Back to Journals » Therapeutics and Clinical Risk Management » Volume 16
Doxycycline Combined with NB-UVB Phototherapy for Acquired Reactive Perforating Collagenosis
Authors Gao L, Gu L, Chen Z, Cao S
Received 10 July 2020
Accepted for publication 21 August 2020
Published 24 September 2020 Volume 2020:16 Pages 917—921
DOI https://doi.org/10.2147/TCRM.S271058
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Limu Gao, Lixiong Gu, Zhen Chen, Shuanglin Cao
Department of Dermatology, Affiliated Hospital of Nantong University, Nantong, Jiangsu Province, People’s Republic of China
Correspondence: Shuanglin Cao
Department of Dermatology, Affiliated Hospital of Nantong University, 20th Xisi Road, Nantong, People’s Republic of China
Email [email protected]
Background: Acquired reactive perforating collagenosis is a rare skin disease characterized by the discharge of collagen fibers through the epidermis. There is no standard treatment for this disease currently. Here, we report a case of ARPC that has been successfully treated and cured.
Case Description: A 32-year-old man developed severe itching papules on his torso and limbs for 3 months. Skin lesions were keratotic papules scattered on the limbs and trunk, with a diameter of 3 to 12 mm. Some lesions had umbilical recesses and the shape of a crater with positive isomorphic reactions. The patient scratched his severe itching lesions which merged into large ones. This patient had histories of hypertension and dilated cardiomyopathy with mild congestive heart failure. The clinical presentation and histopathology of skin lesions met Faver’s diagnostic criteria for ARPC.
Treatment: Oral Doxycycline 100mg/d, NB-UVB phototherapy 3 times a week with initial dose 400mJ/cm2, gradually increased to 1200mJ/cm2(total cumulative dose 16700J/cm2).
Outcomes: After a week of treatment, the patient’s itching symptoms were significantly reduced and stopped presenting any new skin lesions. Most of the lesions healed in 6 weeks of treatment.
Lessons: Doxycycline combined with NB-UVB may be an effective treatment for ARPC.
Keywords: acquired reactive perforating collagenosis, doxycycline, NB-UVB, hypertension
Introduction
Acquired reactive perforating collagenosis (ARPC) is a rare skin disease characterized by the excretion of collagen through the epidermis, first reported by Mehregan in 1967. There are two types of RPC, hereditary RPC and acquired RPC (acquired RPC, ARPC). The former is relatively rare, seen in infancy or early childhood. The acquired RPC is common in adults. The pathogenesis of ARPC is not yet clear. No standardized treatment is available at present. Here we report a case of ARPC that had been successfully cured.
Consent
This patient signed informed consent for the publication of this case report and the associated images. And this study was approved by the ethics committee of Affiliated Hospital of Nantong University.
Case Presentation
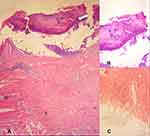
A 32-year-old man came to our outpatient clinic with severe itching papules in his torso and limbs for three months. Initially, itchy keratotic papules appeared on his lower extremities, then on his upper limbs and trunk. The keratotic papules were scattered on the limbs and trunk, with a diameter of 3 to 12 mm. Some skin lesions had a concave umbilical shape and a crater shape (Figure 1). Koebner Phenomenon is positive in this case. The patient scratched both upper arms, waist, and lower limbs due to severe itchiness. Some of the scratched lesions merged into large ones (Figure 2). This patient had a 5-year history of uncontrolled hypertension and a 2-year history of dilated cardiomyopathy with mild congestive heart failure. Lab results showed decreased creatinine clearance (CKD stage 3b), but normal creatinine, urea nitrogen, blood glucose and glycated hemoglobin. Histopathological manifestations were localized epidermal defects with cup-shaped depressions. The defects contained a large number of keratinized plugs (Figure 3A, HE×40). Locally visible collagen fibers that vertically penetrated the epidermis were characteristic, with infiltration of inflammatory cells around them (Figure 3B, HE×100), Masson staining showed collagen fibers stained in the superficial dermis and blue in the epidermis (Figure 3C, Masson stain×400). The clinical presentation and histopathology of skin lesions meet Faver’s diagnostic criteria for ARPC. Treatment: oral Doxycycline 100mg/d, NB-UVB phototherapy 3 times a week, 400mJ/cm2 increasing gradually to 1200mJ/cm2 (total cumulative dose 16700J/cm2). After 1 week of treatment, the patient’s itching symptoms were significantly reduced, and stopped presenting new skin lesions. Most of the lesions subsided after 6 weeks of treatment (Figure 4).
