Back to Journals » Clinical Ophthalmology » Volume 8
Effect of 3 years of treatment with a dorzolamide/timolol (1%/0.5%) combination on intraocular pressure
Authors Takeda S, Mimura T, Matsubara M
Received 13 June 2014
Accepted for publication 11 July 2014
Published 9 September 2014 Volume 2014:8 Pages 1773—1782
DOI https://doi.org/10.2147/OPTH.S69359
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Sakurako Takeda,1,2 Tatsuya Mimura,1 Masao Matsubara1,2
1Department of Ophthalmology, Tokyo Women’s Medical University Medical Center East, Tokyo, Japan; 2Department of Ophthalmology, Nippori Clinic, Medical Center East, Tokyo Women’s Medical University, Tokyo, Japan
Purpose: We aimed to evaluate the effect on the intraocular pressure (IOP) of a dorzolamide/timolol (1%/0.5%) fixed combination (DTFC) ophthalmic agent for 3 years.
Participants: A total of 19 consecutive patients who had previously been treated with monotherapy or any combination of a beta-blocker, carbonic anhydrase inhibitor, or prostaglandin analog, for primary open-angle glaucoma (POAG) (n=5) or normal tension glaucoma (N=14) were enrolled.
Methods: Patients were switched to DTFC from their prior glaucoma therapy. The IOP was measured at intervals of 4–6 weeks for 3 years. Treatment failure was defined as an increase of IOP by ≥10% from baseline after switching to DTFC.
Results: The average IOP decreased significantly from 14.1±2.9 mmHg at baseline to 12.2±2.2, 11.8±2.4, 12.1±2.5, 11.6±1.8, and 12.1±2.7 mmHg at 3, 6, 12, 24, and 36 months, respectively, after switching therapy (all P<0.05). The mean percent decrease of IOP was 12.0%±13.0%, 14.5%±14.2%, 12.2%±18.7%, 16.0%±12.8%, and 12.8%±15.2% at 3, 6, 12, 24, and 36 months, respectively, after switching. Univariate or multivariate analysis revealed the percent decrease of IOP was associated with the type of glaucoma (POAG) at 3 and 12 months, and with the baseline IOP at 3, 12, 24, and 36 months. Kaplan–Meier analysis demonstrated that the percentage of patients who remained on treatment with DTFC was 94.7%, 94.7%, 84.2%, 78.9%, and 78.9% at 3, 6, 12, 24, and 36 months, respectively. Cox proportional hazards analysis showed that the type of glaucoma (POAG) was associated with an increased risk of failure to control the IOP.
Conclusion: The IOP-lowering effect of DTFC was demonstrated for 3 years in this study. The baseline IOP had an important influence on the reduction of IOP achieved by DTFC.
Keywords: switching treatment, glaucoma, Cox proportional hazards analysis
Introduction
Glaucoma is a common cause of preventable visual impairment, which is characterized by progressive degeneration of the optic nerve and visual field changes. Elevation of the intraocular pressure (IOP) is associated with optic nerve damage that leads to visual field defects.1–7 Thus, the primary goal of glaucoma treatment is to reduce the IOP, which can usually be achieved with ocular hypotensive agents. According to the European Glaucoma Society Guidelines, topical monotherapy is recommended as the first-line treatment for medical management.8 Among various antiglaucoma drugs, prostaglandin analogs (PGAs) are most widely used because of their high potency. The European Glaucoma Society recommends adjunctive therapy when first-line monotherapy is not sufficient to reach the target IOP or when there is progressive visual field loss.9
Fixed combination therapy (FCD) is expected to improve compliance and convenience for patients, with less stress, lower costs, and fewer local side effects, due to the use of less preservative.9,10 FCD also avoids the washout effect. In fact, various fixed combination eye drop preparations have been successfully developed to date. The fixed combination of 2% dorzolamide and 0.5% timolol maleate (Cosopt®; Merck & Co., Inc., Whitehouse Station, NJ, USA) contains a topical carbonic anhydrase inhibitor and a topical beta-adrenergic receptor blocking (“beta blocker” [BB]) agent, and is the most widely used combination worldwide.10–13 In Japan, a combination drug with a lower concentration of dorzolamide and timolol maleate (1%/0.5%) (Cosopt®) was released recently. Mizoguchi et al reported that IOP was reduced with 8 weeks of adding the dorzolamide/timolol (1%/0.5%) fixed combination (DTFC) to basal PGA therapy, in patients with normal tension glaucoma (NTG).13 Unfortunately, little information is available regarding the long-term efficacy of DTFC. Accordingly, the aim of the present study was to evaluate the long-term efficacy for IOP reduction and safety after switching to DTFC for 3 years, in patients with open angle glaucoma.
