Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Early response to inhaled bronchodilators and corticosteroids as a predictor of 12-month treatment responder status and COPD exacerbations
Authors Calverley PM , Postma D, Anzueto A, Make B , Eriksson G , Peterson S, Jenkins C , Clowes C
Received 29 July 2015
Accepted for publication 21 December 2015
Published 25 February 2016 Volume 2016:11(1) Pages 381—390
DOI https://doi.org/10.2147/COPD.S93303
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Peter M Calverley,1 Dirkje S Postma,2 Antonio R Anzueto,3,4 Barry J Make,5 Göran Eriksson,6 Stefan Peterson,7 Christine R Jenkins8
1Pulmonary and Rehabilitation Research Group, University Hospital Aintree, Liverpool, UK; 2Department of Pulmonary Medicine and Tuberculosis, Gronigen Research Institute for Asthma and COPD, University Medical Center Groningen, University of Groningen, Groningen, the Netherlands; 3Division of Pulmonary Diseases and Critical Care Medicine, University of Texas Health Sciences Center, School of Medicine, University of Texas, 4South Texas Veterans Health Care System, San Antonio, TX, 5Division of Pulmonary Sciences and Critical Care Medicine, National Jewish Health, University of Colorado, Denver, CO, USA; 6Department of Respiratory Medicine and Allergology, University Hospital, 7StatMind AB, Lund, Sweden; 8George Institute for Global Health, Concord Clincal School, The University of Sydney, Sydney, NSW, Australia
Background: Early treatment response markers, for example, improvement in forced expiratory volume in 1 second (FEV1) and St George’s Respiratory Questionnaire (SGRQ) total score, may help clinicians to better manage patients with chronic obstructive pulmonary disease (COPD). We investigated the prevalence of clinically important improvements in FEV1 and SGRQ scores after 2-month budesonide/formoterol or formoterol treatment and whether such improvements predict subsequent improvements and exacerbation rates.
Methods: This post hoc analysis is based on data from three double-blind, randomized studies in patients with moderate-to-very-severe COPD receiving twice-daily budesonide/formoterol or formoterol alone for 6 or 12 months. Prebronchodilator FEV1 and SGRQ total score were measured before treatment and at 2 and 12 months; COPD exacerbation rates were measured during months 2–12. Responders were defined by ≥100 mL improvement in prebronchodilator FEV1 and ≥4-point decrease in SGRQ total score.
Results: Overall, 2,331 and 1,799 patients were included in the 0–2- and 0–12-month responder analyses, respectively, and 2,360 patients in the 2–12-month exacerbation rate analysis. At 2 months, 35.1% of patients were FEV1 responders and 44.3% were SGRQ responders. The probability of response was significantly greater with budesonide/formoterol than with formoterol or placebo for both parameters. Two-month responders had a greater chance of 12-month response than 2-month nonresponders for both FEV1 (odds ratio, 5.57; 95% confidence interval, 4.14–7.50) and SGRQ (odds ratio, 3.87; 95% confidence interval, 2.83–5.31). Two-month response in FEV1 (P<0.001), but not SGRQ (P=0.11), was associated with greater reductions in exacerbation risk.
Conclusion: Early FEV1 and SGRQ treatment responses relate to their changes at 12 months. FEV1 response, but not SGRQ response, at 2 months predicts the risk of a future COPD exacerbation in some, but not all patients. This is potentially useful in clinical practice, although more sensitive and specific markers of favorable treatment response are required.
Keywords: anti-inflammatories, bronchodilator effect, chronic obstructive pulmonary disease, predictors, risk assessment, risk factors
Introduction
Inhaled long-acting β2-agonists (LABAs), alone or in combination with inhaled corticosteroids (ICS), improve lung function and clinical outcomes in patients with chronic obstructive pulmonary disease (COPD).1–3 Some outcomes, such as improvements in exercise capacity and breathlessness, occur after a single dose of a bronchodilator.4,5 However, for other important events, such as exacerbations, time must elapse before the effect of treatment is clear. The current recommendations for treatments that prevent exacerbations, an important future risk for patients with COPD,6 are based on the average benefit of therapy seen in large patient populations, normally in trials of 12 months’ duration. Identification of an easily measurable disease marker that identifies individuals likely to benefit from continued treatment would aid clinical decision making and prognostication.
