Back to Journals » Journal of Inflammation Research » Volume 15
Dynamic Status of SII and SIRI Alters the Risk of Cardiovascular Diseases: Evidence from Kailuan Cohort Study
Authors Li J, He D, Yu J, Chen S, Wu Q, Cheng Z, Wei Q, Xu Y, Zhu Y, Wu S
Received 2 July 2022
Accepted for publication 18 October 2022
Published 21 October 2022 Volume 2022:15 Pages 5945—5957
DOI https://doi.org/10.2147/JIR.S378309
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Jun Li,1,* Di He,1,* Jiazhou Yu,2,* Shuohua Chen,3 Qiong Wu,1 Zongxue Cheng,1 Qiaohui Wei,1 Yuying Xu,1 Yimin Zhu,1,4 Shouling Wu3
1Department of Epidemiology & Biostatistics and Department of Respiratory Diseases of Sir Run Run Shaw Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China; 2Jockey Club School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong Special Administrative Region, People’s Republic of China; 3Department of Cardiology, Kailuan General Hospital, Tangshan, People’s Republic of China; 4Cancer Center, Zhejiang University, Hangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Shouling Wu, Department of Cardiology, Kailuan General Hospital, 57 Xinhua East Road, Tangshan, People’s Republic of China, Email [email protected] Yimin Zhu, Department of Respiratory Diseases, Sir Run Run Shaw Hospital Affiliated to School of Medicine, Zhejiang University, Hangzhou, Zhejiang, 310020, People’s Republic of China, Email [email protected]
Background: Two novel systemic inflammation indices, SII and SIRI, are associated with increased risk of cardiovascular diseases (CVD). However, SII and SIRI are prone to change over time and the association between changeable status and long-term outcome risk remains to be uncovered. This study aims to examine the association between the dynamic status of SII and SIRI and risk of CVD.
Methods: This prospective study included a total of 45,809 subjects without MI, stroke and cancer prior to or in 2010 (baseline of this study). The dynamic status of SII and SIRI during 2006, 2008, and 2010 was assessed by dynamic trajectories (primary exposure), annual increase, and average value. The outcome was CVD incidence during 8.6 years’ follow-up. Multiple Cox regression models were used to calculate the adjusted hazard ratios (HRs) and confidence intervals (95% CIs).
Results: Four dynamic trajectories of SII and SIRI were identified as follows: low stable pattern, moderate stable pattern, increase pattern, and decrease pattern. For SII, compared with “low stable pattern”, after controlling confounders and level of SII in 2006, adjusted HRs were 1.24 (95% CI = 1.02– 1.51) for “increase pattern” and 1.11 (95% CI = 1.00– 1.23) for “moderate-stable pattern” while the association was not significant for “decrease pattern”. Additionally, the highest group of annual SII increase and average SII had respective HR of 1.20 (95% CI = 1.05– 1.37) and 1.32 (95% CI = 1.13– 1.55). The results were consistent for SIRI. “Increase pattern” and “moderate stable pattern” increased the risk of CVD by 38% (HR = 1.38, 95% CI = 1.17– 1.63) and 12% (HR = 1.12, 95% CI = 1.01– 1.25), while no significant association was found for “decrease pattern”. The highest group of annual SIRI increase and average SIRI had respective HR of 1.25 (95% CI = 1.09– 1.44) and 1.39 (95% CI = 1.19– 1.63).
Conclusion: Dynamic status of SII and SIRI was significantly associated with risk of CVD, which highlighted that we should focus on the dynamic change of SII and SIRI.
Keywords: systemic inflammation, dynamic status, prospective study, cardiovascular diseases
Introduction
Globally, cardiovascular diseases (CVD) are the major cause of mortality and the first-leading cause of disability-adjusted life-years (DALYs) in 2019.1,2 In China, CVD account for 40% of the total deaths in 2019, responsible for approximately 4.58 million CVD deaths.3–5 The development of CVD may be attributable to key events such as loss of homeostasis, acidosis, increased intracellular calcium levels, and excitotoxicity.6,7 Previous studies have suggested that chronic low-grade inflammation is a significant contributing factor in the pathogenesis of CVD.8,9 The biomarkers of chronic low-grade inflammation including peripheral platelet, neutrophil, lymphocyte and monocyte10–12 and the indices of chronic low-grade inflammation, constructed based on these inflammatory biomarkers, such as neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR) and lymphocyte-to-monocyte ratio (LMR),13–16 were associated with increased risk of CVD.
