Back to Journals » Therapeutics and Clinical Risk Management » Volume 12
Dysplasia epiphysealis hemimelica (Trevor disease) in the ankle
Authors Ozan F, Doğar F, Gürbüz K, Ekinci Y , Bilal, Öncel ES
Received 19 July 2015
Accepted for publication 11 February 2016
Published 6 April 2016 Volume 2016:12 Pages 545—547
DOI https://doi.org/10.2147/TCRM.S92684
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Fırat Ozan,1 Fatih Doğar,1 Kaan Gürbüz,1 Yakup Ekinci,2 Ökkeş Bilal,3 Eyyüp Sabri Öncel1
1Department of Orthopedics and Traumatology, Kayseri Training and Research Hospital, 2Department of Orthopedics and Traumatology, Develi Hatice Muammer Kocatürk State Hospital, Kayseri, 3Department of Orthopedics and Traumatology, Kahramanmaraş Sütçü İmam University Medical Faculty, Kahramanmaraş, Turkey
Abstract: Dysplasia epiphysealis hemimelica, also termed Trevor disease, is a rare disorder that, although benign in nature, can be locally aggressive, particularly when affecting the ankle joint, which is the joint most frequently affected, followed by the knee. The female:male ratio is 1:3, and it is generally diagnosed between 2 and 14 years of age. Surgical treatment with complete resection is recommended before irreversible joint damage and deformity occurs. We presented a case in which dysplasia epiphysealis hemimelica was diagnosed on the medial aspect of a right ankle joint.
Keywords: dysplasia epiphysealis hemimelica, Trevor disease, ankle, osteochondroma, epiphyseal hypertrophy
Introduction
Dysplasia epiphysealis hemimelica (DEH), also known as Trevor disease, is a rare disorder with unknown etiology. Its estimated incidence is 1:1,000,000.1–4 The ankle joint is most frequently affected, followed by the knee. The female:male ratio is 1:3, and DEH is generally diagnosed between 2 and 14 years of age.1–4
DEH was first described by Mouchet and Belot5 as “tarsomegalie” in 1926. In 1950, Trevor6 reported a case series, including ten patients and proposed the term “tarso-epiphysial aclasis”. In 1956, Fairbank1 reported a case series of 14 patients and used the term “dysplasia epiphysealis hemimelica”. DEH is considered a benign, asymmetrical, intra-articular mass lesion confined by epiphysis, resulting from an abnormal proliferation of cartilage tissue.3,4 We presented a case in which DEH was diagnosed at the medial aspect of the right ankle joint.
Case report
A 9-year-old girl was presented with swelling of the right ankle and pain during walking, for >3 months. The patient had no history of trauma, and there was pain during palpation at the medial aspect of the ankle. An osteocartilaginous mass (2.5 cm ×2.0 cm ×2.0 cm in size), localized at the distal end of the tibia and extending from the vicinity of the medial malleolus to the medial aspect of the talus, was observed using plain radiograph and computerized tomography (CT) (Figure 1).
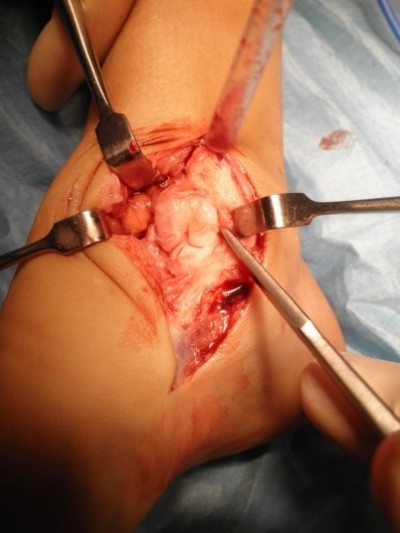
During surgical intervention, a medial incision at the medial aspect of the medial malleolus was made, and subcutaneous tissues were explored. The lesion, of osteocartilaginous appearance and originating from the distal tibial epiphysis at medial malleolus level and extending to the medial aspect of the talus, was exposed, which destructed the medial cortex of the talus. Four large osteocartilaginous lesions were removed from the talus and ankle joint (Figure 2). Histological examination revealed that the lesion was mostly hyperplastic cartilage with little osseous tissue, and these features were identical to that of osteochondroma (Figure 3). However, the patient was diagnosed with DEH when the radiological and gross appearance of the lesion was compared with similar reports in the literature.1–9
During the 14-month follow-up, the patient returned to normal activities. Range of motion at the ankle was normal without pain or disability. This study was conducted in accordance with the ethical guidelines of the Declaration of Helsinki. The patient provided written informed consent before participation. The study protocol was approved by the Kayseri Training and Research Hospital, Kayseri, Turkey.
