Back to Journals » Infection and Drug Resistance » Volume 16
Dynamics of CD4+ T-Cells and Neutralizing Antibody Responses to Three Consecutive Doses of Inactivated COVID-19 Vaccines in PLWH
Authors Zhang W, Liu S, Miao L, Fu A, Bao J, Zheng L, Li E, Yu J, Wang Y
Received 18 February 2023
Accepted for publication 20 April 2023
Published 4 May 2023 Volume 2023:16 Pages 2695—2707
DOI https://doi.org/10.2147/IDR.S409147
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Wenhui Zhang,1,2 Shourong Liu,1 Liangbin Miao,3 Ai Fu,3 Jianfeng Bao,4 Liping Zheng,2 Er Li,2 Jianhua Yu,1,* Yi Wang1,3,*
1Department of Infection, Affiliated Hangzhou Xixi Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China; 2Department of Nursing, Affiliated Hangzhou Xixi Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China; 3Institute of Hepatology and Epidemiology, Affiliated Hangzhou Xixi Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China; 4Department of Hepatology, Affiliated Hangzhou Xixi Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jianhua Yu, Department of Infection, Affiliated Hangzhou Xixi Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China, Email [email protected] Yi Wang, Institute of Hepatology and Epidemiology, Affiliated Hangzhou Xixi Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China, Email [email protected]
Background: Comprehensive characterization of safety and immune responses to vaccines is crucial for the prevention and treatment of COVID-19 among people living with HIV (PLWH). This study aimed to investigate the dynamic changes in SARS-CoV-2-specific CD4+ T-cell subsets and neutralizing antibody after three consecutive doses of inactivated COVID-19 vaccines (BBIBP-CorV) among PLWH.
Methods: The blood samples were collected from 165 PLWH, including 66 PLWH in the 3-month interval between the second and third dose (cohort 1) and 99 PLWH in the 5-month interval (cohort 2). Blood collection for immunogenicity analysis was performed at 1-month post-2nd vaccination, pre-3rd vaccination, and within 2-month post-3rd vaccination. Wilcoxon matched-pairs signed-rank test was applied to compare the SARS-CoV-2-specific CD4+ T cell subsets and neutralizing antibody level at different time points. The relationship among CD4+ T-cells, Tregs subpopulations and SARS-CoV-2-specific neutralizing antibody level were evaluated with Spearman non-parametric correlation test.
Results: No serious adverse reactions were found among PLWH. After two-dose or three-dose inactivated COVID-19 vaccination, the absolute counts of CD4+ T-cells and Tregs subpopulations (CD4+CD25HighCD127Low Tregs, CD45RA+ rTregs and CD45RO+ eTregs) increased in two cohorts. Satisfactory SARS-CoV-2-specific neutralizing antibody responses to the third-dose vaccination were found in two cohorts, including significantly enhanced neutralizing antibody level and high neutralizing antibody seroconversion rate. In addition, SARS-CoV-2-specific neutralizing antibody level were positively associated with the absolute counts of CD4+ T-cells and Tregs subpopulations as well as the frequency of CD45RO+ eTregs in PLWH after three doses of vaccinations.
Conclusion: The three doses of inactivated COVID-19 vaccination were both safe and effective to increase SARS-CoV-2-specific CD4+ T-cells and neutralizing antibody in two PLWH cohorts with different inoculation intervals.
Keywords: CD4+ T-cells, neutralizing antibody, inactivated COVID-19 vaccines, PLWH
Introduction
Coronavirus disease 2019 (COVID-19) caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection has been a great threat to public health,1 and was defined as a pandemic by the World Health Organization (WHO) in 2020.2 Vaccination represents one of the most powerful tools to combat the spread of SARS-CoV-2 infection3 and reduce the mortality risk from COVID-194 among immunocompromised patients.5 People living with HIV (PLWH) are immunodeficient and more vulnerable to SARS-CoV-2 infection6 and clinicians should pay special attention to the safety of COVID-19 vaccines and vaccine-triggered humoral and cellular immune responses in PLWH.
The neutralizing antibody (NAb) against SARS-CoV-2 is particularly important indicator for the evaluation of humoral immunity after vaccination.7,8 Available studies have focused on the NAb responses in PLWH after two-dose or the third-dose COIVD-19 vaccination.9,10 Nevertheless, little is known about the vaccine-induced NAb responses among PLWH at different inoculation intervals, which may affect the management of vaccination in PLWH.
