Back to Journals » Cancer Management and Research » Volume 11
Dosimetry comparison between a 3D printed minimally invasive guidance template and free implantation in the brachytherapy treatment of postoperative recurrent cervical carcinoma
Authors Yuan X, Zhang Y , Cui M, Miao J, Gao L, Hu J, Tian D, You J
Received 24 November 2018
Accepted for publication 19 April 2019
Published 30 May 2019 Volume 2019:11 Pages 5013—5018
DOI https://doi.org/10.2147/CMAR.S195829
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Beicheng Sun
Xiangkun Yuan1,*, Yongxia Zhang1,*, Mangmang Cui,1 Junjun Miao,1 Lei Gao,1 Jianwei Hu,1 Dandan Tian,1 Jinqiang You2
1Department of Radiation Oncology, Hebei Province Cangzhou Hospital of Integrated Traditional and Western Medicine, Cangzhou, Hebei, People’s Republic of China; 2Department of Radiotherapy, Tianjin Medical University Cancer Institute and Hospital, National Clinical Research Center for Cancer, Tianjin Key Laboratory of Cancer Prevention and Therapy, Tianjin, People’s Republic of China
*These authors contributed equally to this work
Objective: This study aimed to investigate the dosimetry difference between a 3D printed minimally invasive guidance template and conventional free implantation in brachytherapy of postoperative recurrent cervical carcinoma under the guidance of computed tomography (CT).
Methods: A total of 21 cases of patients with recurrent cervical cancer after operation were enrolled from January 2017 to June 2018. After external irradiation treatment in 1.8-Gy fractions to 45 Gy, patients were randomly divided into two groups to receive brachytherapy: 11 cases were assisted by a 3D-printed minimally invasive guidance template, and the other 10 cases were free implantation. In the template group, needles were inserted according to the main guide channel of the template commissioned in medical photosensitive resin, while patients in the other group were treated with bare hands under the guidance of CT, which was used in both groups to adjust the position and depth of the implant needles. After transmission of the CT images into the Oncentra® Brachy TPS system, the target organs and organs at risk were delineated for further treatment.
Results: The D90 value of the high-risk clinical target volume in the template group was 6.30±0.21 Gy while that in the other group was 6.07±0.32 Gy (P<0.05). In addition, the D2cm3 (illuminated dose of 2 cm3 of organ at risk) value of the bladder, rectum, sigmoid colon, and bowel was significantly decreased in the template group as compared to the free group (P<0.05). The number of needles used for each treatment in the template group was 5.71±1.82, while that for the free injection group was 7.78±2.35 (P<0.05).
Conclusion: Compared with conventional free implantation, the 3D printed minimally invasive guidance template-assisted treatment has an obvious dosimetry advantage in the treatment of postoperative recurrent cervical carcinoma, with shorter time of implantation and better repeatability.
Keywords: postoperative recurrent cervical carcinoma, 3D printing, minimally invasive guidance template, implantation brachytherapy
Introduction
The recurrence of cervical cancer after operation is a challenging condition for several physicians, which can be resolved by reoperation or radiotherapy. The wide resection range of surgery and multiple postoperative complications are a disadvantage that cannot be accepted by many patients,1–3 thereby rendering radiotherapy a remarkable option in the treatment of postoperative recurrent cervical cancer. However, patients cannot achieve a radical radiation dose through external beam radiation therapy because of its dosage limitation on the organs at risk (OAR),4 which makes brachytherapy indispensable for further treatment along with or after external beam radiation therapy. Also, brachytherapy can obviously improve the dose level of tumor tissues without a significant increase in the dose in the surrounding normal organs.5 The needles can be inserted into the tumor uniformly and accurately through interstitial implantation with optimal conformability, thereby achieving a high dose on the tumor for an enhanced therapeutic effect.6–8 The 3D printed minimally invasive guidance template is a newly emerging technology that can be applied to cervical cancer with the goal of individualized treatment. Thus, the present study aimed to compare the dosimetry difference between a 3D printed minimally invasive guidance template and an unconventional implantation in the brachytherapy of postoperative recurrent cervical carcinoma.
