Back to Journals » Journal of Pain Research » Volume 16
Effect of Collagenase Chemonucleolysis on Residual Pain After Transforaminal Lumbar Endoscopic Discectomy
Authors Han L, Li T, Chen L, Guo Y, Zhao L, Hu J, Wang L
Received 23 December 2022
Accepted for publication 3 April 2023
Published 14 April 2023 Volume 2023:16 Pages 1257—1265
DOI https://doi.org/10.2147/JPR.S402534
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael A Ueberall
Liuhu Han,1,* Tingting Li,1,* Liyang Chen,1 Yuyu Guo,1 Long Zhao,2 Jun Hu,2 Likui Wang2
1AnHui Medical University, HeFei, People’s Republic of China; 2Department of Pain, The First Affiliate Hospital of AnHui Medical University, Hefei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Likui Wang, Department of Pain, The First Affiliate Hospital of AnHui Medical University, No. 218 Jixi Road, Shushan District, Hefei, Anhui Province, People’s Republic of China, Tel +86 13705690702, Email [email protected]
Purpose: To investigate the short-term clinical effect of collagenase chemonucleolysis (CCNL) in the treatment of residual pain after transforaminal lumbar endoscopic discectomy (TLED).
Patients and Methods: The clinical data of 40 patients with residual pain after TLED for lumbar disc herniation (LDH) in our hospital from January 2018 to December 2020 were retrospectively analyzed. The visual analogue scale (VAS) and quality of recovery-15 (QoR-15) were used to evaluate the effect of the operation. Modified MacNab method was used to evaluate the efficacy of CCNL at 6 months and 12 months after operation.
Results: All patients successfully completed the operation without serious complications, such as intervertebral space infection, vascular injury and nerve injury. The VAS 3 days after TLED was not significantly lower than that Pre-TLED (P > 0.05). The VAS at each time point after CCNL was significantly lower than that at Pre-TLED, and the QoR-15 score at each time point after CCNL was significantly higher than that 3 days after CCNL (P < 0.05). The modified MacNab criteria for the last follow-up was 95%.
Conclusion: CCNL can effectively relieve the residual pain after TLED, and the quality of life of patients after TLED is improved with time, and the safety of CCNL is higher.
Keywords: collagenase chemonucleolysis, transforaminal lumbar endoscopic discectomy, lumbar disc herniation, pain, quality of recovery
Introduction
Lumbar disc herniation (LDH) is a common chronic disease in clinic. It is common in middle-aged and elderly people, and its clinical manifestations are lumbar pain, sciatica, with or without lower limb numbness, of which cauda equina syndrome is one of the most serious manifestations.1 LDH with clinical sign and symptom often requires surgery when the conservative treatment is ineffective. In recent years, with the development of technology, minimally invasive spinal surgery has been widely used in the world.2,3 Transforaminal lumbar endoscopic discectomy (TLED) has the advantages of minimal invasion, quick recovery and definite curative effect, and is currently the preferred surgical method for patients with LDH.4–6
However, there are individual differences in the clinical effect of TLED. Lee et al have reported that there are many factors that lead to the incomplete cleaning of the herniated nucleus pulposus after TLED, and the significant compression of the nerve root by the residual part of the lateral recess stenosis, such as the size and location of disc herniation, the degree of disc degeneration and the operator’s proficiency.6,7 There are also some cases of incomplete decompression in which a part of the hidden intervertebral disc tissue protrudes again from the back or contralateral side of the protrusion. In addition, although TLED can eliminate mechanical compression pain, inflammation and nerve root congestion and edema reactions can persist for several days after surgery, so patients with postoperative pain often need additional treatment.8 Collagenase chemonucleolysis (CCNL) is a percutaneous technique in which collagenase is injected into the diseased disc and around the protrusion under CT guidance.9,10 Collagenase is an enzyme that mainly dissolves collagen and can effectively dissolve type I and type II collagen in nucleus pulposus and annulus fibrosus. Collagenase solution with the same osmotic pressure as human tissue does not damage nerve cells, hemoglobin, casein, keratin sulfate and other proteins. Collagenase for injection can specifically hydrolyze the three-dimensional helical structure of collagen in intervertebral disc tissue. Meanwhile, proteoglycan is cracked and degraded into proline, hydroxyproline and other small molecular amino acids, which are finally absorbed by the human body.11 The reduction or disappearance of the protrusion can relieve or eliminate the compression of the protrusion on nerve tissues. In addition, collagenase can also inhibit the activity of phospholipase A2 (PLA2), which is an inflammatory substance in nerve roots, reduce or eliminate the inflammatory reaction in nerve roots, and ultimately improve the clinical signs and symptoms of patients.12 Therefore, for patients with severe inflammation and edema in nerve root, CCNL can play the analgesic effect. CCNL has been developed for more than 50 years, and its exact efficacy and high safety have been widely recognized at home and abroad.13–15 The purpose of this study is to explore the short-term clinical efficacy of CCNL in patients with residual pain after TLED.
