Back to Journals » Patient Related Outcome Measures » Volume 10
Duration of military service is associated with decision quality in Veterans considering total knee replacement: case series
Authors Sabatino MJ , Reilly CA , Kunkel ST, Titus AJ, Ramkumar DB, Goodney PP, Ibrahim SA, Lurie JD, Henderson ER
Received 24 January 2018
Accepted for publication 22 May 2019
Published 5 July 2019 Volume 2019:10 Pages 209—215
DOI https://doi.org/10.2147/PROM.S163691
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Liana Bruce
Matthew J Sabatino,1,2 Clifford A Reilly,1 Samuel T Kunkel,1,2 Alexander J Titus,2,3 Dipak B Ramkumar,1,2 Philip P Goodney,2,4 Said A Ibrahim,5,6 Jonathan D Lurie,1,2 Eric R Henderson2,7
1Department of Orthopaedic Surgery, Dartmouth-Hitchcock Medical Center, Lebanon, NH 03756, USA; 2The Geisel School of Medicine, Dartmouth College, Hanover, NH 03755, USA; 3Program in Quantitative Biomedical Sciences, Geisel School of Medicine, Hanover, NH 03755, USA; 4Vascular Surgery Section, White River Junction VAMC, White River Junction, VT 05009, USA; 5Department of Medicine, University of Pennsylvania School of Medicine, Philadelphia, PA 19104, USA; 6Center of Innovation for Health Equity Research and Promotion (CHERP), VA Health Services and Research Development, Philadelphia, PA, 19104, USA; 7Orthopaedic Section, White River Junction VAMC, White River Junction, VT 05009, USA
Purpose: Due to the nature of military service, the patient–physician relationship in Veterans is unlike that seen in civilian life. The structure of the military is hypothesized to result in barriers to open patient–physician communication and patient participation in elective care decision-making. Decision quality is a measure of concordance between a chosen treatment and the aspects of medical care that matter most to an informed patient; high decision quality is synonymous with patient-centered care. While past research has examined how age and other demographic factors affect decision quality in Veterans, duration of military service, rank at discharge, and years since discharge have not been studied.
Patients and methods: We enrolled 25 Veterans with knee osteoarthritis at a VA hospital. Enrollees completed a survey with demographic, military service, and decision-making preference questions and the Hip-Knee Decision Quality Instrument (HK-DQI), which measures patients’ knowledge about their disease process, concordance of their treatment decision, and the considered elements in their decision-making process.
Results: The HK-DQI knowledge score had a significant, positive correlation with duration of military service (R2,=0.36, p=0.004). Rank at discharge and years since discharge did not show a significant correlation with decision quality (p=0.500 and p=0.317, respectively). The concordance score did not show a statistically significant correlation with rank, duration of service, and years since discharge (p=0.640, p=0.486 and p=0.795, respectively). Additionally, decision process score was not significantly associated with rank, duration of military service, and years since discharge (p=0.380, p=0.885, and p=0.474, respectively).
Conclusion: Decision quality in Veterans considering treatment for knee osteoarthritis appears to be correlated positively with duration of military service. These findings may present an opportunity for identification of Veterans at most risk of low decision quality and customization of shared decision-making methods for Veterans by characteristics of military service.
Keywords: Veterans, decision-quality, orthopaedics, knee osteoarthritis
Introduction
Active-duty military patients experience a unique environment in health care decision-making.1 Military service requires the subordination of the desires and interests of the individual to the needs of the service.2 Promoted in various military settings and campaigns, the message of “service above self” is a tenet based on the presumption of obedience.1 This obedience is not only presumed but also codified in regulations that dictate medical decisions made for military patients based on the interests of the nation and command.3,4 Additionally, rank or role within the military hierarchy often creates an environment of limited autonomy in medical decision-making.5 Due in part to medical expertise, but also to their rank as field grade or senior officers, physicians command a level of authority that places medical decision-making under unique pressures which accentuate the existing power imbalance between patient and physician.1 The behaviors associated with military service may have a lasting effect on the way Veterans engage in healthcare decision-making after their discharge from the military and impede their access to patient-centered care.6
It has been reported that Veterans will defer to physician-directed decision-making over self-directed decision-making with a 2:1 ratio.7 Additionally, Veterans are significantly more likely to defer to physician-directed treatment and have lower decision quality scores than civilian patients.6,8 Previous research directed toward understanding decision quality in the Veteran population has shown differences based on patient demographics (age, race, gender, and socioeconomic status) for nonorthopedic conditions. However, little evidence exists identifying factors associated with military service that may contribute to this disparity in Veterans’ decision quality.9,10 Length of overall service, highest rank obtained in service, and time since discharge are all critical components of a Veteran’s service record and may illuminate important components of decision style and quality.
