Back to Journals » Risk Management and Healthcare Policy » Volume 16
Early Diastolic Peak Velocity of Mitral Valve Annulus and Right Ventricular Systolic Tricuspid Annular Velocity as Predictors in Assessing Prognosis of Patients with Sepsis
Authors Lu NF, Shao J, Niu HX, Han WY, Chen YL, Liu AQ, Liu HN, Xi XM
Received 9 February 2023
Accepted for publication 28 April 2023
Published 17 May 2023 Volume 2023:16 Pages 921—930
DOI https://doi.org/10.2147/RMHP.S407929
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mecit Can Emre Simsekler
Nian-Fang Lu,1 Jun Shao,2 Hong-Xia Niu,3 Wen-Yong Han,4 Ya-Lei Chen,1 An-Qi Liu,1 Hu-Nan Liu,1 Xiu-Ming Xi5
1Department of Critical Care Medicine, Capital Medical University Electric Teaching Hospital/Beijing Electric Power Hospital, Beijing, 100073, People’s Republic of China; 2Department of Critical Care Medicine, Subei People’s Hospital of Jiangsu Province, Yangzhou, Jiangsu, 225001, People’s Republic of China; 3Department of Emergency, Capital medical university electric teaching hospital/Beijing Electric Power Hospital, Beijing, 100073, People’s Republic of China; 4Department of Anesthesiology, Capital Medical University Electric Teaching Hospital/Beijing Electric Power Hospital, Beijing, 100073, People’s Republic of China; 5Department of Critical Care Medicine, Capital Medical University Fuxing Hospital, Beijing, People’s Republic of China
Correspondence: Xiu-Ming Xi, Department of Critical Care Medicine, Capital Medical University Fuxing Hospital, A 20, Fuxingmenwai Street, Xicheng District, Beijing, People’s Republic of China, Tel +86 010 13801244610, Email [email protected]
Objective: To analyze the epidemiological data of patients with septic cardiomyopathy and investigate the relationship between ultrasonic parameters and prognosis of patients with sepsis.
Methods: In this study, we enrolled patients with sepsis who were treated at the Department of Critical Care Medicine in the Beijing Electric Power Hospital (No.1 Taipingqiao Xili, Fengtai District, Beijing) from January 2020 to June 2022. All patients received standardized treatment. Their general medical status and 28-day prognosis were recorded. Transthoracic echocardiography was performed within 24 hours after admission. We compared the ultrasound indexes between the mortality group and the survival group at the end of 28 days. We included parameters with significant difference in the logistic regression model to identify the independent risk factors for prognosis and evaluated their predictive value using receiver operating characteristic (ROC) curve.
Results: We included 100 patients with sepsis in this study; the mortality rate was 33% and the prevalence rate of septic cardiomyopathy was 49%. The peak e’ velocity and right ventricular systolic tricuspid annulus velocity (RV-Sm) of the survival group were significantly higher than those of the mortality group (P < 0.05). Results of logistic regression analysis showed that the peak e’ velocity and RV-Sm were independent risk factors for prognosis. The area under curve of the peak e’ velocity and the RV-Sm was 0.657 and 0.668, respectively (P < 0.05).
Conclusion: The prevalence rate of septic cardiomyopathy in septic patients is high. In this study, we found that the peak e’ velocity and right ventricular systolic tricuspid annulus velocity were important predictors of short-term prognosis.
Keywords: peak e’ velocity by tissue Doppler imaging, prognosis, right ventricular systolic tricuspid annulus velocity, septic cardiomyopathy
Introduction
Sepsis is a life-threatening organ dysfunction caused by an uncontrolled systemic inflammatory response that is induced by infection.1 Previous studies have shown that about 50% of patients with sepsis develop septic cardiomyopathy of varying degrees, and once septic cardiomyopathy occurs, the mortality rate can be as high as 70%–90%.2,3
Echocardiography is the most common non-invasive technique used to evaluate cardiac function. Tissue Doppler ultrasound is not greatly affected by the pre- and post-cardiac load and is relatively accurate. It can be used to objectively and quantitatively evaluate cardiac function and coordination, and has become the gold standard for evaluating septic cardiomyopathy.4
In clinic, the forward flow spectrum of mitral valve during diastolic period obtained by pulsed Doppler ultrasound is the most commonly used method to judge left ventricular diastolic function. However, the spectrum of mitral valve flow is often affected by many factors, such as age, mitral valve pressure gradient, left atrial size, anteroposterior cardiac load and left ventricular systolic function. Especially in the case of “pseudo normalization”, the judgment of left ventricular diastolic function needs to be combined with other ultrasound indicators.