Two potential markers of early treatment effect are the change in lung function and in health status during treatment, evaluated by change in forced expiratory volume in 1 second (FEV1) and St George’s Respiratory Questionnaire (SGRQ) total score, respectively. Both markers improve within days or weeks of bronchodilator treatment,7–9 and each has a defined clinically important difference (CID) that could serve as a threshold to identify change. A 100 mL increase in FEV1 during the recovery period from an exacerbation identified patients less likely to have a subsequent relapse, lending support to the utility of this threshold for CID.10 However, before accepting these variables as being useful, it is crucial to determine: 1) the prevalence of early CID in these outcomes related to treatment; 2) the consistency of early responses over time; and 3) the impact of early response on future exacerbation risk.
To address these questions, we performed a post hoc analysis of data from published trials in which the LABA formoterol, given alone via a dry powder inhaler, was compared with a fixed-dose combination of formoterol and the ICS budesonide, given via a pressurized metered-dose inhaler, over 6–12 months in patients with moderate-to-very-severe COPD at risk of exacerbations.3,11,12
Methods
Study design and patient population
This post hoc analysis is based on data from three multicenter, randomized, double-blind, double-dummy, parallel-group clinical trials of 6 (ClinicalTrials.gov identifier: NCT002061543) and 12 (NCT0020616711 and NCT0041974412) months’ duration in patients with moderate-to-very-severe COPD.
The studies recruited patients ≥40 years of age with COPD and symptoms for >2 years, a smoking history of ≥10 pack-years, prebronchodilator FEV1 ≤50% predicted, FEV1/forced vital capacity ratio of <0.7, modified Medical Research Council dyspnea score ≥2, and a history of ≥1 COPD exacerbation requiring systemic corticosteroids and/or antibiotics within 1–12 months of inclusion. Patients were randomized to receive two inhalations twice daily of budesonide/formoterol 160/4.5 μg (via pressurized metered-dose inhaler) or formoterol 4.5 μg (via dry powder inhaler) for 63 or 1211,12 months. Two studies3,11 included a placebo control group. All participants provided written informed consent and the studies received appropriate ethical approval.
Study assessments
All studies assessed prebronchodilator FEV1 and SGRQ total score at baseline and 2 months postrandomization and, in two of the studies,11,12 also at 12 months. Spirometry was performed according to the American Thoracic Society guidelines.13 COPD exacerbations, defined as worsening symptoms requiring oral corticosteroids and/or hospitalization, were recorded throughout the study periods.
In the present analysis, changes in FEV1 (≥100 mL improvement in prebronchodilator FEV18,14,15) and SGRQ total score (≥4-point decrease [ie, an improvement]16) from 0 to 2 months were used as thresholds to investigate the frequency of response over 0–2 months of treatment (a commonly used clinical follow-up interval). From these 2-month responses, we investigated: 1) the stability of early 2-month FEV1 and SGRQ responses in the two 12-month studies11,12 and 2) the rate of exacerbations during months 2–12 in the responder subgroups of all three studies.3,11,12 Data from the placebo-controlled studies3,11 were analyzed to provide information about spontaneous improvement in the early response measurement. The 6-month study was included in order to evaluate short-term response, including placebo as a control; this approach was necessary in order to achieve the optimum number of patients.
Data analyses and statistical methods
Both FEV1 and SGRQ data were described as continuous variables and binary outcomes defined by their respective thresholds.
Changes in FEV1 and SGRQ total score from 0 to 2 months were compared between treatments using analysis of variance, with treatment and study as factors and the baseline value as a covariate. The proportion of patients achieving an FEV1 or SGRQ response during 0–2 months was compared between all treatments using logistic-regression analysis, with treatment and study as factors. The responder analysis from 0 to 2 months postrandomization excluded patients with missing baseline FEV1 or SGRQ total score data.