Discussion
The etiology and pathogenesis of ARPC are still unclear. Childhood onset is related to autosomal dominant or recessive inheritance. Adult patients are often accompanied by one or more systemic diseases.1 Among systemic diseases accompanied by ARPC, hypertension is the most common, followed by diabetes, and kidney failure.2 At present, some studies have found that there is overexpression of transforming growth factor (TGF)-β3 in many ARPC patients3 suggesting that this factor may be related to the incidence of ARPC. Advanced glycosylation end product receptor (RAGE) is a multi-ligand transmembrane receptor that plays an important role in the inflammatory response. The overexpression of RAGE in skin lesion specimens of ARPC patients may be involved in the pathogenesis of ARPC.4 Micro-trauma caused by itching and scratching has been considered to be an important cause of ARPC and plays an important role in the development of the disease.5 After itching control, the improvement of clinical symptoms supports this view. There is no standardized treatment currently. Various ARPC treatments mainly include topical application of glucocorticoids, antihistamines, retinoic acid drugs, vitamin D analogs, allopurinol, and phototherapy. Glucocorticoids and antihistamines are the most commonly prescribed drugs.6 Therapeutic agents that have been used to treat and reduce lesions without major side effects include isotretinoin, corticosteroids, allopurinol, antibiotics such as doxycycline, and phototherapy. Treatments of ARPC should be prioritized according to patients’ needs and availability. The patient is obese, hyperlipidemia, hypertension, and hyperuricemia. In addition, his skin lesions are large and skin infections are likely to occur. All things considered, doxycycline is considered beneficial and more suitable for him. Combination treatment, rather than monotherapy, has been shown to result in more favorable outcomes.7 So we chose doxycycline combined with NB-UVB phototherapy for acquired reactive perforating collagenosis. Our treatment plan for this patient was oral Doxycycline 100mg/d, combined with narrow-band UVB 3 times a week, the initial dose was 400mJ/cm2, then increased to 1200mJ/cm2 gradually (Total cumulative dose 16700J/cm2). After a week of treatment, the patient’s itching symptoms were significantly improved, and no new skin lesions appeared. Most of the lesions subsided after 6 weeks of treatment. It has been reported Doxycycline was an effective treatment,8 but the exact mechanism of action is unclear. Doxycycline has immunomodulatory and anti-inflammatory effects, of which the inhibitory effect on stroma proteins has been emphasized as a major non-antibacterial effect. Therefore, Doxycycline may play a role by inhibiting matrix metalloproteinases, regulating inflammatory cytokines, and inhibiting the chemotaxis and activation of leukocytes.9 NB-UVB is also a commonly used treatment method and has achieved good results in some patients.10 Neutrophils are the main cells in the pathogenesis of ARPC,11 which may promote the development of disease by releasing matrix metalloproteinases and other serine proteases to destroy the structure of the basement membrane.12 NB-UVB may play a therapeutic role by inhibiting neutrophil infiltration and regulating immune function.13
Conclusions
In summary, we report a case of APRC that showed great response to Doxycycline in combination with NB-UVB. Our treatment is supported by the literature, indicating that Doxycycline combined with NB-NVB may be an effective method for the treatment of ARPC. Due to the rareness of this disease, further Study Is needed to validate the treatment protocol and maximize therapeutic benefit in ARPC.
 |
Figure 1 Clinical images of ARPC. Scattered keratotic papules on the trunk, part of the lesions may have umbilical recesses, and the shape is crater-shaped (White arrow). |
 |
Figure 4 Clinical images before and after ARPC treatment. (A) Scattered rashes all over the body before treatment; (B) most of the lesions subsided after 6 weeks of treatment. |
Abbreviations
ARPC, acquired reactive perforating collagenosis; NB-UVB, narrow bound ultra violet B light.