Materials and Methods
Study Design and Study Population
The trial was approved by the Ethics Committee of the First Affiliated Hospital of Anhui Medical University (Ethical Application Reference: PJ2022-14-43 Anhui, China) and was registered at the Chinese Clinical Trial Registry (ChiCTR2200066535). This study was conducted in accordance with the Declaration of Helsinki and clinical practice guidelines. All patients had previously signed informed consent for the procedure. Consecutive patients who received CCNL for residual pain after TLED between 2018 and 2020 were included in this single-center retrospective cohort study at the First Affiliated Hospital of Anhui Medical University. All patients were diagnosed as LDH by imaging combined with clinical manifestations before operation, and complained of pain and numbness in the back and/or lower limbs, accompanied by limitation of movement. At the same time, the patient complained that the pain was not significantly relieved after TLED, and there was still pain and numbness in the back and/or lower limbs. Inclusion criteria: clear diagnosis of LDH according to imaging and clinical manifestations; residual low back and/or lower limbs pain after TLED. Exclusion criteria: vertebral body instability in lumbar dynamic position; patients with severe degeneration of lumbar intervertebral disc in imaging; patients with puncture site infection, hemorrhagic disease or abnormal coagulation function, and those who cannot understand the visual analogue scale (VAS).
Study Treatments
The patient was monitored by ECG, lying prone on the operating table in the CT scanning room, with a soft pillow under the abdomen, atropine 0.5 mg and ephedrine 30 mg. The surgical puncture site was routinely disinfected and draped. After local infiltration anesthesia with 0.5% lidocaine, according to the image under CT guidance, 5mL of mixed solution (2% Lidocaine 2mL+Normal Saline 2mL+Compound Betamethasone injection 1mL) was locally injected from the puncture point along the lateral edge of the facet joint to the target point of the protrusion (Figure 1). The ten-minute observation time was performed to closely monitor the patient’s vital signs and pay attention to the sensory and motor functions of the patient’s lower limbs. If the patient’s vital signs are stable and there is no obvious sign of loss of motor and sensory function of the lower limbs, 300 U (2 mL) of collagenase can be slowly injected into the protrusion through the inner needle, and then 600 U (2 mL) of collagenase can be injected into the disc through the inner needle, and finally 300 U (2 mL) of collagen can be injected to the surface of the protrusion through the epidural needle. After the operation, the puncture needle was pulled out and the puncture point was covered with sterile dressing. Then, the vital signs of patient were monitored for 10 minutes, and the patient was sent back to the ward without discomfort symptoms.
 |
Figure 1 Target and intradiscal collagenase injection procedure. |
Three days after the operation, the patients were kept in bed absolutely, and the waistline was routinely worn for one month. The patients were in bed for three days to fully relax the waist, back and abdominal muscles, so as to avoid increasing pressure on the intervertebral disc during the dissolution process and prevent the aggravation of postoperative pain. The prolonged supine position may aggravate the patient’s difficulty in excretion and increase the risk of venous thrombosis.12 After three months, the back muscles were properly exercised to avoid torsion and weight-bearing.
