Back to Journals » Journal of Pain Research » Volume 15
Effect of CT-Guided Gasserian Ganglion Block with Local Anesthetics and Steroids on Acute/Subacute Zoster-Related Trigeminal Neuralgia: A Multicenter Retrospective Study
Authors Sun Z, Liu L, Liu H, Luo F
Received 28 May 2022
Accepted for publication 29 July 2022
Published 10 August 2022 Volume 2022:15 Pages 2303—2313
DOI https://doi.org/10.2147/JPR.S375257
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ellen M Soffin
Zhe Sun,1,* Lu Liu,1,* Hongbing Liu,2 Fang Luo1,2
1Department of Day Surgery, Beijing Tiantan Hospital, Capital Medical University, Beijing, 100070, People’s Republic of China; 2Department of Pain Management, Beijing Tiantan Hospital, Capital Medical University, Beijing, 100070, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Fang Luo, Department of Pain Management, Beijing Tiantan Hospital, Capital Medical University, No. 119 West Road, South 4th Ring Road, Fengtai District, Beijing, 100070, People’s Republic of China, Tel +86 10 59976664, Fax +86 10 67050177, Email [email protected]
Purpose: To further evaluate the effects of gasserian ganglion block treatment with local anesthetics and steroids on patients with acute/subacute zoster-related trigeminal neuralgia.
Patients and Methods: This is a multicenteric retrospective study which included patients between the ages of 26– 92 years, who suffered from acute/subacute zoster-related trigeminal neuralgia and had undergone CT-guided gasserian ganglion block. The medical records of these patients between January 13, 2016 and August 25, 2021 were retrieved, and the patients were followed up for 6 months. Follow-up outcomes were Numerical Rating Scale (NRS) scores, medications and dosage. The effective rate was defined as the number of cases with NRS score reduction of > 50%/total number of cases× 100% at 12 weeks postoperatively.
Results: The postoperative NRS scores were significantly decreased in all patients (P < 0.05), and NRS scores in acute zoster group were lower than those in subacute zoster group at different time points (P < 0.05). The percentage of patients who had a reduction of medication use value of > 50% was 56.4% and the effective rate was 66.7% in all patients, at 3 months after the block treatment. There was no significant difference in the reduction of medication use value of > 50% and the effective rates between the two groups. There were no intracranial hemorrhage, infection or other serious adverse effects in either groups.
Conclusion: CT-guided gasserian ganglion block with local anesthetics and steroids can be an effective and safe technique to relieve the pain of acute/subacute zoster-related trigeminal neuralgia.
Keywords: acute/subacute zoster-related trigeminal neuralgia, gasserian ganglion block, local anesthetics, steroids, multicenter retrospective study
Introduction
Herpes zoster (HZ) is a vesicular skin rash caused by varicella zoster virus (VZV) latent in the ganglion, usually resulting in acute pain in the affected dermatome.1 The reactivation of VZV occurs when patient’s immunity is decreased due to risk factors, such as increasing age.2,3 The annual incidence of HZ is approximately 3.4 cases per 1000 persons;4 however, a cohort study indicated that the incidence of HZ might still be rising, more than four folds in the past 60 years.5 Trigeminal nerve is one of the most common cranial nerves infected by HZ,6 accounting for 16.3% of HZ patients.7 Acute zoster-related trigeminal neuralgia presents as facial pain within 30 days of zoster onset, characterized by severe burning pain and tingling in the skin of the innervated area, along with the occasional tearing or stabbing pain.8,9 Subacute zoster-related trigeminal neuralgia is described as facial pain from 31 to 90 days after zoster onset.8,9 Trigeminal postherpetic neuralgia (TPHN) is defined as dermatomal pain after zoster onset, resulting from acute and subacute zoster-related trigeminal neuralgia, which persists for over 3 months and is the most common and the most severe type. TPHN is a refractory chronic neuropathic pain resulting from HZ virus infection,10 which is accompanied by allodynia and hyperalgesia that may continue long after the resolution of mucocutaneous eruption.11 This severe chronic pain also leads to various socioeconomic consequences, including decreased socialization, daily activities and quality of life.12 Therefore, it is necessary to explore the optimal treatment for acute/subacute zoster-related trigeminal neuralgia and prevent further development of TPHN.