On the other hand, CD4+ T lymphocytes cells (CD4+ T cells) as the main target of HIV are reported to be associated with both humoral and cellular immune responses to COVID-19 vaccination, and play a pivotal role in the vaccination management.11 Regulatory T cells (Tregs) are one of CD4+ T cell subsets with the ability to maintain immune homeostasis in COVID-19.12 In addition, a recent study shows that CD4+CD25HighCD127Low Tregs can activate dendritic cells to produce antigen-specific immunity against emerging SARS-CoV-2 antigens.13 Thus, the dynamic analysis of Tregs subpopulations following inactivated COVID-19 vaccination demand increasing attention. Very recently, the You group found the percentage of Tregs decreased but the frequency of memory Treg subpopulations increased in healthy individuals after two-dose COVID-19 vaccination.14 In addition, the distribution of Tregs subpopulations was also assessed among people with multiple sclerosis15 and allergic rhinitis.16 Although some studies that have been devoted to investigate the variation of Tregs subpopulations in healthy individuals after inactivated COVID-19 vaccination, to the best of our knowledge, such a study among PLWH remains elusive. Under this situation, the dynamic changes in Tregs subpopulations following inactivated COVID-19 vaccination deserve to comprehensively characterize.
In this study, the safety and immune responses to three consecutive doses of inactivated COVID-19 vaccinations were investigated comprehensively in two PLWH cohorts with different intervals, by focusing on the CD4+ T-cells and their subsets. In addition, the correlations between NAb level and CD4+ T-cells and their subsets were further evaluated. Our study provided information for the vaccination strategies in PLWH.
Materials and Methods
Study Population and Design
This study was conducted by Hangzhou Xixi Hospital in collaboration with the Zhejiang Provincial Center for Disease Control and Prevention (CDC) in Hangzhou, Zhejiang Province, China. The critical inclusion criteria for PLWH were as follows: (1) Subjects were older than 18 years; (2) Patients were diagnosed with HIV infection by Western blotting; (3) Patients received standardized antiretroviral therapy (ART) treatment, and the viral load of HIV was less than 50 copies/mL in plasma; (4) CD4+ cell count was less than 500 cells/μL, but more than 50 cells/μL; (5) Written informed consent was obtained from each patient. Exclusion criteria: (1) Patients had a history of SARS-CoV-2 infection and vaccination; (2) Patients did not receive ART treatment; (3) CD4+ cell count was less than 50 cells/μL; (3) Patients had malignant tumors or severe opportunistic infections; (4) Patients had severe allergic reactions to vaccines; (5) Patients had other co-morbidities. This was an observational research study that collected data from PLWH vaccinated with three consecutive doses of inactivated COVID-19 vaccines (BBIBP-CorV, Beijing Biotechnic Co., Ltd.) at Hangzhou Xixi Hospital. At T1, all PLWH received two doses (0.5 mL/dose) of inactivated COVID-19 vaccines between September 15 and October 18, 2021. In post-2nd vaccination (T2), 60 PLWH were excluded, because 37 patients refused to provide blood samples and 23 patients failed to timely provide blood samples. Blood samples were collected at T1 and T2 from the remaining 211 PLWH to assess the cellular immune responses to two doses of inactivated COVID-19 vaccines in PLWH.
Among 211 PLWH, only 165 PLWH received the SARS-CoV-2 NAb test at pre-3rd vaccination and post-3rd vaccination timepoints. According to the intervals between the second and the third dose, 165 individuals were divided into two cohorts including cohort 1 (an interval of 3 months) and cohort 2 (an interval of 5 months). In addition to T1 and T2, the peripheral blood samples of cohort 1 were collected at 3 months following the second dose (T3) and 2 months following the third dose (T6), while cohort 2 were sampled at 5 months following the second dose (T4) and one month following the third dose (T5). The cellular immune responses to three consecutive vaccinations were evaluated, and the third-dose vaccination-triggered humoral immunity was analyzed in two cohorts. The flowchart is shown in Figure 1.