Acknowledgments
We thank all members from the Department of Dermatology, Affiliated Hospital of Nantong University for their advice and encouragement.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Karpouzis A, Giatromanolaki A, Sivridis E, et al. Acquired reactive perforating collagenosis: current status. J Dermatol. 2010;37(7):585–592. doi:10.1111/j.1346-8138.2010.00918.x
2. Garrido P, Queirós C, Borges-Costa J, et al. Acquired perforating dermatosis: clinicopathologic study of a 10-year period at a tertiary teaching hospital. Int J Dermatol. 2020;59(4):445–450. doi:10.1111/ijd.14760
3. Gambichler T, Birkner L, Stücker M, et al. Up-regulation of transforming growth factor-beta3 and extracellular matrix proteins in acquired reactive perforating collagenosis. J Am Acad Dermatol. 2009;60(3):463–469. doi:10.1016/j.jaad.2008.06.006
4. Akoglu G, Sungu N, Karaismailoglu E, et al. Expression of the receptor for advanced glycation end products in acquired reactive perforating collagenosis. Indian J Dermatol Venereol Leprol. 2017;83(4):432–435. doi:10.4103/ijdvl.IJDVL_113_16
5. Kim S, Kim M, Lee J, et al. A clinicopathologic study of thirty cases of acquired perforating dermatosis in Korea. Ann Dermatol. 2014;26(2):162–171. doi:10.5021/ad.2014.26.2.162
6. García-Malinis A, Del Valle Sánchez E, Sánchez-Salas M, et al. Acquired perforating dermatosis: clinicopathological study of 31 cases, emphasizing pathogenesis and treatment. J Eur Acad Dermatol Venereol. 2017;31(10):1757–1763. doi:10.1111/jdv.14220
7. Lukács J, Schliemann S, Elsner P. Treatment of acquired reactive perforating dermatosis – a systematic review. J Dtsch Dermatol Ges. 2018;16(7):825–842. doi:10.1111/ddg.13561
8. Brinkmeier T, Schaller J, Herbst R, et al. Successful treatment of acquired reactive perforating collagenosis with doxycycline. Acta Derm Venereol. 2002;82(5):393–395. doi:10.1080/000155502320624249
9. Monk E, Shalita A, Siegel D. Clinical applications of non-antimicrobial tetracyclines in dermatology. Pharmacol Res. 2011;63(2):130–145. doi:10.1016/j.phrs.2010.10.007
10. Sehgal V, Verma P, Bhattacharya S, et al. Familial reactive perforating collagenosis in a child: response to narrow-band UVB. Pediatr Dermatol. 2013;30(6):762–764. doi:10.1111/j.1525-1470.2012.01736.x
11. Zelger B, Hintner H, Auböck J, et al. Acquired perforating dermatosis. Transepidermal elimination of DNA material and possible role of leukocytes in pathogenesis. Arch Dermatol. 1991;127(5):695–700. doi:10.1001/archderm.127.5.695
12. Thiele-Ochel S, Schneider L, Reinhold K, et al. Acquired perforating collagenosis: is it due to damage by scratching? Br J Dermatol 2001;145(1):173–174. doi:10.1046/j.1365-2133.2001.04309.x
13. Leino L, Saarinen K, Kivistö K, et al. Systemic suppression of human peripheral blood phagocytic leukocytes after whole-body UVB irradiation. J Leukoc Biol. 1999;65(5):573–582. doi:10.1002/jlb.65.5.573
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.