Recently, two novel inflammatory indices, which composed of platelet and three subtypes of white blood cell, systemic immune inflammation index (SII)17 and systemic inflammation response index (SIRI),18 were found to have a better predictive value in the prognosis of CVD than other inflammatory biomarkers or indices.19–22 Most studies exploring the effect of SII and SIRI focused on the association between the indices at baseline and CVD.20,21 However, the inflammatory indices may change during the progression of CVD.23,24 Therefore, a single measurement of SII and SIRI at baseline cannot truly represent the whole exposure. To our knowledge, the association between dynamic status of SII and SIRI and the risk of CVD remains to be uncovered. Examining the dynamic change over time and its impact on the risk of CVD may provide imperative evidence to better understand the mechanism of previous identified association.
Hence, this prospective cohort study aims to examine the association between the dynamic status of SII and SIRI and the risk of CVD.
Methods
Study Population
The Kailuan cohort study was a prospective population-based study conducted in Tangshan City, Hebei province, China. The details of this cohort study have been described elsewhere.25,26 In brief, a total of 101,510 participants (81,110 men and 20,400 women) who were currently working or retired employees of the Kailuan Group were recruited. From June 2006, all participants were required to complete biennial health examinations, including health questionnaire, anthropometric measurement, and biochemical tests. In this study, results of the first three health examinations (2006–2010) were used to construct the dynamic status of SII and SIRI and after the third health examination, we followed up subjects to observe whether they were diagnosed with CVD.
Subjects were excluded in the analysis if they met any criteria below in the first three health examinations: 1) absent in the second or third health examinations; 2) with missing SII, SIRI; 3) with SII>1000 or SIRI>3 (to exclude acute inflammatory conditions); 4) with acute inflammation-related disease; 5) diagnosed with myocardial infarction, stroke or cancer. Finally, a total of 45,809 subjects were remained in the analysis (Figure 1). The study was approved by the Zhejiang University, School of Medicine and the Ethics Committee of Kailuan General Hospital. All participants provided written informed consent. This study was conducted according to the provisions of the Declaration of Helsinki.
 |
Figure 1 Flowchart of the study population selection. Abbreviations: SII, systemic inflammation index; SIRI, systemic inflammation response index. |
Data Collection and Assessment
Demographic data were collected using a standard structured questionnaire. Variables included age, gender, educational level (high school, above high school), monthly income level (≤800 ¥/month, >800 ¥/month), smoking status (never, ever smoking), drinking status (never, ever drinking), physical activity status (inactive, active), medication history, history of type 2 diabetes and hypertension, and family history of cardiovascular disease. Ever smoking/drinking was defined as past or current smoking/drinking. Participants who reported taking part in moderate and vigorous physical activities less than once a week were classified as inactive in physical activity, and otherwise as active in physical activity.
Anthropometric data were measured by trained investigators following standard procedures, as previously described.25,26 Variables included height, weight, waist circumference (WC), and blood pressure (BP). Height and weight were measured with the subjects wearing light clothing and no shoes. Body mass index (BMI) was calculated by weight (kg) divided by the square of height (m2). WC was measured at midpoint of lowest rib and iliac crest. BP was measured twice in the sitting position by a mercury sphygmomanometer, with a third measurement taken if the difference between the two measurements was more than 5 mmHg, and the average of all measurements was used for analysis.
Biochemical data were collected from each subject after a 12-h overnight fast by using an auto-analyzer (Hitachi 747, Tokyo, Japan). Variables included total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and fasting blood glucose (FBG). TC, TG, HDL-C, and LDL-C were measured by the enzymatic colorimetric method. FBG was determined by the hexokinase/glucose-6-phosphate dehydrogenase method. Routine blood tests were measured with a full blood count analyzer (Sysmex XT-1800i, Sysmex Corporation), including platelet, neutrophil, lymphocyte, and monocyte counts.