 |
Figure 1 Study profile for the vaccination schedule and follow-up of PLWH. |
Safety Evaluation
Safety evaluation data were collected by the self-reports of participants and clinical findings from hospital visits within 28 days after each vaccination. All participants were asked to record the injection-site adverse events (including pain, rash, swelling and others), and systemic adverse events (including fatigue, cough, fever and others). Vaccine-induced adverse events were graded according to the China National Medical Products Administration guidelines.17
Cellular Immunophenotyping
The peripheral blood samples were collected for the laboratory tests of CD4+ T-cells, Tregs subpopulations (including CD4+CD25HighCD127Low Tregs, CD45RA+CD4+CD25highCD127−/Low resting Tregs [CD45RA+ rTregs] and CD45RO+CD4+CD25high CD127−/Low effector Tregs [CD45RO+ eTregs]). The peripheral blood samples were processed using FITC anti-human CD45RO (clone UCHL1), PE anti-human CD25 (clone BC96), PerCP-Cyaninie5.5 CD45RA (clone HI100), PE-Cyaninie7 CD4 (clone SK3), or APC anti-human CD127 (clone A019D5), followed by lysing with Red Cell Lysing Buffer. These reagents were purchased from UB biotechnology (Zhejiang) Co., Ltd. The Tregs subpopulations (including CD4+CD25highCD127Low Tregs, CD45RA+ rTregs, and CD45RO+ eTregs) were examined on a NovoCyte 2060R Flow Cytometer and analyzed using NovoExpress 14.1 (Agilent Technologies Inc.). The detection of CD4+ T-cells and their subsets was conducted based on the manufacturer’s instructions at the Hangzhou ADICON Clinical Laboratories Co., Ltd.
Detection of Neutralizing Antibody
The SARS-CoV-2 NAb assay (SHENZHEN YHLO BIOTECH CO., LTD, Shenzhen, China) is a paramagnetic particle chemiluminescent immunoassay (CLIA) for qualitative detection of SARS-CoV-2 NAb in human serum using the automated iFlash immunoassay system.18 It is mainly used for the auxiliary evaluation of the effect of inactivated COVID-19 vaccines. The cut-off value is 10 AU/mL for NAb according to the manufacturer’s instructions. The maximum measurable NAb level was 800 AU/mL. The seroconversion of NAb was defined as a change from seronegative (<1:4) to seropositive (≥1:4).19
Statistical Analysis
All statistical analysis was performed via the R statistical software (R version 4.1.3) and IBM SPSS Statistics (Version 25.0). Normally distributed continuous variables are described as means with standard deviations (SD). The median (M) with interquartile range (IQR, 1st quartile, 3rd quartile) and nonparametric Wilcoxon signed-rank tests were applied for variable description and comparison, respectively. The categorical variables are reported as the numbers and percentages of patients in each category. Proportions were compared by the Pearson’s Chi-square test. The correlation analysis was performed with Spearman non-parametric correlation tests. All graphs were delineated using GraphPad Prism 8 software (GraphPad Software Inc., San Diego, CA, USA). A value of P < 0.05 was considered statistically significant.
Results
Safety Evaluation of Three Doses of Inactivated COVID-19 Vaccines in PLWH
The overall incidence of adverse events in 271 PLWH was 15.13% (n = 41) after the first COVID-19 vaccination, and 6.64% after the 2nd vaccination (n = 18). The overall incidence of adverse events following the first vaccination (41/271) was significantly higher than that following the 2nd vaccination (18/271) (P = 0.002) (Table 1). Adverse events caused by COVID-19 vaccination in PLWH were mostly mild, and almost all adverse events occurred within 7 days after vaccination and resolved within 72 h. No obvious adverse events were recorded in 211 PLWH within 28 days after the 3rd vaccination.
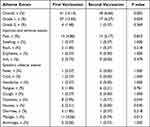 |
Table 1 Overall Adverse Events Within 28 Days After Each Vaccination in 271 PLWH |
Baseline Characteristics of PLWH
In total, 211 PLWH received three consecutive doses of inactivated COVID-19 vaccines. Their baseline characteristics are summarized in Table S1. At enrollment (T1), all PLWH received ART treatment with viral load less than 50 copies/mL and CD4+ T-cell count less than 500 cells/μL.
