Back to Journals » Open Access Rheumatology: Research and Reviews » Volume 11
Early Diagnosis Of Inflammatory Arthritis By Primary Care Physicians Following Training By A Rheumatologist
Authors Magliah R , Hafiz W , Alahmadi ZA , Siddiqui MI, Ahmed HM , Attar SM , Janoudi N, Almoallim H
Received 10 July 2019
Accepted for publication 1 November 2019
Published 13 December 2019 Volume 2019:11 Pages 315—321
DOI https://doi.org/10.2147/OARRR.S222630
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Chuan-Ju Liu
Rami Magliah,1 Waleed Hafiz,2,3 Ziad Abdulaziz Alahmadi,2 Muhammad Irfanullah Siddiqui,4 Haytham Mohamed Ahmed,5 Suzan Mansour Attar,6 Nahed Janoudi,7 Hani Almoallim2,3,7
1Department of Medicine, King Abdullah Medical City, Makkah, Saudi Arabia; 2Department of Medicine, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia; 3Alzaidi Chair of Research in Rheumatic Diseases, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia; 4Department of Community Medicine, Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia; 5Pfizer Biopharmaceutical Group, Emerging Markets, Jeddah, Saudi Arabia; 6Department of Medicine, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia; 7Department of Medicine, Dr. Soliman Fakeeh Hospital, Jeddah, Saudi Arabia
Correspondence: Waleed Hafiz
Department of Medicine, Faculty of Medicine, Umm Al-Qura University, 2254 Al-Taif Road, Al-Mashaer District, Makkah 7250-24255, Saudi Arabia
Tel +966 12 527 0000 4041
Email [email protected]
Background: Early diagnosis and therapeutic management of inflammatory arthritis (IA) is crucial for minimizing disease progression and improving outcomes. We recently developed the New Early Arthritis Referral Criteria to help improve the detection of suspected early IA via musculoskeletal (MSK) examination. The present study aimed to evaluate the agreement between rheumatologists and primary care physicians (PCPs) trained by rheumatologists in detecting IA when applying the standardized MSK examination techniques used to develop this criteria in a real-world setting in Jeddah, Saudi Arabia.
Methods: This quasi-experimental study was conducted in 4 primary health centers and involved 30 PCPs and 3 rheumatologists. All PCPs were trained by rheumatologists to apply the standardized MSK examination techniques used to develop the New Early Arthritis Referral Criteria. Patients were eligible if they were >18 years of age and presented with small-joint pain that persisted for >6 weeks. Patients were excluded if they had prior diagnosis of osteoarthritis, hand fractures, or rheumatic disease associated with IA. All patients were examined separately by a PCP and a rheumatologist, with the findings compared via kappa statistics and the rheumatologist’s findings considered the “gold standard”.
Results: Data from 202 of the 203 enrolled patients were analyzed. There was fair-to-moderate agreement between PCPs and rheumatologists when assessing swelling of the small joints and wrist of the right side (range of kappa: 0.14–0.41) and low-to-moderate agreement in similar examinations of the left side (range of kappa: 0.04–0.42). Assessments of joint tenderness showed fair-to-moderate agreement for both the right side (range of kappa: 0.22–0.47) and left side (range of kappa: 0.24–0.45). P-values were significant for virtually all comparisons.
Conclusion: MSK examinations by PCPs showed a promising extent of agreement in detecting IA with those by rheumatologists following training. Refinement of the standardized training process could further improve accuracy and help PCPs to confidently identify cases of early IA, thus allowing earlier intervention than is typical in this setting.