Definition of Dynamic Status of SII and SIRI
SII was calculated by (Peripheral platelet counts × Neutrophil counts)/Lymphocyte counts. SIRI was calculated by (Monocyte counts × Neutrophil counts)/Lymphocyte counts. The dynamic status of SII and SIRI was assessed based on results of the first three health examinations conducted in 2006, 2008, 2010. We used latent mixture modeling within the Proc Traj procedure27,28 to identify the dynamic trajectories of SII and SIRI. The details had been described elsewhere.29,30 Briefly, censored normal model was chosen given that SII and SIRI were continuous variables. We compared the models with different trajectories and different terms. Bayesian information criterion (BIC) was used to assess the fitness of models. Finally, the model with four trajectories and quadratic term was further analysed. Based on the pattern displayed, the four trajectories of SII and SIRI were labelled as “low stable pattern”, “moderate stable pattern”, “increase pattern”, and “decrease pattern” (Figures 2 and 3).
 |
Figure 2 Dynamic trajectory of SII during 2006–2010. Abbreviation: SII, systemic inflammation index. |
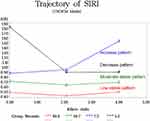 |
Figure 3 Dynamic trajectory of SIRI during 2006–2010. Abbreviation: SIRI, systemic inflammation response index. |
We also composed two additional indicators for SII and SIRI to measure their dynamic status: 1) average value, which was the average of SII/SIRI in 2006, 2008, 2010; 2) annual increase rate, which was defined as the slope of linear regression model where follow-up duration was the independent variable and SII/SIRI in 2006, 2008, 2010 was the dependent variable. Subjects were subsequently divided into four groups according to quartile of annual increase rate and average of SII/SIRI, respectively.
Outcomes Ascertainment and Follow-Up
In the current study, all subjects were followed up after the third examination until the diagnosis of CVD, loss to follow-up, or censoring date (December 31, 2019), whichever happened first. The CVD was defined as the composite of stroke and myocardial infarction (MI). Stroke was diagnosed based on the World Health Organization criteria, which considers clinical symptoms, brain computed tomography, or magnetic resonance imaging.31 MI was diagnosed based on the combinations of chest pain symptoms, electrocardiogram changes, and cardiac enzyme levels.32 All outcome data were obtained from 11 local hospitals and Municipal Social Insurance Institution. The diagnostic records were reviewed by an expert panel of three cardiologists to ensure the accuracy.
Statistical Analysis
Continuous variables with normal distribution are described as mean (standard deviation), otherwise described as median (interquartile range). Categorical variables are described as number (percentage). Characteristics of the four dynamic trajectories of SII and SIRI were compared using one-way ANOVA for continuous variables and chi-square test for categorical variables.
Multiple Cox regression was used to estimate the association between the dynamic status of SII, SIRI and risk of CVD. The reference groups were “low stable pattern” of SII, SIRI and Q1 of annual increase rate and average SII, SIRI. Hazard ratios (HRs) were reported with 95% confidence intervals (CIs). To examine the consistency of the results, three models were applied: Model 1 adjusted for age, sex, education level, income level, smoking status, drinking status, physical activity status, family history of cardiovascular disease, and BMI; Model 2 additionally adjusted for hypertension, diabetes mellitus, LDL-C, anti-hypertensive drug use, anti-diabetic drug use, and lipid-lowering drug based on Model 1; Model 3 additionally adjusted for SII or SIRI in 2006 based on Model 2. Sensitivity analysis were conducted to test the robustness of the results: 1) stratified by age (<50 years and ≥50 years); 2) stratified by gender; 3) excluding incident events during the first 2 years of follow-up; 4) excluding subjects with hypo-hyperthyroidism, liver and kidney diseases, hematological diseases during 2006–2010. All statistical analysis were performed by R software version 4.0.2 and SAS version 9.4 (SAS Institute, Inc., Cary, NC). Statistical significance was set at P<0.05.