Veterans with knee osteoarthritis who are considering a total knee replacement surgery offer an ideal population to study the effect of these factors on decision quality. Knee osteoarthritis is often classified as a preference-sensitive condition, in which a patient has more than one valid treatment option with substantial pros and cons to consider.11–14 Additionally, knee osteoarthritis is prevalent in Veterans, due to the average higher age of the population, and total knee replacement surgeries are associated with a high financial burden for the VA. In 2014, 9,153 Veterans received a total knee replacement, ranking this in the top five surgical procedures in the VA.15 In the United States, total knee replacements have an average per-procedure cost of $31,124, indicating an estimated cost to the VA of about $284 million per year.16
Our objective was to assess a cohort of Veterans with knee osteoarthritis using a validated survey instrument to evaluate how factors relating to their service record impacted decision quality. Our goal was to better understand the important characteristics of a Veteran’s role and time in the military in order to inform an effective patient-centered decision model at the VA.
Methods
Study subjects
We obtained IRB approval and then enrolled Veterans prospectively with knee osteoarthritis consecutively over a 6-month period at the White River Junction VA (WRJVA) in Vermont. Candidates were scheduled for a single, extended (1 hr total) visit with an orthopedic surgeon in the orthopedic clinic to allow for Veteran education, consent, and data collection.
Inclusion criteria consisted of a diagnosis of knee (ICD-9 715.96) osteoarthritis without prior treatment and without preexisting contraindications to nonsurgical and surgical osteoarthritis treatments.
We excluded patients if they had inflammatory arthritis, concomitant hip, and knee pain, prior joint replacement, or if they had sensory, cognitive, or other impairment that precluded informed consent.
We conducted a sample size calculation using PS 3.1.6 (Vanderbilt University, Nashville, TN, USA) with an alpha of 0.05 and a power of 0.8 based on our primary outcome of decision quality. We determined that 13 patients were needed to sufficiently power our analysis. Twenty-five (25) patients were enrolled in the cohort after meeting the study criteria. Twenty-four (24) patients were male, and one was female. Please see Table 1 for a compilation of cohort demographic measures and distributions.
 |
Table 1 Cohort characteristics based on highest service rank achieveda |
Study questionnaire
Patients enrolled in the cohort underwent informed consent to participate in a pre- and post-visit survey. The primary survey administered to assess decision quality was the Hip and Knee Osteoarthritis Decision Quality Instrument (HK-DQI). The HK-DQI is a validated instrument with 16 questions measuring patients’ understanding of their disease, treatment options, and expected treatment benefits with an emphasis on joint replacement.17 The questionnaire is scored in 3 domains (knowledge score, concordance, and decision process).17
The knowledge score reflects the patient’s understanding about evidence-based facts surrounding osteoarthritis and available treatments on a scale of 0–100%. The concordance section has patients rate their goals and concerns and then select which treatment they choose to treat their knee osteoarthritis (surgery vs nonsurgery). Patients are scored on whether their preference matched the treatment they received (0–100%). The decision process section asks patients to complete questions regarding the interaction between the patient and the provider with answers scored on a scale of 0–100%.
Demographic information, survey results, and decision choices were recorded and entered into MS Excel spreadsheet (Microsoft, Redmond, WA, USA). Included in demographic information were categorical data regarding prior military service, rank, discharge status, and education level.
Data analysis
Statistical analysis was performed using Stata 13.0 statistical software (Statacorp, College Station, TX, USA) and R 3.3 statistical software (R Foundation, Vienna, Austria). Continuous variables were assessed for normal distribution and evaluated using parametric tests (Student’s t-test or ANOVA) or nonparametric tests (Kruskal–Wallis). Additionally, survey scores were compared with paired t-tests to evaluate significance in change and correlation of variables associated with change. Categorical variables were tested using χ2 or Fisher’s exact test.