Discussion
DEH is a rare, osseous developmental disorder manifesting with epiphyseal involvement.3,9 The localized form of the disease generally involves bones in the ankle and hindfoot. DEH is benign and its prognosis is favorable; no malignant transformation has been reported.4,7–9 The etiology of DEH is uncertain. Potential causes include a congenital error affecting the limb bud during early fetal life or the presence of abnormal chondrocytes that continue to proliferate in an unregulated manner.9
In Trevor disease, histopathological diagnosis is not pathognomonic.3 However, EXT1 and EXT2 gene expressions can be studied by additional molecular assays.9 Gene expressions are within normal ranges in DEH, whereas they are lower in osteochondroma owing to a mutation. These tests are costly; hence, clinical and radiological findings are important diagnostic tools.7 CT and magnetic resonance imaging can confirm the diagnosis, aid surgical planning, and define the relationship of the mass to local structures.3,4,9,10 Specifically, CT can help define the anatomical relationship between the mass and the host bone, and magnetic resonance imaging can show the extent of epiphyseal involvement, joint deformity, and the status of the articular surface.1,3,4,9 Radiographs usually demonstrate a partially ossified, lobulated, cartilaginous mass arising unilaterally from the affected epiphysis with or without an osseous connection.3,4,9,10
DEH was classified by Azouz et al11 as having three distinct presentations: localized, classic, and generalized. In Trevor disease, histopathological findings are similar to those in benign osteochondroma,3,4,9,10 and it is also difficult to discriminate DEH from benign osteochondroma clinically and pathologically.4,10 Both diseases are specific to the developmental period. Thus, radiological findings are important in differential diagnosis. Irregular bone growth originating from epiphysis and a distinct ossification focus that can be seen in radiological evaluation are the most important discriminative features of Trevor disease.2–4,9,10 In addition to osteochondroma, intra-articular loose body, myositis ossificans, or synovial chondromatosis can be considered in differential diagnosis.3,4,9
Management options for Trevor disease include observation and surgical excision. Asymptomatic lesions may be treated nonoperatively,3,4,7,8 but surgery should be considered when the lesion causes pain, loss of function, limitation of movement, and deformity.3,4,7,8
Conclusion
In conclusion, DEH is an uncommon, benign disease. Although histopathological findings in Trevor disease are similar to those in osteochondroma, it has differential features that can be distinguished clinically and radiologically. However, molecular analysis has to be done for the definitive diagnosis. Early diagnosis and treatment are necessary to prevent articular dysfunction.
Disclosure
The authors report no conflicts of interest in this work.
References
Fairbank TJ. Dysplasia epiphysialis hemimelica (tarso-ephiphysial aclasis). J Bone Joint Surg Br. 1956;38(1):237–257. | ||
Yurdoglu C, Sahlan S, Oklu T. Hemimelic epiphyseal dysplasia (a case report). Acta Orthop Traumatol Turc. 2004;26(5):348–349. | ||
Kuo RS, Bellemore MC, Monsell FP, Frawley K, Kozlowski K. Dysplasia epiphysealis hemimelica: clinical features and management. J Pediatr Orthop. 1998;18(4):543–548. | ||
Nowicki PD, Borders H. Dysplasia epiphysealis hemimelica (Trevor disease) of the ankle. Orthopedics. 2015;38(4):269–271. | ||
Mouchet A, Belot J. Tarsomegalie. J Radiol Electrol. 1926;10:289–293. | ||
Trevor D. Tarso-epiphysial aclasis: a congenital error of epiphysial development. J Bone Joint Surg Br. 1950;32(2):204–213. | ||
Gokkus K, Aydin AT, Uyan A, Cengiz M. Dysplasia epiphysealis hemimelica of the ankle joint: a case report. J Orthop Surg (Hong Kong). 2011;19(2):254–256. | ||
Ouyang Z, Xu M, Li X, Peng D. Dysplasia epiphysealis hemimelica with involvement of the distal tibial epiphysis and talus: recurrence of a case and literature review. J Foot Ankle Surg. 2014;53(2):199–202. | ||
Tyler PA, Rajeswaran G, Saifuddin A. Imaging of dysplasia epiphysealis hemimelica (Trevor’s disease). Clin Radiol. 2013;68(4):415–421. | ||
Struijs PA, Kerkhoffs GM, Besselaar PP. Treatment of dysplasia epiphysealis hemimelica: a systematic review of published reports and a report of seven patients. J Foot Ankle Surg. 2012;51(5):620–626. | ||
Azouz RM, Slomic AM, Marton D, Rigault P, Finidori G. The variable manifestations of dysplasia epiphysealis hemimelica. Pediatr Radiol. 1985;15(1):44–49. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