Result
Baseline Characteristics
A total of 45,809 subjects were included in this study. The mean age was 52.8 years and 75.9% of the participants were male. During the 8.6-year follow-up, 2218 incident CVD cases were identified, including 387 MI cases and 1852 stroke cases. The baseline characteristics of subjects by the trajectory patterns of SII and SIRI were summarised in Tables 1 and 2.
 |
Table 1 Characteristics of Subjects by the Trajectory Patterns of SII in 2010 |
 |
Table 2 Characteristics of Subjects by the Trajectory Patterns of SIRI in 2010 |
Overall, by the trajectory patterns of SII, 56.4% of the subjects were “low-stable pattern”, 31.8% were “moderate-stable pattern”, 6.9% were “increase pattern”, and 4.8% were “decrease pattern”. For SIRI, the percentages were 46.6%, 40.7%, 7.3%, and 5.3%, respectively. Subject characteristics showed significant differences in age, sex, education level, income level, smoking and drinking behaviors, physical activity, BMI, WC, SBP, DBP, FBG, and LDL-C between four trajectory patterns of SII and SIRI (p<0.05). To explore the consistency of subject characteristics over years, the characteristics measured in 2006 were also presented in Supplementary Tables 1 and 2. For lifestyles, the percentage of ever smokers and ever drinkers decreased and the percentage of active physical activity increased among four trajectory patterns of SII and SIRI from 2006 to 2010. For metabolic components, the means of SBP, DBP, WC, FBG, LDL-C increased and there was no significant change in the distribution of BMI during the 4 years.
Associations Between the Dynamic Status of SII, SIRI and CVD
The effects of different dynamic trajectories of SII and SIRI on CVD are summarised in Table 3. For SII, compared with “low stable pattern”, after controlling confounders and level of SII in 2006, adjusted HRs were 1.24 (95% CI = 1.02–1.51) for “increase pattern” and 1.11 (95% CI = 1.00–1.23) for “moderate-stable pattern” while the association was not significant for “decrease pattern” (HR = 1.03, 95% CI = 0.78–1.36). The results were consistent for SIRI. Compared with “low stable pattern”, after controlling the confounding factors and SIRI level in 2006, “increase pattern” and “moderate stable pattern” increased the risk of CVD by 38% (HR=1.38, 95% CI=1.17–1.63) and 12% (HR=1.12, 95% CI=1.01–1.25) while no significant association was found for “decrease pattern” (HR=0.88, 95% CI=0.65–1.19). The Kaplan–Meier cumulative incidence curves of CVD by the dynamic trajectories of SII and SIRI were show in the Figures 4 and 5. Significant difference of cumulative incidence curves were found for CVD among four dynamic trajectories of SII and SIRI (Log rank P < 0.01).
 |
Table 3 Incidence Rates and Risks of the Cardiovascular Disease by the Trajectory Patterns of SII and SIRI |
 |
Figure 4 Kaplan-Meier cumulative incidence curves of CVD for the dynamic patterns of SII. Abbreviation: SII, systemic inflammation index. |
 |
Figure 5 Kaplan-Meier cumulative incidence curves of CVD for the dynamic patterns of SIRI. Abbreviation: SIRI, systemic inflammation response index. |
The average of SII and SIRI and the annual increase of SII and SIRI were also calculated to further assess the association between the dynamic status of two indices and the risk of CVD, which are summarised in Tables 4 and 5. For SII, compared with the Q1 group, after controlling confounders and level of SII in 2006, HRs for Q4 group of annual increase rate and Q4 group of average SII were 1.20 (95% CI=1.05–1.37) and 1.32 (95% CI=1.13–1.55), respectively. Similarly, for SIRI, compared with the Q1 group, after controlling confounders and level of SIRI in 2006, Q4 group of annual increase rate showed a HR of 1.25 (95% CI=1.09–1.44) and Q4 group of average SIRI showed an HR of 1.39 (95% CI=1.19–1.63).
 |
Table 4 Incidence Rates and Risks of the Cardiovascular Disease by Quartiles of Annual SII Increase and Quartiles of Average SII |
 |
Table 5 Incidence Rates and Risks of the Cardiovascular Disease by Quartiles of Annual SIRI Increase and Quartiles of Average SIRI |
The analysis of two subtypes of CVD was summarised in Supplemental Tables 3–6. The results were similar for stroke. The “increase pattern” and “moderate pattern” of SII and SIRI increased the risk of stroke while no significant association was found in “decrease pattern”. Additionally, the highest group of annual increase and average of SII and SIRI displayed the significant higher risk of stroke. However, for MI, whichever method of assessing the dynamic status, the associations were no significant.