Materials and methods
Clinical data
A total of 21 cases of postoperative recurrent cervical cancer admitted to our hospital from January 2017 to June 2018 were enrolled. The inclusion criteria were as follows: 1) pathological diagnosis of postoperative pathology which was consistent with that of recurrence after surgery; 2) imaging examination, such as pelvic magnetic resonance imaging, confirming local recurrence of different degrees; 3) no distant metastasis of other organs or tissues found in the imaging examination; and 4) no chance of reoperation or refusal to operate. All patients were randomly divided into two groups after the intensity-modulated radiotherapy dose reached 45 Gy in 25 fractions of 1.8 Gy, and were treated with a high dose of 192Ir 3D after loading on the brachytherapy machine, 6 Gy/fraction, 4–6 times in total. Some patients were treated with concurrent cisplatin chemotherapy (30–40 mg/m2, 1 time/week) during this period (Table 1).9,10 There is no selection bias in the clinical characteristics of the two groups of patients. The present study was conducted under the approval, supervision, and guidance of the Ethics Committee of Cangzhou Chinese and Western Medicine Integrated Hospital, and all patients signed the informed consent to fulfill the ethical requirement. This study was conducted in accordance with the Declaration of Helsinki.
 | Table 1 Patient characteristics |
Procedure of 3D interstitial implantation brachytherapy
Design and production of the 3D printed minimally invasive guidance template
Patients were asked to undergo some preoperative preparation including vaginal irrigation, emptying themselves of urine and stool, radiography swallowing, and catheterization. Different types and lengths of vaginal 3D templates (QL-YXK-HZ) were selected for patients in the template group according to the length of the vagina and the narrow degree of vaginal postoperation. A volume of 120 mL saline was injected into the bladder before computed tomography (CT) scan, and images were transmitted into the Oncentra® Brachy TPS plan system. The tumor target volume and OAR were delineated by the physician based on the pelvic magnetic resonance imaging scan before the treatment, following which the images were uploaded to the planning system, Prowess Panther V4.72, through the Qilin data cloud platform (Ucloud V2.3.7). According to the design of the target area, the spatial distribution of the main needle tracks was designed, and an auxiliary stitch was also designed at 0.5 cm next to each main needle track, up/down and left/right. The data were imported into the template production system (Unicorn 3D template system V3.1) to establish a 3D model, which was then input into the 3D printer (EP-A650) (Figure 1A). Finally, an individualized 3D printed minimally invasive guidance template with a satisfactory conformability degree, including information on the needle track position, was acquired (Figure 1B).
 | Figure 1 Schematic representation of needle track design (A) and 3D-printed minimally invasive-guided template (B). |
Implantation process
The 3D printed minimally invasive guided template was inserted into the vagina in the template group, with the template wing fully attached to the perineum, which was further fastened by transparent dressings. The needles were inserted into the preset tracks. The position and depth of the inserted needles were adjusted according to the CT scan result. The conventional implantation in the free group was relatively simple, as described previously (Figure 2A).11
Treatment planning
The CT images were transmitted into the Oncentra Brachy TPS plan system, and the high-risk clinical target volume (HR-CTV) as well as the OAR, such as the rectum, bladder, sigmoid colon, and bowel, were delineated according to the guidelines of the European Association of Gynecological Radiotherapy.12,13 The prescription dosage of HR-CTV was 6 Gy/fraction, 1 time/week. The patients underwent brachytherapy 4–6 times (Figure 2B).
Observation variables
Data for each patient were recorded with respect to the number of needles used, the number of CT scans, and the time for the implantation needle to reach a satisfactory position during every treatment. The dose distribution of the target volume was evaluated using the D98, D95, and D90 values of HR-CTV, and the OAR volume dose limitation was evaluated using illuminated dose of 2 cm3 of organ at risk (D2cm3).12,13
Statistical methods
The data are represented as mean±SD and analyzed using SPSS 17.0. The Wilcoxon rank sum nonparametric test was performed to compare the clinical tumor characteristics between the two groups. The two groups were tested to conform to the normal distribution, and an independent-samples t-test was applied. P<0.05 was considered a statistically significant difference.