Considering 165 PLWH with blood samples at each time point, they were divided into two cohorts according to the different time intervals between the second dose and the third dose. The cohort 1 (intervals of 3 months) included 66 PLWH, while cohort 2 (intervals of 5 months) included 99 PLWH. The baseline characteristics mainly included age, sex, education, marital status, residence, household type, body mass index (BMI), hypertension, sexual transmission route and time of therapy initiated (Table 2).
 |
Table 2 Baseline Characteristics of Cohort 1 and Cohort 2 |
CD4+ T-Cells and Subsets After Two Doses of Inactivated COVID-19 Vaccines in 211 PLWH
To fully evaluate cellular immune responses to two doses of inactivated COVID-19 vaccines, the SARS-CoV-2-specific CD4+ T-cells and their subsets were detected in PLWH. Among 211 PLWH, the absolute counts of CD4+ T-cells (Figure 2a), CD4+CD25HighCD127Low Tregs (Figure 2b), CD45RA+ rTregs (Figure 2d) and CD45RO+ eTregs (Figure 2f) significantly increased after two-dose COVID-19 vaccination (from T1 to T2) (P < 0.001), while the frequency of CD45RO+ eTregs (Figure 2g) dramatically dropped (P = 0.003) (Table S2). There were no significant differences in other variates between T1 and T2, including the frequency of CD4+CD25HighCD127Low Tregs (Figure 2c), CD45RA+ rTregs (Figure 2e) and eTregs/rTregs ratio (Figure 2h).
Dynamic Changes in CD4+ T-Cells and Subsets After Three Doses of Inactivated COVID-19 Vaccines in Two PLWH Cohorts
Among cohort 1, the absolute counts of CD4+ T-cells increased rapidly (P < 0.001) until pre-3rd vaccination (from T1 to T3), and then slightly dropped after the 3rd vaccination (from T3 to T6), but it was still significantly higher than that at baseline (pre-vaccination; T1) (Figure 3a, Tables 3 and S3). Coincidentally, a similar pattern was observed in the absolute count and frequency of CD4+CD25HighCD127Low Tregs (Figure 3b and c, Tables 3 and S3). Furthermore, the absolute count and frequency of CD45RA+ rTregs also increased after two-dose COVID-19 vaccination, but reduced remarkably from T3 to T6 (P < 0.001) (Figure 3d and e, Tables 3 and S3). Steep reductions were also found in the absolute count and frequency of CD45RO+ eTregs after the 3rd vaccination (P < 0.001, Figure 3f and g, Tables 3 and S3). There was no significant change in the eTregs/rTregs ratio from T3 to T6 (Figure 3h, Tables 3 and S3).
 |
Table 3 Differences in CD4+ T Cells and Tregs Subpopulations at Three Time Points (T1, T3, T6) in Cohort 1 (n = 66, Interval of 3 Months) |
Among cohort 2, the absolute counts of CD4+ T-cells (Figure 3i), CD4+CD25HighCD127Low Tregs (Figure 3j), CD45RA+ rTregs (Figure 3l) and CD45RO+ eTregs (Figure 3n) continuously raised from T1 to T4 to T5, and they increased significantly at T4 and T5 as compared to those at baseline except for CD45RO+ eTregs (Tables 4 and S4). Interestingly, the changes in the frequencies of CD4+CD25HighCD127Low Tregs (Figure 3k), CD45RA+ rTregs (Figure 3m) and CD45RO+ eTregs (Figure 3o) were quite different (Tables 4 and S4). Specifically, the frequency of CD4+CD25HighCD127Low Tregs increased from T1 to T4, while it decreased from T4 to T5 (Figure 3k, Tables 4 and S4). The frequency of CD45RA+ rTregs remained unchanged after three doses of vaccines (Figure 3m, Tables 4 and S4), and the frequency of CD45RO+ eTregs prominently decreased after each dose of vaccine as compared to that at T1 (Figure 3o, Tables 4 and S4). The ratio of eTregs/rTregs declined markedly at T4 and T5 as compared to that at T1, but only slightly decreased from T4 to T5 (Figure 3p, Tables 4 and S4).
 |
Table 4 Differences in CD4+ T Cells and Tregs Subpopulations at Three Time Points (T1, T4, T5) in Cohort 2 (n = 99, Intervals of 5 Months) |
Neutralizing Antibody Level After the Third Dose of Inactivated COVID-19 Vaccine in Two PLWH Cohorts
The NAb level after the 3rd dose of inactivated COVID-19 vaccine dramatically increased (Both P < 0.001) in both cohort 1 (Figure 4a) and cohort 2 (Figure 4b and Table 5) as compared to that at pre-3rd vaccination time point. Moreover, among 99 PLWH in cohort 2 receiving the 3rd vaccination, the seroconversion rate of SARS-CoV-2-specific NAb was 93.9% (93/99) after one month, while it only reached 60.6% (40/66) at two months after the 3rd dose of inactivated COVID-19 vaccine in cohort 1 (Table 6).