Sensitivity Analysis
After excluding the incident events during the first 2 years of follow-up, the marginal significant results were found for SII and SIRI (Supplemental Tables 7 and 8). Subgroup analysis by age also documented marginal association of SII and SIRI. When stratified by gender, the consistent results were found with the original analysis in males. The association between the dynamic trajectory of SII and SIRI and risks of cardiovascular disease became nonsignificant for females. After excluding subjects with hypo-hyperthyroidism, liver and kidney diseases and hematological diseases during 2006–2010, the results were consistent for SII and SIRI (Supplemental Tables 9 and 10).
Discussion
In this large prospective study, we examined the association between dynamic status of two systemic inflammatory indices, SII and SIRI, and risk of CVD. We had identified four different trajectory patterns of SII and SIRI, which were “low stable pattern”, “moderate stable pattern”, “increase pattern” and “decrease pattern”. For both indices, compared with “low stable pattern”, “moderate stable pattern” and “increase pattern” significantly increased the risk of CVD, while no significant difference was noted for “decrease pattern”. The analysis of two additional indicators suggested that annual increase rate and average of SII and SIRI were positively associated with risk of CVD.
The association between SII and SIRI at baseline and risk of CVD had been previously examined.33–35 For example, Aydin et al found that higher SII level would increase the risk of stroke.33 Jin et al concluded that higher SII and SIRI were associated with higher risk of developing CVD during a median follow-up period of 10 years.34 A cohort study with a median follow-up of 8.28 years found that higher SII was associated with higher risk of stroke and coronary heart disease among middle-aged and elderly Chinese adults.35 However, these studies only focused on the SII and SIRI at baseline without considering their possible dynamic change during the follow-up. In our study, SII showed an increasing pattern in 6.9% of the subjects and a decreasing pattern in 4.8% of the subjects over a 4-year period. Similarly, SIRI had increased in 7.3% of the subjects and decreased in 5.3% of the subjects, which revealed that two indices were prone to change during the follow-up. Hence, bias may exist when results were generated from baseline indices only.
Our study explored the association between the dynamic status, which assessed by dynamic trajectory, annual increase and average value, of two indices and risk of CVD. We found that the risk of CVD was significantly higher among subjects whose SII and SIRI were maintained at a moderate level and subjects with high average SII and SIRI. Moreover, we noted that subjects who showed an increasing pattern of SII and SIRI had considerably higher risk of stroke, and this was supported by the finding of increased risk for high annual increase rate, while subjects with reduced SII and SIRI had better outcome. These results suggested that the risk of CVD was not only associated with the high overall level but also the increasing trend of SII and SIRI. Analysing the dynamic status of SII and SIRI may provide additional information in risk assessment of CVD. Individuals whose SII and SIRI maintained at a high level or showed an increasing trend over time should be timely identified and offered early intervention to improve the clinical outcomes.