The 0–12-month analysis was restricted to the formoterol and budesonide/formoterol groups because of high dropout rates in the placebo groups during the follow-up period of the studies, a finding noted previously.17 Changes in FEV1 and SGRQ total score from 0 to 12 months were analyzed using a linear model, with treatment and study as factors and baseline values and change from 0 to 2 months as covariates. The odds ratio (OR), with 95% confidence intervals (CIs), of being a 12-month responder was analyzed using logistic-regression analysis with study, treatment, and 2-month response as factors. The interaction between treatment allocation and 2-month FEV1 and SGRQ response rates was also investigated.
In subjects achieving thresholds of ≥100 mL improvement in FEV1 and a decrease of ≥4 points in SGRQ total score at 2 months, exacerbation rates (events per patient per year) by response and treatment were estimated using a Poisson model, with treatment, study, response, and treatment response interaction as factors. Rate ratios between treatments and response groups, with 95% CIs and P-values, were calculated. In addition, exacerbation rates after the 2-month visit were analyzed using a Poisson model with treatment and study as factors; covariates were baseline values and change in FEV1 and SGRQ total scores over 0–2 months, adjusted for the remaining observation time and over-dispersion.
Results
Patient demographics and clinical characteristics
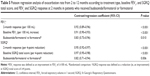
A total of 2,331 and 1,799 patients were included in the 0–23,11 and 0–12-month11,12 responder analyses, respectively, and 2,360 patients were included in the 2–12-month exacerbation rate analysis.3,11,12 Missing data are described in the supplementary materials. There were no significant differences in baseline clinical or demographic characteristics among the three analyses (Table 1) and between the three different treatment groups included in the 0–2-month responder analysis (Table 2).
Two-month response in FEV1 and SGRQ as a predictor of longer-term response to ICS/LABA or LABA
At 2 months, an FEV1 response (≥100 mL improvement) was seen in 35.1% of patients (Figure S1A) and an SGRQ response (≥4-point improvement in total score) was seen in 44.3% of patients (Figure S2A). FEV1 responders had better baseline lung function and SGRQ responders had higher initial SGRQ total scores than the respective nonresponders (Tables S1 and S2). Responders took fewer maintenance medications (long-acting bronchodilators or ICS) at study entry than nonresponders (Tables S1 and S2).
The odds of being an FEV1 and SGRQ responder were significantly greater with budesonide/formoterol versus formoterol alone (OR, 1.56 [P<0.001] and OR, 1.36 [P<0.006], respectively) and for budesonide/formoterol versus placebo (OR, 2.21 [P<0.001] and OR, 1.42 [P=0.002], respectively) (Table 3). The budesonide/formoterol group had higher response rates than either formoterol- or placebo-treated patients over a range of cut-points for FEV1 and SGRQ score (Figure 1A and B, respectively).
At 12 months, the prespecified FEV1 and SGRQ responses were seen in 36.0% (Figure S1B) and 49.0% (Figure S2B) of patients, respectively. Responses at 2 months were highly predictive of 12-month response: an FEV1 response at 12 months was 5.6 times more likely among 2-month responders than nonresponders (OR, 5.57; 95% CI, 4.14–7.50; P<0.001) and a 12-month SGRQ response was 3.9 times more likely if the patient responded at 2 months (OR, 3.87; 95% CI, 2.83–5.31; P<0.001).
Two-month response in FEV1 and SGRQ as a predictor of exacerbations
Exacerbations during months 2–12 were significantly less frequent in FEV1 2-month responders than in nonresponders (P<0.001; Table 4). This effect was observed in both treatment groups. In 2-month FEV1 responders, reductions in 12-month exacerbation rates were similar for budesonide/formoterol and formoterol alone (Table 4). In 2-month FEV1 nonresponders, the 12-month exacerbation rate was significantly lower for budesonide/formoterol-treated patients compared with formoterol alone (P=0.015; Table 4; Figure 2A). Exacerbation frequency during months 2–12 was unrelated to SGRQ response at 2 months (32.2% vs 34.2%; Table 4; Figure 2B). However, exacerbations were less frequent with the budesonide/formoterol combination, irrespective of 2-month SGRQ response (Table 4; Figure 2B).
