Back to Journals » International Journal of General Medicine » Volume 15
Early Prediction Model of Acute Aortic Syndrome Mortality in Emergency Departments
Authors Wang D, Zhang H , Du L, Zhai Q, Hu G, Gao W, Zhang A, Wang S, Hao Y, Shang K, Liu X, Gao Y, Muyesai N, Ma Q
Received 11 January 2022
Accepted for publication 23 March 2022
Published 6 April 2022 Volume 2022:15 Pages 3779—3788
DOI https://doi.org/10.2147/IJGM.S357910
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Daidai Wang,1,* Hua Zhang,2,* Lanfang Du,1,* Qiangrong Zhai,1 Guangliang Hu,1 Wei Gao,1 Anyi Zhang,1 Sa Wang,1 Yajuan Hao,1 Kaijian Shang,1,3 Xueqing Liu,1 Yanxia Gao,4 Nijiati Muyesai,5 Qingbian Ma1
1Department of Emergency Medicine, Peking University Third Hospital, Beijing, People’s Republic of China; 2Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing, People’s Republic of China; 3Department of Emergency Medicine, Second hospital of Shanxi Medical University, Shanxi, People’s Republic of China; 4Department of Emergency Medicine, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, People’s Republic of China; 5Department of Emergency Medicine, Xinjiang Ulger Municipal People’s Hospital, Urumqi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qingbian Ma; Nijiati Muyesai, Tel +86 15611908229, Email [email protected]; [email protected]
Purpose: Acute aortic syndrome is a constellation of life-threatening medical conditions for which rapid assessment and targeted intervention are important for the prognosis of patients who are at high risk of in-hospital death. The current study aims to develop and externally validate an early prediction mortality model that can be used to identify high-risk patients with acute aortic syndrome in the emergency department.
Patients and Methods: This retrospective multi-center observational study enrolled 1088 patients with acute aortic syndrome admitted to the emergency departments of two hospitals in China between January 2017 and March 2021 for model development. A total of 210 patients with acute aortic syndrome admitted to the emergency departments of Peking University Third Hospital between January 2007 and December 2021 was enrolled for model validation. Demographics and clinical factors were collected at the time of emergency department admission. The predictive variables were determined by referring to the results of previous studies and the baseline analysis of this study. The study’s endpoint was in-hospital death. To assess internal validity, we used a fivefold cross-validation method. Model performance was validated internally and externally by evaluating model discrimination using the area under the receiver-operating characteristic curve (AUC). A nomogram was developed based on the binary regression results.
Results: In the development cohort, 1088 patients with acute aortic syndromes were included, and 88 (8.1%) patients died during hospitalization. In the validation cohort, 210 patients were included, and 20 (9.5%) patients died during hospitalization. The final model included the following variables: digestive system symptoms (OR=2.25; P=0.024), any pulse deficit (OR=7.78; P< 0.001), creatinine (μmol/L)(OR=1.00; P=0.018), lesion extension to iliac vessels (OR=4.49; P< 0.001), pericardial effusion (OR=2.67; P=0.008), and Stanford type A (OR=10.46; P< 0.001). The model’s AUC was 0.838 (95% CI 0.784– 0.892) in the development cohort and 0.821 (95% CI 0.750– 0.891) in the validation cohort, and the Hosmer–Lemeshow test showed p=0.597. The fivefold cross-validation demonstrated a mean accuracy of 0.94, a mean precision of 0.67, and a mean recall of 0.13.
Conclusion: This risk prediction tool uses simple variables to provide robust prediction of the risk of in-hospital death from acute aortic syndrome and validated well in an independent cohort. The tool can help emergency clinicians quickly identify high-risk acute aortic syndrome patients, although further studies are needed for verifying the prospective data and the results of our study.
Keywords: acute aortic syndrome, risk prediction model, emergency department
Introduction
Acute aortic syndrome (AAS) is a constellation of life-threatening medical conditions, including classic acute aortic dissection (AAD), intramural hematoma (IMH), penetrating atherosclerotic aortic ulcer (PAU), and even thoracic aortic rupture. They share common pathophysiological pathways, specifically the breakdown of the intima and media, common clinical characteristics, and present diagnostic and therapeutic challenges.1–3 Emergency physicians need a simple and accessible tool to identify patients suffering from AAS who are at high risk of in-hospital mortality, thereby helping them make medical decisions and allocate resources for high-risk patients as soon as possible.4 Making use of such a tool would also help patients’ families understand the severity of the disease so they can make quicker and better decisions for their family member.
