different sources. At baseline, patients had a structured face-to-face interview with a pharmacist to collect the sociodemographic (birth date, gender, highest educational level completed, co-residence status and number of people living in the subject’s household), anthropometrics (weight and height were measured at enrollment by pharmacy staff in order to calculate the body mass index [BMI] which was categorized as underweight: <18.50 kg/m2, normal: 18.50–24.99 kg/m2, overweight: 25.0–29.9 kg/m2 and obese: ≥30 kg/m2) and clinical characteristics (age at time of T2DM diagnosis, usual diabetes outpatient clinical care [eg, primary care, hospital-specialized diabetes care appointments, private practice], T2DM treatment [dose and prescribed posology of inception GLD and other current and past treatments], diabetes-related complications [eg, retinopathy, nephropathy, diabetic foot], comorbidities and concomitant therapy).
Over the study period, data regarding persistence and adherence (eg, refill dates and medication possession) were collected by an electronic data capture system developed for the electronic extraction of pharmacy records, from the pharmacy where the participant was recruited. Follow-up data also included structured telephone questionnaires conducted 2 weeks, 3 months and 6 months after the reported index date (starting date of the inception-monitored GLD), where information about the real pattern of use was asked. When the subjects were identified as potentially nonpersistent through the pharmacy records database (which was checked prior to each telephone questionnaire administration), the questions for confirmation of nonpersistence status (eg, acquisition of inception GLD from a different pharmacy, and if yes, the number of packages refilled and the corresponding refill dates) were asked. If the patients confirmed inception GLD withdrawal, reasons for drug discontinuation or switching (defined as withdrawal of monitored drug and initiation of another GLD) were collected (eg, adverse drug events conceivably considered to be associated with the use of inception drug, physician’s decision, economic reasons and poor glycemic control, among other reasons). In the case of switching, information about the new GLD prescribed was recorded. To minimize the potential recall bias, a maximum 4-week period was allowed to obtain responses from the telephone questionnaires. However, the patient would still be invited to complete the following questionnaire if a response was not obtained within this period. Follow-up ceased whenever a patient confirmed switching or discontinuation of the inception GLD.
Data analysis
Discrete variables were summarized by absolute and relative counts. Continuous variables were summarized using central tendency measures and dispersion (mean and standard deviation [SD]; median and interquartile range [IQR]). Chi-square test or Fisher’s exact test was used to compare the characteristics between subgroups, as well as the distribution of refusals with the distribution of participants.
Overall persistence and adherence were calculated through two different methods: Method 1 – using pharmacy records exclusively and Method 2 – using pharmacy records and their combination with patients’ self-reported data on persistence collected during the telephone follow-up questionnaires (inception GLD refilled in a different pharmacy). The proportion of pharmacy-loyal patients, defined as those who always refilled the inception GLD at the same pharmacy, was calculated.
Persistence was defined as the accumulation of time from initiation to withdrawal (switching or discontinuation) of the monitored treatment, based on the number of consecutive days of inception GLD dispensed to the subject through pharmacies within a grace period of 30 days (after the supply from the previous prescription was exhausted). A nonpersistent subject was defined as one who missed prescription cycles according to the definition of persistence and was considered nonpersistent for the remainder of the study period, regardless of whether the subject had refilled the inception GLD for the subsequent months. In Method 2, self-reported information on the number of packages refilled and the refill dates was used. Time to nonpersistence was calculated as the time in days between the index date and the last day the patient was still classified as persistent. The refill interval considered in the analysis was calculated using the baseline information of the real prescribed posology, when available. Whenever that information was missing, we used the information provided by the drug’s summary of product characteristics. Patients were censored in the survival analysis if they were lost to follow-up (subjects who could not be reached by telephone or those who withdrew consent), died or were hospitalized.