Outcome Measures
In this study, the primary outcome was measured by the VAS16 and the global quality of recovery-15 score (QoR-15)17 assessed postoperatively for 24 h in five dimensions: emotional state (4 items), physical comfort (5 items), psychological support (2 items), physical independence (2 items), and pain (2 items). The total score on the QoR-15 ranges from 0 (the poorest quality of recovery) to 150 (the best quality of recovery). The surgical efficacy was evaluated according to the modified MacNab criteria,18 which were divided into four criteria: excellent, good, fair, and poor. The efficacy was evaluated at 6 and 12 months after surgery. Excellent (no pain; no restriction of activity); Good (occasional back or leg pain of sufficient; severity to interfere with the patient’s ability to do his normal work or his capacity to enjoy himself in his leisure hours); Fair (functional ability is improved, but intermittent pain is serious enough to reduce or change work or leisure activities); Poor (no improvement or insufficient improvement to enable increase in activities; further operative intervention required).
Statistical Analysis
SPSS 25.0 software was used for statistical analysis of the data. The measurement data were presented as mean ± standard. When the data were in line with normal distribution, one-way repeated-measures ANOVA was used to compare different time points. Bonferroni method was used to correct the test. When the data were not in line with normal distribution, rank sum test was used. χ2 test was used for enumeration data, and P<0.05 was considered to be statistically significant.
Results
Patients
From January 2018 to December 2020, 40 patients with LDH and residual pain after TLED were selected from the pain department of our hospital. Figure 2 gives a graphic overview of the follow-up of the included patients. Table 1 gives an overview of the baseline demographics of the patients included. There were 21 males and 19 females, aged from 32 to 81 years, with a mean age of 59.58 ± 13.97, a mean BMI of 23.29 ± 1.78, and a mean VAS scores of 6.42 ± 1.47 Pre-TLED. Among them, there were 7 patients with disc herniation located at L3/4, 20 patients with disc herniation located at L4/5, and 13 patients with disc herniation located at L5/S1.
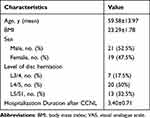 |
Table 1 General Condition of Patients |
 |
Figure 2 Graphical overview of the study procedures and the treatment protocols performed. Abbreviation: CN, coblation nucleoplasty; |
Outcomes
There was statistically significant difference in VAS and QoR-15 scores of 40 patients at different time points (VAS, F = 85.58, P < 0.05; QoR-15, F = 375.53, P < 0.05). There was no significant difference in VAS scores between Pre-TLED and 3 days after TLED (P > 0.05). There were significant differences in VAS scores at 3 days, 3 months, 6 months, 12 months after CCNL and Pre-TLED (P < 0.05). There was statistical difference between QoR-15 at 3 months, 6 months, and 12 months after CCNL and QoR-15 at 3 days after CCNL (P < 0.05) (Table 2). The operation was successfully completed in all patients, and there were no nerve and blood vessel injuries, no loss of motor and sensory function of both lower extremities, and no serious adverse events, such as lumbar infection after operation. The operation time was 30–60 min, with an average of (36.50 ± 4.19) min; all surgical incisions were healed, and the hospitalization duration after CCNL was 3.40 ± 0.71 days (Table 1). The VAS scores of all patients at each follow-up time point were significantly lower than that before operation, and showed a downward trend over time (P < 0.05) (Table 2 and Figure 3). QoR-15 scores were significantly lower at each time point than at 3 days after CCNL, and showed an upward trend over time (P < 0.05) (Table 2 and Figure 4). There was no significant difference between the two groups at 3 months, 6 months and 12 months after CCNL (P > 0.05). The excellent and good rate of the modified MacNab criteria at the last follow-up was 95% (Table 3). Six months after the operation, one case of LDH recurred. After communicating with the patient, TLED was decided to be performed.
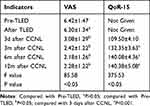 |
Table 2 Comparison of VAS and QoR-15 Scores of 40 Patients at Different Time Points |
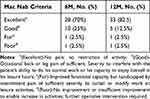 |
Table 3 Outcomes as Measured by Modified Mac Nab Criteria |
 |
Figure 3 Change trend of VAS of 40 patients over time. |
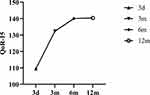 |
Figure 4 Change trend of QoR-15 scores of 40 patients over time. |
Demonstration Case 1
A 76-year-old woman with low back pain and right lower limb pain for more than one month. Sagittal and axial T2-weighted MRI images showed L4/5 disc herniation compressing the dural sac and right nerve roots (Figure 5a and b). The patient complained of a VAS score of 8 and Right Lasegue Sign (+) and underwent TLED. Ten days later, the patient complained that the symptoms were not significantly relieved, and the VAS score was 6. The lumbar MRI showed that the L4/5 intervertebral disc bulged and compressed the dural sac (Figure 5c and d). The patient underwent CCNL immediately. Three days after the operation, the patient reported that the pain was relieved. Three months after the CCNL, the VAS score was 2. The lumbar MRI showed that the annulus fibrosus of the intervertebral disc was retracted (Figure 5e and f).