Materials and methods
Study design
This was a prospective, longitudinal, uncontrolled, nonrandomized, and consecutive case series study that was conducted at the Nippori Clinic of the Tokyo Women’s Medical University Medical Center East and the Department of Ophthalmology, Tokyo Women’s Medical University Medical Center East Hospital. This study was performed in accordance with the Helsinki Declaration. The institutional review board at the Tokyo Women’s Medical University Medical Center East gave approval. This study received no financial support from any pharmaceutical company, or sponsorship.
Subjects
The purpose and nature of the study were explained in detail to all patients, and informed consent was obtained. Patients who fulfilled the eligibility criteria were recruited consecutively during routine visits to the participating institutions between June 2010 and September 2010.
The inclusion criteria were: (1) an age of 18 years or older; (2) characteristic glaucomatous visual field loss and optic nerve damage in at least one eye; (3) treatment with a PGA, BB, and/or carbonic anhydrase inhibitor (CAI) for at least 3 months; and (4) best-corrected visual acuity ≥20/200.
The exclusion criteria were (1) closed or barely open anterior chamber angle; (2) a history of acute angle closure or ocular trauma; (3) neovascular glaucoma; (4) a history of ocular surgery, including refractive surgery or glaucoma filtering surgery; (5) ocular inflammation or infection during the previous 6 months; (6) clinically significant dry eyes syndrome; and (7) inability to adhere to the treatment and follow-up plan.
Consequently, the study population consisted of 19 patients with NTG (N=15) or primary open-angle glaucoma (POAG) (N=5), aged 66.3±7.4 years (mean ± SD) with an age range of 51 to 81 years (Table 1). All patients were Japanese and residents of Japan. As for prior antiglaucoma drugs, four (21.1%) patients were using BB, two (10.5%) were using CAI, nine (47.3%) were using PGA+BB, one (5.3%) was using a PGA/BB combination, and three (15.8%) were using PGA+BB+CAI (Table 1).
Intervention
Patients were switched to DTFC (Cosopt®) without a washout period between treatments. Switching was performed at the attending physician’s discretion. The main reasons for switching to DTFC were inadequate control of IOP and progression of visual field defects.14 When the increase of IOP was greater than 2 mmHg in two consecutive visits compared with the average of the last two measurements, IOP control was considered to be inadequate. Visual field progression was defined as deterioration of the visual fields, that is, at least three identical continuous points showing at least 3 dB of deterioration on glaucoma change probability maps, based on the changes of pattern deviation values in two consecutive tests. Six (31.6%) patients with prior BB (N=4) or CAI monotherapy (N=2) were switched to DTFC, while nine (47.3%) patients with prior PGA+BB therapy were switched to PGA+DTFC. The one (5.3%) patient with prior PGA/BB combination therapy was switched to DTFC, while three (15.8%) patients with prior PGA+BB+CAI therapy were switched to PGA+DTFC. To assess the efficacy of DTFC in patients who were previously on multidrug therapy (BB, CAI, and/or PGA) or monotherapy (BB or CAI), the subjects were divided into the following two groups according to the change in the number of antiglaucoma agents: the increased group (N=15 [78.9%]) switched from BB or CAI to DTFC or from PGA+BB to PGA+DTFC, while the nonincreased group (N=4 [21.1%]) switched from PGA/BB combination to DTFC or from PGA+BB+CAI to PGA+DTFC. If both eyes fulfilled the eligibility criteria, the eye with the higher IOP at baseline was used for analysis. If both eyes had the same baseline IOP, the right eye was used for analysis.