Keywords: arthritis, physician training, primary care, referral criteria, rheumatic disease
Introduction
Inflammatory arthritis (IA) is a broad clinical term that covers various rheumatic diseases and represents one of the most common causes of disability among the general population.1,2 The damage caused to joints by IA can lead to a loss of function that creates difficulties for those affected in terms of their ability to care for themselves and to work. Early diagnosis and therapeutic management of IA is therefore crucial for minimizing the progression of joint damage and improving outcomes.3,4
Rheumatic diseases often affect multiple organs and there is often a lack of any clear sign or symptom that provides a physician with an indication of the specific nature of the condition. This uncertainty can lead to patients experiencing a delay in receiving a diagnosis and treatment, which increases their risk of permanent joint damage and disability.3,4 Indeed, a study of Saudi patients with rheumatoid arthritis (RA) showed that the period between symptom onset and diagnosis can be as long as 30 months,5 while a separate study showed that the majority (55%) of Saudi patients with RA experience a >50% decrease in their work capacity.6 The prevalence of RA in Saudi Arabia has been reported to be approximately 2.2 cases per 1000 individuals.7 It is unclear whether this disparity represents a true difference in susceptibility within these national populations or a consequence of differences in diagnostic criteria, or a combination of both these factors. Nonetheless, musculoskeletal (MSK) disorders overall represent the second most frequent cause of outpatient visits to primary health centers (PHCs) and private clinics in Saudi Arabia.8 In addition, research from various regions around the world suggests that the level of expertise in applying MSK examination techniques by non-rheumatologists is inconsistent.9–14
The most common scenario in which an individual with potential IA interacts with the Saudi health care system is when they first visit a primary care physician (PCP) and describe experiencing joint pain. According to local procedures, the PCP will then likely apply a set of referral criteria in order to identify cases appropriate for a consultation with a rheumatologist. Despite the growing dependence upon advanced radiologic techniques for the diagnosis of rheumatic diseases,15 their lack of availability in PHCs makes it important for PCPs to be confident and knowledgeable regarding MSK examinations for suspected IA. We have recently published a set of referral criteria (the New Early Arthritis Referral Criteria) that are intended to improve the detection of early IA via MSK examination.16,17 The aim of the present study, which used the same cohort of patients enrolled in the new referral criteria study,16,17 was to evaluate the agreement between rheumatologists and PCPs trained by rheumatologists in detecting IA when applying the standardized MSK examination techniques used in the New Early Arthritis Referral Criteria in a real-world setting in Saudi Arabia.
Methods
Study Design
This quasi-experimental study was conducted in 4 of the 39 PHCs located in Jeddah, Saudi Arabia, with a single PHC from each of Jeddah’s 4 main regions selected randomly from those within each. Prior to the study’s commencement, the protocol was approved by the institutional review boards at each of the participating PHCs, as well as by the Directorate of Health Affairs at the Saudi Ministry of Health. This study has been conducted in accordance to the Declaration of Helsinki. A total of 30 PCPs and 3 rheumatologists participated in the study. All 30 PCPs received the same training at the same time from the 3 rheumatologists, via a standardized process that ensured they were capable of correctly applying the MSK examinations of the hands and wrists described in the New Early Arthritis Referral Criteria. Detailed definitions and descriptions of these MSK examination techniques have been described previously.16
Patients
Any patient who visited a PHC clinic at one of the 4 participating PHCs (Al-Safa, Al-Hamra, Ghulail, or Al-Bawadi) was eligible to be included in the study if they were >18 years of age, presented with pain in the small joints that had persisted for >6 weeks, and provided written informed consent. Patients were excluded if they had already been diagnosed with osteoarthritis, fractures of the hands, or a rheumatic disease associated with IA. Each patient who met the eligibility criteria was examined separately by a PCP and then by a rheumatologist, with the findings from each examination recorded and subsequently compared via statistical analysis. The final diagnosis that each patient received was based on the findings of the rheumatologist and the results from subsequent ultrasound and laboratory tests.