There are some limitations of the application of mitral flow spectrum in judging left ventricular diastolic function. Different with the mitral flow spectrum, the principle of tissue Doppler technology is to measure the regional myocardial motion velocity, and its measurement value is not affected by left atrial or left ventricular filling pressure. What is more, the early diastolic mitral annular velocity is directly related to the elastic contraction of ventricular muscle. So, the tissue Doppler technology can assess left ventricular diastolic function well. At present, the early diastolic mitral annular velocity (e’) or E/ e’(E: the early diastolic mitral annular flow velocity) measured by tissue Doppler technology is one of the main indicators to evaluate left ventricular diastolic function.
For a long time, left heart function was the focus of heart function, while the understanding of right heart function was clearly lagging. In recent years, as the importance of right heart function is increasingly being recognized, the emergence of more clinical indicators has contributed to significant progress in the research of right heart function. The right heart is a key link in the hemodynamic management of critically ill patients. Increased pulmonary vascular resistance caused by different reasons in critically ill patients can affect right heart function. Also, the right heart function has an extremely important role in the diagnosis, differential diagnosis, treatment, and prognosis of critically ill patients, which has attracted extensive clinical attention.
At present, the most advanced index for the evaluation of right ventricular systolic function is the peak systolic tricuspid annulus velocity (Sm). Currently, there are differences in the international standards pertaining to the right ventricular systolic tricuspid annulus velocity (RV-Sm) for evaluating right ventricular systolic dysfunction. Some studies have suggested that the sensitivity and specificity of RV-Sm <11.5 cm/s for predicting right ventricular ejection fraction <50% should be 90% and 85%, respectively.5 Other scholars have argued that Sm <10 cm/s indicated abnormal right ventricular systolic function, which had a good correlation with RVEF measured by MRI.6,7 Some studies also used RV-Sm <15 cm/s as the standard for right ventricular systolic dysfunction.8
The tissue Doppler ultrasound is commonly used internationally for the evaluation of left ventricular systolic dysfunction. The criterion used to assess left ventricular systolic dysfunction is the maximum left ventricular systolic mitral annulus velocity (LV-Sm) <8 cm/s.9 Early diastolic flow peak velocity of the mitral valve (E) and early diastolic peak velocity of mitral valve annulus (e’) is used for evaluating left ventricular diastolic function, where E/e’ >15 or e’ <8 cm/s indicates left ventricular diastolic dysfunction.10 The aim of this study was to analyze the epidemiological data of patients with septic cardiomyopathy and the role of different ultrasound indicators in predicting the prognosis of patients through echocardiography, so as to provide a theoretical basis for the early diagnosis and treatment of septic cardiomyopathy.
Materials and Methods
Research Participants
All the procedures performed in this study were in accordance with medical ethics standards and were reviewed and approved by the Medical Ethics Committee.
This prospective study included patients with sepsis treated in the Department of Critical Care Medicine of Beijing Electric Power Hospital between January 2020 and June 2022. Inclusion criteria were as follows: Patients with sepsis who met the sepsis 3.0 diagnostic criteria as per the latest definition of sepsis jointly issued by the Society of Critical Care Medicine (SCCM) and the European Society of Intensive Care Medicine (ESICM) in 2016, which were as follows: Sepsis was defined as life-threatening organ dysfunction caused by a dysregulated host response to infection; sepsis diagnostic criteria were: infection + Sequential (Sepsis-Related) Organ Failure Assessment (SOFA) score ≥2 points. Diagnostic criteria for septic shock: Vasopressors were still required to maintain mean arterial pressure ≥65 mmHg after adequate fluid resuscitation and blood lactate >2 mmol/L.11
Exclusion criteria were as follows: (1) Patients with a history of chronic cardiac insufficiency; (2) Patients with localized ventricular wall motion abnormalities (possibly acute or previous myocardial infarction); (3) Patients with a history of dilated myocardium or hypertrophic obstructive myocardium; (4) Patients with previous heart valve disease; (5) Patients aged <18 years or >80 years; (6) Pregnant women; (7) Patients with atrial fibrillation; (8) Patients with a hospitalization time <24 hours; (9) Patients in whom an echocardiogram was not performed within 24 hours; (10) Patients whose ultrasound image was unclear.
