Back to Journals » Cancer Management and Research » Volume 12
Economic Burden and Predictors of Cost Variability Among Adult Cancer Patients at Comprehensive Specialized Hospitals in West Amhara, Northwest Ethiopia, 2019
Authors Hagos A, Yitayal M , Kebede A, Debie A
Received 19 September 2020
Accepted for publication 10 November 2020
Published 18 November 2020 Volume 2020:12 Pages 11793—11802
DOI https://doi.org/10.2147/CMAR.S282746
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ahmet Emre Eşkazan
Asebe Hagos, Mezgebu Yitayal, Adane Kebede, Ayal Debie
Department of Health Systems and Policy, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Correspondence: Ayal Debie
Department of Health Systems and Policy, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, P. O. Box 196, Gondar, Ethiopia
Tel +251 910151929
Email [email protected]
Background: Cancer is the second leading cause of death in the world and accounts for 5.8% of deaths in Ethiopia. High out-of-pocket payment for the cost of illness of cancer could be linked to the low adherence to cancer treatment. This study aimed to assess the economic burden and predictors of cost variability among adult cancer patients at comprehensive specialized hospitals in West Amhara, Northwest Ethiopia.
Methods: An institutional-based cross-sectional study was conducted from January to February 2019 at the University of Gondar and Felege Hiwot hospitals. The cost of illness of cancer was estimated using a bottom-up micro-costing approach. Direct costs of illness of cancer were measured by calculating out-of-pocket expenditure. The indirect costs were estimated using human capital model approach. Multiple linear regression was used to identify the predictors for the log-transformed data. Unstandardized β-coefficient with 95% CI and p-value < 0.05 were used to declare factors associated with cost of illness of cancer.
Results: The mean cost of cancer illness among adult patients was US$ 1103.7 ± 33.2, and median cost was US$ 951.0 with IQR of 822.1. Factors such as urban residents (β = 0.147; 95% CI: 0.047, 0.246), distance (β = 0.0007; 95% CI: 0.0002, 0.001), married (β = 0.125; 95% CI: 0.037, 0.212), higher education (β = 0.318; 95% CI: 0.202, 0.435), buying drugs at private facilities (β = 0.134; 95% CI: 0.026, 0.243), richest households (β = 0.320; 95% CI: 0.143, 0.496) and frequent cycles of chemotherapy (β = 0.093; 95% CI: 0.061, 0.125) were positively associated with cost, while being female patients (β = − 0.144; 95% CI: − 0.210, − 0.018) were negatively associated.
Conclusion: The cost of illness of cancer was high. The government, therefore, should expand health insurance and invest an additional budget to safeguard patients from financial catastrophic shock.
Keywords: adult cancer patients, cost, economic burden, hospitals, Ethiopia
Background
Cancer is a group of diseases characterized by the uncontrolled growth and spread of abnormal cells.1 It is the second leading cause of deaths globally, and approximately 70% of deaths occurred in low- and middle-income countries due to cancer.2 Cancer of trachea, bronchus, lung (TBL), liver, and stomach in men, and breast cancer, TBL, and colorectal cancers in women were the top leading causes of death.3 Cancer has been spreading unprecedentedly in Africa, and the continent has not yet adequately prepared to tackle this public health challenge.4 The burden of cancer overlaps with infectious diseases, such as HIV/AIDS, tuberculosis, hepatitis virus, and human papillomavirus in low- and middle-income countries.5
Studies indicate that approximately 150 cases per 100,000 cases attributed to cancer and 800 per 100,000 non-communicable diseases in Ethiopia,6 and cancer accounted for about 5.8% of the total mortality in the country.7 It is also the second leading causes of death from non-communicable diseases next to cardiovascular disorders.8 The cost of illness of cancer has an impact on the personal financial wellness of cancer patients and their families due to the loss of family income and the increased expense of out-of-pocket payment (OOP) for medical and non-medical expenditures.9 As a result, cancer can lead to catastrophic effects with several consequences including a reduction in total household earnings and cut-back on “extras” such as social expenditures or holidays, sale of existing family assets, borrowing money, and triggering for psychological problems.10 Cancer treatment might be inequitable and lead to the risk of catastrophic shock since many countries rely on OOP payments for treatment.11 This high OOP expenses can lead to impoverishment among patients in low- and middle-income countries like Ethiopia.12 However, the cost of illness of cancer and associated factors has not been well investigated in Ethiopia. Therefore, this study aimed to assess the economic burden and predictors of cost variability among adult cancer patients at Comprehensive Specialized Hospitals in West Amhara, Northwest Ethiopia.