A Poisson analysis with treatment, baseline, and 2-month response as factors showed that improvements in 2-month FEV1 of ≥100 mL and SGRQ total score of ≥4 points were associated with an 8% and 5% decrease, respectively, in exacerbation frequency during months 2–12 (Table 5). Greater FEV1 (100 mL) and lower SGRQ score (−4 points) at baseline were also predictive of a decrease in exacerbation frequency (Table 5).
Discussion
In this post hoc analysis of data from published trials, we have shown that: 1) improvements in FEV1 and SGRQ total score after 12 months are more likely to be observed in patients showing an early 2-month treatment response compared with 2-month nonresponders; 2) a 2-month treatment response in FEV1, but not SGRQ, was associated with greater reductions in exacerbation risk; and 3) 2-month FEV1 and SGRQ nonresponders had fewer exacerbations if they received an ICS/LABA rather than a LABA alone. These data help set the “early response” to treatment in a wider context.
Our analysis sought to establish whether early responses to treatment have predictive ability by measuring changes in FEV1 and SGRQ total score after 2 months of treatment. It was expected that changes in these variables would be clinically noticeable after 2 months, a follow-up interval commonly used in clinical practice when assessing the impact of treatment in patients with COPD. Although somewhat arbitrary, an improvement of 100 mL in FEV1 appears to be a reasonable threshold as it exceeds the day-to-day reproducibility of this measurement in patients with COPD,18 identifies patients with a lower risk of relapse during recovery from an acute event,8 and has previously been proposed as the minimal CID between measurements.15 A change in SGRQ total score of ≥4 units has been validated as a minimal CID in health status measured in mild-to-severe COPD with this questionnaire.19 Changes of this magnitude have been observed in short- and longer-term trials of bronchodilators in COPD.1,7,10 Data from the placebo arms of our analysis show that spontaneous increases in FEV1 sufficient to exceed the 100 mL threshold were less frequent than 4-point improvements in the SGRQ total score, reflecting the multiple factors that influence health status measurement.
Patients meeting our FEV1 response criterion had better baseline lung function and took less maintenance medication at study entry than nonresponders. These data support other studies showing that acute postbronchodilator improvements in FEV1 are greater in patients with less severe disease.20,21 The chances of a response in SGRQ total score from 0 to 2 months were greater than those for FEV1 response. This was unrelated to baseline lung function but was more likely if the initial SGRQ total score was high, raising the possibility of regression to the mean in some cases.
Predicting longer-term response to treatment
Over the trial period, 80% of FEV1 nonresponders at 2 months remained in this group at 12 months, while FEV1 responders showed more variation, with only 58% of these showing a 100 mL improvement in FEV1 at 2 months still remaining responders at 12 months. In contrast, SGRQ responders were more likely to sustain their initial improvement and in addition, more patients became responders over time. Despite these encouraging findings in the whole group, it would be difficult to advise an individual patient about his or her future lung function or health status based on the change in health status at 2 months.
Predicting future exacerbation risk
The investigation of an early response to treatment as a predictor of future risk differs from previously published studies, which have investigated the predictive utility of baseline values. For example, the Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (NCT00292552) study22 showed that a wide range of baseline FEV1 and SGRQ values were predictive of exacerbation outcomes. Furthermore, a post hoc analysis by Make et al23 observed that all baseline lung function variables studied were strong predictors of severe exacerbations. Conversely, other studies have suggested that there is no relationship between airflow obstruction characteristics and exacerbation rates.24,25
Based on these contrasting observations, it is clear that additional predictors of exacerbation frequency are needed, and our data show that early response to treatment offers an alternative approach, which has predictive value in some (those patients with an early response to FEV1, ie, 35.1% of patients in our study), but not all patients. A 2-month FEV1 response of ≥100 mL for both formoterol and budesonide/formoterol identified patients less likely to exacerbate during follow-up. In general, the greater the improvement in FEV1, the lower the chance of a future exacerbation, although we cannot exclude the possibility that other factors may contribute to both an FEV1 response and a reduction in exacerbations. However, FEV1 response at 2 months was not the only predictive factor, as a between-treatment difference in exacerbation risk was still present in nonresponders. This may reflect the smaller FEV1 responses seen in patients with worse initial lung function,26 as changes in operating lung volume rather than FEV1 are important drivers of exacerbation in such patients.27 Our data extend the observations from indacaterol trials where change in trough FEV1 at 12 weeks was related to change in exacerbation risk and dyspnea score, although a specific, arbitrary threshold value was not utilized.10
Despite the baseline level of health status predicting an overall risk of exacerbation in our study, SGRQ response at 2 months was not predictive of exacerbation risk over 2–12 months. Health status is adversely affected by disease exacerbations,28 and the change in SGRQ total score at 2 months may reflect variables other than an effect of exacerbation prevention. Although reverse causality cannot be excluded, it seems more likely that an SGRQ total score responds to previous exacerbation events rather than predicting the risk of future events. Thus, while a significant association is shown for FEV1, no such link is evident for SGRQ over the score range in the current analysis.