Several AAS prediction models have already been developed and published,5–8 but most of them cannot be easily applied by emergency physicians. First, most studies have evaluated the variables of AAD only, rather than the other AAS conditions.6,9 However, acute aortic dissection and intramural hematoma share similar clinical features and complications.10,11 Also, the recognition in recent years that intramural haematoma, or bleeding into the aortic wall, is related to aortic dissection has demonstrated that both conditions can coexist and may constitute a spectrum.10,12 Thus, it is necessary to develop a risk stratification model for AAS. Second, a large proportion of existing models are based on surgery, which is less useful in the emergency department (ED).9,13 Third, some of the identified predictors need a manual assessment process, such as false lumen/true lumen of ascending aorta ≥0.75,4 which can be too time consuming for emergency physicians. Our objective was to develop and validate a practical risk stratification approach that could be used to identify AAS patients’ in-hospital mortality in the emergency department.
Methods
Patient Selection
This study uses two datasets: a development and a validation set. The development dataset was derived from The First Affiliated Hospital of Zhengzhou University and Xinjiang Ulger Municipal People’s Hospital. The validation database was derived from Peking University Third Hospital. This retrospective cohort study enrolled patients diagnosed with AAS who admitted to the emergency departments of The First Affiliated Hospital of Zhengzhou University and Xinjiang Ulger Municipal People’s Hospital between January 2017 and March 2021 for model development. Patients with AAS admitted to the emergency departments of Peking University Third Hospital between January 2007 and December 2021 were enrolled for model validation. Inclusion criteria for both cohorts were patients who were diagnosed with AAD, IMH, or PAU by computed tomography angiography and/or transthoracic echocardiography. Exclusion criteria were: 1) >14 days from onset of symptoms, 2) patient under 18 years old, 3) presence of traumatic or iatrogenic acute aortic syndrome, 4) acute aortic syndrome in pregnancy, 5) missing data relevant to the analysis.
Data Collection Measures
The research team worked with senior clinicians and statisticians to design our comprehensive registry, which consists of five parts: demographic characteristics, medical history, laboratory examinations, imaging studies, and in-hospital outcome. The registry was designed and implemented on the Research Electronic Data Capture (REDCap) v 11.1.0 platform, which provides an intuitive interface for validated data entry and audit trails to track the history of data entry and revision.14
Data were collected by ED staff from electronic medical records and was entered into the REDcap by research staff. All of them have undergone unified training to ensure consistency in the data entry process. Each research center has a research director who check the entered data regularly. The entered data included the patient demographics (including age, gender and diagnosis); medical history (including etiology and history); clinical presentation; physical findings; laboratory examinations and imaging studies that were collected at the time of ED admission. The endpoint event was in-hospital death. The follow-up was carried out at discharge. Acute aortic dissection is defined as a separation of the layers of the aortic wall due to an intimal tear; IMH is defined as a hematoma confined within the medial layer of the aorta in the absence of a detectable intimal tear; PAU is defined as a contained aortic rupture due to slow oozing from the damaged aorta at or near the site of aortic lesion; In-hospital mortality was defined as death occurring before hospital discharge.
Statistical Analysis
Study data were managed as well as collected using REDCap electronic data capture tools hosted at the National Institute of Health Data Science of Peking University. Patients included in the study were divided into the survivor group and the non-survivor group. Data were described using mean ± standard deviation or median (25th–75th percentiles) for continuous variables; frequencies and proportions were used for categorical variables. Denominators represent only fully reported cases; cases with missing data were not included. The student’s t-test was used to compare normally distributed continuous variables, while the Mann–Whitney U-test was used for non-normally distributed continuous variables. Categorical variables were analyzed using by a χ2 test and Fisher exact test, when appropriate.
Binary logistic regression analysis was used to build an early prediction model. In-hospital death was taken as the dependent variable, and the predictive variables were determined by referring to the results of previous studies and the baseline analysis of this study. When an independent variable was a categorical variable, the minimum value group was taken as the reference group. When an independent variable was a continuous variable, it was directly included into the binary logistic regression model. The fivefold cross-validation method was used to calculate and verify its accuracy, precision, recall, and F-measure. Model performance was validated internally and externally by evaluating model discrimination using the area under the receiver-operating characteristic curve (AUC). To facilitate the application of the model, we drew a nomogram according to the coefficients of the regression model. A p-value<0.05 was considered statistically significant. Data analysis was performed with the use of IBM SPSS statistics software (v25, IBM, New York, USA) and R software (v4.0.3, Vienna, Austria).