Main outcomes
The age, sex, medical history, current antiglaucoma drugs, and ocular history of each patient were assessed at the baseline visit. All subjects underwent a complete ophthalmic examination that included anterior segment biomicroscopy, fundus examination, and refraction with an automated kerato-refractometer (RC-5000; Tomey Corp, Nagoya, Japan). The spherical power and cylindrical power were both measured, after which the spherical equivalent (sphere +1/2 cylinder) was used to calculate the refractive error.
Follow-up visits were scheduled at intervals of approximately 4–6 weeks for 3 years. If a patient missed a scheduled visit, data from the visit closest to the scheduled one were used for analysis. At each visit, the IOP was measured by Goldmann applanation tonometry, in the morning (between 9 am and 12 noon) by the same ophthalmologist (ST). The percent reduction of the IOP was calculated as follows: ([baseline IOP − mean IOP]/baseline IOP) ×100. All data were stored in a computer database at the time of each visit.
Statistical analysis
Normality was evaluated using the normal probability plot. Continuous variables were compared between two groups, with the two-tailed paired or unpaired Student’s t-test. Frequencies were compared with the χ2 test or Fisher’s exact test. Relations among variables were investigated by calculating Pearson’s correlation coefficients. Factors associated with the IOP reduction rate at 3, 6, 12, 24, and 36 months after switching were investigated by multivariate logistic regression analysis, with the explanatory variables including age (years); sex (male/female); right/left eye; refraction (diopters); type of glaucoma (POAG/NTG); the group, stratified according to the number of medications after switching (nonincreased/increased group); and the baseline IOP.
Kaplan–Meier analysis was employed to assess the success rate of IOP control after switching to DTFC. When the increase of IOP after switching was greater than 10%, IOP control was considered to have failed. Multivariate analysis with the Cox proportional hazards model was performed to investigate the influence of potential confounders on IOP control after switching. The same seven explanatory variables were used for the model. The level of significance was set at P<0.05. Statistical analyses were performed with SAS System software version 9.1 (SAS Institute Inc., Cary, NC, USA).
Results
The demographic features of the subjects are summarized in Table 1. Blepharitis only occurred in one patient, at 36 months after switching. There were no side effects and toxicity during the treatment with DTFC. No patient discontinued the study due to lack of efficacy or adverse effects of DTFC; ocular surgery, including cataract surgery; ocular infection; or use of topical steroids, during the 36 months after switching.
The mean IOP was 14.1±2.9 mmHg at baseline, 12.2±2.2 mmHg at 3 months after switching, 11.8±2.4 mmHg at 6 months, 12.1±2.5 mmHg at 12 months, 11.6±1.8 mmHg at 24 months, and 12.1±2.7 mmHg at 36 months after switching (Figure 1A). There was a significant decrease of IOP compared with baseline at all visits after switching (P<0.05, paired two-tailed Student’s t-test) (Figure 1A). There was no significant difference of IOP between the nonincreased and increased groups at all times of assessment (unpaired two-tailed Student’s t-test) (Figure 1B). After switching, IOP was higher in patients with POAG than in those with NTG, and a statistically significant difference was only seen between the two groups at 3 months after switching (P=0.0044, unpaired two-tailed Student’s t-test) (Figure 1C).
The mean percent decrease of IOP (IOP reduction rate) was 12.0%±13.0% at 3 months, 14.5%±14.2% at 6 months, 12.2%±18.7% at 12 months, 16.0%±12.8% at 24 months, and 12.8%±15.2% at 36 months after switching, and the reduction relative to the baseline IOP was greater than 10% at all visits (Figure 2A). The mean IOP reduction rate was larger in the increased group than in the nonincreased group at all visits, although there was no significant difference between the two groups (unpaired two-tailed Student’s t-test) (Figure 2B). There was also no significant difference in the percent reduction of IOP between NTG and POAG patients at all visits (unpaired two-tailed Student’s t-test) (Figure 2C).