Areas for further study
There may be other markers of an early treatment effect than those analyzed here. One example could be lung hyperinflation, which is not reflected in routine spirometry and may be used to measure therapeutic response; however, our analysis provides evidence based on responses that are more easily measured in primary care. Blood eosinophil count may also be a parameter for response to ICS in patients with COPD,29 but such data were not available for analysis.
Whether a change that exceeds our threshold values occurs at earlier time points and is a comparable or better predictor of clinical outcome also needs to be determined. Defining responses by early FEV1 response has some utility when the therapy has the potential to alter that variable, although this is not true for all interventions.26
Other considerations
This study has some limitations. Our analysis restricted the placebo comparisons to the early 2-month response analysis as missing data due to early dropouts significantly reduced data quality in the placebo arms of the relevant studies, as noted previously.1 The issue of missing data is a frequent problem in trials of COPD therapy. The absence of data in 15% of patients over a 12-month period is not unusual for analyses of this type. Loss of data due to discontinuation in clinical trials of this type is more frequent on the less effective treatment,30 which in the present analysis is formoterol.
Our data were derived from a clinical trial population, yet we believe that they have wider clinical relevance as the necessity of adding an ICS to a long-acting bronchodilator in patients with COPD, and assessing its benefit, is an important therapeutic consideration in both primary and secondary care. These data also show that a greater proportion of patients with COPD receiving budesonide/formoterol demonstrate a positive treatment response compared with those receiving formoterol alone.
Conclusion
FEV1 and SGRQ are commonly used in specialist clinics to assess patient progress. Our results, which were obtained in patients with moderate-to-very-severe COPD who had an exacerbation in the previous year, suggest that an early response at 2 months in either domain is associated with better long-term outcomes in that domain and, in the case of improvement in FEV1, a lower chance of future exacerbations. However, such changes occur in a minority of cases and therapeutic benefit can also occur in patients who do not have an “early” response to treatment. Further investigations and prospective studies are needed to identify more sensitive and specific markers of a favorable treatment response. The need to assess patients soon after treatment is changed is worth considering.
Acknowledgments
This analysis was funded by AstraZeneca. Anna Mett and Shaun Foley of inScience Communications, Springer Healthcare, provided medical writing assistance, funded by AstraZeneca. The authors thank Malin Fagerås of AstraZeneca R&D, Gothenburg, Sweden, and Thomas Similowski, of Groupe Hospitalier Pitié-Salpêtrière, Paris, France, for their assistance with the development of this manuscript. Anders Persson of AstraZeneca R&D, Gothenburg, Sweden, performed additional statistical analyses.
Disclosure
PMC is a board member for Boehringer Ingelheim, the Department of Health Respiratory Programme Board, GlaxoSmithKline, and Nycomed. He has been a consultant for Novartis and provided expert testimony for Forest. PMC has received honoraria for advising on the conduct and analysis of clinical trial data from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Novartis, and Nycomed. He has also spoken at meetings supported by these companies. Support for travel to meetings has been provided by AstraZeneca.