Research Methods
All ultrasonographic examinations were performed by the same senior doctor who had undergone rigorous and considerable time of ultrasound training and had good ultrasound expertise. We collected the following echocardiogram data within 24 hours of admission to the intensive care unit (ICU): left ventricular end-diastolic diameter (LVDD), left ventricular ejection fraction (LVEF), early diastolic flow peak velocity of the mitral valve (E), diastolic flow peak velocity of the mitral valve (A), early diastolic peak velocity of mitral valve annulus (e’), left ventricular systolic mitral annular velocity (LV-Sm), and right ventricular systolic tricuspid annular velocity (RV-Sm).
During the measurement, the apical four-chamber section view of the heart was taken, the tissue Doppler mode was activated, and the pulsed tissue Doppler sampling volume was placed on the lateral wall of the mitral valve annulus. The velocity of the mitral annulus in the left ventricular systole on the obtained spectrum was the systolic S wave peak velocity, and LV-Sm <8 cm/s or LVEF <50% indicated left ventricular systolic dysfunction (Figure 1). The pulsed tissue Doppler sampling volume was placed on the lateral wall of the tricuspid annulus, the systolic S wave peak velocity was obtained on the spectrogram, and RV-Sm <12 cm/s indicated abnormal right ventricular systolic function. The pulsed tissue Doppler sampling volume was placed on the lateral wall of the mitral valve annulus, and the early diastolic peak velocity of the mitral valve annulus was measured, and E/e’ >15 or e’ <8 cm/s indicated left ventricular diastolic dysfunction.
Diagnostic criteria for septic cardiomyopathy included sepsis + any of the following ultrasound results and no previous underlying cardiac diseases.
Ultrasound Results
LV-Sm <8 cm/s indicated left ventricular systolic dysfunction; RV-Sm <12 cm/s indicated right ventricular systolic dysfunction; E/e’ >15 or e’ <8 cm/s indicated left ventricular diastolic cardiomyopathy. Previous underlying cardiac diseases included chronic cardiac insufficiency, limited ventricular wall motion abnormalities, dilated myocardium, history of hypertrophic obstructive cardiomyopathy, and heart valve disease.
Sample Collection and Processing Methods
We collected general information, including age, gender, body mass index, previous diseases (especially the presence of hypertension, diabetes, and coronary heart disease), infection site, and disease diagnosis from all patients. We also collected the SOFA score within 24 hours of admission, 28-day prognosis, and other indicators.
Statistical Analysis
We used SPSS 22.0 statistical software package for all statistical analyses. Count data were expressed as frequency (F), constituent ratio, or percentage, and all measurement data were expressed as mean ± standard deviation  . Measurement data conforming to normal distribution were compared between the two groups using independent sample t-test, and measurement data not conforming to normal distribution were compared using the Wilcoxon rank sum test. The chi-square test was used to compare the rates between the two groups. Linear correlation between the ultrasound parameters LVEF and LV-Sm, E/e’, and e’ was analyzed using Spearman’s rank correlation analysis. The receiver operating characteristic curve (ROC) was used to evaluate the predictive value of echocardiograph-related indicators for death in patients with sepsis, while the evaluation indexes were the area under the ROC curve (AUC) and 95% confidence interval (95% CI). Multivariate binary logistic regression analysis was used to analyze the risk factors affecting the prognosis of patients with sepsis, and the evaluation index was odds ratio (OR). P < 0.05 was considered statistically significant.