Ethical Approval
The study conformed to the Declaration of Helsinki. This study was a multi-center cohort study and the leading research center of this study was Peking University Third Hospital. The study was approved by the institutional review board of Peking University Third Hospital and all participating hospitals (M2020410, Peking University Third Hospital Medical Science Research Ethics Committee). The informed consent requirement was waived for the following reasons: a. This study was a retrospective analysis of medical records, involving no potential risk. b. All Data was anonymous.
Results
Patient Characteristics
A total of 1088 patients with acute aortic syndromes were included in the development cohort. Among them, 88 (8.1%) patients died during hospitalization. About 62.9% of patients were Stanford type A. Most of them were middle-aged men, with a male predominance of 77.2%. For the validation cohort, 210 patients were included. Among them, 20 (9.5%) patients died during hospitalization. About 41.4% of patients were Stanford type A. Most of them were middle-aged men, with a male predominance of 79.0%. Patients’ characteristics of both cohorts are shown in Table 1.
 |
Table 1 Baseline Clinical Characteristics of All Patients with AAS |
Univariate Predictors of in-Hospital Death for Patients with AAS in Emergency Departments
In the development cohort, clinical characteristics that showed significant association with in-hospital mortality included chest pain, abdominal pain, palpitation, sweating, dyspnea, digestive system symptoms, central nervous system symptoms, limb involved symptoms, mean systolic blood pressure, mean diastolic blood pressure, and any pulse deficit. Patients whose laboratory examinations showed higher levels of white blood cell count, neutrophil count, total bilirubin, creatinine, prothrombin time (PT), activated partial thromboplastin time (APTT), international normalized ratio (INR), and D-dimer were additionally associated with higher in-hospital mortality. Also, some CT angiography signs differ significantly between survivors and non-survivors, including brachiocephalic trunk involvement, lesion extension to iliac vessels, abdominal organ involvement (any degree), and pericardial effusion (Table 1). In the Peking University Third hospital validation cohort, clinical characteristics that showed significant association with in-hospital mortality included digestive system symptoms, central nervous system symptoms, mean systolic blood pressure. Patients whose laboratory examinations showed higher levels of white blood cell count, neutrophil count, prothrombin time (PT), international normalized ratio (INR), and D-dimer were additionally associated with higher in-hospital mortality. Also, some CT angiography signs differ significantly between survivors and non-survivors, including brachiocephalic trunk involvement, abdominal organ involvement (any degree), and pericardial effusion (Table 1).
Multivariate Predictors for in-Hospital Death in Patients with AAS in Emergency Departments
In the multivariable analysis, the following variables, when present at admission, were shown to be independently associated with increased in-hospital mortality: digestive system symptoms (OR=2.25; P=0.024), any pulse deficit (OR=7.78; P<0.001), creatinine (µmol/L)(OR=1.00; P=0.018), lesion extension to iliac vessels (OR=4.49; P<0.001), pericardial effusion (OR=2.67; P=0.008), and Stanford type A (OR=10.46; P<0.001) (Table 2). The AUC (C-index) was 0.838 (95% CI 0.784–0.892) using these multivariate predictors (Figure 1A). The Hosmer-Lemeshow results indicated a significant level of goodness of fit for the logistic regression model (χ2 =6.45, p=0.597) (Figure 1B). We conducted a fivefold cross-validation, which demonstrated a mean accuracy of 0.94, a mean precision of 0.67, and a mean recall of 0.13.
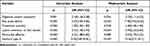 |
Table 2 Multivariate Logistic Regression of Predictive Variables with In-Hospital Death |
 |
Figure 1 (A) ROC of the model: the AUC (C index) was 0.838 (95% range 0.784–0.892). (B) Calibration curves for the prediction model. |
Validation of Predictive Model for in-Hospital Mortality in Patients with AAS
External validation resulted in an AUC of 0.821 (95% CI 0.750–0.891). The external validation indicates a good discriminative capacity of the model (Figure 2).