 |
Table 5 Differences in Neutralizing Antibody Level Between Pre-3rd Vaccination and Post-3rd Vaccination in Cohort 1 and Cohort 2 |
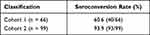 |
Table 6 Seroconversion Rate of Neutralizing Antibody at Post-3rd Vaccination in Cohort 1 and Cohort 2 |
 |
Figure 4 Neutralizing antibody responses to the third dose of inactivated COVID-19 vaccine in cohort 1 (a) and cohort 2 (b). *** P < 0.001. |
Associations of CD4+ T-Cells and Tregs Subpopulations with SARS-CoV-2‐specific Neutralizing Antibody Level in PLWH
The relationships of CD4+ T-cells and Tregs subpopulations with serum SARS‐CoV-2 specific NAb level were further evaluated in PLWH. As shown in Table 7, the absolute counts of CD4+ T-cells (r = 0.256, P < 0.001), CD4+CD25HighCD127Low Tregs (r = 0.217, P = 0.005), CD45RA+ rTregs (r = 0.261, P < 0.001), CD45RO+ eTregs (r = 0.233, P = 0.003), and frequency of CD45RA+ rTregs (r = 0.159, P = 0.041) had positive relationships with SARS-CoV-2-specific NAb in the 3rd vaccination timeframe. After the 3rd vaccination, CD4+ T-cells count (r = 0.222, P = 0.004, Figure 5a), CD4+CD25HighCD127Low Tregs count (r = 0.199, P = 0.011, Figure 5b), CD45RA+ rTregs count (r = 0.238, P = 0.002, Figure 5c), CD45RA+ rTregs frequency (r= 0.171, P = 0.028, Figure 5d) and CD45RO+ eTregs count (r = 0.215, P = 0.006, Figure 5e) were positively correlated with SARS-CoV-2-specific NAb level in PLWH (Table 7).
 |
Table 7 Correlation Analysis Between CD4+ T-Cells, Tregs Subpopulations and SARS-CoV-2-Neutralizing Antibody Level |
Discussion
Comprehensive analysis of COVID-19 vaccine-induced immunity is central for the implementation of vaccination strategies. Despite some research on the safety and immune responses with respect to diverse COVID-19 vaccines and different populations, our data were a complement to assess the safety and immunogenicity of three doses of inactivated COVID-19 vaccines in PLWH. This study focused on the dynamic changes in SARS-CoV-2-specific CD4+ T-cells and their subsets after three consecutive doses of inactivated COVID-19 vaccines. This study also analyzed two cohorts with different intervals of vaccination. Moreover, the relationships between humoral and cellular immune response were evaluated, especially for the relationships of SARS-CoV-2-specific CD4+ T-cells and Tregs subpopulations with serum NAb level.
To date, available evidence has demonstrated SARS-CoV-2 vaccine-induced T-cell responses are pivotal for directly attacking and killing virus-infected cells.20,21 Thus, the characterization of CD4+ T-cells subsets responses to inactivated COVID-19 vaccines provides new insights on a potential target for the prevention and treatment of COVID-19. As a complement, we reported the dynamic changes in the CD4+ T-cells and Tregs subpopulations (CD4+CD25HighCD127Low Tregs, CD45RA+ rTregs and CD45RO+ eTregs) to three consecutive doses of inactivated COVID-19 vaccines.9,22 Our results indicated the absolute counts of CD4+ T-cells and Tregs subpopulations increased as compared to the pre-vaccination levels in two cohorts, regardless of if it was after two- or three-dose inactivated COVID-19 vaccination. Accordingly, our results highlighted the importance of inactivated COVID-19 vaccines among PLWH.