Discussion
LDH is a syndrome caused by the degeneration of intervertebral disc, rupture of annulus fibrosus, protrusion of internal nucleus pulposus, and compression and stimulation of adjacent lumbosacral nerve roots and cauda equina nerve. The pathogenesis of LDH mainly involves mechanical compression, inflammatory stimulation, immune response and pain sensitization, and the predilection sites are L4/5 and L5/S1.13,19
In recent years, with the improvement of optical technology and equipment, as well as the rapid development of TLED, this minimally invasive surgical method with less trauma, faster recovery and less damage to nerve tissues has been widely used in the treatment of patients with LDH. Stylianos Kapetanakis et al have reported that TLED has been used satisfactorily in some extreme cases, such as foraminal stenosis (FS) in adult degenerative scoliosis (ADS), recurrent foraminal stenosis (RFS) after previous open decompression surgery, and adjacent segment disease (ASD) after previous lumbar fusion.20 However, the use of TLED as a revision surgery can be challenging for beginners because it involves factors such as the alteration of normal physiological anatomy by scar tissue after previous surgery.20 Moreover, the learning curve of TLED is very steep, and mastering it requires the operator to have high fine operation skills and three-dimensional thinking, while endoscopic operation requires the operator to master the anatomical structure skillfully.21 Thus, despite the rapid development of new surgical techniques and the reported success of lumbar disc surgery, more than 10% of patients experience long-term recurrent pain, which is associated with substantial health care costs.22 Besides, beginners have a higher incidence of postoperative complications.
Sussman, an American scholar, used collagenase to dissolve intervertebral disc tissue in vitro and carried out animal experiments in 1968, which proved that collagenase dissolved collagen specifically.23,24 The effectiveness of collagenase lysis in the treatment of LDH was first reported in China in 1981. With the continuous exploration of clinical application of collagenase in China and the formulation of expert consensus, CCNL has become one of the safe and effective surgical methods for the treatment of LDH. Chen Jiahua of our department put forward the concept of “target injection, enzyme dissolving substrate” in 1999, which greatly improved the efficiency of collagenase in the treatment of LDH and reduced postoperative complications. However, since the rapid development of TLED, CCNL has not been the first choice for patients with LDH. Although it has the advantages of small trauma and low incidence of postoperative complications, compared with TLED, CCNL has a slower effect. In this study, target injection combined with intradiscal injection was adopted, that is, under the guidance of CT, the puncture route was first designed and then the needle technique was adopted. The outer needle reached the surface of the protrusion, the inner needle reached the center of the protrusion, and a certain dose of collagenase was injected into both the inner and outer needle tubes. Then, the inner needle was punctured into the intervertebral disc behind the protrusion and a certain dose of collagenase was injected. This measure can not only make the protrusion degrade inside and outside at the same time, greatly alleviate the symptoms of transient pain aggravation after operation, but also reduce the probability of recurrence after operation.
In this study, after one year of follow-up, the VAS score decreased from 6.30 ± 1.34 to 2.28 ± 1.22, and the QoR-15 score increased from 109.50 ± 4.10 to 140.38 ± 5.08. The pain symptoms of most patients were obviously relieved or disappeared without obvious adverse reactions, and the excellent and good rate of operation reached 95%. At the same time, the author observed that intradiscal injection of collagenase increased the probability of pain response after operation, but most of them occurred within one week. Relevant studies showed that it may be caused by increased intradiscal pressure and nerve root congestion and edema during the dissolution of nucleus pulposus.25 It should be noted that injection of collagenase into subarachnoid space is absolutely contraindicated, so injection of anti-inflammatory analgesic solution before injection of collagenase will not only increase the safety of surgery, but also reduce the incidence of postoperative pain and the use of analgesic drugs.