The University of Groningen has received honoraria for DSP advising on the conduct and analysis of clinical trial data from AstraZeneca, Nycomed, and Teva as well as for lectures at meetings supported by AstraZeneca, Chiesi, GlaxoSmithKline, Nycomed, and Teva. The University of Groningen has received money for research by unrestricted educational grants from AstraZeneca and Chiesi. AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, and Nycomed have provided support for travel to meetings.
ARA is a consultant and speaker for AstraZeneca, Bayer Pharma, Boehringer Ingelheim, Dey Pharma, GlaxoSmithKline, and Pfizer, and has received honoraria from these companies. Educational presentations have been developed for AstraZeneca, Bayer Pharma, Boehringer Ingelheim, Dey Pharma, and Pfizer. Support for travel to meetings has also been provided by AstraZeneca.
BJM is a board member for AstraZeneca, Boehringer Ingelheim, Dey Pharma, Embryon, Forest, Johnson and Johnson, MedImmune, Novartis, Nycomed, Pfizer, and Respironics, and a consultant for Astellas and Chiesi. Clinical trial data have been reviewed for Spiration, with grants currently pending with AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, MedImmune, Nabi, Pfizer, and Sunovian. Lectures have been presented on behalf of Boehringer Ingelheim, GlaxoSmithKline, and Pfizer, with video presentations developed for Boehringer Ingelheim and questionnaires produced for Union Chimique Belge. Educational presentations and programs have been developed (Circulate WebMD, Creative Educational Concepts, France Foundation, Johns Hopkins University, Medscape, National Jewish Health, and the Veteran’s Health Administration [VHA]), and BJM has been a speaker for educational programs at Abbott, the American Academy of Family Practice, the American College of Chest Physicians, the American Thoracic Society, Breathe LA, the Cleveland Clinic, and VHA. Support for travel to meetings has also been provided by AstraZeneca.
GE and SP are former employees of AstraZeneca and own stocks within the company.
CRJ is a board member for AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Merck Limited, and Novartis, and a consultant for Chiesi and AstraZeneca. Educational presentations have been developed for AstraZeneca and GlaxoSmithKline, with grants also pending for these companies. Lectures have been presented on behalf of AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Hunter Immunology, and Novartis. Support for travel to meetings has been provided by AstraZeneca. The authors report no other conflicts of interest in this work.
References
Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775–789. | ||
Calverley PM, Boonsawat W, Cseke Z, Zhong N, Peterson S, Olsson H. Maintenance therapy with budesonide and formoterol in chronic obstructive pulmonary disease. Eur Respir J. 2003;22(6):912–919. | ||
Tashkin DP, Rennard SI, Martin P, et al. Efficacy and safety of budesonide and formoterol in one pressurized metered-dose inhaler in patients with moderate to very severe chronic obstructive pulmonary disease: results of a 6-month randomized clinical trial. Drugs. 2008;68(14):1975–2000. | ||
Aliverti A, Rodger K, Dellaca RL, et al. Effect of salbutamol on lung function and chest wall volumes at rest and during exercise in COPD. Thorax. 2005;60(11):916–924. | ||
O’Donnell D, Lam M, Webb KA. Spirometric correlates of improvement in exercise performance after anticholinergic therapy in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;160(2):542–549. | ||
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease [online]. 2011; Available from: http://www.goldcopd.org/. Accessed September 25, 2012. | ||
Jones PW, Bosh TK. Quality of life changes in COPD patients treated with salmeterol. Am J Respir Crit Care Med. 1997;155(4):1283–1289. | ||
Niewoehner DE, Collins D, Erbland ML. Relation of FEV(1) to clinical outcomes during exacerbations of chronic obstructive pulmonary disease. Department of Veterans Affairs Cooperative Study Group. Am J Respir Crit Care Med. 2000;161(4 Pt 1):1201–1205. | ||