As SII and SIRI were composed based on the inflammation cells, including neutrophil, monocyte, lymphocyte, platelet, the dynamic change of SII and SIRI may be attributed to the dynamic changes of these inflammation cells, which probably involved in the pathological process of CVD.36–39 In the early stage of atherosclerosis inflammatory response, neutrophils can extreme release of enzymes with hydrolytic properties and proinflammatory agents and be able to produce protease MMP-9, which could damage the basal lamina and harm the brain tissue causing CVD.36 In atherosclerosis, apolipoprotein B-lipoproteins accumulated in the matrix beneath the endothelial cell layer of blood vessels, which led to the recruitment of monocytes. Derived from these recruited monocytes, macrophages were involved in a maladaptive inflammatory response that enlarged the subendothelial layer due to accumulation of cells, lipids, and matrix. Some lesions subsequently form a necrotic core, triggering CVD.37–39 Platelets, adhere to subendothelial components, were activated and released a variety of mediators that allow new platelets to aggregate. At the same time, thrombin was produced on the platelet surface and enhanced the phenomenon. Arterial thrombosis consisted primarily of platelets with low fibrin content, as high blood flow avoids localized thrombin accumulation. Mural artery thrombosis may embolize, incorporate into the vessel wall, or obstruct the arterial lumen.40–42 Conversely, lymphocytes can probably regulate inflammation response and exert the inhibitory effect on atherosclerosis.43 Thus, higher SII and SIRI value could activate the immune and inflammatory response in humans, which could lead to the poor outcomes. Several evidence have found that SII and SIRI have a higher predictive value than other inflammatory biomarkers and indices in predicting cardiovascular events.21,44 Candemir et al found that SII was a risk factor for atherosclerosis and compared with ratios such as the NLR, MLR, and PLR, SII might be a better predictor for coronary artery lesion severity.44 Zhang et al concluded that outperformed NLR, PLR, LMR, and RDW in predictive power, SIRI was a promising low-grade inflammatory indicator for predicting stroke prognosis.21 Based on routine measurements of blood cells counts in clinical setting, SII and SIRI were both noninvasive and easily accessible approaches, which may become promising tools for predicting cardiovascular events in the future clinical practice.
Another notable finding of this study was that the association was found to be significant for stroke but not MI. The results of several previous studies remained unconcluded.34,35 SII and SIRI at baseline were associated with risk of both stroke and MI,34 while another study found that a significant association was found in stroke but not MI.35 One possible explanation was that bias may exist when results were generated from baseline indices or the low incidence of MI in our study undermined the statistical power in examining the relationship between SII and SIRI and MI. Future studies were needed to confirm this finding. Subgroup analysis by gender showed that significant association was found in males but not females. Most subjects were males, therefore the relatively smaller sample size in female subjects may be a likely reason. Much efforts need to be conducted to explain the results.
Strengths and Limitations
The major strengths of this study are the large prospective cohort and long follow-up period. This study has provided novel evidence on the association between SII, SIRI and risk of CVD by focusing on the dynamic change of indices over time. To the best of our knowledge, this is the first study to investigate the association between dynamic status of SII and SIRI and risk of CVD.
There are also several limitations in our study. First, due to the subjects were recruited from the currently working or retired employees of the Kailuan Group, approximately 80% subjects were males, which may restrict the generalization of results. Second, the dynamic status of SII and SIRI was measured based on the first three health examination, which only reflected the change over 4 years. Future studies may consider extending the assessment period for better precision. Third, although the analysis adjusted the impact of various confounding factors, other unmeasured variables such as genetic susceptibility might exist and influence our results.