Kaplan–Meier (KM) curves, 95% confidence interval (CI) and log-rank test were computed to compare the time to nonpersistence between subgroups. A sensitivity analysis was conducted for both methods using a grace period of 14 days. Cox models were used to explore potential factors that could contribute to time to nonpersistence. Univariate and multivariate hazard ratios (HRs) were computed and Wald’s 95% CI presented. In the multivariate model-building strategy, KM curves for all covariates were plotted univariately, as the first step. Subsequently, a stepwise selection was implemented (significance levels of 0.20 and 0.25 for a variable to enter and to stay in the model, respectively). Model diagnoses comprised the computation of likelihood ratio, Wald and score Chi-square statistics and the variance inflation factor (VIF). In-depth residuals analysis, including plots with the scaled Schoenfeld residuals, was performed, the latter to assess proportional hazards assumption.
Adherence was computed for each participant based on the proportion of days covered (PDC). PDC was calculated as the number of days of medication supplied within the refill interval divided by the number of days of the observation period. By calculating the PDC, the proportion of days for which the inception GLD was available during the observation period was assessed. Overlapping refill days were moved forward to the first day that the patient would not have medication from the previous dispensing. In Method 2, self-reported information on the number of packages refilled and refill dates was used to estimate adherence. A patient was classified as adherent when PDC was ≥80%.15,25,26 Patients were excluded from the analysis if they were lost to follow-up, died, were hospitalized or stopped the inception GLD after a physician’s decision. Adherence level estimates were compared between subgroups. A sensitivity analysis was performed to take into consideration patients who stopped the inception GLD by physician decision, and new estimates of adherence levels were obtained including these patients. Logistic regression was used to explore the factors associated with nonadherence. Univariate and multivariate odds ratio (OR) and Wald’s 95% CI were estimated. In the model-building strategy, all variables were evaluated univariately, as the first step. Subsequently, a stepwise selection was implemented (significance levels of 0.20 and 0.25 for a variable to enter and to stay in the model, respectively). Model diagnoses comprised the calculation of Hosmer and Lemeshow goodness-of-fit test and VIF. In-depth residuals analysis including plots with deviance residuals was performed.
All tests were two-sided and the statistical significance level adopted was 5%. Data analysis was performed using SAS® software.
Ethics and data protection
This study was approved by the Portuguese Data Protection Authority (5339/2014) and by the Ethics Committee of the Institute of Public Health of the University of Porto (CE14021), and was conducted in accordance with the ethical principles stated in the Declaration of Helsinki. A written, signed informed consent form was obtained from all participants prior to initiation of any study procedures. This study was registered in the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance E-register of studies (ENCEPP/SDPP/8433).
Results
Pharmacies and patients flow
A total of 670 (33.9%) pharmacies agreed to participate in the study, out of which 385 (19.5%) pharmacies recruited at least one patient. Regional (p=0.0974) and urban/suburban/rural setting (p=0.3716) distribution of pharmacies with recruited patients was similar to the national distribution of pharmacies, but participating pharmacies had significantly more pharmacists, in their staff (p<0.0001). A total of 1,569 patients were invited to participate, of whom 231 (14.7%) refused to participate and 10 were excluded because they did not satisfy the eligibility criteria. Compared to the study participants, refusals had similar (p>0.05) age and gender distributions. A total of 1,328 eligible patients were considered: 61.3% were incident new users and 38.7% were prevalent new users. Patient flow and the respective response rate per questionnaire are available in the Supplementary material.