Interestingly, despite the similar trend in the absolute counts of CD4+ T-cells subsets, the frequency of CD4+ T-cells subsets were different from each other even in the same cohort, which is probably related to the different rates of increase in the absolute counts. Compared with the pre-3rd vaccination levels, the CD4+ T-cells and subsets increased after the 3rd dose of vaccine in cohort 2, but they reduced in cohort 1. This may be explained as that the blood samples were collected from cohort 1 at two months after the 3rd vaccination, while those in cohort 2 were collected at one month. In fact, the drop of CD4+ T cell count over time was normal, which has been reported in PLWH inoculated with BNT162b2 mRNA vaccine21 and inactivated COVID-19 vaccine (BBIBP-CorV).9 Considering the decreased absolute counts of CD4+ T-cells and Tregs subpopulations at 2 months after the 3rd vaccination, we speculated reasonably that the absolute counts of CD4+ T-cells and Tregs subpopulations reached a peak within 2 months after the 3rd vaccination and then decreased. These data imply the importance of re-vaccination over a period of time in PLWH.
The SARS-CoV-2-specific humoral immune responses were also tested in the term of NAb level and NAb seroconversion rate. The increase in NAb level after the 3rd dose of inactivated COVID-19 vaccine was observed in two cohorts. In a previous study, the 3rd dose of SARS-CoV-2 mRNA vaccine was reported to enhance NAb responses among PLWH in Italy.10 Our findings highlighted the role of inactivated COVID-19 vaccines among PLWH. In one month after the 3rd vaccination, our results showed that the NAb seroconversion in cohort 2 was 93.9% (93/99) (Table 6), which is close to the rate of PLWH vaccinated with inactivated COVID-19 vaccines (Sinopharm Inactivated Whole Virus or SinoVac Inactivated Whole Virus) in Guangzhou (97%).23 Moreover, the gradual reductions in the NAb level and seroconversion rate of NAb were noted over time.24 Broadly speaking, the 3rd dose of inactivated COVID-19 vaccine effectively induced SARS-CoV-2-specific NAb seroconversion (over 60%) in two PLWH cohorts. The above results demonstrated that the 3rd dose of inactivated COVID-19 vaccine could induce a heightened humoral immune response in PLWH including elderly individuals (age >50), which highlights the significance of the 3rd vaccination in PLWH.
There is a lack of guidelines regarding the optimal vaccination interval for inactivated COVID-19 vaccination in PLWH. To our knowledge, only one cross-sectional study revealed a longer interval between the first and second dose (21–28 days or >28 days) was likely to facilitate neutralizing activity.25 Our data fill the knowledge gap concerning immune responses to inactivated COVID-19 vaccines among PLWH with different vaccination intervals.26 In our study, two cohorts with different inoculation intervals between the second and third dose all had elevated cellular immune responses to two doses or three doses of vaccines as compared to that at baseline, and enhanced humoral immune responses to the 3rd dose, even in elderly PLWH.
Furthermore, our study was a complement to the factors associated with SARS-CoV-2-specific NAb level after COVID-19 vaccination. Our findings not only confirmed the correlation between CD4+ T-cells and NAb level previously reported,27,28 but also revealed the relationship between Tregs subpopulations and NAb level in PLWH. These results imply that the absolute counts of CD4+ T-cells, CD4+CD25HighCD127Low Tregs, CD45RA+ rTregs, and CD45RO+ eTregs may serve as important factors for predicting the outcome of SARS-CoV-2-specific NAb in PLWH after three doses of inactivated COVID-19 vaccine. Of note, the memory Treg cells (CD45RO+) are considered as an independent predictor for NAb level after two-dose COVID-19 vaccination among other population, which further favors the practical significance of characterization of Tregs subpopulations.14 However, the exact role of Tregs in the effective production of NAb remains unknown and warranted to be investigated in more studies.
This study has several limitations. First, it was a single-center study with limited sample size. Nevertheless, most PLWH in Zhejiang Province were vaccinated with the COVID-19 vaccines at Hangzhou Xixi Hospital, which is the largest AIDS designated hospital in Zhejiang Province. Second, although the inactivated COVID-19 vaccine induced NAb responses in the most PLWH, whether this could protect against SARS-CoV-2 variants infection in the real-world remains unknown. In addition, there were no appropriately matched healthy controls in this study. The vaccination program was relatively delayed for PLWH compared with healthy controls in China’s Zhejiang Province, and therefore it is difficult for us to recruit appropriately matched healthy controls. Finally, the fourth collection of blood from cohort 1 should be at one month after the third dose of inactivated COVID-19 vaccine. However, the time of blood collection was delayed by one month in cohort 1 due to the COVID-19 epidemic.