. Measurement data conforming to normal distribution were compared between the two groups using independent sample t-test, and measurement data not conforming to normal distribution were compared using the Wilcoxon rank sum test. The chi-square test was used to compare the rates between the two groups. Linear correlation between the ultrasound parameters LVEF and LV-Sm, E/e’, and e’ was analyzed using Spearman’s rank correlation analysis. The receiver operating characteristic curve (ROC) was used to evaluate the predictive value of echocardiograph-related indicators for death in patients with sepsis, while the evaluation indexes were the area under the ROC curve (AUC) and 95% confidence interval (95% CI). Multivariate binary logistic regression analysis was used to analyze the risk factors affecting the prognosis of patients with sepsis, and the evaluation index was odds ratio (OR). P < 0.05 was considered statistically significant.
Results
General Information of Patients
A total of 155 patients diagnosed with sepsis or septic shock were screened between January 2020 and June 2022. We excluded 55 patients based on the exclusion criteria, and finally included 100 patients who met the criteria. There were 33 deaths, amounting to a mortality rate of 33%, and 76 patients had septic shock. We compared the 28-day indicators of sepsis patients from the survival group and the mortality group (Table 1).
 |
Table 1 Comparison of the Primary Infection Site and General Condition Between the Death Group and the Survival Group |
The most common site of infection was the respiratory tract, followed by the gastrointestinal tract and urinary system. There were no significant differences in the number of primary infections in each site between the two groups (P > 0.05). There were also no significant differences in age, gender, body mass index, prevalence of hypertension, diabetes, and coronary heart disease between the two groups (P > 0.05).
Proportion of Different Types of Septic Cardiomyopathy
Among the 100 patients, 49 of them had septic cardiomyopathy, and the prevalence of septic cardiomyopathy was 49%. There were 40 patients with left ventricular diastolic dysfunction cardiomyopathy, 24 patients with left ventricular systolic dysfunction cardiomyopathy, 3 patients with simple left ventricular systolic dysfunction cardiomyopathy, and 18 patients with left ventricular systolic and diastolic dysfunction cardiomyopathy. There were also 12 patients with right ventricular systolic dysfunction cardiomyopathy, and 4 patients with left ventricular systolic and diastolic and right ventricular dysfunctional cardiomyopathy (Figure 2).
 |
Figure 2 Chart showing the proportion of different types of septic cardiomyopathy. |
Comparison of Ultrasound Parameters Between the Survival Group and the Mortality Group
As shown in Table 2, the survival group had significantly higher e’ and RV-Sm than the mortality group (e’: 8.61±0.99 vs 8.01±1.01, P = 0.006; RV-Sm: 13.69±1.74 vs 12.10±2.47, P = 0.00). The LVEF and LV-Sm in the survival group were slightly lower than those in the mortality group, but the difference between the groups was not significant (P > 0.05).
 |
Table 2 Comparison of Ultrasound Parameters Between Survival and Deceased Group |
Logistic Regression Analysis of Prognostic Factors in Patients with Sepsis
We included the e’ and RV-Sm indicators with significant differences between the mortality group and the survival group in the multivariate binary logistic regression analysis. The results revealed that both e’ and RV-Sm were independent risk factors affecting the prognosis of patients (all P < 0.05) (Table 3).
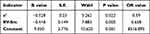 |
Table 3 Logistic Regression Analysis of Prognostic Factors in Patients with Sepsis |
ROC Curve Analysis of Ultrasound Indicators in Predicting the Prognosis of Patients with Sepsis
The AUC of e’ in predicting the prognosis of ICU patients with sepsis was 0.657, the sensitivity was 67.7% and the specificity was 71% when the optimal cut-off value was 8.65 (P=0.005). The AUC of RV-Sm in predicting the prognosis of patients with sepsis was 0.668 (P=0.007), the optimal cutoff value was 12.85, the sensitivity was 51.6%, and the specificity was 73.9% (Figure 3, Table 4).