Baseline population characteristics
Participants’ demographic and clinical characteristics are depicted in Table 1. Slightly more than half of the cohort were male (n=673; 50.7%) and the mean age was 64.1 (SD=11.4) years. Approximately two-thirds (66.7%; n=865) had only completed 9 years of education, and 84.3% were living in household with at least two people (n=1,115). At cohort entry, the median BMI and T2DM duration were 30.1 (IQR=26.8–33.7) kg/m2 and 8.0 years (IQR=3.0–15.0), respectively. About one-quarter (n=317; 24.1%) of patients self-reported having at least one diabetes-related complication, with retinopathy (n=225; 17.1%) being the most frequent. Prevalent new users reported a significantly higher T2DM duration, prevalence of diabetes-related complications and follow-up by a specialist diabetes physician at hospital, compared with incident new users.
  | Table 1 Participants’ baseline demographic, anthropometric and self-reported clinical characteristics |
In addition to T2DM, 88.7% (n=1,176) self-reported having chronic illnesses, with hypertension (71.8%; n=952) and dyslipidemia (55.9%; n=741) being the most frequent. No statistically significant differences were found between subgroups regarding the most common chronic illnesses and the number of different medicines taken in addition to T2DM treatment.
Results showed that 9.7% (n=128) of patients were treatment-naïve for T2DM, 66.6% (n=884) were receiving other antidiabetic therapy than the inception GLD and 18.7% (n=248) were currently taking insulin. Overall, prevalent new users were significantly more likely to receive another antidiabetic therapy, including insulin, compared with incident new users. A total of 905 (68.2%) patients reported having changed (including switching, discontinuation or intensification with a fixed-dose combination) T2DM medication prior to recruitment.
Persistence and potential factors associated with time to nonpersistence
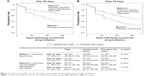
KM analysis (Figure 1) showed that overall persistence to the inception GLD, which was estimated exclusively with electronic data from pharmacy records (Method 1), was 38.70% (95% CI: 35.98–41.40), whereas including patient self-reported information on persistence (Method 2) was 65.61% (95% CI: 62.91–68.16). In both estimates, persistence rates were similar between cohort subgroups (p>0.05). Sensitivity analysis using a 14-day grace period revealed lower levels of persistence estimates; however, no differences were observed between subgroups irrespective of the method used. Differences were found in the level of pharmacy loyalty, whereas significantly (p=0.0035) higher proportion of loyal patients was found within the prevalent new users subgroup (67.5% of prevalent new users and 32.6% of incident new users were considered loyal patients).
In the multivariate Cox analysis, differences were found between the two methods regarding the factors associated with the risk of persistence failure (Table 2). When considering pharmacy records exclusively, patients living alone (HR=1.302; 95% CI: 1.058–1.602) and living in urban/suburban setting (HR=1.580; 95% CI: 1.134–2.203) had a significantly higher risk of persistence failure. Conversely, subgroup with GLP-1 inception-monitored treatment patients had a significantly lower risk of persistence failure than patients using an inception oral GLD. Analysis combining both pharmacy records and self-reported information showed that increasing age was the only factor significantly associated with the risk of persistence failure (1.6% increase in risk of persistence failure for every 1-year increase in age).
Over the study period, a total of 327 (24.8%) patients stopped using the inception GLD: 186 (22.9%) incident and 141 (27.4%) prevalent new users. Withdrawal rates were similar (p=0.0591) between subgroups. The most reported reasons given for inception GLD withdrawal were physician decision (61.5%), followed by adverse drug event (ADE) (53.5%), poor glycemic control (23.2%) and patient decision (7.3%). One ADE met the criteria of seriousness (hospitalization) and was reported to the national spontaneous reporting system, where it was handled according to the regulations regarding serious reports. Treatment switching recommended by physician was recorded for 137 (41.8%) cases who stopped inception GLD (93 DPP-4 alone or in fixed-dose combination with metformin, 31 dapagliflozin, eight exenatide and five liraglutide). Among patients administered DPP-4 alone or in fixed-dose combination with metformin, it was noted that 50.5% (n=47) switched within the same drug class, whereas among dapagliflozin inception users, 29.0% (n=9) and 25.8% (n=8) switched to fixed-dose combinations of DPP-4 with metformin and insulin, respectively.