Conclusions
In summary, the safety and efficacy of three consecutive doses of inactivated COVID-19 vaccines were investigated in two PLWH cohorts with different inoculation intervals. Our study indicates three doses of inactivated COVID-19 vaccines are safe enough among PLWH, and can induce the responses of CD4+ T-cells and Tregs subpopulations. On the other hand, the NAb responses are also enhanced after the 3rd dose of inactivated COVID-19 vaccine, which is also associated with CD4+ T-cells and Tregs subpopulations.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
This research was reviewed and approved by the Clinical Research Ethics Committee of the Hangzhou Xixi Hospital (202109131211000115379) in accordance with the tenets of the Declaration of Helsinki. All donors provided written informed consent. All samples were anonymized before use.
Acknowledgments
We appreciate Zhejiang Provincial Center for Disease Control and Prevention for their assistance with this study. We appreciate the Hangzhou ADICON Clinical Laboratories Co., Ltd. for assistance in detecting SARS-CoV-2-specific T-cell responses to vaccination.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by the Infectious Diseases of Hangzhou Medical Key Subject, Key Programs of Hangzhou Bureau of Science and Technology (No. 202204A02), Hangzhou Biomedicine and Health Industry Development Project (No. 2021WJCY367 and 2022WJC174), Guidance Programs of Hangzhou Bureau of Science and Technology (No. 20211231Y050), Medical Science and Technology Project of Hangzhou (No. A20210014) and Medical Science and Technology Project of Zhejiang Province (No. 2023KY196 and 2023KY978).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021;19(3):141–154.
2. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Medica. 2020;91(1):157–160. doi:10.23750/abm.v91i1.9397
3. Abdelmaksoud A, Wollina U, Temiz SA, Hasan A. SARS-CoV-2 vaccination-induced cutaneous vasculitis: report of two new cases and literature review. Dermatol Ther. 2022;35(6):e15458. doi:10.1111/dth.15458
4. Dotiwala F, Upadhyay AK. A comprehensive review of BBV152 vaccine development, effectiveness, safety, challenges, and prospects. Front Immunol. 2022;13:940715. doi:10.3389/fimmu.2022.940715
5. Bert F, Pivi A, Russotto A, et al. COVID-19 vaccination among HIV+ patients: an Italian cross-sectional survey. Vaccines. 2022;10:9. doi:10.3390/vaccines10091438
6. British HIV Association. Comment from BHIVA and THT on UK Government guidance on coronavirus (COVID-19), social distancing to protect vulnerable adults and shielding to protect extremely vulnerable adults; 2020. Available from: https://www.bhiva.org/comment-from-BHIVA-and-THT-on-UK-Government-guidance-on-Coronavirus-COVID-19.
7. Krammer F. A correlate of protection for SARS-CoV-2 vaccines is urgently needed. Nat Med. 2021;27(7):1147–1148. doi:10.1038/s41591-021-01432-4
8. Dapporto F, Marchi S, Leonardi M, et al. Antibody avidity and neutralizing response against SARS-CoV-2 omicron variant after infection or vaccination. J Immunol Res. 2022;2022:4813199. doi:10.1155/2022/4813199
9. Feng Y, Zhang Y, He Z, et al. Immunogenicity of an inactivated SARS-CoV-2 vaccine in people living with HIV-1: a non-randomized cohort study. EClinicalMedicine. 2022;43:101226. doi:10.1016/j.eclinm.2021.101226
10. Vergori A, Cozzi Lepri A, Cicalini S, et al. Immunogenicity to COVID-19 mRNA vaccine third dose in people living with HIV. Nat Commun. 2022;13(1):4922. doi:10.1038/s41467-022-32263-7
11. Painter MM, Mathew D, Goel RR, et al. Rapid induction of antigen-specific CD4(+) T cells is associated with coordinated humoral and cellular immunity to SARS-CoV-2 mRNA vaccination. Immunity. 2021;54(9):2133–2142 e3. doi:10.1016/j.immuni.2021.08.001
12. Wang Y, Zheng J, Islam MS, Yang Y, Hu Y, Chen X. The role of CD4(+)FoxP3(+) regulatory T cells in the immunopathogenesis of COVID-19: implications for treatment. Int J Biol Sci. 2021;17(6):1507–1520. doi:10.7150/ijbs.59534
13. Uraki R, Imai M, Ito M, et al. Foxp3+ CD4+ regulatory T cells control dendritic cells in inducing antigen-specific immunity to emerging SARS-CoV-2 antigens. PLoS Pathog. 2021;17(12):e1010085. doi:10.1371/journal.ppat.1010085
14. Huang WT, Weng SW, Tzeng HT, Yen FC, Chiang YS, You HL. Lymphocyte subpopulations associated with neutralizing antibody levels of SARS-CoV-2 for COVID-19 vaccination. Vaccines. 2022;10(9):1550. doi:10.3390/vaccines10091550
15. Faissner S, Heitmann N, Plaza-Sirvent C, et al. Immune response in ofatumumab treated multiple sclerosis patients after SARS-CoV-2 vaccination. Front Immunol. 2022;13:980526. doi:10.3389/fimmu.2022.980526
16. Yao Y, Wang ZZ, Huang A, et al. TFH 2 cells associate with enhanced humoral immunity to SARS-CoV-2 inactivated vaccine in patients with allergic rhinitis. Clin Transl Med. 2022;12(1):e717. doi:10.1002/ctm2.717
17. National Medical Products Administrations. NMPA issued the guidelines for adverse event classification standards for clinical trials of preventive vaccines; 2019. Available from: https://www.nmpa.gov.cn/xxgk/ggtg/qtggtg/20191231111901460.html.