Statistical Analysis
As described previously,17 the overall sample size calculated to be appropriate for the cross-sectional study that served as the basis for the current analysis was 203 patients. Kappa statistics with 95% confidence intervals and Fisher’s exact tests were used to evaluate the extent of agreement between the MSK examination findings reported by the PCPs and the rheumatologists, with the findings of the rheumatologists’ examinations, laboratory findings included, considered as the gold standard. The extent of agreement as indicated by kappa values was defined, according to Cohen’s criteria, as follows: none to slight (kappa <0.20), fair (kappa 0.21–0.40), moderate (kappa 0.41–0.60), substantial (kappa 0.61–0.80), and almost perfect (kappa 0.81–1.00).18 The statistical software we used was SPSS (Version 23).
Results
Patient Demographics
A total of 203 participants were enrolled, with data from 202 patients included in the present analysis and data from 1 patient excluded due to incompleteness. This cohort has been described previously (Table 1).17
 |
Table 1 Patient-Reported Clinical And Demographic Variables |
Application Of The Standardized MSK Examination Techniques Used In The New Early Arthritis Referral Criteria By PCPs Following Training By Rheumatologists
Joint Swelling
Comparison of the examination findings obtained by the PCPs and rheumatologists showed that kappa values for the extent of agreement with regards to assessing swelling of the metacarpophalangeal (MCP) and proximal interphalangeal joints (PIP) and wrist of the right side ranged from 0.14 to 0.41, indicating a slight-to-moderate extent of agreement, with the majority of kappa values in the slight-to-fair range (Table 2). P values were significant for all (p<0.01 for all except MCP 4, for which p=0.04), which indicates that the extent of agreement observed was highly unlikely to be due to chance. The extent of agreement with regard to swelling of the MCP and PIP joints of the left side was in the slight-to-fair range of kappa values (0.04 to 0.37), while agreement in regard to swelling of the left wrist was moderate (kappa value: 0.41). P values were significant (p<0.01 for all) for all comparisons except the MCP 4 and MCP 5 joints.
 |
Table 2 Agreement Between PCPs And Rheumatologists In The Detection Of Joint Swelling |
Joint Tenderness
Similar to the results obtained from evaluations of joint swelling, comparisons of the examination findings obtained by the PCPs and rheumatologists when assessing joint tenderness in the MCP and PIP joints gave kappa values that ranged from 0.22 to 0.39 for the right side, indicating a fair extent of agreement, with a moderate extent of agreement for the right wrist (kappa value: 0.47). P values were highly significant for all (p<0.001 for all; Table 3). Similarly, fair-to-moderate extent of agreement was observed in comparisons of joint tenderness on the left side, with kappa values ranging from 0.24 to 0.45 and p values being highly significant for all (p<0.001 for all).
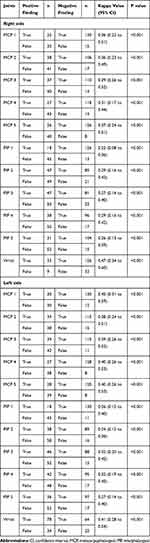 |
Table 3 Agreement Between PCPs And Rheumatologists In The Detection Of Joint Tenderness |
Confirmed Diagnoses Of Inflammatory Arthritis
Overall, there were 128 of the 203 enrolled patients (63.1%) who received a final diagnosis of IA.
Discussion
The present study investigated the extent of agreement between rheumatologists and PCPs trained by rheumatologists in detecting IA when applying the standardized MSK examination techniques used in the New Early Arthritis Referral Criteria to suspected cases of IA in a real-world setting in Saudi Arabia. Overall, agreement between PCPs and rheumatologists was fair and in some cases moderate. We believe that these promising findings may be built upon by further refining the standardized training process so that, ultimately, the PCPs are capable of identifying early IA with an accuracy similar to that of a rheumatologist. Providing PCPs with the requisite level of training needed to identify IA via MSK examination early and with confidence is expected to improve outcomes for patients, in terms of earlier diagnosis and treatment to minimize disease progression and improve quality of life. Additional positive outcomes for society in general would include reducing the impact of the disease on family and friends and limiting the costs associated with advanced disease and lost workplace productivity.