Adherence and potential factors associated with nonadherence
At the end of the study, when adherence estimates considered patient self-reported information (Method 2), 73.6% (95% CI: 70.9–76.3) of participants were adherent (PDC ≥80%). No significant differences were observed between subgroups (p=0.1614). However, when adherence rates were estimated exclusively considering electronic data from pharmacy records (Method 1), a significant higher proportion of nonadherents was found among incident new users (p=0.0112; Table 3). Adherence sensitivity analysis (patients who stopped the inception drug due to physician decision were included) revealed lower levels of adherence estimates (Method 1: 35.9% [95% CI: 33.8–39.2]; Method 2: 63.9% [95% CI: 63.5–64.6]), yet no differences were observed between subgroups irrespective of the method used. In the multivariate regression analysis, although differences were found between the two methods, factors associated with nonadherence (Table 4) were overall similar with those found in the risk of persistence failure analysis. In both methods, living alone and using an oral inception GLD were factors associated with nonadherence.
  | Table 3 Adherence to inception-monitored glucose-lowering drug |
Discussion
Contrasting with most published studies that use claims databases to measure persistence and adherence, we used an intensive monitoring design that collected information from the first day of drug use and explored the differences between two methods, namely pharmacy records and their combination with patient self-reported data, each yielding different estimates. The use of patient self-reports also allowed us to explore the important features of medication-taking behavior, namely reasons for treatment switching or discontinuation, which are not often captured in administrative databases. As with other chronic diseases, low persistence rates for new GLD were found: 38.7% considering information exclusively from pharmacy records and 65.6% in combination with self-reported information. Almost two-thirds of patients were identified as nonadherent when considering pharmacy records exclusively, which decreased to almost one-quarter of patients, when including patient self-reported data.
Overall, considering the persistence and adherence estimates obtained in this study, together with sensitivity analysis results, we believe that the “true” persistence/adherence rates reported for the new GLD might possibly be between the lower limit of estimates retrieved from pharmacy records exclusively and the upper limit of estimates retrieved from the combination of pharmacy records and patient self-reported information. From this perspective, it is assumed that, on the one hand, patient self-reported information on medication-taking behavior could overestimate the results. On the other hand, over a 6-month period, given that, in Portugal, patients can go to more than one pharmacy and there is no single database that records all prescription refills from different pharmacies at an individual patient level, estimates retrieved exclusively from pharmacy records could be underestimated. More than one-third of patients who started the monitored GLD self-declared at least one refill in a different pharmacy where they were recruited.
Regardless of these assumptions, at 6 months from therapy initiation, persistence and adherence rates observed, although very low, were in line with, or to some extent lower than, the existent literature. A recent systematic review of observational studies revealed a persistence mean rate to T2DM medication of 56.2% (95% CI: 46.1–66.3).27 However, it should be noted that the included studies in the review had a longer follow-up period than our study, and pharmacy or prescription records data used in the studies were centralized. Concerning adherence, in another recent systematic review of 27 studies published between 2003 and 2014,28 it was found that the levels ranged from 38.5% to 93.1%, based on surveys on specific instruments or on claims databases. When considering only studies that used the medication possession ratio methodology (in general, for a follow-up duration of 12 months), the prevalence of adherence ranged between 46.0% and 89.8%.
With regard to factors that could contribute to nonpersistence and nonadherence, irrespective of the differences found between each method, they were broadly in line with what has been described in previous studies elsewhere. When combining pharmacy records with patient self-reported information, it was observed that increasing age was the only factor associated with persistence failure risk.11 Yet, when analyzing pharmacy records only, patients living alone,29 living in a suburban/urban setting30,31 and using an oral inception GLD had a higher risk of persistence failure. The later disputes findings from previous studies,32,33 although comparison studies using the new GLD for persistence and adherence, are scarce due to its recent availability in the market.