Methods and Materials
Study Settings and Period
An institution-based cross-sectional study was conducted using a micro-costing bottom-up approach among adult cancer patients attending at University of Gondar and Felege Hiwot comprehensive specialized hospitals from January to February 2019. The hospitals are located in Gondar and Bahir Dar towns which are 738 km and 564 km away from Addis Ababa (the capital city of Ethiopia), respectively. University of Gondar Comprehensive Specialized Hospital (UoGCSH) is expected to serve about 5 million people while Felege Hiwot Comprehensive Specialized Hospital (FHCSH) is also expected to serve about 7 million people. The University of Gondar and Felege Hiwot comprehensive specialized hospitals offer diagnosis and treatment for more than 400,000 and 250,000 patients per year, respectively. These hospitals are the only hospitals that have oncology centers in the Western part of Amhara National Regional State, Ethiopia.
Population and Sampling Procedures
All adult patients diagnosed with cancer who had been attending at UOGCSH and FHCSH were the source population of the study, while all adult cancer patients who were attending at these hospitals for at least one year and had followed up were the study population. All adult cancer patients who had histological or pathological confirmed cancer and took at least one cycle of cancer chemotherapy were included in this study. The sample size was determined using a single population mean formula with an assumption of Z(a/2) at 95% Confidence Level (CL = 1.96, standard deviation ( US$ 1.95), 5% of the mean of a margin of error (d= US$ 3.77)13 and 10% non-response rate. Therefore, the final sample size was 464. The sample was proportionally allocated to each hospital based on their average number of cancer patients attended in these hospitals. A consecutive sampling technique was used to select study participants. All adult cancer patients whose age greater than 18 years were included, but cancer patients who had less than 12 months for cancer care follow up were excluded from the study.
US$ 1.95), 5% of the mean of a margin of error (d= US$ 3.77)13 and 10% non-response rate. Therefore, the final sample size was 464. The sample was proportionally allocated to each hospital based on their average number of cancer patients attended in these hospitals. A consecutive sampling technique was used to select study participants. All adult cancer patients whose age greater than 18 years were included, but cancer patients who had less than 12 months for cancer care follow up were excluded from the study.
Measurements and Methods of Cost Estimation
Direct cost, indirect cost, and intangible costs are the major component of the cost of illness studies. In this study, direct and indirect costs of illness were the main cost categories, whereas intangible costs were excluded. Intangible costs are usually relating to suffering (eg, pain) and grief from illness and its cost is not included due to its subjective nature of measurement.14 Direct medical costs are expenditures that incurred related to medical treatment such as consultation, diagnostic, medication, surgery, hospitalization costs, while, direct nonmedical costs are expenditures that do not relate directly to medical treatment like transport, bed rent, food costs during the course of cancer treatment. On other hand, indirect cost is the value of lost production (income lost) because of reduced working time for patients during the illness period or while seeking cancer treatment. The cost of cancer illness was measured for a one-year time frame using a prevalence-based approach and estimated by micro-costing with bottom-up technique. Micro-costing is a cost estimation method that involves direct enumeration and costing out of all relevant inputs. It measures the actual resources and economic costs by collecting detailed data on resources utilized and the unit costs of those resources.15,16 Direct costs of cancer illness were all out-of-pocket expenditures for the cost of illness in the last 12 months who have spent on the course of diagnosing and seeking cancer treatment. The indirect cost of cancer illness was calculated by using the Human Capital Model (HCM) approach.