Results
All patients successfully underwent 3D interstitial implantation brachytherapy 4–6 times, and 116 times in total.
Comparison of target volume and OAR: the D98, D95, and D90 values of HR-CTV in the template group were significantly higher than in the free implantation group (P<0.05) (Table 2). Compared to the free group, the D2cm3 value of the bladder, rectum, sigmoid colon, and bowel in the template group was significantly decreased (P<0.05) (Table 3).
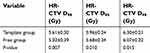 | Table 2 Therapeutic parameters of the target volume (mean±SD) |
 | Table 3 Therapeutic parameters of the organs at risk (mean±SD) |
Number of CT scans, time of insertion, and number of needles: the average number of CT scans was 1.61±0.52 for each implantation treatment in the template group, the average consumption time for each implant treatment from the time of insertion of the needles up to that of reaching the satisfactory position was 10.21±2.16 min, and the number of needles used for each implant treatment was 5.71±1.82. Nevertheless, the data for the free implantation group were 3.12±0.82 scans, 30.52±6.08 min, and 7.78±2.35 needles, respectively, and the differences were statistically significant (P<0.05) (Table 4).
 | Table 4 Number of CT scans, time for insertion, and number of needles used |
Discussion
Interventional implantation brachytherapy is usually adopted in the treatment of recurrent cervical cancer with the advantage of the degree of conformation and encompassing the target volume to the maximum, thereby achieving a satisfactory therapeutic effect.14–16 However, this conventional technique has several limitations. First, due to an error of judgment in the insertion angle, needles can easily deviate from the direction of the original design, requiring adjustment of the direction and depth of the insertion needle several times during the treatment process, thereby prolonging the operation time and increasing the risk of complications such as local bleeding. Second, the skills and experience of surgeons play a critical role in the treatment. However, the prolonged period of this technique renders difficulty in establishing a standard. Third, multiple CT scans increase the patient’s exposure to radiation. Finally, the irregular shape of the postoperative stump and vaginal stenosis may lead to poor adhesion between the applicator and mucosa, resulting in a poor distribution of the dose.17 For the classic transperineal template applicators, such as the Syed–Neblett butterfly applicator and the Martinez Universal Perineal Interstitial Template applicator, the distance between the template and the tumor is so large that it is difficult to ensure accuracy of the needle insertion. In addition, the risk of complications increases with the increasing number of inserted needles. Moreover, patients are required to wait with needles inserted for the whole process of treatment, which lasts for several days, causing great pain for patients.18,19 Considering the above deficiencies, our center has independently developed a 3D printed minimally invasive guidance template for the treatment of recurrent cervical cancer. Currently, no reports are available on the clinical application of this template in the treatment of recurrent cervical cancer worldwide.
The 3D printed minimally invasive guidance template adopted in this study is a technology that has newly emerged in recent years. The technology adopts 3D digitization to establish an individualized template, which contains the needle track information of the designed plan and can be used for preplanning the design in order to guarantee the conformability and accuracy of the tumor target volume. The angle and depth of insertion can be rapidly achieved with the help of predesigned needle tracks, thereby reducing the difficulty of operation and shortening the operation time. In addition, the technology not only limits residual irradiation but also significantly reduces the OAR dose and substantially reduces treatment pain.20,21 Several studies have investigated the application of a 3D printing template for particle implantation therapy,22–24 suggesting the advantages of accurate localization and orientation, and deeming it an effective and accurate auxiliary tool.
The radiation dose D90 value of the HR-CTV should be between 80 and 90 Gy as recommended by the American Brachytherapy Society.25 In this study, all of the doses for the target volume fulfilled the requirement; however, a significantly high dose could be achieved for the target volume in the template group as compared to the free group.26 Also, it is recommended that the bladder D2cm3 value is <90 Gy EQD2, and the D2cm3 value of the rectum and sigmoid colon is <75 Gy EQD2. In this study, the cumulative doses of the OAR for all patients met the requirement, with the dose of the OAR in the template group significantly lower than that of the free group. Liu et al11 studied 16 cases of recurrent cervical carcinoma treated by free needle implantation guided by CT and found that the average number of CT scans was 3.1±0.9, the average time from the first implantation to the final CT scan was 30.9±8.6 min, and the average number of needles was 6.1±1.5, which are similar results to those of the free group in the current study. Conversely, fewer CT scans were required for the template group, the adjustment time was shorter, and the number of therapeutic needles was lower. These factors lessened the pain. Therefore, studies with a larger sample size are an urgent requisite to verify the conclusion achieved by those involving a smaller number of samples.