The promising results demonstrated by the PCPs trained during our study should also be considered in light of published accounts of the inconsistent level of expertise in applying MSK examination techniques by non-rheumatologists in various geographic regions. Indeed, Zaini and colleagues reported low confidence among internal medicine residents in Saudi Arabia when conducting MSK examinations,14 and a US study reported that 78% of internal medicine residents demonstrated a lack of skills in assessing the MSK system via examination.11 Furthermore, a study of medical students from Harvard University noted their inadequate preparation in MSK medicine, including a lack of clinical confidence and cognitive mastery in the field.10 Similar conclusions have been reached by Coady and colleagues, who identified a lack of agreement on what to teach, a lack of confidence in teaching amongst non-MSK specialties, and poor communication between specialties as barriers to improving the teaching of MSK examination,9 Oswald and colleagues, who noted the relatively limited hours devoted to training of MSK examination skills in Canadian medical schools, which ignores the prevalence of these conditions within the general population,12 and Stansfield and colleagues, who reported an evident lack of clinical skills in diagnosing common pathologies of the knees, shoulders, and back among final-year students.13
Our study has some limitations. It was conducted at 4 PHCs within the same geographic region of Saudi Arabia (Jeddah) and the training of PCPs was provided by 3 rheumatologists who were involved in the development of the New Early Arthritis Referral Criteria and who have expert knowledge of the techniques involved. Whether the training of PCPs can be as effective when scaled up and implemented by a wider team of rheumatologists is not known. Furthermore, our study excluded patients who had a prior diagnosis of osteoarthritis, hand fractures, and rheumatic diseases associated with IA. Understanding the outcomes of our training process in a population that includes those patients would require additional investigation. Moreover, to demonstrate the effect of training in MSK examination skills, a control group of PCPs who did not undergo training by rheumatologist to identify IA would have reduced bias in agreement. Additional limitations include the fact that variability in skills among PCPs and agreement among rheumatologists could not be determined.
In conclusion, our results demonstrate that the training of PCPs by rheumatologists led to an overall fair extent of agreement in detecting IA between these two groups when applying the New Early Arthritis Referral Criteria to suspected cases of IA in a real-world setting in Saudi Arabia. Given the lack of confidence and technical skills that have been highlighted in published studies investigating the competency of MSK examinations, we believe that the use of standardized MSK examination techniques in a standardized teaching process provided by rheumatologists may be capable of equipping PCPs with the skills they need in order to accurately identify cases of early IA. This would, in turn, be expected to provide benefits to patients and wider society in general by allowing earlier therapeutic intervention that would limit the progression of joint damage and improve quality of life for patients as well as reducing associated health care costs and workplace disability.
Acknowledgments
This study was supervised by Alzaidi Chair of Research in Rheumatic Diseases (Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia), and was sponsored by Alzaidi Chair of Research in Rheumatic Diseases and Pfizer. Medical writing support was provided by David Wateridge, PhD, of Engage Scientific Solutions and was funded by Pfizer.
Disclosures
Hani Almoallim reports research support from Alzaidi Chair of Research in Rheumatic Diseases (Faculty of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia) and Pfizer. Haytham Mohamed Ahmed is an employee of Pfizer and holds stock or stock options in Pfizer. Rami Magliah, Waleed Hafiz, Ziad Abdulaziz Alahmadi, Muhammad Irfanullah Siddiqui, Suzan Attar, and Nahed Janoudi report no conflicts of interest in this work.
References
1. Centers for Disease Control and Prevention (CDC). Prevalence of disabilities and associated health conditions among adults – United States, 1999. MMWR Morb Mortal Wkly Rep. 2001;50(7):120–125.
2. Stoddard S, Jans L, Ripple J, Kraus L. Chartbook on Work and Disability in the United States, 1998. An InfoUse Report. Washington, DC: Research USNIoDaR; 1998.