Accordingly, the indirect cost, the number of working days lost was multiplied by the daily wage rate. For monthly paid patients and companion was estimated by dividing their net monthly salary by 30 days. The wage rate is based on patient reports. The cost for unemployed, students and patients who were not able to work due to physical or mental disability was not incorporated in the cost estimation.17 Additionally, the wages of unpaid patients such as the cost of housewives were calculated using the 2013 average monthly wage rate for agricultural workers’ National Labor Force Survey (NLFS) report for Ethiopia ETB 697 (US$24.46).18 The unit of measurement for direct and indirect costs of illness was Ethiopian Birr and the exchange rate to US$ during the time of the study was (1 US$ = 28.49 ETB). Out-Of-Pocket (OOP) expenditures are payments made by a household for care and treatment for cancer illness without compensations from a third party. The wealth status of participants was determined using Principal Component Analysis (PCA) and classified as the poorest, poor, middle, rich and richest. The psychological aspect of financial hardship was measured using the clients’ perceived judgment of whether they worried or faced financial constraints to pay for cancer illness.
Data Collection Tools and Procedures
An interviewer administered semi-structured questionnaire was developed through reviewing different literature.13,17,19 The questionnaire was first prepared in English then translated to Amharic and back to English to check its consistency. The questionnaire contains socio-demographic variables, clinical characteristics of patients, indirect costs, direct costs, and other variables. Five diploma graduated clinical nurses for data collectors and two BSc graduated nurses for supervisors were recruited and one-day training was given for them on the basic techniques of data collection. The questionnaire was also pretested among 25 adult cancer patients attending at University of Gondar comprehensive specialized hospital and the necessary modification was made based on the pre-test findings. The participants of the pre-test were excluded from the final study. The exit interview was conducted among outpatients and at the time of discharge for inpatients to capture all expenditures. The supervisors ensured the quality, completeness, and consistency of data. The principal investigator made a spot-checking to review the completed questionnaire to ensure completeness and consistency of the collected information.
Data Management and Analysis
Data were entered and analyzed using EPI-INFO version 7 and Stata version 14, respectively. Descriptive statistics such as frequency, proportion, mean, standard deviation, median, and IQR were calculated and presented using graphs and tables. Linear regression assumption tests, such as normality, linearity, independence, homoscedasticity, and multi-collinearity were checked. Shapiro–Wilk test was significant and the data were positively skewed to the right so that the normality assumption for linear regression model was not fulfilled. As a result, the outcome variable, cost of cancer, was log-transformed and after transformation, the assumptions had met. Data were analyzed using the log-transformed data, and reported in percentage after transformation to percent [(eβ) −1)] *100;20 e=2.71 and β: stands for unstandardized β-coefficient value. Independent variables having p-value of less than 0.2 during bivariable analysis were entered into the multiple linear regression model to identify the potential predictors for the cost of cancer illness. Finally, the transformed value of unstandardized β–coefficient with 95% CI and p-value less than 0.05 were used to declare the variables significantly associated with the cost of cancer illness.
Results
Socio-Demographic and Economic Characteristics
A total of 464 cancer patients participated in the study. The study shown that among the study participants, 72.4% were females, 83.8% were Orthodox Christians, and 60.8% were unable to read and write. The mean age of the participants was 47± (14SD) years. The mean monthly household income of respondents was US$ 166.6 ± (76.5 SD) and the median income was US$ 40.7 with an IQR of 119.3. The average household family size of the participants was six. Additionally, 57.5% of cancer patients resided 50 or more kilometers away from the hospitals, and 52.6% of the participants resided in rural areas (Table 1).
 |
Table 1 Socio-Demographic and Economic Characteristics of Study Participants at UOGCHS and FHCHS, West Amhara, Northwest Ethiopia, 2019 (n=464) |
Distribution of Cancer by Type
Breast (24.6%), cervical (23.7%), and colorectal (14.6%) were the three leading cancers in the study area. Colorectal (25.8%), leukemia (14.8%), and lung cancer (11.7%) were the common cancer illness among males; and Cervical (32.7%), breast (32.1%), and colorectal (10.4%) cancers were the three leading cancer illnesses among women in the study area. Breast, cervical, and ovarian cancer account for nearly half (49.7%) of the total cancer types (Table 2).