 |
Table 4 The Predictive Value of Ultrasound-Related Indicators for the Prognosis of Patients with Sepsis |
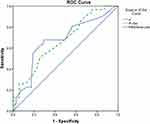 |
Figure 3 ROC curve analysis of ultrasound-related indicators for predicting the prognosis of patients with sepsis. |
Discussion
Sepsis-induced cardiac dysfunction is not limited to the left heart, and often, the right heart is involved.12,13 The results of the present study revealed that among 100 patients with sepsis, 49 had septic cardiomyopathy, resulting in a 49% prevalence of septic cardiomyopathy. Among 100 patients, the prevalence of left ventricular diastolic dysfunction cardiomyopathy was the highest, ie, 40% (40 cases); the prevalence of left ventricular systolic dysfunction cardiomyopathy was 24% (24 cases); the prevalence of right ventricular systolic dysfunction cardiomyopathy was 12% (12 cases); the prevalence of left ventricular systolic, diastolic and right ventricular dysfunction cardiomyopathy was 4%.
Charlhall et al14 detected LV-Sm in 28 healthy people using tissue Doppler and found that the mitral annular systolic displacement was closely related to the maximum oxygen consumption per kg body weight and stroke volume but was not correlated with LVEF, ie, LV-Sm could be used to assess left ventricular systolic function, while LVEF did not result as a good evaluation index of left ventricular systolic function. Furian et al15 found that LV-Sm was moderately positively correlated with LVEF, and that LVEF and LV-Sm were moderately positively correlated. However, more studies are needed to examine the correlation between LV-Sm and LVEF, which remains a controversial issue.
The most commonly used method for judging left ventricular diastolic dysfunction is determining left ventricular diastolic filling characteristics by using early diastolic flow peak velocity of the mitral valve (E), diastolic flow peak velocity of the mitral valve (A), and their ratio (E/A). However, multiple factors interfere with the mitral valve flow spectrum, and these include anterior and posterior cardiac load, transvalvular pressure difference, left ventricular systolic function, left ventricular diastolic function, left atrial size, left atrial compliance, age, and heart rate. Especially in the case of “pseudo normalization”, the assessment of left ventricular diastolic function should be combined with other ultrasound indicators.16
Unlike the principle of using mitral valve blood flow spectrum to evaluate left ventricular diastolic function, tissue Doppler ultrasound technology is based on the velocity of the mitral annulus. Since it is not affected by left atrial and left ventricular filling pressure, the velocity of the mitral annulus is directly related to ventricular muscle elastic recoil, and e’ is an extremely important index for evaluating left ventricular diastolic function. Internationally, E/e’ >15 or e’ <8 cm/s is commonly used to evaluate the presence of left ventricular diastolic dysfunction.14
In the present study, we found a moderately significant negative correlation between E/e’ and e’ (P < 0.05). This may be related to the fact that there may have been many factors that interfered with the mitral flow spectrum E, while there was not much interference in the e’ measured by tissue Doppler technique. E/e’ and e’, two commonly used parameters to evaluate left ventricular diastolic function, were correlated, albeit moderately.
LVEF and LV-Sm and Prognosis in Patients with Sepsis
In the present study, we found that LVEF and LV-Sm in the mortality group were slightly higher than those in the survival group; however, the difference was not significant. In 1984, Parker et al17 found that EF values in the mortality group were normal or even higher than normal among patients with septic shock, while LVEF in the survival group was lower than normal. Also, cardiac function in these survivors with low EF values returned to normal within 10 days. At the same time, compared with the deceased patients, the survival group had dilated left ventricles and increased end-diastolic volume and end-systolic volume, while the deceased patients had lower systemic circulation resistance and higher cardiac output index. In 1990, Jardin et al18 observed the same phenomenon as above, so they opined that left ventricular dilation and decreased EF were benign responses to septic shock, and patients with poor ventricular compliance and who were unable to adapt to left ventricular dilation had a lower survival rate. As the left ventricular EF value was not only related to myocardial contractility but also left ventricular afterload, the left ventricular EF value of the patients who died of sepsis was normal or even high, and this may be related to the lower afterload.19
Weng et al20 studied 61 patients with septic shock and found that LV-Sm in the mortality group was significantly higher than that in the survival group within 24 hours, and high LV-Sm was an independent risk factor for 28-day mortality in patients with septic shock. In the present study, we found that left ventricular LVEF and LV-Sm in the survival group were slightly lower than those in the mortality group; however, there was no significant difference between the two groups. This finding in our study is inconsistent with the above-mentioned studies. It should be noted that all the research participants in the study conducted by Weng et al20 were patients with septic shock, and among the 100 patients with sepsis in our study, only 76 patients had septic shock. It is possible that the inconsistencies are due to the different inclusion criteria of patients in the two studies and the different severity of the disease. As early as 2010, Sturgess et al21 studied the role of LV-Sm in patients with early sepsis and found that the mortality group had a slightly higher LV-Sm than the survival group. However, the observed difference was not significantly different. The conclusion of the present study is consistent with this finding.