The overall clinical demographics of our study participants were generally similar to a large Portuguese T2DM patient cohort analyzed in 2013, in a primary care setting. From the data available, we found that our study population had comparable gender distribution, mean age and similar distribution regarding the most frequent comorbidities.34 The prevalent new users subgroup, representing almost two-fifths of all participants, had a significant higher T2DM duration, a higher prevalence of diabetes complications, use of insulin and use of specialist care visits, compared with incident new users. This was not surprising, as T2DM is a progressive condition, and therefore, prevalent new users are more likely to be complex patients.35,36
Given the differences observed in T2DM characteristics between incident and prevalent new user subgroups, we would expect dissimilar persistence and adherence results. However, rates estimated through the two methods were comparable overall. Only adherence estimates considering pharmacy records exclusively showed that prevalent new users (46.3%; 95% CI: 41.3–51.2) were significantly (p=0.0112) more adherent than incident new users (38.23%; 95% CI: 34.5–42.0). This could be explained partially by the fact that a significantly higher proportion (almost double: 67.5% versus 32.6%) of pharmacy-loyal patients was found among the prevalent new user subgroup. Our findings are consistent with the literature. In a recent study conducted in the Canadian province of Quebec, it was observed that pharmacy-loyal patients were more likely to be adherent (PDC≥80%) with T2DM medication (OR=1.22; 95% CI: 1.19–1.26).37 The positive association between pharmacy loyalty and persistence or adherence has also been demonstrated with other therapeutic groups, such as that including antipsychotic treatment38 and cardiovascular medication.39 Similarly, a study from the USA that included older adults with Medicare Part D demonstrated that filling prescriptions at multiple pharmacies, which was a prevalent phenomenon (38.1% of beneficiaries), was associated with lower medication adherence across a range of chronic medications.40
Over the study period, almost one-quarter of participants stopped using the inception GLD. These results are slightly lower than some reports from other studies, where a higher stopping rate of 31.4% was found.27 Our study adds information on commonly reported reasons for discontinuation from the patients’ perspective, which are not frequently captured in database studies. Physician decision, followed by ADE and reported poor glycemic control, was the most frequent reason stated for interrupting the inception GLD. It should be emphasized that among patients who stopped the inception GLD due to physician decision, only 67% switched to another antidiabetic drug, commonly the drug they were taking prior to recruitment. In these cases, conflicting decisions between doctors (primary care versus specialists) were frequently the reason, as some patients in our study declared. Addressing early risk of treatment failure for the new GLD should be put in place, and improvements in patient–health care provider communication as well as between health care providers are required. Furthermore, proactive management of ADE, including those which are expected and transient, but which may lead to unnecessarily early therapy discontinuation, should be a priority. In particular, clinicians should closely monitor patients with previous discontinuations related to ADE, because it is assumed that these patients might have an increased susceptibility to ADE compared to others.41
The results of the present study should be viewed in light of the following limitations. First, although it has been demonstrated that patients’ self-reported GLD utilization patterns are reliable,42 the use of self-reported information to ascertain medication-taking behavior could be biased by a reluctance to admit inappropriate behavior (social desirability bias); hence, a potential misclassification bias of patients being classified as persistent should be considered. Notwithstanding, inaccuracies in self-reported information are believed to be minimized, since independent research interviewers and not patients’ health care providers were responsible for conducting the follow-up interviews.43,44 Even when including patient self-reported information, the rates found were still very low; that is to say, the majority of patients did not show reluctance to declare they had stopped taking the medication. Second, persistence estimates were calculated on an individual drug level, and the impact of switching to other antidiabetic medication during the study period was not assessed.