Simple and multiple regression models were constructed for the outcome measures associated with each domain of the HK-DQI. Logistic regression was performed for concordance as this was a direct match dichotomous variable.
Exposures were assessed for potential confounding, and effect rates were analyzed in both crude and adjusted forms. This was particularly important, given the potential pitfalls in stratifying results from related variables of time in service, rank, and education level. Specifically, increases in education level and time in service can be directly correlated with increase in rank.
Results
Decision quality
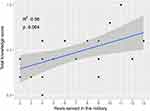
Total knowledge score did not have a significant association with highest rank achieved in the military or years since discharge from the military (p=0.500 and p=0.317, respectively). (Figure 1) There was, however, a significant association between years of service and knowledge score. This significance was present in crude analysis (R2=0.36, p=0.017) and when adjusted for potential confounders of rank, years since discharge and education level (R2=0.42, p=0.023). (Figure 2) Based on the coefficient from the regression model, for each year that a Veteran spent in active service, there was a corresponding increase of knowledge score of 3.4% (p=0.023).
Additionally, knowledge score was significantly associated with graduate education level in crude analysis and when adjusted for rank, years of service, and years since discharge (p=0.014).
The HK-DQI concordance score was not significantly associated with any of the primary exposure variables in the adjusted logistic regression model. Rank, years in service, years since discharge, and education level demonstrated no significant association with the concordance outcome (p=0.640, p=0.486, p=0.795 and p=0.174, respectively).
Decision process score was not significantly associated with any of the primary exposure variables in the adjusted regression model. No significant association with the decision process outcome was demonstrated for rank (p=0.380), years in service (p=0.885), years since discharge (p=0.474), or education level (p=0.067). A summary of main effects of the covariates on decision quality outcomes is seen in Table 2.
 |
Table 2 Service characteristics and HK-DQI results |
Discussion
Patient-centered care is designed to facilitate health care based upon the best available evidence and match treatment with patients’ individual goals and beliefs while establishing realistic expectations for outcome.8,14,18,19 While there are numerous facets to patient-centered care, the single best indicator of patient-centered care is decision quality.20,21 High decision quality requires two essential components: 1) patients’ decisions are based on the best available evidence; 2) patients’ decisions are consistent with the treatment endpoints that matter most to each individual patient.17,21
The disparities between a collaborative, patient-centered process compared to a process in which physicians direct treatment decisions have been well established. Physician-directed treatment is known to yield increased surgical rates and anxiety, as well as reduced decision quality and patient satisfaction following treatment.12,14,17,18,22–27 Furthermore, research supports that surgeons are often poor patient educators, accentuating the need for a formal process to inform patients’ decisions when considering surgical intervention.20
Previous research has demonstrated a disparity between decision quality in Veterans and the civilian population.6 However, no previous studies have investigated how factors relating to military service might be associated with this disparity.9,10 Our study attempted to fill this gap by evaluating the association between military service factors and decision quality in a cohort of Veterans seeking treatment for knee osteoarthritis. Our intent was to determine how rank, time in service, and years since discharge are associated with decision quality.28 Our primary finding showed a significant association between years in service and knowledge score, a domain of the HK-DQI. Specifically, the greater the Veteran’s years of service, the higher the Veteran’s knowledge score. This association remained significant when adjusted for all other measured components of service record and education level. Our study also found that Veterans with post-graduate level of education had significantly better knowledge scores. This supports previous findings that show an association between education and decision quality in Veterans.109
While a causal relationship cannot be concluded from our primary finding of an association between length of service and decision quality, it is important to attempt to understand the mechanism behind this association. It is possible that a greater time in service could confer a greater level of comfort in medical decision-making in a VA medical center setting. Since knowledge score measures the patient’s understanding of risks, benefits, and alternatives of treatment, comfort in a setting in which a provider explains the details of treatment would convey an advantage for retaining important knowledge about treatment factors.