E’ is an Independent Risk Factor Affecting the Prognosis of Patients
In the survival group, e’ was significantly higher than in the mortality group, while E/e’ was not statistically different between the two groups. e’ is a specific index reflecting left ventricular diastolic function, whose measured value is not affected by factors such as anterior and posterior cardiac load and left ventricular systolic function, thus enabling it to accurately reflect left ventricular diastolic function. In the present study, e’ in the survival group was significantly higher than that in the mortality group, thus indicating that the mortality of patients with left ventricular diastolic dysfunction was significantly higher than that in the survival group. This finding is consistent with the conclusion of most previous studies.22,23
E/e is another commonly used index to reflect left ventricular diastolic function.24 However, the measurement value of E is affected by many factors, such as age, left atrial size, mitral valve pressure gradient, left ventricular compliance, cardiac preload and postload, left ventricular systolic function. Therefore, there are certain defects in using E/e to reflect left ventricular diastolic function. The present study showed that there was no statistically significant difference in E/e’ between the survival group and the mortality group.
Sepsis-Associated Right Ventricular Dysfunction
Sepsis-induced cardiac dysfunction occurs not only in the left heart but also in the right heart. However, sepsis-related lowering of right heart function is often ignored. In the present study, we considered Sm <12 cm/s as the standard of right ventricular systolic dysfunction,7 and found that the prevalence of right ventricular systolic dysfunction cardiomyopathy was 12%. This rate was significantly lower than the 31% reported in the study by Pulido.8 Inconsistencies in the results may be due to the following reasons: 1) Human factors could have influenced the ultrasound data significantly, and the sample size of this study was small. Harmankaya et al found that the variation rate of RV-Sm value obtained by different operators ranged between 2.9% and 5.1%;25 2) The standard of right ventricular dysfunction in the study by Pulido et al8 was Sm ≤15 cm/s, while in this study, we considered RV-Sm ≤12cm/s as the standard for right ventricular dysfunction, which is in line with the standard of Furian.15 The different research standards used could have contributed to the inconsistent findings.
In the present study, right heart dysfunction was found to be an independent risk factor for mortality in patients with sepsis. So far, the relationship between right ventricular dysfunction and prognosis in sepsis has remained controversial. Orde et al26 reported that right heart dysfunction was significantly associated with 6-month mortality in patients with sepsis. Another study27 found a significant correlation between right ventricular systolic dysfunction and in-hospital mortality in patients with sepsis. Vallabhajosyula et al28 conducted an 8-year study on sepsis patients with right heart dysfunction and found right heart dysfunction to be an independent risk factor for death in sepsis patients after one year. Yet, in their meta-analysis, Huang et al29 found that right heart dysfunction in patients with sepsis did not affect their short-term prognosis.
Due to limited clinical studies on sepsis-induced right heart dysfunction and the fact that the physiological anatomy of the right heart is more complex than that of the left heart, evaluating its function is more challenging. In addition, the criteria for evaluation of right heart dysfunction and the methods of research pertaining to right heart dysfunction among patients with sepsis are inconsistent, and this may lead to considerable differences in research results.