Conclusion
The 3D minimally invasive guidance template has wide application in the brachytherapy of postoperative recurrent cervical cancer with accurate localization, improved repeatability, short operation time, and a lower number of needles. However, further observation is essential to deduce the long-term efficacy and side effects of the technology.
Disclosure
The authors report that a patent is pending: Xiangkun Yuan, inventor; Beijing Unicorn Science And Technology Ltd., assignee. Positioning and guiding device for minimally invasive surgery for cervical cancer. Chinese patent 201820430815.7. 2018 Mar 29. The authors report no other conflicts of interest in this work.
References
1. Sardain H, Lavoue V, Redpath M, et al. Curative pelvic exenteration for recurrent cervical carcinoma in the era of concurrent chemotherapy and radiation therapy: asystema-tic review. Eur J Surg Oncol. 2015;41(8):975–985. doi:10.1016/j.ejso.2015.03.235
2. Li L, Ma SQ, Tan XJ, et al. Pelvic exenteration for recurrent and persistent cervical cancer. Chin Med J (Engl). 2018;131(13):1541–1548. doi:10.4103/0366-6999.235111
3. Chiantera V, Rossi M, De Iaco P, et al. Survival after curative pelvic exenteration for primary or recurrent cervical cancer: a retrospective multicentric study of 167 patients. Gynecol Cancer. 2014;24(5):916–922. doi:10.1097/IGC.0b013e3182a80aec
4. Ng MK, Leong T, Heriot AG, et al. Once-daily reirradiation for rectal cancer in patients who have received previous pelvic radiotherapy. Med Imaging Radiat Oncol. 2013;57:512–518. doi:10.1111/1754-9485.12057
5. Sadozye AH, Reed N. A review of recent developments in image-guided radiation therapy in cervix cancer. Curr Oncol Rep. 2012;14(6):519–526. doi:10.1007/s11912-012-0275-3
6. Yoshida K, Yamazaki H, Kotsuma T, et al. Treatment results of image-guided high-dose-rate interstitial brachytherapy for pelvic recurrence of uterine cancer. Brachytherapy. 2015;14(4):440–448. doi:10.1016/j.brachy.2015.02.195
7. Mabuchi S, Takahashi R, Isohashi F, et al. Reirradiation using high-dose-rate interstitial brachytherapy for locally recurrent cervical cancer: a single institutional experience. Gynecol Cancer. 2014;24(1):141–148. doi:10.1097/IGC.0000000000000028
8. Mahantshetty U, Kalyani N, Engineer R, et al. Reirradiation using high-dose-rate brachytherapy in recurrent carcinoma of uterine cervix. Brachytherapy. 2014;13(6):548–553. doi:10.1016/j.brachy.2014.06.005
9. Takekuma M, Kuji S, Tanaka A, et al. Platinum sensitivity and non-cross-resistance of cisplatin analogue with cisplatin in recurrent cervical cancer. Gynecol Oncol. 2015;26(3):185–192. doi:10.3802/jgo.2015.26.3.185
10. Aoki Y, Ochiai K, Lim S, et al. Phase III study of cisplatin with or without S-1 in patients with stage IVB, recurrent, or persistent cervical cancer. Br J Cancer. 2018;119(8):530–537. doi:10.1038/s41416-018-0206-7
11. Liu ZS, Guo J, Zhao YZ, et al. Dosimetric analysis of CT-guided salvage interstitial brachytherapy for recurrent cervical cancer. Chin J Radiat Oncol. 2018;27(1):74–78. doi:10.3760/cma.j.issn.1004-4221.2018.01.015
12. Haie-Meder C, Potter R, Van Limbergen E, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group(I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2005;74(3):235–245. doi:10.1016/j.radonc.2004,12.015