Consistent with the treatment of herpes-related pain in other parts of the body, treatment of acute/subacute zoster-related trigeminal neuralgia includes systemic drug therapy, local drug therapy, physical therapy and so on.13 For patients with acute/subacute zoster-related trigeminal neuralgia, where conservative treatment could not achieve satisfactory pain relief, pulsed radiofrequency (PRF) therapy can play an important role as a non- or minimally neurodestructive technique.10 However, the sample size of previous research is relatively small and there are very few reports available; therefore, evidences supporting their effectiveness are limited. Thus, once conservative treatment is ineffective, acute/subacute zoster-related trigeminal neuralgia is generally considered a challenge for clinicians, and more effective treatment modalities are needed.
Nerve block therapy has been reported as a technique for the treatment of zoster-related pain. The reduction of acute HZ pain can be achieved by blocking C-nociceptors and afferent transmission of pain stimulus using local anesthetics.12,14 Although much controversy surrounds the use of systemic steroids,15 the inclusion of steroid in the block decreases acute neuronal inflammation.16 Previous studies have demonstrated that, the closer to the site of inflammation the local anesthetic and the steroid are injected, the better the anti-inflammatory effect.16 Sympathetic or somatic nerve blocks during the acute phase of HZ may not only help control acute pain, allodynia and hyperalgesia but also prevent postherpetic neuralgia (PHN).17 In addition, favorable outcomes for epidural or paravertebral blocks have also been reported.18,19 However, only few reports on nerve block in the treatment of acute zoster-related trigeminal neuralgia are available. Philippe Gain performed daily frontal and/or nasal blocks with bupivacaine plus adrenaline added to clonidine, which relieved severe pain in acute ophthalmic zoster.20 Gasserian ganglion block and retrobulbar nerve block has previously been demonstrated as a useful method for treating pain and inflammation caused by herpes simplex virus infection of the ophthalmic division of the trigeminal nerve.2 Since only a few cases have been reported, these studies cannot provide standard guidelines for nerve block therapy for acute/subacute zoster-related trigeminal neuralgia.21 Gasserian ganglion is the largest cranial sensory ganglion, where the VZV can lie dormant.3 Gasserian ganglion is the affected target and can be treated as the therapeutic site in trigeminal HZ.2,10 In order to determine and provide guidance regarding a specific treatment, the analgesic effect of CT-guided gasserian ganglion block with local anesthetics and steroids in the treatment of acute/subacute zoster-related trigeminal neuralgia was analyzed retrospectively at multiple centers.
Materials and Methods
The retrospective research protocol was approved by the Medical Ethics Committee of Beijing Tiantan Hospital, Capital Medical University before collecting patients’ data (KY2022-049). This study was conducted in compliance with the Declaration of Helsinki. Patient data was strictly confidential and de-identified for analysis. This retrospective study involved no more than minimal risk to subjects, and the waiver of consent did not harm the welfare and rights of subjects. The Medical Ethics Committee of Beijing Tiantan Hospital approved the application for waiver of informed consent for this study. Patient informed consent was not required because of the study’s retrospective nature. A total of three hospitals, including Beijing Tiantan Hospital, Beijing Red Cross Peace Orthopedic Hospital and Beijing Puhua International Hospital Hospital in Beijing, China, served as participating centers. The medical records of patients with acute/subacute zoster-related trigeminal neuralgia, who had undergone CT-guided gasserian ganglion block treatment between January 2016 and August 2021, were retrieved from hospital information systems (HIS) medical records.