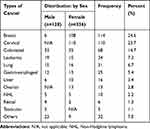 |
Table 2 Distribution of Cancer Type Among Study Participants at UoGCSH and FHCSH, West Amhara, Northwest Ethiopia, 2019 (n=464) |
Clinical Characteristics of Cancer Patients
More than ninety percent (92.2%) of the participants had three or more hospital visits in the last 12 months. The majority (65.1%) of the patients received both chemotherapy and surgical treatment modalities. The study indicated that 22.0% of participants had got healthcare services related to cancer, 84.1% of patients had at least one admission in the last 12 months. The study also revealed that 84.1% of cancer patients were admitted and treated as inpatients in which 65.1% of participants stayed as inpatients for more than 10 days (Table 3).
 |
Table 3 Clinical Characteristics of Study Participants at UoGCSH and FHCSH, West Amhara, Northwest Ethiopia, 2019 (n=464) |
Economic Burden of Cancer Illness
The overall mean cost of cancer illness among adult patients over 12 months was US$ 1103.7 ± (33.2 SD) or ETB 31,444.4± (945.9 SD), and the median cost of cancer illness was estimated to be US$ 951.0 with IQR of 822.1 or ETB 27,094.0 with IQR of 23,421.6. The mean direct cost was US$ 880.0± (25.2 SD), and the median cost was US$ 789.2 with an IQR of 708.4. Cancer patients had incurred the largest cost for medications (drugs) with a mean cost of US$ 562.5± (212.2 SD) and the median cost was US$ 486.1 with IQR 530.0. The study indicated that the mean number of days participants remained ill in the past 12 months was 211.5 ± (5.1 SD) and the median was 190 with an IQR of 222.5 days; the mean number of days patients remained out of work was 104.9 ± (3.5 SD) and the median was 90.0 with IQR of 90 days, and the mean wage lost (indirect cost cancer illness) was estimated to be US$ 223.7±16.1SD and the median was US$ 107.4 with IQR of 180.4 (Table 4).
 |
Table 4 Cost of Illness Among Adult Cancer Patients Attended at UoGCSH and FHCHS, West Amhara, Northwest Ethiopia, 2019 (n=464) |
Sources of Money for Cancer Treatment
The study revealed that 35.7% of the participants were saving some amount of money from their monthly income to cover the cost of cancer illness. The majority (67.1%) of cancer patients sold their assets, such as household items, live stocks, and farmland to cover their cost of cancer illness. Nearly one-third (32.3%) of the participants covered their cost of cancer illness by their families’ and relatives’ supports. The study also revealed that 21.8% of the study participants borrowed money to cover their treatment. Moreover, 12.9% of the participants were Community-Based Health Insurance (CBHI) users and 17.9% were fee waiver package users. The study reported that 76.1% of cancer patients had faced psychological aspects of financial hardship during cancer treatment (Table 5).