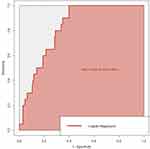 |
Figure 2 ROC of the model in validation cohort: the AUC (C index) was 0.821 (95% range 0.750–0.891). |
Nomogram for Bedside Application
Based on these multivariable regression results, a nomogram for bedside application was established (Figure 3).
Discussion
Developed on the basis of routinely collected and easily available clinical information, our model was demonstrated to be an effective tool for the early prediction of the in-hospital mortality rate of AAS in its initial phase after ED arrival. Digestive system symptoms, any pulse deficit, creatinine, lesion extension to iliac vessels, pericardial effusion, and Stanford type A accurately and pragmatically predicted the risk of in-hospital death. The AUC of 0.838 and showed the model had overall good discrimination in identifying patients at risk. Also, it validated well in an independent cohort.
Compared with previous models, our binary logistic regression model has several strengths. First, our predictor variables can be acquired quickly and effectively at the time of ED admission, making it feasible for early identification of patients at high risk of in-hospital death in the ED. Also, the model has only six variables, and they do not require mathematical manipulation, making it easy for emergency clinicians to use. Some studies have proposed prediction models that have also shown strong discrimination, but they have used more variables, which makes the models less efficient.15,16 Second, our study has a large sample size, with 1088 patients involved, larger, as far as we can determine, than most other studies. Recently, a systematic review of prediction models for acute aortic dissection concluded that the sample size varied from 35 to 1034 (median 165, IQR,103–348).17 Tolenaar et al used multinational data from the International Registry of Acute Aortic Dissection (IRAD) that involved 1034 patients, but their aim was to investigate predictors of mortality among patients presenting with acute type B aortic dissection.6 Czerny et al developed the German Registry of Acute Aortic Dissection Type A (GERAADA) score with 2537 patients involved, but the endpoint of their study was the 30-day mortality rate, and the patients who were diagnosed all underwent surgery, which is not suitable to use in ED.9 Third, our study focuses exclusively on unselected consecutive patients admitted to the emergency department, whereas the currently existing models target patients already admitted to various wards, such as cardiac surgery.9,15 Patients admitted to the ED may die before they are admitted to specific wards, or they may refuse to be admitted to those wards, or they may be transferred to other hospitals. Consequently, the group of patients admitted to emergency departments is more heterogeneous, making it more challenging for the model to achieve accurate predictions based on particular wards. For these reasons, our study can be generalized to all patients with AAS presenting at the emergency department regardless of their clinical status or treatment strategy.
The model’s six variables are digestive system symptoms, any pulse deficit, creatinine (µmol/L), lesion extension to iliac vessels, pericardial effusion, and Stanford type A. It is not surprising that Stanford type A is associated with worse outcomes, which had been demonstrated by many previous studies.18,19 Pericardial effusion has also been shown to be a predictive variable in previous studies.20 According to some studies, pericardial effusion may result from rupture of the thoracic aorta into the pericardial cavity or from the transudation of fluid into the pericardial cavity through the intact wall of the false lumen.21,22 Several studies have shown that the presence of any pericardial effusion is an ominous sign.22,23
More importantly, our study shows that digestive system symptoms, any pulse deficit, lesion extension to iliac vessels, and creatinine confer an even higher mortality rate. These findings may have therapeutic implications, as these four predictors are associated with malperfusion syndrome (MPS). Several studies have shown that AAS patients with MPS have poorer clinical outcomes.24–26 MPS can affect any vascular bed, with mesenteric malperfusion being the most challenging, as it is associated with a three to fourfold increase in mortality in both acute type A and B aortic dissections.27 Ischemic damage of malperfused organs should be minimized by restoring perfusion as early as possible in order to improve surgical outcomes.24 The presence of these predictors in our model can help emergency physicians with early identification of potential MPS, which may help improve prognosis of these patients. If patients have these clinical manifestations on presentation, physicians need to attempt to find whether and which vessels may have been affected, such as mesenteric, renal, or limb. Identifying these vessels will help physicians find potential MPS quickly and relieve organ ischemia in a timely fashion, either through surgery or by percutaneous techniques. With the development of technique in medical diagnosis, we can add some novel variable, such as the change in blood hemodynamics which can be detected in CTA using the technique of computational fluid dynamic technique, in our model to identify patients with MPS in the future.28,29 This study additionally established a nomogram for bedside application, which has implications for the education of the patient’s family and for clinical practices. As the nomogram can be readily understood, patients with acute aortic syndromes and their relatives can obtain reliable information without needing to depend on their physician’s descriptions of the prognosis of this acutely devastating condition, thereby helping them to realize the severity of the disease quickly and participate effectively in shared decision making. Making appropriate decisions quickly can help emergency physicians manage the disease effectively, such as consulting with the surgeon as soon as possible; surgery must be started quickly, as it may be critical for improving the outcome of patients suffering from type A acute aortic syndrome.30,31
Limitations
This study has several limitations. First, the design is a two-center retrospective study and therefore subject to selection bias, information bias, and other confounders. Second, the model was externally validated only in one independent hospital, and the model needs to be validated in more independent population, so additional studies are needed to evaluate our predictive model and risk assessment tool.