Study Design and Participants
This was a multicenteric retrospective study, without a control group, conducted at Beijing Tiantan Hospital, Capital Medical University. Patients who met the following criteria were eligible for study: (1) Age >18 years; (2) Patients with acute (within 30 days after zoster onset) and subacute zoster-related trigeminal neuralgia (at 30 to 90 days from zoster onset) who had undergone CT-guided nerve block treatment of gasserian ganglion alone or gasserian ganglion combined with peripheral nerve (supraorbital nerve, infraorbital nerve, mental nerve or multiple nerves combination). The exclusion criteria were as follows: (1) Patients with incomplete medical records (lack of baseline data or follow-up of less than 12 weeks after gasserian ganglion block procedure); (2) Patients with unhealed herpes.
Procedures
All gasserian ganglion block procedures were conducted by experienced pain physicians. Treatment was delivered with patients lying in supine position on the computed tomography (CT) scanner bed while receiving oxygen at 3 liters per minute. Electrocardiogram (ECG), heart rate (HR), blood pressure (BP), oxygen saturation and respiratory rate (RR) were monitored continuously. CT was used to determine the percutaneous puncture route. Gasserian ganglion block was performed after sterilization and local anesthesia with 1% lidocaine at the puncture site.
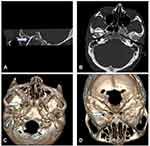
The puncture site was positioned approximately 3 cm lateral to the corner of the mouth. The Hartel anterior approach was performed for patients undergoing gasserian ganglion block. A disposable anesthetic needle (a 10-cm trocar, AN-S 0.7X90; Zhejiang volte medical Inc.) was inserted and slowly advanced toward the foramen ovale along a predefined path under the guidance of three-dimensional (3D) CT. The patient’s mouth was inspected to avoid inadvertent penetration of buccal mucosa at this point. A new CT scan was performed to confirm the location of the needle tip when the needle reached the predefined depth (Figure 1). Once the needle reached its proper location, the stylet of the trocar was withdrawn and the syringe with local anesthetics and steroids was connected. Two milligrams of dexamethasone sodium phosphate and 1 mL of 1% plain lidocaine (total volume 1.4 mL) were then slowly injected through the needle.2 The needle was finally flushed with 0.5 mL normal saline and then withdrawn. The gasserian ganglion block was occasionally combined with peripheral nerves such as supraorbital nerve, infraorbital nerve or mental nerve block in some patients, as deemed required by our experienced pain physicians.
Data Collection
Preoperative baseline characteristics, intraoperative records and postoperative efficacy were retrieved from HIS medical record system. Preoperative baseline data included gender, age and BMI of patients, affected side, affected branch, days after zoster onset, numerical rating scale (NRS) score, previous medications and dosage, related symptoms such as facial numbness and swelling along with comorbidities such as hypertension, diabetes mellitus (DM), coronary heart disease and stroke. Intraoperative data included operation time, whether combined with peripheral nerve block treatment, NRS score immediately after nerve block and intraoperative complications. HIS medical record system was routinely updated for medical quality control. Patients were routinely followed up at day 1, week 1, week 2, month 1, month 3 and month 6 postoperatively. Follow-up outcomes were NRS scores, medications and dosage.22 Patients could reduce the dose of analgesics on their own, based on their degree of pain. For patients who took more than one analgesic drug preoperatively, if the postoperative dose of each analgesic drug was reduced by more than 50%, the reduction of medication use value was considered to be ≥50%. The effective rate was defined as the number of cases with NRS score reduction of >50%/total number of cases×100% at 12 weeks postoperatively. The percentage of patients who had a reduction of medication use value of >50% were collected at 12 weeks postoperatively. Follow-up was terminated once the NRS score decreased to 0 without oral analgesics or when patients received other interventional or surgical treatments due to ineffective nerve block treatment. In addition, postoperative complications such as facial swelling, facial numbness, ecchymosis, decreased masticatory muscle strength, infection or hematoma at puncture site and intracranial hemorrhage or infection were also recorded by HIS medical record system or via telephone follow-up.