 |
Table 5 Source of Money for the Cost of Cancer Illness Among Patients at UOGCSH and FHCSH, West Amhara, Northwest Ethiopia, 2019 (n=464) |
Factors Associated with the Cost of Cancer Patients
Female cancer patients (β = −0.144; 95% CI: − 0.210, − 0.018) were incurred a lower cost for cancer illness by 13.4% compared with male. The cost of cancer illness among urban residents (β = 0.147; 95% CI: 0.047, 0.246) was increased by 15.8% compared with their counterparts. When the place of residence of cancer patients is far from the hospital by 1 km increased (β = 0.0007; 95% CI: 0.0002, 0.001) the cost of illness by 0.07%. Married participants (β = 0.125; 95% CI: 0.037, 0.212) were incurred a higher cost of treatment by 13.3% compared with unmarried. The cost of cancer illness was higher among higher education attended respondents (β = 0.318; 95% CI: 0.202, 0.435) by 37.4% compared with uneducated participants. The cost of cancer illness among participants who bought drugs at private facility (β = 0.134; 95% CI: 0.026, 0.243) were increased by 14.3% than patients who bought at public health facility. Participants categorized under the richest wealth status (β = 0.320; 95% CI: 0.143, 0.496) were incurred higher cost by 37.7% compared with the poorest participants. When the cycles of chemotherapy among patients with cancer increased with one unit (β = 0.093; 95% CI: 0.061, 0.125), the cost of treatment for cancer was increased by 9.7% (Table 6).
 |
Table 6 Factors Associated with Cost of Cancer Illness Among Patients at UoGCSH and FHCSH, West Amhara, Northwest Ethiopia, 2019 (n=464) |
Discussion
Results from this study indicated that cancer patients experienced several financial challenges, and this research adds compelling evidence to the arguments for effective cancer control policies and timely access to affordable treatment in low- and middle-income countries. This study revealed that the overall mean cost of cancer illness among adult patients was US$ 1103.7 ± (33.2 SD), and the median was also estimated to be US$ 951.0 with an IQR of 822.1. This finding was higher than the cost of cancer in a study done at Addis Ababa, Ethiopia with the mean cost of US$ 407.2 and median US$ 206.917 and lower than the studies conducted in Anhui, China US$ 1671.821 and India US$ 1715.0.22 The possible explanation for this cost variability might be due to the difference in the study period and health care setups. Additionally, it might be due to the differences in design and study area.
The mean direct cost of cancer in the study area was US$ 880.0 ± (25.2SD). This finding was lower than the study done at Tikur Anibesa Specialized Hospital (TASH) Addis Ababa, Ethiopia (US$ 1188.3).23 The possible justification might be due to the difference in the study area and cancer cases. In this study, the cost of illness for all cancer patients who had got any kind of treatment for at least 12 months was taken into consideration. However, the previous study focused on the cost of breast cancers only. Direct medication costs accounted for the highest share of costs followed by investigation cost for cost of cancer illness with a mean cost of medications (drugs, surgery, and hospitalization) was US$ 644.1 ± 28.0, and US$ 138.0 ± 6.8, respectively. This finding was lower than studies done in India with a mean medication cost of (US$751.0), and investigation (US$304.0),19 and TASH Addis Ababa, Ethiopia (US$ 898.1).23 This implies that cancer patients did not have adequate medical cover, particularly to cover the direct medical costs to relieve their financial burden and they largely needed financial support to enable them to meet the costs of care. The government of Ethiopia, therefore, introduces another financial reimbursement modality or included in the list of exempted services to cover the cost of cancer illness and reduce their catastrophic shock.
The mean loss of working days was 104.9 days ± (3.5 SD) and the median was 90 days with IQR 90 days, and the mean indirect cost US$ 223.7± (16.1SD). This finding was lower than a study conducted in India US$ 495.524 and higher than a study conducted in Addis Ababa Ethiopia US$ 84.7.17 This indicated that the indirect cost of cancer illness was also one of the major financial challenges/burdens for patients to receive the healthcare services, however, this has not yet got attention. This might lead the cancer patients to have poor adherence to their treatment.