Conclusions
In our study, the risk factors for preoperative mortality were analyzed in patients with acute aortic syndromes who visited emergency departments, and a simple and effective risk assessment method was established to help emergency clinicians quickly identify high-risk patients and make appropriate medical decisions.
Acknowledgments
We would like to acknowledge the reviewers for their invaluable comments on this study. Daidai Wang, Hua Zhang, and Lanfang Du are co-first authors for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bossone E, LaBounty TM, Eagle KA. Acute aortic syndromes: diagnosis and management, an update. Eur Heart J. 2018;39(9):739–749d. doi:10.1093/eurheartj/ehx319
2. Morello F, Santoro M, Fargion AT, Grifoni S, Nazerian P. Diagnosis and management of acute aortic syndromes in the emergency department. Intern Emerg Med. 2021;16(1):171–181. doi:10.1007/s11739-020-02354-8
3. Bossone E, Czerny M, Lerakis S, et al. Imaging and biomarkers in acute aortic syndromes: diagnostic and prognostic implications. Curr Probl Cardiol. 2021;46(3):100654. doi:10.1016/j.cpcardiol.2020.100654
4. Kuang J, Yang J, Wang Q, et al. A preoperative mortality risk assessment model for Stanford type A acute aortic dissection. BMC Cardiovasc Disord. 2020;20(1):508. doi:10.1186/s12872-020-01802-9
5. Feng WZ, Zhou JQ, Yu GM, Zeng Y, Xu P. Association of serum cystatin C levels with mortality in patients with acute type A aortic dissection. Oncotarget. 2017;8(60):101103–101111. doi:10.18632/oncotarget.20593
6. Tolenaar JL, Froehlich W, Jonker FHW, et al. Predicting in-hospital mortality in acute type B aortic dissection: evidence from International Registry of Acute Aortic Dissection. Circulation. 2014;130:S45–S50. doi:10.1161/CIRCULATIONAHA.113.007117
7. Mehta RH, Suzuki T, Hagan PG, et al. Predicting death in patients with acute type a aortic dissection. Circulation. 2002;105(2):200–206. doi:10.1161/hc0202.102246
8. Zhang J, Cheng B, Yang M, et al. Predicting in-hospital death in patients with type B acute aortic dissection. Medicine. 2019;98(32):e16462. doi:10.1097/MD.0000000000016462
9. Czerny M, Siepe M, Beyersdorf F, et al. Prediction of mortality rate in acute type A dissection: the German registry for acute type A aortic dissection score. Eur J Cardiothorac Surg. 2020;58(4):700–706. doi:10.1093/ejcts/ezaa156
10. Mussa FF, Horton JD, Moridzadeh R, et al. Acute aortic dissection and intramural hematoma: a systematic review. JAMA. 2016;316(7):754–763. doi:10.1001/jama.2016.10026
11. Nienaber CA, Powell JT. Management of acute aortic syndromes. Eur Heart J. 2012;33(1):26b–35b. doi:10.1093/eurheartj/ehr186
12. Nienaber CA, Clough RE, Sakalihasan N, et al. Aortic dissection. Nat Rev Dis Primers. 2016;2(1):16053. doi:10.1038/nrdp.2016.53
13. Ong CS, Nam L, Yesantharao P, et al. The strongest risk factor for operative mortality in acute type A aortic dissection is acidosis: validation of risk model. Semin Thorac Cardiovasc Surg. 2020;32(4):674–680. doi:10.1053/j.semtcvs.2020.02.023
14. Pang X, Kozlowski N, Wu S, et al. Construction and management of ARDS/sepsis registry with REDCap. J Thorac Dis. 2014;6(9):1293–1299. doi:10.3978/j.issn.2072-1439.2014.09.07
15. Rampoldi V, Trimarchi S, Eagle KA, et al. Simple risk models to predict surgical mortality in acute type A aortic dissection: the International Registry of Acute Aortic Dissection score. Ann Thorac Surg. 2007;83(1):55–61. doi:10.1016/j.athoracsur.2006.08.007