Statistical Analysis
Kolmogorov–Smirnov test was used to assess the normality of demographic data. Normally distributed continuous data were presented as means ± standard deviations (SDs) and analyzed by independent t-test. Non-normally distributed continuous data were presented as medians and interquartile ranges (IQRs) and analyzed by Mann–Whitney U-test. Categorical data were described as frequency and percentage and analyzed by Chi square test or Fisher’s exact test (when the expected values were <5). All tests were two-tailed, and P value <0.05 was considered statistically significant. All data were analyzed using IBM SPSS Statistics software (Version 26, IBM Inc., USA).
Results
A total of 123 patients with acute/subacute zoster-related trigeminal neuralgia who underwent CT-guided gasserian ganglion block at the study centers, were reviewed between January 2016 and August 2021. Of the 123 patients, 6 patients were excluded based on the exclusion criteria. Therefore, the medical records of 117 patients were used. Among the 117 patients, 36 patients had undergone gasserian ganglion block in the acute zoster group and 81 patients had undergone gasserian ganglion block in the subacute zoster group.
Baseline Characteristic
Preoperative and intraoperative baseline data of participants are summarized in Table 1. Mean time from the onset of pain to the initiation of CT-guided gasserian ganglion block was 39.5 days, 20.2 days in the acute zoster group and 48.1 days in the subacute zoster group. Sixteen patients (13.7%) suffered from preoperative facial numbness and 10 patients (8.5%) suffered from preoperative facial swelling. There were no significant differences between the two groups with regards to gender, age and BMI of patients, affected side, affected branch, comorbidities, preoperative NRS score, previous medications, related symptoms including facial numbness and swelling, operation time and the percentage of participants receiving gasserian ganglion block alone or combined with peripheral nerve block (Tables 1 and 2).
 |
Table 1 Preoperative Baseline Data |
 |
Table 2 Primary Outcome and Postoperative Recovery Situation |
NRS Score
The preoperative NRS score was 8.6, and the NRS scores immediately after block was 0 in all patients, probably due to the effect of local anesthetics. The postoperative NRS scores significantly declined at day 1, week 1, week 2, month 1, month 3 and month 6 after block treatment in all patients (P < 0.05) (Figure 2A). The postoperative NRS scores at each follow-up time points were lower in the acute zoster group compared to the subacute zoster group (P < 0.05) (Figure 2B).
Medication Use
The percentage of patients who had a reduction in medication use value of >50% was 41.0%, 49.6% and 56.4% at week 2, month 1, month 3, respectively, after the block treatment in all patients. There was no significant difference between the two groups (Table 3).
 |
Table 3 Reduction of Medication Use >50% at Each Follow-Up Time Point |
Effective Rate
The percentage of patients who had a reduction in NRS score value of >50% was 66.7% in all patients, 77.8% in the acute zoster group and 61.7% in the subacute zoster group at month 3 after the block treatment. There was no significant difference between the two groups (Table 4).
 |
Table 4 Effective Rate at Each Follow-Up Time Point |
Side Effects
During the operation, while the foramen ovale was being punctured, five patients (4.3%) suffered transient bradycardia. Eight patients (6.8%) suffered from increased facial numbness and six patients (5.1%) suffered from increased facial swelling. Nineteen patients (16.2%) suffered from facial ecchymosis; whereas hematoma at puncture site occurred in four patients (3.4%). There were no other perioperative adverse effects such as decreased strength of masticatory muscles, infection and intracranial hemorrhage. There were no significant differences in side effects between the two groups (Figure 3). None of the patients withdrew from study due to adverse reactions during treatment.
 |
Figure 3 Postoperative complications. Compared between acute zoster group and subacute zoster group, *P<0.05. |
Comparison of Gasserian Ganglion Alone or Combined with Peripheral Nerve Block
There were no significant differences in preoperative NRS scores, postoperative NRS scores at day 1, week 1, week 2, month 1, month 3, month 6, effective rate, intraoperative bradycardia and postoperative complications, whether combined with peripheral nerve block or not (Figures 4 and 5).