Female cancer patients incurred a lower cost of illness by 13.4% compared with male patients. This finding was consistent with a study done in Pakistan.25 The possible justification might be due to women might not have access to all cancer diagnostic and treatment services because of their low decision-making power and financial resources in the household and this might lower the cost of treatment. On the contrary, this finding was contradicted with the studies done in Vietnam26 and Europe.27 The possible justification might be due to the methods for indirect cost estimation which means the HCM approach had considered patients earning for cancer illness. These groups often expressed their cost in terms of the kind that might be underestimated while converting their earning into monetary value. Moreover, the economic burden of cancer among women is difficult to measure using HCM because most females involve in non-income generating household works, such as preparing foods and caring for children.28,29
The cost of cancer illness among patients who attended a higher level education was increased by 37.4% compared with that of participants who had no formal education. This study is in line with the study done in Vietnam.26 This might be due to the fact that educated participants could have a good understanding of health, better health-seeking behavior, regular medical follow up, and able to buy or use all the prescribed drugs and investigations. Regarding chemotherapy, as the cycles of chemotherapy among patients with cancer increased with one unit, the cost of treatment was increased by 9.7%. This finding is consistent with a study on cancer‐related financial problems to decide the delay of medical care.30 The possible justification might be the frequency of medications can expose patients to additional medical expenses.
The cost of cancer illness among participants who bought drugs at the private facility was increased by 14.3% than that of cancer patients who had got drugs at public health facilities. The possible justification might be the cost of drugs in the private health facility was high since they are profitable organizations. This also implies that the healthcare policymakers and managers had not given more emphasis on the availability of the diagnostic modalities and drugs at public healthcare facilities to alleviate the financial risk related to cancer illness. Therefore, it is better to design the reimbursement mechanism for those patients who bought the drugs and received diagnostic services at the private facility in relation to the unavailability of the services.
Richest participants incurred a higher cost of cancer illness by 37.7% compared with the poorest. This finding was supported by a study done in India.22 This finding indicated that patients with the highest wealth status spend more on their health and can afford all cancer care and treatment services. However, the proportion of expenditure for cancer care and treatment might be higher among the poorest, and it is supported by a study report in Pakistan.25
In this study, 12.9% and 17.9% of the costs of cancer illness was covered by CBHI and fee waiver systems, respectively. This finding is similar to the previous studies done in Pakistan25 and Ethiopia.31 Two-thirds of patients (67.1%) sold their assets and 23.3% borrowed money from their relatives for their treatment. This finding is supported by the studies done in India.22,24 However, the CBHI scheme and fee waiver package only cover direct medical costs. Cancer patients might sell their assets to cover the non-medical costs such as food, transportation, and other accommodation costs and this could make patients in catastrophic health expenditure. The high out-of-pocket payment for the cost of cancer illness could also be linked with the lower adherence to cancer treatment. The limitation of this study was that it has not measured intangible costs in the cost estimation. Moreover, the indirect cost of cancer illness has been calculating based on the patient’s self-report. This might lead to over or under-reporting of the cost of illness and prone to recall bias. The cost of cancer illness was not assessed by the type of cancer (organ involved) was one of the other limitations.
Conclusion
The overall mean cost of illness for adult cancer patients was high. Direct costs for cancer illness were the major costs and the cost of drugs accounting for the highest share of the cost of illness. Factors such as sex of participants, educational status, buying drugs at the private health facility, cycles for cancer chemotherapy, distance, and wealth status were significantly associated with the cost of cancer illness. Therefore, the government should design financial protection mechanisms such as CBHI and SHI for reducing the cost of cancer illness which leads to catastrophic expenditure for the patients. Furthermore, hospitals should fulfill all the necessary diagnostic facilities and promote early detection of cancer. Researchers have better conduct a longitudinal study at the national level to evaluate the impact and level of impoverishment as a result of cancer illness. Future researchers have better assessed the cost of cancer illness by the type of cancer disease (organ involved).
Abbreviations
COI, cost of illness; ETB, Ethiopian Birr; FCSH, Felege Hiwot Comprehensive Specialized Hospital; IQR, inter-quartile range; NCD, non-communicable disease; OPP, out-of-pocket; TASH, Tikur Anbessa Specialized Hospital; UOGCSH, University of Gondar Comprehensive and Specialized Hospital; WHO, World Health Organization.