Despite the mentioned limitations, this study has several strengths. Data presented were collected through a pharmacy-based intensive monitoring model, which is a noninterventional inception cohort study mirroring the real use of new GLD, prescribed by both general practitioners and specialists, with no limiting inclusion (with the exception of a T2DM treatment indication) or exclusion criteria compared with clinical trials. Further, although self-selection of pharmacies could have occurred since participation was not mandatory, it seems reasonable to assume that the study sample is representative of the overall country population of TDM2 patients taking new GLD, given the similarities found with the reference population and since pharmacies included were representative of the Portuguese pharmacies. Also, refusals had a similar age and gender distribution as compared to the study participants, and several strategies to minimize patients’ nonsystematic selection were put in place during the enrollment period (namely pop-up reminders at the pharmacy software whenever a new GLD was dispensed). Finally, this study provided a good source for persistence/adherence investigation because, on the one hand, data were collected directly from pharmacy dispensing, rather than physicians’ prescriptions that may never be dispensed. This is of relevance, as primary nonadherence is a frequent phenomenon: it was identified in almost a quarter of patients in both the USA45 and Portugal.46 On the other hand, as previously highlighted, patient self-reported usage data may well collect and explore the important features of medication use and behavior, namely reasons for treatment discontinuation, which are not captured in claims databases.47
Conclusion
Regardless of the method used, in case of pharmacy records or their combination with patient self-reported information, low levels of new GLD persistence and adherence were found. The combination of pharmacy records with self-reported information yielded higher estimates, even though they were in line with existent literature. Adherence estimates considering pharmacy records exclusively showed that prevalent new users, who were more complex in terms of T2DM disease but more likely to be pharmacy-loyal patients, were significantly more adherent than incident new users. Strategies to improve adherence and persistence should be implemented right from the commencement of therapy, and continuous attention should be given to nonserious ADE, since they represent half of the reported reasons for treatment switching or discontinuation.
Acknowledgments
The authors acknowledge all the community pharmacists and patients who voluntarily agreed to participate in this study.
Author contributions
CT was responsible for the implementation of the study, data analysis and drafting the manuscript. APM and HL had the original idea for the manuscript; they conducted and supervised the study and helped drafting the manuscript. JG and PL participated in data collection, analysis and revision of the manuscript. JFR participated in the collection of additional literature, contributed to the writing of the manuscript and revised it critically for important intellectual content. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Disclosure
CT was working at CEFAR/National Association of Pharmacies (ANF) when the study was performed and is currently employed by the Portuguese Pharmaceutical Society and has no conflict of interest to declare. JFR has received honoraria for consultancy or giving lectures from Merck Sharp & Dohme, Lilly and Novo Nordisk over the last year. All costs associated with the development and implementation of this study were fully supported by the Portuguese ANF. ANF had no role in study protocol, data analysis or interpretation of this study. The authors report no other conflicts of interest in this work.
References
Stratton IM. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. | ||
Turner RC, Millns H, Neil HAW, et al. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom prospective diabetes study (UKPDS: 23). Br Med J. 1998;316(7134):823–828. | ||