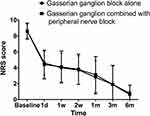 |
Figure 4 Postoperative NRS scores at each follow-up time point. Compared between the gasserian ganglion alone group and the gasserian ganglion combined with peripheral nerve block group, *P<0.05. |
 |
Figure 5 Postoperative complications. Compared between gasserian ganglion alone group and gasserian ganglion combined with peripheral nerve block group, *P<0.05. |
Discussion
Our study retrospectively reported the effect of CT-guided gasserian ganglion block in patients with acute/subacute zoster-related trigeminal neuralgia at multiple centers. Our results reveal that gasserian ganglion block can be a successful therapy with an effective rate of 66.7% in all patients at 3 months after the block treatment without serious complications. However, the effective rate must be acknowledged with caution due to the lack of a control group. Our results were consistent with Huang et al’s study,2 which demonstrated that, gasserian ganglion block could relieve pain in acute zoster-related trigeminal neuralgia patients. Different from Huang et al’s case report, our study retrospectively reported of 117 patients with acute/subacute zoster-related trigeminal neuralgia who had undergone CT-guided gasserian ganglion block treatment. In our study, we chose dexamethasone and lidocaine as drugs for nerve block instead of clonidine, bupivacaine and adrenaline, which was different from Gain et al’s research.20 However, the optimal drug formulation of gasserian ganglion block for the treatment of acute/subacute zoster-related trigeminal neuralgia needs to be investigated further in future studies.
In our study, pain disappeared immediately after nerve blocks in patients with acute/subacute zoster-related trigeminal neuralgia due to the effects of local anesthetic. The results of this study proved that the accuracy of puncture site and diagnosis of pain source affect the results of treatment significantly.10 The average NRS score decreased significantly at postoperative day 1, which was 52.3% of the preoperative NRS score in all patients. The results showed that nerve block reduced the degree of pain and took effect rapidly. The NRS scores continued to decline at postoperative week 1, week 2, month 1, month 3, month 6, which suggested that the degree of pain decreased continuously without recurrence after nerve block. Jeon et al23 believed that nerve block could effectively relieve acute sacral HZ pain, which was consistent with our results that nerve block provided fast and effective relief in acute/subacute zoster-related trigeminal neuralgia.
The average NRS score in the acute zoster group and the subacute zoster group decreased significantly at postoperative day 1, compared to the preoperative NRS scores, by 46.6% and 55.3% of, respectively. The results of this study revealed that the pain relief effects of gasserian ganglion block with local anesthetics and steroids in patients with acute zoster might be better than those in patients with subacute zoster. Our results were consistent with Fabian et al’ s study, which demonstrated that, the nerve damage of HZ was reversible inflammatory demyelinating change and early clinical treatment measures help relieve pain.24 However, there was no significant difference in effective rate between the two groups, which might be due to the small sample size of the study. In this study, only 36 patients (30.8%) were in the acute zoster group, while 81 patients (69.2%) were in the subacute zoster group. This composition ratio showed that most patients did not receive gasserian ganglion block treatment until the subacute stage. In the future, large-scale cross-sectional studies must be carried out to explore the correlation between early nerve block treatment and prognosis, so as to provide guidance for accurate clinical decision-making.
The percentage of patients who had a reduction of medication use value of >50% was 56.4% with an effective rate of 66.7% at month 3 after nerve block treatment in all patients. The study showed that some patients had lower NRS scores but not less medication use, which might be due to patients’ concern about pain recurrence after gasserian ganglion block. However, the results of our study must be acknowledged with caution due to the lack of a control group.
The effective rate of gasserian ganglion alone or combined with peripheral nerve block were 67.4% and 64.3% at month 3 after the block treatment, respectively. The results did not show that the treatment effect of gasserian ganglion combined with peripheral nerve block was better. However, these conclusions could only be acknowledged with caution because of the small sample size.