Data Sharing Statement
Datasets supporting the conclusions of this article are available upon request to the corresponding author.
Ethical Approval and Consent to Participate
This study was conducted in accordance with the Declaration of Helsinki. Ethical clearance was obtained from the Ethical Review Committee of Institute of Public Health, College of Medicine and Health Sciences, University of Gondar. Permission letter was also obtained from Amhara National Regional Health Bureau and the respective hospitals. Written informed consent was taken from each participant. Moreover, verbal informed consent was obtained from those participants who did not able to read and write, and this was approved by the ethical committee. Each eligible participant was informed about the purpose of the study. Participants were also assured that their name was not written on the questionnaire and confidentiality of the data kept at all levels.
Acknowledgments
Authors would like to thank the Institute of Public Health, College of Medicine and Health sciences, the University of Gondar for giving an opportunity to study in this area. This manuscript is part of master thesis work for the principal investigator. In addition, our gratitude goes to Amhara National Regional State Health Bureau and the respective hospital staffs for their co-operation. Finally, we would like to thank the participants and data collectors for their contribution in the study.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study was sponsored by the principal investigator.
Disclosure
The authors report no conflicts of interest for this work and declare that there are no conflicts of interest regarding the publication of this paper.
References
1. Society AC. Global Cancer Facts & Figures 3rd Edition. Am Cancer Soc. 2015;800:1–64.
2. World health organization Wafai ZA. Key Cancer Facts; 2018.
3. Fitzmaurice C, Allen C, Barber RM; Global Burden of Disease Cancer C. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3(4):524–548. doi:10.1001/jamaoncol.2016.5688
4. Adewole I, Martin DN, Williams MJ, et al. Building capacity for sustainable research programmes for cancer in Africa. Nat Rev Clin Oncol. 2014;11(5):251–259. doi:10.1038/nrclinonc.2014.37
5. Abegaz TM, Ayele AA, Gebresillassie BM. Health Related Quality of Life of Cancer Patients in Ethiopia. J Oncol. 2018;2018:1467595. doi:10.1155/2018/1467595
6. Awoke Misganaw DHM, Ali A. Epidemiology of Major Non-communicable Diseases in Ethiopia: A Systematic Review. J Health Popul Nutr. 2014;32(1):1–13.
7. Health FMO. National Cancer Control Plan 2016–2020. This Prev Control Dir. 2015:10;83.
8. Memirie ST, Habtemariam MK, Asefa M, et al.Estimates of Cancer Incidence in Ethiopia in 2015 Using Population-Based Registry Data. J Global Oncol. 2018;(4):1–11. doi:10.1200/JGO.17.00175
9. Barry R, AV Meisenberg, Ellis ERIN. Patient Attitudes Regarding the Cost of Illness in Cancer Care. TheOncologist. 2015;19;24.
10. Owenga JA, Nyambedha EO. Perception of Cervical Cancer Patients on their Financial Challenges in Western Kenya. BMC Health Serv Res. 2018;18(1):261. doi:10.1186/s12913-018-3073-2
11. Azzani M, Roslani AC, Su TT. The perceived cancer-related financial hardship among patients and their families: a systematic review. Supportive Care Cancer. 2015;23(3):889–898. doi:10.1007/s00520-014-2474-y
12. Erku DA. Complementary and Alternative Medicine Use and Its Association with Quality of Life among Cancer Patients Receiving Chemotherapy in Ethiopia: A Cross-Sectional Study. Evidence Based Complementary Alternative Med. 2016;2016:2809875.
13. Pavel MS, Chakrabarty S, Gow J. Cost of illness for outpatients attending public and private hospitals in Bangladesh. Int J Equity Health. 2016;15(1):167.