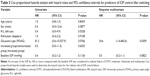
The baseline IOP was correlated with the percent decrease of IOP at 3 months (r=0.56, P=0.0118), 6 months (r=0.41, P=0.0836), 12 months (r=0.54, P=0.0180), 24 months (r=0.59, P=0.0084), and 36 months (r=0.47, P=0.0446, two-tailed Pearson’s correlation coefficient analysis) (Table 2 and Figure 3) after switching, and significant correlations were found at 3, 12, 24, and 36 months but not at 6 months. In addition, multivariate analysis demonstrated that the IOP reduction rate at 3 months was associated with age (odds ratio [OR] =0.59, P=0.0084), the type of glaucoma (POAG/NTG) (OR =0.56, P=0.0095), and the baseline IOP (OR =2.10, P=0.0006), while the IOP reduction rate at 12 months was associated with the type of glaucoma (OR =0.57, P=0.0452) and the baseline IOP (OR =2.37, P=0.0017), and that at 24 months was associated with baseline IOP (OR =1.90, P=0.0141) (Table 2).
  | Figure 3 The correlation between the baseline IOP and percent reduction of IOP, in all patients (A), the nonincreased group (B), and the increased group (C). |
Figure 4 shows the results of Kaplan–Meier analysis. Elevation of IOP by 10% or more compared with the baseline IOP was defined as failure. The success rates for all patients were 94.7%, 94.7%, 84.2%, 78.9%, and 78.9% at 3, 6, 12, 24, and 36 months, respectively. There were no significant differences in the success rates between the nonincreased group and the increased group (75.0% vs 100.0% [P=0.2105]; 75.0% vs 86.7% [P=0.9030]; 75.0% vs 80.0% [P=0.8217]; and 75.0% vs 80.0% [P=0.8217] at 6, 12, 24, and 36 months, respectively [Fisher’s exact test]) (Figure 4A). Success rates were higher in patients with NTG than in those with POAG, but no significant differences were observed between the two groups (100.0% vs 80.0% [P=0.2632]; 92.9% vs 60.0% [P=0.1548]; 92.9% vs 60.0% [P=0.2722]; and 92.9% vs 60.0% [P=0.2722] at 6, 12, 24, and 36 months, respectively [Fisher’s exact test]) (Figure 4B).
Univariate and multivariate Cox proportional hazards models were used to identify predictors of IOP control after switching therapy (Table 3). Continuous data, such as baseline IOP (P=0.1650), age (P=0.1981), and refraction (P=0.0601) were consistent with normal distribution. According to univariate analysis, the type of glaucoma (POAG) was associated with a lower IOP control rate (OR =81.2), although no significant difference was noted (P=0.0766). Multivariate analysis with the Cox proportional hazards model also showed that the type of glaucoma (POAG) was associated with an increased risk of failure of IOP control (OR =34.6, P=0.0309).
Discussion
In the present study, the following main findings were obtained: (1) There were no severe complications of DTFC treatment for 3 years in all patients. (2) IOP was reduced by an average of 2.0 mmHg from baseline IOP, and the percent reduction from baseline was approximately 12.7% at 36 months. (3) There were no significant differences in the mean IOP and percent decrease of IOP between the nonincreased and increased groups, but the mean IOP reduction rate was larger in the increased group than in the nonincreased group. (4) The success rate was 78.9% at 36 months, when an increase of IOP by ≥10% after switching to DTFC was defined as failure. (5) The reduction of IOP was mainly influenced by the baseline IOP and the type of glaucoma (POAG). These results suggest that DTFC therapy safely and effectively controlled the IOP for 3 years and that the baseline IOP was an important determinant of the effectiveness of this agent.