Campbell PT, Newton CC, Patel AV, Jacobs EJ, Gapstur SM. Diabetes and cause-specific mortality in a prospective cohort of one million U.S. adults. Diabetes Care. 2012;35(9):1835–1844. | ||
Cho NH, Shaw JE, Karuranga S, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. | ||
Pereira M, Carreira H, Lunet N, Azevedo A. Trends in prevalence of diabetes mellitus and mean fasting glucose in Portugal (1987–2009): a systematic review. Public Health. 2014;128(3):214–221. | ||
IDF. IDF Diabetes Atlas. Brussels: IDF; 2015. | ||
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38(1):140–149. | ||
Direcção-Geral da Saúde/Ministério da Saúde. Abordagem Terapêutica Farmacológica na Diabetes Mellitus Tipo 2 no Adulto [Pharmacological approach to type 2 diabetes mellitus in adults]. Norma da Direção-Geral da Saúde; 2015. Portuguese. | ||
Boye KS, Curtis SE, Lage MJ, Garcia-Perez LE. Associations between adherence and outcomes among older, type 2 diabetes patients: evidence from a Medicare Supplemental database. Patient Prefer Adherence. 2016;10:1573–1581. | ||
Currie CJ, Peyrot M, Morgan CL, et al. The impact of treatment noncompliance on mortality in people with type 2 diabetes. Diabetes Care. 2012;35(6):1279–1284. | ||
García-Pérez L-E, Álvarez M, Dilla T, Gil-Guillén V, Orozco-Beltrán D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther. 2013;4(2):175–194. | ||
Pratley RE. The efficacy and effectiveness of drugs for diabetes: how do clinical trials and the real world compare? Diabetologia. 2014;57(7):1273–1275. | ||
Suissa S, Moodie EEM, Dell’Aniello S. Prevalent new-user cohort designs for comparative drug effect studies by time-conditional propensity scores. Pharmacoepidemiol Drug Saf. 2017;26(4):459–468. | ||
Pawaskar M, Bonafede M, Johnson B, Fowler R, Lenhart G, Hoogwerf B. Medication utilization patterns among type 2 diabetes patients initiating Exenatide BID or insulin glargine: a retrospective database study. BMC Endocr Disord. 2013;13:20. | ||
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC. An empirical basis for standardizing adherence measures derived from administrative claims data among diabetic patients. Med Care. 2008;46(11):1125–1133. | ||
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. | ||
Choudhry NK, Shrank WH, Levin RL, et al. Measuring concurrent adherence to multiple related medications. Am J Manag Care. 2009;15(7):457–464. | ||
Roussel R, Charbonnel B, Behar M, Gourmelen J, Emery C, Detournay B. Persistence with insulin therapy in patients with type 2 diabetes in France: an insurance claims study. Diabetes Ther. 2016;7(3):537–549. | ||
Grabner M, Peng X, Geremakis C, Bae J. Demographic and clinical profiles of type 2 diabetes mellitus patients initiating canagliflozin versus DPP-4 inhibitors in a large U.S. managed care population. J Manag Care Spec Pharm. 2015;21(12):1204–1212. | ||
Suissa S, Garbe E. Primer: administrative health databases in observational studies of drug effects – advantages and disadvantages. Nat Clin Pract Rheumatol. 2007;3(12):725–732. | ||
Torre C, Martins A. Overview of pharmacoepidemiological databases in the assessment of medicines under real-life conditions. In: Current Perspectives on Research and Practice. In Tech; Nuno Lunet; Croatia. 2012:131–154. | ||
Park BJ, Stergachis A. Automated databases in pharmacoepidemiologic studies. In: Pharmacoepidemiology and Therapeutic Management. Cincinnati, OH: Harvey Whitney Books; 2008. | ||
Choudhry NK. Promoting persistence improving adherence through choice of drug class. Circulation. 2011;123(15):1584–1587. | ||
Torre C, Guerreiro J, De Oliveira Martins S, Raposo JF, Martins AP, Leufkens H. Patterns of glucose lowering drugs utilization in Portugal and in the Netherlands. Trends over time. Prim Care Diabetes. 2015;9(6):482–489. | ||
Vink NM, Klungel OH, Stolk RP, Denig P. Comparison of various measures for assessing medication refill adherence using prescription data. Pharmacoepidemiol Drug Saf. 2009;18:159–165. | ||
Karve S, Cleves MA, Helm M, Hudson TJ. Good and poor adherence: optimal cut-point for adherence measures using administrative claims data. Curr Med Res Opin. 2009;25(9):2303–2310. | ||