This study shows that CCNL can not only eliminate the stimulation of residual protrusion and re-protrusion to nerve roots and dural sac, but also eliminate the residual inflammatory effect by local injection of anti-inflammatory analgesic liquid before collagenase injection in patients with pain after transforaminal endoscopic surgery for LDH. Compared with open surgery and revision surgery, CCNL can effectively reduce the incidence of complications, such as nerve root injury, and has the advantages of less trauma, higher safety and lower economic/cost ratio.9 In terms of 1-year follow-up results, this treatment not only reduced the size of the re-protrusion and the residual inflammatory effect, effectively relieved the postoperative pain of patients, but also improved the recovery of neurological function and quality of life to a satisfactory level.26
To sum up, CCNL can effectively relieve the residual pain of patients with LDH after TLED, with exact efficacy, high safety and relatively low economic/cost ratio, which is worthy of reference for clinicians. However, there are still limitations in this study, such as the long-term efficacy of this therapy and other potential problems, such as the recurrence rate of LDH after 12 months of long-term follow-up and the degree of disc space height change and adjacent disc degeneration. Such problems need to be further studied.
Conclusion
In conclusion, this study reveals that targeted injection of CCNL combined with intradiscal injection is effective in the treatment of residual pain after TLED and improves postoperative comfort level.
Abbreviations
CCNL, collagenase chemonucleolysis; TLED, transforaminal lumbar endoscopic discectomy; VAS, visual analogue scale; QoR-15, quality of recovery-15; LDH, Lumbar disc herniation; ECG, electrocardiogram; BMI, body mass index; CN, coblation nucleoplasty; FS, foraminal stenosis; ADS, adult degenerative scoliosis; RFS, recurrent foraminal stenosis; ASD, adjacent segment disease; PLA2, phospholipase A2.
Data Sharing Statement
All the processed data were included in the current study. If reviewers or readers have any questions regarding our published data, they can contact the corresponding author [email, [email protected]] for access to the original data.
Acknowledgments
We thank all those who supported and participated in the study, including our staff, patients and their family members.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Liu C, Zhou Y. Percutaneous endoscopic lumbar discectomy and minimally invasive transforaminal lumbar interbody fusion for massive lumbar disc herniation. Clin Neurol Neurosurg. 2019;176:19–24. doi:10.1016/j.clineuro.2018.10.017
2. Kolcun JPG, Chieng LO, Madhavan K, et al. Minimally-invasive versus conventional repair of spondylolysis in athletes: a review of outcomes and return to play. Asian Spine J. 2017;11(5):832–842.
3. Lee LY, Idris Z, Beng TB, et al. Outcomes of minimally invasive surgery compared to open posterior lumbar instrumentation and fusion. Asian J Neurosurg. 2017;12(4):620–637. doi:10.4103/ajns.AJNS_331_16
4. Kapetanakis S, Gkantsinikoudis N, Charitoudis G. Implementation of percutaneous transforaminal endoscopic discectomy in competitive elite athletes with lumbar disc herniation: original study and review of the literature. Am J Sports Med. 2021;49(12):3234–3241. doi:10.1177/03635465211032612
5. Sun J, Fang C, Gao F, et al. Comparison of effectiveness and safety between epidural anesthesia vs local anesthesia for percutaneous transforaminal endoscopic discectomy: a systematic review and meta-analysis. Medicine. 2020;99(1):e18629. doi:10.1097/MD.0000000000018629
6. Pan M, Li Q, Li S, et al. Percutaneous endoscopic lumbar discectomy: indications and complications. Pain Physician. 2020;23(1):49–56.