16. Macrina F, Puddu PE, Sciangula A, et al. Artificial neural networks versus multiple logistic regression to predict 30-day mortality after operations for type A ascending aortic dissection. Open Cardiovasc Med J. 2009;3(1):81–95. doi:10.2174/1874192400903010081
17. Ren Y, Huang S, Li Q, et al. Prognostic factors and prediction models for acute aortic dissection: a systematic review. BMJ Open. 2021;11(2):e042435. doi:10.1136/bmjopen-2020-042435
18. Zhang J, Jiang Y, Gao C, Feng J, Wang A. Risk factors for hospital death in patients with acute aortic dissection. Heart Lung Circ. 2015;24(4):348–353. doi:10.1016/j.hlc.2014.10.009
19. Pape LA, Awais M, Woznicki EM, et al. Presentation, diagnosis, and outcomes of acute aortic dissection: 17-year trends from the International Registry of Acute Aortic Dissection. J Am Coll Cardiol. 2015;66(4):350–358. doi:10.1016/j.jacc.2015.05.029
20. Lingzhi C, Hao Z, Weijian H, et al. Outcome predictors in patients presenting with acute aortic dissection. J Cardiothorac Vasc Anesth. 2016;30(5):1272–1277. doi:10.1053/j.jvca.2016.03.149
21. Castaner E, Andreu M, Gallardo X, et al. CT in nontraumatic acute thoracic aortic disease: typical and atypical features and complications. Radiographics. 2003;23(suppl_1):S93–S110. doi:10.1148/rg.23si035507
22. Khan IA, Nair CK. Clinical, diagnostic, and management perspectives of aortic dissection. Chest. 2002;122(1):311–328. doi:10.1378/chest.122.1.311
23. Evangelista A, Maldonado G, Gruosso D, et al. The current role of echocardiography in acute aortic syndrome. Echo Res Pract. 2019;6(2):R53–R63. doi:10.1530/ERP-18-0058
24. Shimamoto T, Komiya T. Clinical dilemma in the surgical treatment of organ malperfusion caused by acute type A aortic dissection. Gen Thorac Cardiovasc Surg. 2014;62(7):398–406. doi:10.1007/s11748-014-0406-x
25. Berretta P, Trimarchi S, Patel HJ, et al. Malperfusion syndromes in type A aortic dissection: what we have learned from IRAD. J Vis Surg. 2018;4:65. doi:10.21037/jovs.2018.03.13
26. Yang B, Norton EL, Rosati CM, et al. Managing patients with acute type A aortic dissection and mesenteric malperfusion syndrome: a 20-year experience. J Thorac Cardiovasc Surg. 2019;158(3):675–687. doi:10.1016/j.jtcvs.2018.11.127
27. Velayudhan BV, Idhrees AM, Mukesh K, Kannan RN. Mesenteric malperfusion in acute aortic dissection: challenges and frontiers. Semin Thorac Cardiovasc Surg. 2019;31(4):668–673. doi:10.1053/j.semtcvs.2019.03.012
28. Polanczyk A, Piechota-Polanczyk A, Domenig C, et al. Computational fluid dynamic accuracy in mimicking changes in blood hemodynamics in patients with acute type IIIb aortic dissection treated with TEVAR. Appl Sci. 2018;8(8):1309. doi:10.3390/app8081309
29. Polanczyk A, Piechota-Polanczyk A, Huk I, et al. Computational fluid dynamic technique for assessment of how changing character of blood flow and different value of hct influence blood hemodynamic in dissected aorta. Diagnostics. 2021;11(10):1866. doi:10.3390/diagnostics11101866
30. Jaja BNR, Saposnik G, Lingsma HF, et al. Development and validation of outcome prediction models for aneurysmal subarachnoid haemorrhage: the SAHIT multinational cohort study. BMJ. 2018;360:j5745. doi:10.1136/bmj.j5745
31. Carroll BJ, Schermerhorn ML, Manning WJ. Imaging for acute aortic syndromes. Heart. 2020;106(3):182–189. doi:10.1136/heartjnl-2019-314897
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