Iglay K, Cartier SE, Rosen VM, et al. Meta-analysis of studies examining medication adherence, persistence, and discontinuation of oral antihyperglycemic agents in type 2 diabetes. Curr Med Res Opin. 2015;31(7):1283–1296. | ||
Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: a systematic review. Diabet Med. 2015;32(6):725–737. | ||
Balkrishnan R. Predictors of medication adherence in the elderly. Clin Ther. 1998;20(4):764–771. | ||
Kim H, Kim HS, Bowman JD, Cho NH. Comparing diabetic patient characteristics related to stated medication adherence in a rural vs. urban community in Korea. J Clin Pharm Ther. 2016;41(1):40–46. | ||
Guénette L, Moisan J, Breton MC, Sirois C, Grégoire JP. Difficulty adhering to antidiabetic treatment: factors associated with persistence and compliance. Diabetes Metab. 2013;39(3):250–257. | ||
Cai J, Wang Y, Baser O, Xie L, Chow W. Comparative persistence and adherence with newer anti-hyperglycemic agents to treat patients with type 2 diabetes in the United States. J Med Econ. 2016;19(12):1175–1186. | ||
Cai J, Divino V, Burudpakdee C. Adherence and persistence in patients with type 2 diabetes mellitus newly initiating canagliflozin, dapagliflozin, dpp-4s, or glp-1s in the United States. Curr Med Res Opin. 2017;33(7):1317–1328. | ||
Laranjo L, Rodrigues D, Pereira AM, Ribeiro RT, Boavida JM. Use of electronic health records and geographic information systems in public health surveillance of type 2 diabetes: a feasibility study. JMIR Public Health Surveill. 2016;2(1):e12. | ||
Conget I, Mauricio D, Ortega R, Detournay B. Characteristics of patients with type 2 diabetes mellitus newly treated with GLP-1 receptor agonists (CHADIG Study): a cross-sectional multicentre study in Spain. BMJ Open. 2016;6(7):e010197. | ||
Fonseca VA. Defining and characterizing the progression of type 2 diabetes. Diabetes Care. 2009;32 (Suppl 2):S151–S156. | ||
Dossa AR, Grégoire JP, Lauzier S, Guénette L, Sirois C, Moisan J. Association between loyalty to community pharmacy and medication persistence and compliance, and the use of guidelines-recommended drugs in type 2 diabetes. Medicine (Baltimore). 2015;94(27):e1082. | ||
Zongo FE, Moisan J, Grégoire J-P, Lesage A, Dossa AR, Lauzier S. Association between community pharmacy loyalty and persistence and implementation of antipsychotic treatment among individuals with schizophrenia. Res Soc Adm Pharm. 2016;14(1):53–61. | ||
Choudhry NK, Fischer MA, Avorn J, et al. The implications of therapeutic complexity on adherence to cardiovascular medications. Arch Intern Med. 2011;171(9):814–822. | ||
Marcum ZA, Driessen J, Thorpe CT, Gellad WF, Donohue JM. Effect of multiple pharmacy use on medication adherence and drug–drug interactions in older adults with medicare part D. J Am Geriatr Soc. 2014;62(2):244–252. | ||
Hakobyan L, Haaijer-Ruskamp FM, de Zeeuw D, Dobre D, Denig P. A review of methods used in assessing non-serious adverse drug events in observational studies among type 2 diabetes mellitus patients. Health Qual Life Outcomes. 2011;9:83. | ||
Glintborg B, Hillestrøm PR, Holm Olsen L, Dalhoff KP, Enghusen Poulsen H. Are patients reliable when self-reporting medication use? Validation of structured drug interviews and home visits by drug analysis and prescription data in acutely hospitalized patients. J Clin Pharmacol. 2007;47(11):1440–1449. | ||
Garfield S, Clifford S, Eliasson L, Barber N, Willson A. Suitability of measures of self-reported medication adherence for routine clinical use: a systematic review. BMC Med Res Methodol. 2011;11(1):149. | ||
Kaplan RM, Simon HJ. Compliance in medical care: reconsideration of self-predictions. Ann Behav Med. 1990;12(2):66–71. | ||
Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25(4):284–290. | ||
da Costa FA, Pedro AR, Teixeira I, Bragança F, da Silva JA, Cabrita J. Primary non-adherence in Portugal: findings and implications. Int J Clin Pharm. 2015;37(4):626–635. | ||
Kalsekar I, Sheehan C, Peak A. Utilization patterns and medication adherence in patients with type 2 diabetes: variations based on type of pharmacy (chain vs independent). Res Soc Adm Pharm. 2007;3(4):378–391. |
Supplementary material
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.