The present study has some limitations. This was not a multicenter study, and only 100 patients were included. Accordingly, future multicenter studies with more patients are needed to obtain more robust data. The repeatability of the ultrasound data collected in this study needs to be evaluated. Ultrasound measurement is easily influenced by the operator’s subjectivity, so there may have been some variations in data collection that were inevitable. One of the limitations is that the echocardiographic examination was performed only once. In addition to this, patients who received vasopressor therapy were not excluded as the hemodynamic status was not stable, which may also affect the cardiac functions. Among the 100 patients, 73 patients had septic shock, but we did not further stratify the relevant data or analyze subgroups of patients, such as the relevant between who used vasoactive or inotropic drugs, which need further research in a follow-up study. We studied the differences in related ultrasound indicators between patients with or without shock in the sepsis mortality group and survival group. We only analyzed the correlation and differences in ultrasound parameters within 24 hours but did not study the correlation and differences among related parameters after 24 hours. Two-dimensional speckle tracking echocardiography is a new ultrasound technology to accurately evaluate cardiac function. It has good repeatability without angle dependence. It also solves the problem that the ventricular wall motion is affected by the global motion of the heart and the passive traction of the surrounding myocardial segments. These effects make it an effective method for evaluating cardiac function.30,31 It is a pity that prognostic indicators assessed by two-dimensional speckle tracking echocardiography were not evaluated in the present study.
In conclusion, the results of this study revealed a high prevalence of septic cardiomyopathy. Additionally, both RV-Sm and e’ had important predictive value in the 28-day prognosis of patients with sepsis.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval and Consent to Participate
I confirm that I have read the Editorial Policy pages. This study was conducted with approval from the Ethics Committee of Capital medical university electric teaching hospital/Beijing Electric Power Hospital (No. S2018106). This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
This work was supported by Scientific Research Project of Jiangsu Commission of Health of the People’s Republic of China (grant number: Z2020055), and the Ministry of Science and Technology of the People’s Republic of China (grant number: 2012BAI11B05).
Disclosure
The authors declare that they have no competing interests.
References
1. Ackerman MH, Ahrens T, Kelly J, et al. Sepsis. Critical Care Nursing Clin North Am. 2021;33(4):407–418. doi:10.1016/j.cnc.2021.08.003
2. Lu N-F, Jiang L, Zhu B, et al. Elevated Plasma Histone H4 Levels Are an Important Risk Factor in the Development of Septic Cardiomyopathy. Balkan Med J. 2020;37(2):72–78. doi:10.4274/balkanmedj.galenos.2019.2019.8.40
3. Wan S-Y, Hu J-G, Zhang Y, Yu B-Y, Kou J-P, Li F. Recent advances of traditional Chinese medicine in the regulation of myocardial mitochondrial function. World Journal of Traditional Chinese Medicine. 2022;8(1):50–58. doi:10.4103/wjtcm.wjtcm_78_20
4. Ince ME, Turgut K, Akar A, et al. Prognostic importance of tissue Doppler imaging of systolic and diastolic functions in dogs with severe sepsis and septic shock. Acta Vet Hung. 2019;67(4):517–528. doi:10.1556/004.2019.051
5. Meluzin J, Špinarová L, Bakala J, et al. Pulsed Doppler tissue imaging of the velocity of tricuspid annular systolic motion. A new, rapid, and non-invasive method of evaluating right ventricular systolic function. Eur Heart J. 2001;22(4):340–348. doi:10.1053/euhj.2000.2296
6. Meluzin J, Spinarova L, Hude P, et al. Prognostic importance of various echocardiographic right ventricular functional parameters in patients with symptomatic heart failure. J Am Soc Echocardiogr. 2005;18(5):435–444.
7. Wang J, Prakasa K, Bomma C, et al. Comparison of novel echocardiographic parameters of right ventricular function with ejection fraction by cardiac magnetic resonance. J Am Soc Echocardiogr. 2007;20(9):1058–1064.
8. Pulido JN, Afessa B, Masaki M, et al. Clinical spectrum, frequency, and significance of myocardial dysfunction in severe sepsis and septic shock. Mayo Clin Proc. 2012;87(7):620–628.
9. Vinereanu D, Khokhar A, Tweddel AC, et al. Estimation of global left ventricular function from the velocity of longitudinal shortening. Echocardiography. 2002;19(3):177–185.
10. Nagueh SF, Appleton CP, Gillebert TC, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009;10(2):165–193.
11. Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801–810.
12. Lanspa MJ, Cirulis MM, Wiley BM, et al. Right Ventricular Dysfunction in Early Sepsis and Septic Shock. Chest. 2021;159(3):1055–1063.