In the present study, the main reason for switching to DTFC was insufficient IOP control. Generally, the reasons for switching to a FCD are the desire to improve IOP control and to avoid the adverse effects of prior therapy, as well as to increase compliance and the convenience of treatment.11 FCDs have several advantages.10,15 First, these drugs have a lower cost than the individual medications. Second, FCDs may be more convenient, leading to better adherence due to a lower frequency of application. Third, a lower number of doses per day also decreases side effects. For instance, DTFC could potentially reduce exposure of the ocular surface to preservative compared with use of the two agents (dorzolamide and timolol) as separate drugs. Fourth, FCDs are sometimes more effective at reducing the IOP. DTFC also avoids the washout effect of administering a second eye drop after first drop. These improvements of compliance and the washout effect may explain why the combination reduced the IOP further in the present study. The effect of DTFC on the IOP was maintained for 36 months; during this time, there were no dropouts, and no additional therapies or surgery were needed. Thus, the present combination was preferable for multiple reasons.
We found that DTFC reduced the IOP by 2.2±2.3 and 2.0±2.7 mmHg from baseline IOP at 6 and 36 months after switching, respectively (Figure 1A). The percent reduction of IOP from baseline was 14.5%±14.2% and 12.8%±15.2% at 6 and 36 months after switching, respectively (Figure 2A). Sonty et al reported that DTFC reduced the IOP from 21.4±2.5 mmHg at baseline to 17.9±3.5 at 12 weeks after switching from latanoprost (n=57).12 Mizoguchi et al reported that DTFC reduced the IOP from 15.6±2.0 mmHg at baseline to 13.7±2.2 mmHg at 8 weeks after addition to PGA monotherapy (n=40). The percent reduction of IOP from the baseline value was 11.7%±13.1% at 8 weeks.13 The percent reduction of IOP in the present study was similar to those reported previously.12,13 However, there is not necessarily agreement as to whether DTFC would reduce the IOP after switching. For example, some studies have shown a decrease of IOP after switching from DTFC to latanoprost.16–19 To explain this apparent inconsistency, two possibilities can be suggested. First, the previous medication was less effective regardless of its type, and the new medication had a superior IOP-reducing effect. Second, patient education for this clinical trial may have improved compliance with the new medication.12
We need to consider whether the IOP-lowering effect of DTFC in the present study was adequate or not. A reduction of the IOP by 2.0±2.7 mmHg from baseline was observed 36 months after switching (Figure 2A), and the percentage of patients who achieved a 1 mmHg or more reduction of IOP from baseline was 78.9% (15/19) at 6 months and 68.4% at 36 months. The Early Manifest Glaucoma Trial showed that each increase (or decrease) of the IOP by 1 mmHg was associated with an approximately 10% increase (or decrease) in the risk of progressive visual field loss.20 However, we must consider a potential racial difference in the mean IOP. In the Early Manifest Glaucoma Trial, 48.2% (123/255) of participants had an IOP of 21 mmHg or higher.6 However, in the Tajimi Study performed in Japan, only 8% of the patients with POAG had an IOP of 22 mmHg or higher in the population older than 40 years, with the average IOP being 15.4±2.8 mmHg in the right eye and 15.2±2.8 mmHg in the left eye.21 The IOP is generally lower in Japanese patients compared with European or American patients.22 Higher baseline pressures lead to a greater percent reduction of the IOP with medication. In fact, our study demonstrated that the IOP reduction rate was correlated with the baseline IOP (Table 2 and Figure 3A). Thus, the IOP reduction rate would be smaller in Japanese patients due to lower baseline IOP levels. Considering these factors, an IOP reduction of 2.0±2.7 mmHg after switching to DTFC may be effective for the treatment of glaucoma.
There was no significant difference of IOP between the nonincreased and increased groups, after switching to DTFC (Figure 1B). However, the mean IOP reduction rate was greater in the increased group than in the nonincreased group at all visits (Figure 2B). This seems a reasonable result because the number of active ingredients was increased by switching to DTFC in the increased group. Another reason may be that the mean baseline IOP was higher in the increased group (14.4±3.1 mmHg) than in the nonincreased group (12.8±1.5 mmHg) (Figure 1B). A higher baseline IOP may lead to a larger percent reduction, resulting in a larger IOP reduction rate in the increased group than the nonincreased group.