14. Pavel MS, Chakrabarty S, Gow J. Cost of illness for outpatients attending public and private hospitals in Bangladesh. Int J Equity Health. 2016;15(1):167. doi:10.1186/s12939-016-0458-x
15. Weinstein MC, Russell LB, Gold MR. Cost-Effectiveness in Health and Medicine. Oxford university press; 1996.
16. Xu X, Nardini HKG, Ruger JP. Micro-costing studies in the health and medical literature: protocol for a systematic review. Syst Rev. 2014;3(1):47. doi:10.1186/2046-4053-3-47
17. A MD H, Mariam DH. Patient side cost and its predictors for cervical cancer in Ethiopia: a cross sectional hospital based study. BMC Cancer. 2013;13(1):69. doi:10.1186/1471-2407-13-69
18. Hailu A, Lindtjorn B, Deressa W, Gari T, Loha E. Economic burden of malaria and predictors of cost variability to rural households in south-central Ethiopia. PLoS One. 2017;12(10):e0185315. doi:10.1371/journal.pone.0185315
19. KS RS N, Tiwari VK, Piang LK, Piang LK. Cost of Treatment for Cancer: experiences of Patients in Public Hospitals in India. Asian Pacific J Cancer Prevent. 2013;14(9):5049–5054.
20. Library. UoV: interpreting Log Transformations in a Linear Model. https://data.library.virginia.edu/interpreting-log-transformations-in-a-linear-model/.
21. Zhao T, Cheng J, Chai J, et al. Inpatient care burden due to cancers in Anhui, China: a cross-sectional household survey. BMC Public Health. 2016;16(1):308. doi:10.1186/s12889-016-2995-z
22. Rajpal S, Kumar A, Joe W, Virgili G. Economic burden of cancer in India: evidence from cross-sectional nationally representative household survey, 2014. PLoS One. 2018;13(2):e0193320. doi:10.1371/journal.pone.0193320
23. G WA M, Lemma S. Cost of Illness of Breast Cancer Patients on Chemotherapy in Addis Ababa Public Hospitals, the Case of Tikur Anbessa Specialized Teaching Hospital-Cross-Sectional Types of Study. Health Eco Outcome Res. 2017;03:04.
24. Nair KS, Raj S, Tiwari VK, Piang LK. Cost of treatment for cancer: experiences of patients in public hospitals in India. Asian Pacific J Cancer Prevent. 2013;14(9):5049–5054. doi:10.7314/APJCP.2013.14.9.5049
25. Zaidi AA, Ansari TZ, Khan A. The financial burden of cancer: estimates from patients undergoing cancer care in a tertiary care hospital. Int J Equity Health. 2012;11(1):60. doi:10.1186/1475-9276-11-60
26. Hung NV, Giang PTH. CENPHER five year report 2009–2014: from a research project to a research center: ILRI (aka ILCA and ILRAD). Int J Med. 2014.
27. Hanly P, Soerjomataram I, Sharp L. Measuring the societal burden of cancer: the cost of lost productivity due to premature cancer‐related mortality in E Europe. Int j Cancer. 2015;136(4):E136–E145. doi:10.1002/ijc.29105
28. Sarker M, Krishnan S, Parham G, et al. The global burden of women’s cancers: a grand challenge in global health. This Prev Control Dir. 2016.
29. Rice DP, Hodgson TA. The economic costs of illness: a replication and update. Health Care Financ Rev. 1985;7(1):61.
30. Kent EE, Forsythe LP, Yabroff KR, Weaver KE, de Moor JS, Rodriguez JL. Are survivors who report cancer‐related financial problems more likely to forgo or delay medical care? Cancer. 2013;119(20):3710–3717. doi:10.1002/cncr.28262
31. Erku DA. Complementary and alternative medicine use and its association with quality of life among cancer patients receiving chemotherapy in Ethiopia: a cross-sectional study. Evid Based Complement Alter Med. 2016;2016:1–8. doi:10.1155/2016/2809875
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