Conclusion
In conclusion, dynamic status of SIRI and SII were significantly associated with risk of CVD. Our findings highlight that we should focus on the dynamic change of SII and SIRI.
Acknowledgments
The authors also would like to thank all the participants and investigators that took part in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Roth GA, Mensah GA, Johnson CO, et al.; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021. doi:10.1016/j.jacc.2020.11.010
2. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/S0140-6736(20)30925-9
3. Wang W, Liu Y, Ye P, et al. Trends and associated factors in place of death among individuals with cardiovascular disease in China, 2008–2020: a population-based study. Lancet Reg Health West Pac. 2022;21:100383. doi:10.1016/j.lanwpc.2022.100383
4. Du X, Patel A, Anderson CS, Dong J, Ma C. Epidemiology of cardiovascular disease in China and opportunities for improvement: JACC international. J Am Coll Cardiol. 2019;73(24):3135–3147. doi:10.1016/j.jacc.2019.04.036
5. Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16(4):203–212. doi:10.1038/s41569-018-0119-4
6. Kuriakose D, Xiao Z. Pathophysiology and treatment of stroke: present status and future perspectives. Int J Mol Sci. 2020;21(20):7609. doi:10.3390/ijms21207609
7. Tibaut M, Mekis D, Petrovic D. Pathophysiology of myocardial infarction and acute management strategies. Cardiovasc Hematol Agents Med Chem. 2017;14(3):150–159. doi:10.2174/1871525714666161216100553
8. Donath MY, Meier DT, Böni-Schnetzler M. Inflammation in the pathophysiology and therapy of cardiometabolic disease. Endocr Rev. 2019;40(4):1080–1091. doi:10.1210/er.2019-00002
9. van Hout GP, Bosch L. The inflammasomes in cardiovascular disease. Exp Suppl. 2018;108:9–40. doi:10.1007/978-3-319-89390-7_2
10. Willoughby S, Holmes A, Loscalzo J. Platelets and cardiovascular disease. Eur J Cardiovasc Nurs. 2002;1(4):273–288. doi:10.1016/s1474-5151(02)00038-5
11. Pinto EM, Huppert FA, Morgan K, et al. Neutrophil counts, monocyte counts and cardiovascular disease in the elderly. Exp Gerontol. 2004;39(4):615–619. doi:10.1016/j.exger.2003.12.011
12. Núñez J, Miñana G, Bodí V, et al. Low lymphocyte count and cardiovascular diseases. Curr Med Chem. 2011;18(21):3226–3233. doi:10.2174/092986711796391633
13. Kim S, Eliot M, Koestler DC, Wu WC, Kelsey KT. Association of neutrophil-to-lymphocyte ratio with mortality and cardiovascular disease in the Jackson Heart Study and modification by the Duffy antigen variant. JAMA Cardiol. 2018;3(6):455–462. doi:10.1001/jamacardio.2018.1042
14. Kurtul A, Ornek E. Platelet to lymphocyte ratio in cardiovascular diseases: a systematic review. Angiology. 2019;70(9):802–818. doi:10.1177/0003319719845186
15. Wu L, Zou S, Wang C, Tan X, Yu M. Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratio in Chinese Han population from Chaoshan region in South China. BMC Cardiovasc Disord. 2019;19(1):125. doi:10.1186/s12872-019-1110-7
16. Ren H, Liu X, Wang L, Gao Y. Lymphocyte-to-monocyte ratio: a novel predictor of the prognosis of acute ischemic stroke. J Stroke Cerebrovasc Dis. 2017;26(11):2595–2602. doi:10.1016/j.jstrokecerebrovasdis.2017.06.019
17. Hu B, Yang XR, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20(23):6212–6222. doi:10.1158/1078-0432.CCR-14-0442
18. Qi Q, Zhuang L, Shen Y, et al. A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer. 2016;122(14):2158–2167. doi:10.1002/cncr.30057
19. Yang YL, Wu CH, Hsu PF, et al. Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. Eur J Clin Invest. 2020;50(5):e13230. doi:10.1111/eci.13230
20. Li LH, Chen CT, Chang YC, Chen YJ, Lee IH, How CK. Prognostic role of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and systemic immune inflammation index in acute ischemic stroke: a STROBE-compliant retrospective study. Medicine. 2021;100(25):e26354. doi:10.1097/MD.0000000000026354
21. Zhang Y, Xing Z, Zhou K, Jiang S. The predictive role of Systemic Inflammation Response Index (SIRI) in the prognosis of stroke patients. Clin Interv Aging. 2021;16:1997–2007. doi:10.2147/CIA.S339221
22. Jin Z, Hao D, Song Y, Zhuang L, Wang Q, Yu X. Systemic inflammatory response index as an independent risk factor for ischemic stroke in patients with rheumatoid arthritis: a retrospective study based on propensity score matching. Clin Rheumatol. 2021;40(10):3919–3927. doi:10.1007/s10067-021-05762-z