The success rate of therapy was high even at 36 months (78.9%) (Figure 4). This result suggests that DTFC effectively controlled the IOP for 36 months, supporting its long-term efficacy. Univariate and multivariate analyses showed that the type of glaucoma (POAG) was associated with a lower success rate for IOP control (Table 3). The success rate also tended to be higher in the patients with NTG (85.7%) than in those with POAG (60.0%) at 36 months after switching (Figure 4B). POAG patients had a higher baseline IOP than the patients with NTG (16.4±3.4 vs 13.2±3.1 mmHg) (Figure 1C), while the type of glaucoma (POAG/NTG) and the baseline IOP were associated with each other. Thus, these results suggest that IOP reduction and long-term maintenance of a lower IOP are mainly mediated by the baseline IOP and the type of glaucoma (POAG). This interpretation is supported by the observation that a higher baseline pressure is associated with a greater percent reduction of IOP. Medications such as PGA and alpha-2 agonists may be required for patients with POAG or a high baseline IOP, in addition to switching to DTFC.
The present study had several limitations. The main limitation is that the study was not randomized and had no control group. Our study was also small (19 patients), leading to possible selection bias. Additionally, our patients had received many different antiglaucoma medications prior to switching into DTFC. The second limitation is that switching to a new medication generally improves adherence to treatment,11 so DTFC might have appeared to be more effective as a result. Third, the IOP was measured only in the morning – Konstas et al and Quaranta et al reported that daytime peak IOP is clinically important in predicting long-term glaucomatous progression.23,24 Moreover, timolol is effective during the daytime, and dorzolamide is effective at night.25 For that reason, DTFC and dorzolamide increase mean 24-hour diastolic ocular perfusion pressure, with a substantial reduction in IOP.26 Therefore, we need to measure IOP in the morning and evening.
In conclusion, DTFC achieved greater reduction of the IOP than prior medications and was well tolerated when administered for 36 months with/without other ophthalmic medications. There were no serious side effects of DTFC, and it may improve the adherence of patients with glaucoma.
Acknowledgment
This work was supported in part by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Disclosure
The authors report no conflicts of interest in this work.
References
Collaborative Normal-Tension Glaucoma Study Group. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Am J Ophthalmol. 1998;126(4):498–505. | ||
The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol. 2000;130(4):429–440. | ||
Drance S, Anderson DR, Schulzer M; Collaborative Normal-Tension Glaucoma Study Group. Risk factors for progression of visual field abnormalities in normal-tension glaucoma. Am J Ophthalmol. 2001;131(6):699–708. | ||
Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701–713; discussion 829–830. | ||
AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 12. Baseline risk factors for sustained loss of visual field and visual acuity in patients with advanced glaucoma. Am J Ophthalmol. 2002;134(4):499–512. | ||
Leske MC, Heijl A, Hyman L, Bengtsson B, Dong L, Yang Z; EMGT Group. Predictors of long-term progression in the early manifest glaucoma trial. Ophthalmology. 2007;114(11):1965–1972. | ||
Gordon MO, Torri V, Miglior S, et al; Ocular Hypertension Treatment Study Group; European Glaucoma Prevention Study Group. Validated prediction model for the development of primary open-angle glaucoma in individuals with ocular hypertension. Ophthalmology. 2007;114(1):10–19. | ||