13. Potter R, Haie-Meder C, Van Limbergen E, et al. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (II): concepts and terms in 3D image-based 3D treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol. 2006;78(1):67–77. doi:10.1016/j.radonc.2005:11.014
14. Zolciak-Siwinska A, Bijok M, Jonska-Gmyrek J, et al. HDR brachytherapy for the reirradiation of cervical and vaginal cancer: analysis of efficacy and dosage delivered to organs at risk. Gynecol Oncol. 2014;132(1):93–97. doi:10.1016/j.ygyno.2013.10.018
15. Umezawa R, Murakami N, Nakamura S, et al. Image-guided interstitial high-dose-rate brachytherapy for locally recurrent uterine cervical cancer: asingle-institution study. Brachytherapy. 2018;17(2):368–376. doi:10.1016/j.brachy.2017.11.011
16. Kotsuma T, Yoshida K, Yamazaki H, et al. Preliminary results of magnetic resonance imaging-aided high-dose-rate interstitial brachytherapy for recurrent uterine carcinoma after curative surgery. Radiat Res. 2011;52(3):329–334. doi:10.1269/jrr.10172
17. Sethi R, Cunha JAN, Mellis K, et al. 3D printed custom applicator for high-dose-rate intracavitary vaginal cuff brachytherapy. Brachytherapy. 2014;13(1):S93. doi:10.1016/j.brachy.2014.02.371
18. Amsbaugh MJ, Bhatt N, Hunter T, et al. Computed tomography planned interstitial brachytherapy for recurrent gynecologic cancer. Brachytherapy. 2015;14(5):600–605. doi:10.1016/j.brachy.2015.05.007
19. Fokdal L, Tanderup K, Nielsen SK, et al. Image and laparoscopic guided interstitial brachytherapy for locally advanced primary or recurrent gynaecological cancer using the adaptive GEC ESTRO target concept. Radiother Oncol. 2011;100(3):473–479. doi:10.1016/j.radonc.2011.08.016
20. Fokdal L, Tanderup K, Hokland SB, et al. Clinical feasibility of combined intracavitary/interstitial brachytherapy in locally advanced cervical cancer employing MRI with a tandem/ring applicator in situ and virtual preplanning of the interstitial component. Radiother Oncol. 2013;107(1):63–68. doi:10.1016/j.radonc.2013.01.010
21. Wiebe E, Easton H, Thomas G, et al. Customized vaginal vault brachytherapy with computed tomography imaging-derived applicator prototyping. Brachytherapy. 2015;14(3):380–384. doi:10.1016/j.brachy.2014.12.006
22. Jiang P, Guo FX, Jiang YL, et al. 3D-printing non-coplanar template assisted CT-guided 125I seed implantation on pelvic recurrent cervical cancer. Chin J Radiol Med Pro. 2017;37(7):490–494. doi:10.3760/cma.j.issn.0254-5098.2017.07.003
23. Jiang YL, Wang H, Ji Z, et al. Computed tomography image-guided and personalized 3D printed template-assisted 125-iodine seed implantation for recurrent pelvic tumor: adosimetric study. Chin J Radiat Oncol. 2016;25(9):959–964. doi:10.3760/cma.j.issn.1004-4221.2016.09.012
24. Hongtao Z, Xuemin D, Huimin Y, et al. Dosimetry study of three-dimensional print template-guided precision 125I seed implantation. Cancer Res Ther. 2016;12(2):159–165. doi:10.4103/0973-1482.200607
25. Viswanathan AN, Beriwal S, De Los Santos JF, et al. American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part II: high-dose-rate brachytherapy. Brachytherapy. 2012;11(1):47–52. doi:10.1016/j.brachy.2011.07.002
26. Lewis SC, Mahantshetty U, Enginee R, et al. Reirradiation with high-dose-rate brachytherapy in recurrent cervical cancer - an update. Brachytherapy. 2016;15(1):S91–S91. doi:10.1016/j.brachy.2016.04.148
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