The mechanism of gasserian ganglion block in the treatment of acute/subacute zoster-related trigeminal neuralgia is not completely clear. Reactivation of VZV can lead to acute hemorrhagic inflammation in the corresponding dermatomes and neuronal damage,2,25 which causes change in the distribution and function of the transmembrane ion channels of sensory neurons.10 Abnormal electric impulses produced by sensory neurons induce spontaneous pain.10,26,27 Nerve blocks obstruct the vicious cycle of pain, block sympathetic nerve, expand nutrient vessels in the lesion area and improve neurotrophic status.28 Gasserian ganglion block provides sedative effect, which reduces the excessive excitation of sympathetic nerve and the release of neurotransmitters.9 Lidocaine makes the lesion area reach a painless state quickly and plays the role of muscle relaxant, vasodilator and improved microcirculation.29 Dexamethasone provides anti-inflammatory, analgesic and immunosuppressive effects and prolongs the effect time when combined with local anesthetics.30–33
The application of nerve block has been proven to be safe in the treatment of herpes zoster.18,19 Consistent with previous reports, all patients in this study had no drug-related serious adverse effects and all punctures were performed under CT guidance without puncture-related serious adverse effects. Bradycardia occurred in some patients while the foramen ovale was being punctured; all of whom recovered spontaneously without treatment. Facial numbness and facial swelling occurred in some patients preoperatively due to nerve injury. The percentage of patients with facial numbness and swelling were slightly increased after gasserian ganglion alone or combined with peripheral nerve block treatment, which suggested the presence of mild tissue damage caused by nerve block due to puncture. Facial ecchymoma and hematoma at puncture site might have been caused by injury to facial vessels such as maxillary artery during puncture. Fortunately, the incidence of side effects were very low, which gradually reduced or completely resolved during follow-up.
There are several limitations to our study. First, the conclusion of the study must be acknowledged caution due to the lack of a control group and a relatively smaller sample size. Prospective randomized controlled studies with larger sample size must be conducted to explore the effects of gasserian ganglion block on acute/subacute zoster-related trigeminal neuralgia. Second, NRS scores and medications of patients were followed up at different time points after gasserian ganglion block, but not at 3 months after zoster onset, so the accurate incidence of TPHN between the two groups could not be obtained. Third, the patients were followed up for 6 months after gasserian ganglion block. Future prospective studies with longer lengths of follow-up must be conducted. Fourth, in this study, CT guidance was used instead of fluoroscopy because CT images, especially 3D reconstruction images, were particularly intuitive and clearer for puncture guidance. However, fluoroscopy can guide punctures in real time, is less expensive, has less radiation exposure and is more widespread. Undoubtedly, the comparison between these two imaging techniques must be further compared in future studies to determine the ultimate effective and safer choice. In conclusion, the current study provides preliminary evidence that gasserian ganglion block can be an effective pain relief method for acute/subacute zoster-related trigeminal neuralgia.
Conclusions
CT-guided gasserian ganglion block with local anesthetics and steroids can be an effective and safe technique to relieve the pain of acute/subacute zoster-related trigeminal neuralgia.
Abbreviations
HZ, herpes zoster; VZV, varicella zoster virus; TPHN, trigeminal postherpetic neuralgia; PRF, pulsed radiofrequency; PHN, postherpetic neuralgia; ECG, electrocardiogram; HR, heart rate; BP, blood pressure; RR, respiratory rate; 3D, three-dimensional; NRS, numerical rating scale; DM, diabetes mellitus; IQRs, interquartile ranges.
Data Sharing Statement
Patient data will not be available because this was not a concern when the study was conducted and the patients were not informed.
Ethics Approval and Informed Consent
Ethics approval was obtained from the Ethics Committee of Beijing Tiantan Hospital, Capital Medical University (KYKY2022-049). The application for a waiver of informed consent for this study was approved.
Consent for Publication
All the authors confirm that the details of any images, videos, recordings, etc, can be published, and the consent have been shown the article contents to be published. Authors are prepared to provide copies of signed consent forms to the journal editorial office if requested.
Acknowledgment
We thank the patients who enrolled in this study.
Funding
This research was supported by the Capital’s Funds for Health Improvement and Research (No. 2020-2-2046). The funder had no role in the study design, data collection, data analysis, data interpretation, or writing of the manuscript. The corresponding author had complete access to all the data in the study; all the co-authors were responsible for making the final decision to submit for publication.
Disclosure
The authors declare that they have no conflict of interest.