Gordon MO, Beiser JA, Brandt JD, et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):714–720; discussion 829–830. | ||
European Glaucoma Society. Terminology and Guidelines for Glaucoma. 3rd ed. Savona: Editrice Dogma Srl; 2008. | ||
Rossi GC, Pasinetti GM, Sandolo F, Bordin M, Bianchi PE. From dorzolamide 2%/timolol 0.5% to brinzolamide 1%/timolol 0.5% fixed combination: a 6-month, multicenter, open-label tolerability switch study. Expert Opin Pharmacother. 2011;12(16):2425–2431. | ||
Konstas AG, Bányai L, Blask KD, et al. Intraocular pressure and safety in glaucoma patients switching to latanoprost/timolol maleate fixed combination from mono- and adjunctive therapies. J Ocul Pharmacol Ther. 2004;20(5):375–382. | ||
Sonty S, Henry JC, Sharpe ED, et al. Success rates for switching to dorzolamide/timolol fixed combination in timolol responders who are insufficiently controlled by latanoprost monotherapy. Acta Ophthalmol. 2008;86(4):419–423. | ||
Mizoguchi T, Ozaki M, Wakiyama H, Ogino N. Additive intraocular pressure-lowering effect of dorzolamide 1%/timolol 0.5% fixed combination on prostaglandin monotherapy in patients with normal tension glaucoma. Clin Ophthalmol. 2011;5:1515–1520. | ||
Hommer A, Kimmich F. Switching patients from preserved prostaglandin-analog monotherapy to preservative-free tafluprost. Clin Ophthalmol. 2011;5:623–631. | ||
Syed MF, Loucks EK. Update and optimal use of a brinzolamide-timolol fixed combination in open-angle glaucoma and ocular hypertension. Clin Ophthalmol. 2011;5:1291–1296. | ||
Zimmerman TJ, Stewart WC; Latanoprost Axis Study Group. Intraocular pressure, safety, and quality of life in glaucoma patients switching to latanoprost from monotherapy treatments. J Ocul Pharmacol Ther. 2003;19(5):405–415. | ||
Bayer A, Weiler W, Oeverhaus U, Skrotzki FE, Stewart WC; Xplore Observation Group. Two-year follow-up of latanoprost 0.005% monotherapy after changing from previous glaucoma therapies. J Ocul Pharmacol Ther. 2004;20(6):470–478. | ||
Haverkamp F, Wuensch S, Fuchs M, Stewart WC. Intraocular pressure, safety and quality of life in glaucoma patients switching to latanoprost from adjunctive and monotherapy treatments. Eur J Ophthalmol. 2004;14(5):407–415. | ||
Hamacher T, Schinzel M, Schölzel-Klatt A, et al. Short term efficacy and safety in glaucoma patients changed to the latanoprost 0.005%/timolol maleate 0.5% fixed combination from monotherapies and adjunctive therapies. Br J Ophthalmol. 2004;88(10):1295–1298. | ||
Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E; Early Manifest Glaucoma Trial Group. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol. 2003;121(1):48–56. | ||
Iwase A, Suzuki Y, Araie M, et al; Tajimi Study Group, Japan Glaucoma Society. The prevalence of primary open-angle glaucoma in Japanese: the Tajimi Study. Ophthalmology. 2004;111(9):1641–1648. | ||
Leske MC. Open-angle glaucoma – an epidemiologic overview. Ophthalmic Epidemiol. 2007;14(4):166–172. | ||
Konstas AG, Quaranta L, Mikropoulos DG, et al. Peak intraocular pressure and glaucomatous progression in primary open-angle glaucoma. J Ocul Pharmacol Ther. 2012;28(1):26–32. | ||
Quaranta L, Katsanos A, Russo A, Riva I. 24-hour intraocular pressure and ocular perfusion pressure in glaucoma. Surv Ophthalmol. 2013;58(1):26–41. | ||
Quaranta L, Gandolfo F, Turano R, et al. Effects of topical hypotensive drugs on circadian IOP, blood pressure, and calculated diastolic ocular perfusion pressure in patients with glaucoma. Invest Ophthalmol Vis Sci. 2006;47(7):2917–2923. | ||
Quaranta L, Miglior S, Floriani I, Pizzolante T, Konstas AG. Effects of the timolol-dorzolamide fixed combination and latanoprost on circadian diastolic ocular perfusion pressure in glaucoma. Invest Ophthalmol Vis Sci. 2008;49(10):4226–4231. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.