Additionally, the finding that greater duration of service is associated with better decision quality could conversely undermine the premise that the atmosphere of obedience stifles patient autonomy. While the Veteran’s comfort in the military atmosphere may indeed improve interaction with the provider, more research is needed to determine if length of service is associated with subjugating one’s treatment goals to the recommendations stated by the provider. Future research should focus on understanding the mechanism behind this association and how to implement these findings to create a better environment for medical decision-making in the Veteran population, such as a formal shared decision-making model.
One strength of our study was the completeness of our decision data in the cohort. We obtained follow-up with Veterans to obtain survey scores and treatment decisions with 100% completion rate. Another strength was our prospective use of a validated instrument (HK-DQI) to measure decision quality. Multiple studies and instruments have been developed to evaluate the quality of decision-making in the osteoarthritis population.14,17,22,29 These instruments help inform providers focused on improving patient decision quality.
However, our study is not without limitations. We were able to define areas of association between decision quality and Veteran service characteristics, but we were not able to determine causality. We also note that this study is limited by the cohort size and patient demographics. Twenty-five patients were enough to power our present analysis. However, our analysis was somewhat limited as further subclassification of the cohort weakened the power of our calculations and prevented us from running a larger multivariate analysis. Additionally, our cohort was almost entirely male (24/25) and predominantly white (20/25), limiting generalizability to the population.
Although limited in the scope of its application, this study addresses a population that would benefit from structured shared decision-making and decision aids. Active duty soldiers function daily in a setting of military hierarchy and top-down communication structure. As these soldiers leave military service and begin to receive care as Veterans in VA medical centers, the degree to which their medical decision-making is affected by their comfort with authority leaves them potentially vulnerable to poorly informed or incomplete decisions.
Conclusion
Our study is the first to evaluate Veteran decision quality based on the characteristics of their military service. In our cohort of Veterans with knee osteoarthritis, we found that Veterans with longer time of military service had higher decision quality scores than those with a shorter service tenure. Rank and time since discharge were not significantly associated with overall decision quality. Overall, our study highlights an opportunity for a formal shared decision-making process to better inform Veterans and improve decision quality.
Ethics Approval
This study was approved by the Committee for the Protection of Human Subjects at Dartmouth-Hitchcock Medical Center and the Veteran’s IRB of Northern New England (VINNE); study number 00028655. All enrolled participants were provided written informed consent.
Acknowledgments
Dr. Ibrahim is supported in part by a K24 Mid-Career Development Award from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (K24AR055259). The views expressed in this paper are those of the author and do not represent those of the Department of Veterans Affairs, the National Institute of Arthritis and Musculoskeletal and Skin Diseases, or the National Institutes of Health.
Disclosure
Dr. Ibrahim's current employment is at the Department of Healthcare Policy and Research, Weill Cornell School of Medicine, New York, NY, USA. The authors report no other conflicts of interest in this work.
References
1. Maya H. Patient-physician relationships in the military. Heal Law Policy. 2008;2(1):8.
2. Orloff v. Willoughby. 345 U.S. 83, 92. 1953.
3. A soldier on active duty or active duty for training will usually be required to submit to medical care considered necessary to preserve his or her life, alleviate undue suffering, or protect of maintain the health of others. In: Unites States Department of Defense, editor. Army Regulation. Army Command Policy 5-4(a); 2014:600–620.
4. The FDA may decide that potential recipients of a drug under an emergency use authorization should have the option to refuse it. the president may waive this option for military personnel. In: United States Department of Defense, editor. Army Regulation 40–562, Immunizations and Chemoprophylaxis. US Department of Army; 2014:3–8.
5. Thunholm P. Military leaders and followers–do they have different decision styles? Scand J Psychol. 2009;50(4):317–324. doi:10.1111/j.1467-9450.2009.00714.x
6. Henderson ER, Titus AJ, Keeney BJ, Goodney PP, Lurie JD, Ibrahim SA. Military service and decision quality in the management of knee osteoarthritis. Mil Med. 2018;183(7–8):e208–e213. doi:10.1093/milmed/usy104
7. Mazur DJ, Hickam DH. Patients’ preferences for risk disclosure and role in decision making for invasive medical procedures. J Gen Intern Med. 1997;12(2):114–117. doi:10.1046/j.1525-1497.1997.00016.x