23. Gelderblom M, Leypoldt F, Steinbach K, et al. Temporal and spatial dynamics of cerebral immune cell accumulation in stroke. Stroke. 2009;40(5):1849–1857. doi:10.1161/STROKEAHA.108.534503
24. Lelekov-Boissard T, Chapuisat G, Boissel JP, Grenier E, Dronne MA. Exploration of beneficial and deleterious effects of inflammation in stroke: dynamics of inflammation cells. Philos Trans A Math Phys Eng Sci. 2009;367(1908):4699–4716. doi:10.1098/rsta.2009.0184
25. Dai L, Song L, Li X, et al. Association of visit-to-visit blood pressure variability with the risk of all-cause mortality and cardiovascular events in general population. J Clin Hypertens. 2018;20(2):280–288. doi:10.1111/jch.13192
26. Liu X, Cui L, Wang A, et al. Cumulative exposure to ideal cardiovascular health and incident diabetes in a Chinese population: the Kailuan study. J Am Heart Assoc. 2016;5(9):e004132. doi:10.1161/JAHA.116.004132
27. Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29:374–393. doi:10.1177/0049124101029003005
28. Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol Methods Res. 2007;35:542–571. doi:10.1177/0049124106292364
29. Jin C, Chen S, Vaidya A, et al. Longitudinal change in fasting blood glucose and myocardial infarction risk in a population without diabetes. Diabetes Care. 2017;40(11):1565–1572. doi:10.2337/dc17-0610
30. Wu S, An S, Li W, et al. Association of trajectory of cardiovascular health score and incident cardiovascular disease. JAMA Netw Open. 2019;2(5):e194758. doi:10.1001/jamanetworkopen.2019.4758
31. WHO Task Force. Stroke--1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO task force on stroke and other cerebrovascular disorders. Stroke. 1989;20(10):1407–1431. doi:10.1161/01.str.20.10.1407
32. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018;72(18):2231–2264. doi:10.1016/j.jacc.2018.08.1038
33. Aydin C, Alpsoy Ş, Akyüz A, et al. Could the systemic immune-inflammation index be a predictor to estimate cerebrovascular events in hypertensive patients? Blood Press Monit. 2022;27(1):33–38. doi:10.1097/MBP.0000000000000560
34. Jin Z, Wu Q, Chen S, et al. The associations of two novel inflammation indexes, SII and SIRI with the risks for cardiovascular diseases and all-cause mortality: a ten-year follow-up study in 85,154 individuals. J Inflamm Res. 2021;14:131–140. doi:10.2147/JIR.S283835
35. Xu M, Chen R, Liu L, et al. Systemic immune-inflammation index and incident cardiovascular diseases among middle-aged and elderly Chinese adults: the Dongfeng-Tongji cohort study. Atherosclerosis. 2021;323:20–29. doi:10.1016/j.atherosclerosis.2021.02.012
36. Maida CD, Norrito RL, Daidone M, Tuttolomondo A, Pinto A. Neuroinflammatory mechanisms in ischemic stroke: focus on cardioembolic stroke, background, and therapeutic approaches. Int J Mol Sci. 2020;21(18):6454. doi:10.3390/ijms21186454
37. Honold L, Nahrendorf M. Resident and monocyte-derived macrophages in cardiovascular disease. Circ Res. 2018;122(1):113–127. doi:10.1161/CIRCRESAHA.117.311071
38. Moore KJ, Sheedy FJ, Fisher EA. Macrophages in atherosclerosis: a dynamic balance. Nat Rev Immunol. 2013;13(10):709–721. doi:10.1038/nri3520
39. Moore KJ, Tabas I. Macrophages in the pathogenesis of atherosclerosis. Cell. 2011;145(3):341–355. doi:10.1016/j.cell.2011.04.005
40. Boneu B. Rôle des plaquettes dans l’athérosclérose et la thrombose artérielle [Role of platelets in atherosclerosis and arterial thrombosis]. Rev Prat. 1989;39(25):2215–2218. French.
41. Khodadi E. Platelet function in cardiovascular disease: activation of molecules and activation by molecules. Cardiovasc Toxicol. 2020;20(1):1–10. doi:10.1007/s12012-019-09555-4
42. Papapanagiotou A, Daskalakis G, Siasos G, Gargalionis A, Papavassiliou AG. The role of platelets in cardiovascular disease: molecular mechanisms. Curr Pharm Des. 2016;22(29):4493–4505. doi:10.2174/1381612822666160607064118
43. Azab B, Zaher M, Weiserbs KF, et al. Usefulness of neutrophil to lymphocyte ratio in predicting short- and long-term mortality after non-ST-elevation myocardial infarction. Am J Cardiol. 2010;106(4):470–476. doi:10.1016/j.amjcard.2010.03.062
44. Candemir M, Kiziltunç E, Nurkoç S, Şahinarslan A. Relationship between Systemic Immune-Inflammation Index (SII) and the severity of stable coronary artery disease. Angiology. 2021;72(6):575–581. doi:10.1177/0003319720987743
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