7. Lee SH, Kang BU, Ahn Y, et al. Operative failure of percutaneous endoscopic lumbar discectomy: a radiologic analysis of 55 cases. Spine. 2006;31(10):E285–90. doi:10.1097/01.brs.0000216446.13205.7a
8. Keorochana G, Pairuchvej S, Setrkraising K, et al. Comparative outcomes of perioperative epidural steroids after percutaneous endoscopic lumbar discectomy for lumbar disc herniation: a randomized placebo-controlled trial. World Neurosurg. 2018;119:e244–e249. doi:10.1016/j.wneu.2018.07.122
9. Wang ZJ, Zhu MY, Liu XJ, et al. Cervical intervertebral disc herniation treatment via radiofrequency combined with low-dose collagenase injection into the disc interior using an anterior cervical approach. Medicine. 2016;95(25):e3953. doi:10.1097/MD.0000000000003953
10. Wu Z, Wei LX, Li J, et al. Percutaneous treatment of non-contained lumbar disc herniation by injection of oxygen-ozone combined with collagenase. Eur J Radiol. 2009;72(3):499–504. doi:10.1016/j.ejrad.2008.07.029
11. Yuan P, Shi X, Wei X, et al. Development process and clinical application of collagenase chemonucleolysis in the treatment of lumbar disc herniation: a narrative review in China. Postgrad Med J;2022;2022:141208. doi:10.1136/postgradmedj-2021-141208
12. Pain Physicians Branch of Chinese Medical Doctor Association, Pain Society of Chinese Medical Association. Chinese expert consensus on Clinical application of lumbar intervertebral disc collagenase lysis. Chin J Pain Med. 2022;28(2). Chinese.
13. Wang M, Zhang X, Yu Y, et al. Low-dose collagenase chemonucleolysis combined with radiofrequency in the treatment of lumbar disc herniation: a 10-year retrospective study. Evid Based Complement Alternat Med. 2021;2021:8234558. doi:10.1155/2021/8234558
14. Han HJ, Kim JY, Jang HY, et al. Fluoroscopic-guided intradiscal oxygen-ozone injection therapy for thoracolumbar intervertebral disc herniations in dogs. In Vivo. 2007;21(4):609–613.
15. Zhang D, Zhang Y, Wang Z, et al. Target radiofrequency combined with collagenase chemonucleolysis in the treatment of lumbar intervertebral disc herniation. Int J Clin Exp Med. 2015;8(1):526–532.
16. Faiz KW. VAS – visuell analog skala [VAS--visual analog scale]. Tidsskr nor Laegeforen. 2014;134(3):323. Danish. doi:10.4045/tidsskr.13.1145
17. Bowyer AJ, Royse CF. Postoperative recovery and outcomes--what are we measuring and for whom? Anaesthesia. 2016;71(Suppl 1):72–77. doi:10.1111/anae.13312
18. Macnab I. Negative disc exploration. An analysis of the causes of nerve-root involvement in sixty-eight patients. J Bone Joint Surg Am. 1971;53(5):891–903. doi:10.2106/00004623-197153050-00004
19. Dower A, Davies MA, Ghahreman A. Pathologic basis of lumbar radicular pain. World Neurosurg. 2019;128:114–121. doi:10.1016/j.wneu.2019.04.147
20. Kapetanakis S, Floros E, Gkantsinikoudis N. Extreme cases in percutaneous transforaminal endoscopic surgery: case series and brief review of the literature. Br J Neurosurg. 2021;1–5. doi:10.1080/02688697.2021.1944981
21. Lee DY, Lee SH. Learning curve for percutaneous endoscopic lumbar discectomy. Neurol Med Chir. 2008;48(9):383–388. doi:10.2176/nmc.48.383
22. Ambrossi GL, Mcgirt MJ, Sciubba DM, et al. Recurrent lumbar disc herniation after single-level lumbar discectomy: incidence and health care cost analysis. Neurosurgery. 2009;65(3):574–578. doi:10.1227/01.NEU.0000350224.36213.F9
23. Sussman BJ. Intervertebral discolysis with collagenase. J Natl Med Assoc. 1968;60(3):184–187.
24. Sussman BJ, Mann M. Experimental intervertebral discolysis with collagenase[J]. J Neurosurg. 1969;31(6):628–635. doi:10.3171/jns.1969.31.6.0628
25. Wintermantel E, Emde H, Loew F. Intradiscal collagenase for treatment of lumbar disc herniations. A comparison of clinical results and computed tomography follow-up. Acta Neurochir. 1985;78(3–4):98–104. doi:10.1007/BF01808686
26. Akinduro OO, Miller BA, Haussen DC, et al. Complications of intraoperative epidural steroid use in lumbar discectomy: a systematic review and meta-analysis. Neurosurg Focus. 2015;39(4):E12. doi:10.3171/2015.7.FOCUS15269
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