13. Martin L, Derwall M, Al Zoubi S, et al. The Septic Heart: current Understanding of Molecular Mechanisms and Clinical Implications. Chest. 2019;155(2):427–437.
14. Carlhall CJ, Lindstrom L, Wranne B, et al. Atrioventricular plane displacement correlates closely to circulatory dimensions but not to ejection fraction in normal young subjects. Clin Physiol. 2001;21(5):621–628.
15. Furian T, Aguiar C, Prado K, et al. Ventricular dysfunction and dilation in severe sepsis and septic shock: relation to endothelial function and mortality. J Crit Care. 2012;27(3):319.
16. Silbiger JJ. Pathophysiology and Echocardiographic Diagnosis of Left Ventricular Diastolic Dysfunction. J Am Soc Echocardiogr. 2019;32(2):216–232.
17. Parker MM, Shelhamer JH, Bacharach SL, et al. Profound but reversible myocardial depression in patients with septic shock. Ann Intern Med. 1984;100(4):483–490.
18. Jardin F, Brun-Ney D, Auvert B, et al. Sepsis-related cardiogenic shock. Crit Care Med. 1990;18(10):1055–1060.
19. Repesse X, Charron C, Vieillard-Baron A. Evaluation of left ventricular systolic function revisited in septic shock. Crit Care. 2013;17(4):164.
20. Weng L, Liu YT, Du B, et al. The prognostic value of left ventricular systolic function measured by tissue Doppler imaging in septic shock. Crit Care. 2012;16(3):R71.
21. Sturgess DJ, Marwick TH, Joyce C, et al. Prediction of hospital outcome in septic shock: a prospective comparison of tissue Doppler and cardiac biomarkers. Crit Care. 2010;14(2):R44.
22. Mourad M, Chow-Chine L, Faucher M, et al. Early diastolic dysfunction is associated with intensive care unit mortality in cancer patients presenting with septic shock. Br J Anaesth. 2014;112(1):102–109.
23. Santos TM, Franci D, Schweller M, et al. Left Ventricle Tissue Doppler Imaging Predicts Disease Severity in Septic Patients Newly Admitted in an Emergency Unit. J Emerg Med. 2015;49(6):907–915.
24. Mitter SS, Shah SJ, Thomas JD. A Test in Context: e/A and E/e’ to Assess Diastolic Dysfunction and LV Filling Pressure. J Am Coll Cardiol. 2017;69(11):1451–1464.
25. Harmankaya A, Akilli H, Gul M, et al. Assessment of right ventricular functions in patients with sepsis, severe sepsis and septic shock and its prognostic importance: a tissue Doppler study. J Crit Care. 2013;28(6):1111–1117.
26. Orde SR, Pulido JN, Masaki M, et al. Outcome prediction in sepsis: speckle tracking echocardiography based assessment of myocardial function. Crit Care. 2014;18:R149.
27. Landesberg G, Jaffe AS, Gilon D, et al. Troponin elevation in severe sepsis and septic shock: the role of left ventricular diastolic dysfunction and right ventricular dilatation. Crit Care Med. 2014;42(4):790–800.
28. Vallabhajosyula S, Kumar M, Pandompatam G, et al. Prognostic impact of isolated right ventricular dysfunction in sepsis and septic shock: an 8-year historical cohort study. Ann Intensive Care. 2017;7(1):94.
29. Huang S, Nalos M, Mclean AS. Is early ventricular dysfunction or dilatation associated with lower mortality rate in adult severe sepsis and septic shock? A meta-analysis. Crit Care. 2013;17(3):R96.
30. Hai PD, Phuong LL, Dung NM, et al. Subclinical Left Ventricular Systolic Dysfunction in Patients with Septic Shock Based on Sepsis-3 Definition: a Speckle-Tracking Echocardiography Study. Crit Care Res Pract. 2020;2020:6098654.
31. Sonaglioni A, Cara MD, Nicolosi GL, et al. Rapid Risk Stratification of Acute Ischemic Stroke Patients in the Emergency Department: the Incremental Prognostic Role of Left Atrial Reservoir Strain. J Stroke Cerebrovasc Dis. 2021;30(11):106100.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