References
1. Vanneste T, Van Lantschoot A, Van Boxem K, Van Zundert J. Pulsed radiofrequency in chronic pain. Curr Opin in Anaesth. 2017;30:577–582. doi:10.1097/ACO.0000000000000502
2. Huang J, Ni Z, Finch P. Gasserian ganglion and retrobulbar nerve block in the treatment of ophthalmic postherpetic neuralgia: a case report. Pain Pract. 2017;17(7):961–967. doi:10.1111/papr.12547
3. Shapiro M, Kvern B, Watson P, Guenther L, McElhaney J, McGeer A. Update on herpes zoster vaccination: a family practitioner’s guide. Can Fam Physician. 2011;57(10):1127–1131.
4. Johnson RW, Rice AS, Solomon CG. Clinical practice: postherpetic neuralgia. N Engl J Med. 2014;371(16):1526–1533. doi:10.1056/NEJMcp1403062
5. Kawai K, Yawn BP, Wollan P, et al. Increasing incidence of herpes zoster over a 60-year period from a population-based study. Clin Infect Dis. 2016;63(2):221–226. doi:10.1093/cid/ciw296
6. Paquin R, Susin LF, Welch G, Barnes JB, Stevens MR, Tay FR. Herpes zoster involving the second division of the trigeminal nerve: case report and literature review. J Endodont. 2017;43:1569–1573. doi:10.1016/j.joen.2017.03.004
7. Attal N, Cruccu G, Baron R, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17:1113–1123. doi:10.1111/j.1468-1331.2010.02999.x
8. Dong DS, Yu X, Wan CF, et al. Efficacy of short-term spinal cord stimulation in acute/subacute zoster-related pain: a retrospective study. Pain Physician. 2017;20(5):E633–E645.
9. Liu DY, Chen JS, Lin CY, Gong QJ, Zhao Q, Wan L. Subcutaneous peripheral nerve stimulation for treatment of acute/subacute herpes zoster-related trigeminal neuralgia: a retrospective research. Clin J Pain. 2021;37:867–871. doi:10.1097/AJP.0000000000000981
10. Wan C, Dong DS, Song T. High-voltage, long-duration pulsed radiofrequency on gasserian ganglion improves acute/subacute zoster-related trigeminal neuralgia: a randomized, double-blinded, controlled trial. Pain Physician. 2019;22(4):361–368.
11. Feller L, Khammissa R, Fourie J, Bouckaert M, Lemmer J. Postherpetic neuralgia and trigeminal neuralgia. Pain Res Treat. 2017;2017:1681765. doi:10.1155/2017/1681765
12. Kim J, Kim MK, Choi GJ, Shin HY, Kim BG, Kang H. Pharmacological and non-pharmacological strategies for preventing postherpetic neuralgia: a systematic review and network meta-analysis. Korean J Pain. 2021;34(4):509–533. doi:10.3344/kjp.2021.34.4.509
13. Chang MC. Efficacy of pulsed radiofrequency stimulation in patients with peripheral neuropathic pain: a narrative review. Pain Physician. 2018;21:225–234. doi:10.36076/ppj.2018.3.E225
14. Cui JZ, Zhang XB, Zhu P, et al. Effect of repetitive intracutaneous injections with local anesthetics and steroids for acute thoracic herpes zoster and incidence of postherpetic neuralgia. Pain Med. 2017;18:1566–1572. doi:10.1093/pm/pnw190
15. Karbassi M, Raizman MB, Schuman JS. Herpes zoster ophthalmicus. Surv Ophthalmol. 1992;36(6):395–410. doi:10.1016/S0039-6257(05)80021-9
16. Johansson A, Bennett GJ. Effect of local methylprednisolone on pain in a nerve injury model. A pilot study. Reg Anesth. 1997;22:59–65. doi:10.1016/S1098-7339(06)80057-X
17. Johnson RW. Consequences and management of pain in herpes zoster. J Infect Dis. 2002;186(Suppl 1):S83–90. doi:10.1086/342970