18. Kaneko Y, Sugiyama A, Tanaka T, et al. The serological diversity of serum IgG/IgA/IgM against SARS-CoV-2 nucleoprotein, spike, and receptor-binding domain and neutralizing antibodies in patients with COVID-19 in Japan. Health Sci Rep. 2022;5(3):e572. doi:10.1002/hsr2.572
19. Zhang J, Xing S, Liang D, et al. Differential antibody response to inactivated COVID-19 vaccines in healthy subjects. Front Cell Infect Microbiol. 2021;16(11):791660. doi:10.3389/fcimb.2021.791660
20. Grifoni A, Weiskopf D, Ramirez SI, et al. Targets of T cell responses to SARS-CoV-2 coronavirus in humans with COVID-19 disease and unexposed individuals. Cell. 2020;181(7):1489–1501. doi:10.1016/j.cell.2020.05.015
21. Bai J, Chiba A, Murayama G, Kuga T, Tamura N, Miyake S. Sex, age, and ethnic background shape adaptive immune responses induced by the SARS-CoV-2 mRNA vaccine. Front Immunol. 2022;13:786586. doi:10.3389/fimmu.2022.786586
22. Han X, Yu X, Han Y, et al. Safety and immunogenicity of inactivated COVID-19 vaccines among people living with HIV in China. Infect Drug Resist. 2022;15:2091–2100. doi:10.2147/IDR.S353127
23. Cai S, Liao G, Yu T, et al. Immunogenicity and safety of an inactivated SARS-CoV-2 vaccine in people living with HIV: a cross-sectional study. J Med Virol. 2022;94(9):4224–4233. doi:10.1002/jmv.27872
24. Zou S, Guo W, Wu S, et al. Six-month humoral immune response to inactivated COVID-19 vaccine among people living with HIV. Front Immunol. 2022;13:988304. doi:10.3389/fimmu.2022.988304
25. Huang X, Yan Y, Su B, et al. Comparing immune responses to inactivated vaccines against SARS-CoV-2 between people living with HIV and HIV-negative individuals: a cross-sectional study in China. Viruses. 2022;14(2):277. doi:10.3390/v14020277
26. Yin J, Chen Y, Li Y, Wang C, Zhang X. Immunogenicity and efficacy of COVID-19 vaccines in people living with HIV: a systematic review and meta-analysis. Int J Infect Dis. 2022;124:212–223. doi:10.1016/j.ijid.2022.10.005
27. Antinori A, Cicalini S, Meschi S, et al. Humoral and cellular immune response elicited by mRNA vaccination against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in people living with human immunodeficiency virus receiving antiretroviral therapy based on current CD4 T-lymphocyte count. Clin Infect Dis. 2022;75(1):e552–e563. doi:10.1093/cid/ciac238
28. Rydyznski Moderbacher C, Kim C, Mateus J, et al. NVX-CoV2373 vaccination induces functional SARS-CoV-2-specific CD4+ and CD8+ T cell responses. J Clin Invest. 2022;132(19):e160898. doi:10.1172/JCI160898
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