8. Strull WM, Lo B, Charles G. Do patients want to participate in medical decision making? JAMA. 1984;252(21):2990–2994.
9. Park SG, Derman M, Dixon LB, et al. Factors associated with shared decision-making preferences among veterans with serious mental illness. Psychiatr Serv. 2014;65(12):1409–1413. doi:10.1176/appi.ps.201400131
10. Rodriguez V, Andrade AD, Garcia-Retamero R, et al. Health literacy, numeracy, and graphical literacy among veterans in primary care and their effect on shared decision making and trust in physicians. J Health Commun. 2013;18(Suppl 1):273–289. doi:10.1080/10810730.2013.829137
11. Wennberg JE. Unwarranted variations in healthcare delivery: implications for academic medical centres. BMJ. 2002;325(7370):961–964. doi:10.1136/bmj.325.7370.961
12. O’Connor AM, Llewellyn-Thomas HA, Flood AB. Modifying unwarranted variations in health care: shared decision making using patient decision aids. Heal Aff. 2004;Suppl Vari:VAR63–VAR72. doi:10.1377/hlthaff.var.63
13. Slover J, Shue J, Koenig K. Shared decision-making in orthopaedic surgery. Clin Orthop Relat Res. 2012;470(4):1046–1053. doi:10.1007/s11999-011-2156-8
14. Bozic KJ, Chiu V. Emerging ideas: shared decision making in patients with osteoarthritis of the hip and knee. Clin Orthop Relat Res. 2011;469(7):2081–2085. doi:10.1007/s11999-010-1740-7
15. Q1 FY15 VA National Surgery Office Quarterly Report. Unites States Department of Veterans Affairs - National Surgery Office; 2015.
16. Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169(12):1112–1113. doi:10.1001/archinternmed.2009.136
17. Sepucha KR, Stacey D, Clay CF, et al. Decision quality instrument for treatment of hip and knee osteoarthritis: a psychometric evaluation. BMC Musculoskelet Disord. 2011;12:149. doi:10.1186/1471-2474-12-181
18. Sepucha KR, Fowler FJ
19. Bozic KJ, Lau E, Kurtz S, et al. Patient-related risk factors for periprosthetic joint infection and postoperative mortality following total hip arthroplasty in Medicare patients. J Bone Jt Surg Am. 2012;94(9):794–800. doi:10.2106/JBJS.K.00072
20. Braddock CH
21. Elwyn G, O’Connor A, Stacey D, et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ. 2006;333(7565):417. doi:10.1136/bmj.38926.629329.AE
22. Bozic KJ, Belkora J, Chan V, et al. Shared decision making in patients with osteoarthritis of the hip and knee: results of a randomized controlled trial. J Bone Jt Surg Am. 2013;95(18):1633–1639. doi:10.2106/JBJS.M.00004
23. Mistler LA, Drake RE. Shared decision making in antipsychotic management. J Psychiatr Pr. 2008;14(6):333–344.
24. Van Citters AD, Fahlman C, Goldmann DA, et al. Developing a pathway for high-value, patient-centered total joint arthroplasty. Clin Orthop Relat Res. 2014;472(5):1619–1635. doi:10.1007/s11999-013-3398-4
25. Weng HH, Kaplan RM, Boscardin WJ, et al. Development of a decision aid to address racial disparities in utilization of knee replacement surgery. Arthritis Rheum. 2007;57(4):568–575. doi:10.1002/art.22670
26. Lurie JD, Weinstein JN. Shared decision-making and the orthopaedic workforce. Clin Orthop Relat Res. 2001;385:68–75. doi:10.1097/00003086-200104000-00012
27. Youm J, Chenok KE, Belkora J, Chiu V, Bozic KJ. The emerging case for shared decision making in orthopaedics. Instr Course Lect. 2013;62:587–594.
28. Ankuda CK, Block SD, Cooper Z, et al. Measuring critical deficits in shared decision making before elective surgery. Patient Educ Couns. 2014;94(3):328–333. doi:10.1016/j.pec.2013.11.013
29. Klassbo M, Larsson E, Mannevik E. Hip disability and osteoarthritis outcome score. An extension of the Western Ontario and McMaster Universities Osteoarthritis Index. Scand J Rheumatol. 2003;32(1):46–51.
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.