18. Choi EM, Mi HC, Jun JH, et al. Efficacy of intermittent epidural dexamethasone bolus for zoster-associated pain beyond the acute phase. Int J med sci. 2020;17(12):1811–1818. doi:10.7150/ijms.46038
19. Don KE, In LY, Jung PH, Charles GJ, Glorioso JC. Comparison of efficacy of continuous epidural block and pulsed radiofrequency to the dorsal root ganglion for management of pain persisting beyond the acute phase of herpes zoster. PLoS One. 2017;12(8):e0183559. doi:10.1371/journal.pone.0183559
20. Gain P, Thuret G, Chiquet C, Navez ML, Pascal J. Frontal and nasal nerve blocks in the treatment of severe pain in acute ophthalmic zoster. Anesth Analg. 2002;95(2):503. doi:10.1213/00000539-200208000-00069
21. Kim HJ, Ahn HS, Lee JY, et al. Effects of applying nerve blocks to prevent postherpetic neuralgia in patients with acute herpes zoster: a systematic review and meta-analysis. Korean J Pain. 2017;30(1):3–17. doi:10.3344/kjp.2017.30.1.3
22. Ding YY, Hong T, Li H, Yao P, Zhao G. Efficacy of CT guided pulsed radiofrequency treatment for trigeminal postherpetic neuralgia. Front Neurosci. 2019;13:708. doi:10.3389/fnins.2019.00708
23. Jeon Y, Jin Y. Caudal block with steroid in the treatment of acute voiding dysfunction and pain caused by sacral herpes zoster: a case report. Medicine. 2020;99:e20680. doi:10.1097/MD.0000000000020680
24. Fabian VA, Wood B, Crowley P, Kakulas BA. Herpes zoster brachial plexus neuritis. Clin Neuropathol. 1997;16(2):61–64.
25. Argoff CE, Katz N, Backonja M. Treatment of postherpetic neuralgia: a review of therapeutic options. J Pain Symptom Manage. 2004;28(4):396–411. doi:10.1016/j.jpainsymman.2004.01.014
26. Bartley J. Post herpetic neuralgia, Schwann cell activation and vitamin D. Med Hypotheses. 2009;73(6):927–929. doi:10.1016/j.mehy.2009.06.039
27. Johnson RW. Herpes zoster in the immunocompetent patient: management of post-herpetic neuralgia. Herpes. 2003;10(2):38–45.
28. Zhao P, Mei L. A clinical study of paraspinal nerve block on treatment of herpes zoster under ultrasonic guidance. Neurochirurgie. 2019;65(6):382–386. doi:10.1016/j.neuchi.2019.06.007
29. Lee HJ, Park HS, Moon HI, Yoon SY. Effect of ultrasound-guided intercostal nerve block versus fluoroscopy-guided epidural nerve block in patients with thoracic herpes zoster: a comparative study. J Ultrasound Med. 2019;38(3):725–731. doi:10.1002/jum.14758
30. Desmet M, Vanneste B, Reynvoet M, et al. A randomised controlled trial of intravenous dexamethasone combined with interscalene brachial plexus blockade for shoulder surgery. Anaesthesia. 2015;70(10):1180–1185. doi:10.1111/anae.13156
31. Waldron NH, Jones CA, Gan TJ, Allen TK, Habib AS. Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br J Anaesth. 2013;110(2):191–200. doi:10.1093/bja/aes431
32. Desmet M, Braems H, Reynvoet M, et al. IV and perineural dexamethasone are equivalent in increasing the analgesic duration of a single-shot interscalene block with ropivacaine for shoulder surgery: a prospective, randomized, placebo-controlled study. Br J Anaesth. 2013;111(3):445–452. doi:10.1093/bja/aet109
33. Clement JC, Besch G, Puyraveau M, et al. Clinical effectiveness of single dose of intravenous dexamethasone on the duration of ropivacaine axillary brachial plexus block: the randomized placebo-controlled ADEXA trial. Reg Anesth Pain Med. 2019;44(3):e100035. doi:10.1136/rapm-2018-100035
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.