3. Finckh A, Liang MH, van Herckenrode CM, de Pablo P. Long-term impact of early treatment on radiographic progression in rheumatoid arthritis: a meta-analysis. Arthritis Rheum. 2006;55(6):864–872. doi:10.1002/(ISSN)1529-0131
4. van Nies JA, Krabben A, Schoones JW, Huizinga TW, Kloppenburg M, van der Helm-van Mil AH. What is the evidence for the presence of a therapeutic window of opportunity in rheumatoid arthritis? A systematic literature review. Ann Rheum Dis. 2014;73(5):861–870. doi:10.1136/annrheumdis-2012-203130
5. Hussain W, Noorwali A, Janoudi N, et al. From symptoms to diagnosis: an observational study of the journey of rheumatoid arthritis patients in Saudi Arabia. Oman Med J. 2016;31(1):29–34. doi:10.5001/omj.2016.06
6. Janoudi N, Almoallim H, Husien W, Noorwali A, Ibrahim A. Work ability and work disability evaluation in Saudi patients with rheumatoid arthritis. Special emphasis on work ability among housewives. Saudi Med J. 2013;34(11):1167–1172.
7. Al-Dalaan A, Al Ballaa S, Bahabri S, Biyari T, Al Sukait M, Mousa M. The prevalence of rheumatoid arthritis in the Qassim region of Saudi Arabia. Ann Saudi Med. 1998;18(5):396–397. doi:10.5144/0256-4947.1998.396
8. Kingdom of Saudi Arabia Ministry of Health. The Annual Health Report – 1430H-2009. Riyadh: Health KoSAMo; 2009.
9. Coady DA, Walker DJ, Kay LJ. Teaching medical students musculoskeletal examination skills: identifying barriers to learning and ways of overcoming them. Scand J Rheumatol. 2004;33(1):47–51. doi:10.1080/03009740310004108
10. Day CS, Yeh AC, Franko O, Ramirez M, Krupat E. Musculoskeletal medicine: an assessment of the attitudes and knowledge of medical students at Harvard Medical School. Acad Med. 2007;82(5):452–457. doi:10.1097/ACM.0b013e31803ea860
11. Freedman KB, Bernstein J. Educational deficiencies in musculoskeletal medicine. J Bone Joint Surg Am. 2002;84(4):604–608. doi:10.2106/00004623-200204000-00015
12. Oswald AE, Bell MJ, Snell L, Wiseman J. The current state of musculoskeletal clinical skills teaching for preclerkship medical students. J Rheumatol. 2008;35(12):2419–2426. doi:10.3899/jrheum.080308
13. Stansfield RB, Diponio L, Craig C, et al. Assessing musculoskeletal examination skills and diagnostic reasoning of 4th year medical students using a novel objective structured clinical exam. BMC Med Educ. 2016;16(1):268. doi:10.1186/s12909-016-0780-4
14. Zaini R, Almoallim H, Hafiz W, et al. Musculoskeletal teaching and training in Saudi internal medicine residency programmes. Creat Educ. 2016;7(6):824–830. doi:10.4236/ce.2016.76085
15. Tan YK, Østergaard M, Conaghan PG. Imaging tools in rheumatoid arthritis: ultrasound vs magnetic resonance imaging. Rheumatology (Oxford). 2012;51(Suppl 7):vii36–vii42. doi:10.1093/rheumatology/kes329
16. Almoallim H, Attar S, Jannoudi N, et al. Sensitivity of standardised musculoskeletal examination of the hand and wrist joints in detecting arthritis in comparison to ultrasound findings in patients attending rheumatology clinics. Clin Rheumatol. 2012;31(9):1309–1317. doi:10.1007/s10067-012-2013-5
17. Almoallim H, Janoudi N, Attar SM, et al. Determining early referral criteria for patients with suspected inflammatory arthritis presenting to primary care physicians: a cross-sectional study. Open Access Rheumatol. 2017;9:81–90. doi:10.2147/OARRR
18. Brennan P, Silman A. Statistical methods for assessing observer variability in clinical measures. BMJ. 1992;304(6840):1491–1494. doi:10.1136/bmj.304.6840.1491
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