Vestbo J, Pauwels R, Anderson JA, Jones P, Calverley P. Early onset of effect of salmeterol and fluticasone propionate in chronic obstructive pulmonary disease. Thorax. 2005;60(4):301–304. | ||
Jones P, Donohue J, Nedelman J, Pascoe S, Pinault G, Lassen C. Correlating changes in lung function with patient outcomes in chronic obstructive pulmonary disease: a pooled analysis. Respir Res. 2011;12:161. | ||
Rennard SI, Tashkin DP, McElhattan J, et al. Efficacy and tolerability of budesonide/formoterol in one hydrofluoroalkane pressurized metered-dose inhaler in patients with chronic obstructive pulmonary disease: results from a 1-year randomized controlled clinical trial. Drugs. 2009;69(5):549–565. | ||
Sharafkhaneh A, Southard JG, Goldman M, Uryniak T, Martin UJ. Effect of budesonide/formoterol pMDI on COPD exacerbations: a double-blind, randomized study. Respir Med. 2012;106(2):257–268. | ||
Standardization of spirometry, 1994 update. American Thoracic Society. Am J Respir Crit Care Med. 1995;152(3):1107–1136. | ||
Cazzola M, MacNee W, Martinez FJ, et al. Outcomes for COPD pharmacological trials: from lung function to biomarkers. Eur Respir J. 2008;31(2):416–469. | ||
Donohue JF. Minimal clinically important differences in COPD lung function. COPD. 2005;2(1):111–124. | ||
Jones PW. Interpreting thresholds for a clinically significant change in health status in asthma and COPD. Eur Respir J. 2002;19(3):398–404. | ||
Calverley PM, Spencer S, Willits L, Burge PS, Jones PW, Group IOSLDE. Withdrawal from treatment as an outcome in the ISOLDE study of COPD. Chest. 2003;124(4):1350–1356. | ||
Calverley PM, Albert P, Walker PP. Bronchodilator reversibility in chronic obstructive pulmonary disease: use and limitations. Lancet Respir Med. 2013;1(7):564–573. | ||
Jones PW. St George’s respiratory questionnaire: MCID. COPD. 2005;2(1):75–79. | ||
Jenkins CR, Jones PW, Calverley PM, et al. Efficacy of salmeterol/fluticasone propionate by GOLD stage of chronic obstructive pulmonary disease: analysis from the randomised, placebo-controlled TORCH study. Respir Res. 2009;10:59. | ||
Decramer M, Celli B, Kesten S, Lystig T, Mehra S, Tashkin DP. Effect of tiotropium on outcomes in patients with moderate chronic obstructive pulmonary disease (UPLIFT): a prespecified subgroup analysis of a randomised controlled trial. Lancet. 2009;374(9696):1171–1178. | ||
Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. New Engl J Med. 2010;363(12):1128–1138. | ||
Make BJ, Eriksson G, Calverley PM, et al. A score to predict short-term risk of COPD exacerbations (SCOPEX). Int J COPD. 2015;10:201–209. | ||
Wan ES, DeMeo DL, Hersh CP, et al. Clinical predictors of frequent exacerbations in subjects with severe chronic obstructive pulmonary disease (COPD). Respir Med. 2011;105(4):588–594. | ||
Al-ani S, Spigt M, Hofset P, Melbye H. Predictors of exacerbations of asthma and COPD during one year in primary care. Family Pract. 2013;30(6):621–628. | ||
Albert P, Agusti A, Edwards L, et al. Bronchodilator responsiveness as a phenotypic characteristic of established chronic obstructive pulmonary disease. Thorax. 2012;67(8):701–708. | ||
Stevenson NJ, Walker PP, Costello RW, Calverley PM. Lung mechanics and dyspnea during exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;172(12):1510–1516. | ||
Spencer S, Calverley PM, Burge PS, Jones PW. Impact of preventing exacerbations on deterioration of health status in COPD. Eur Respir J. 2004;23(5):698–702. | ||
Pascoe S, Locantore N, Dransfield MT, Barnes NC, Pavord ID. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomised controlled trials. Lancet Respir Med. 2015;3(6):435–442. | ||
Kesten S, Plautz M, Piquette CA, Habib MP, Niewoehner DE. Premature discontinuation of patients: a potential bias in COPD clinical trials. Eur Respir J. 2007;30(5):898–906. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.