Back to Journals » Clinical Ophthalmology » Volume 14
Donor Profile, Tissue Evaluation and Comparison of Voluntary and Motivated Corneal Donation in Nepal Eye Bank
Authors Bajracharya L , Bhandari SK, Twyana SN
Received 4 August 2019
Accepted for publication 26 November 2019
Published 14 January 2020 Volume 2020:14 Pages 95—101
DOI https://doi.org/10.2147/OPTH.S225922
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Leena Bajracharya, 1 Sachit Kumar Bhandari, 2 Shankha Narayan Twyana 3
1Department of Cornea, Tilganga Institute of Ophthalmology, Kathmandu, Province No. 3, Nepal; 2Tilganga Institute of Ophthalmology, Kathmandu, Province No. 3, Nepal; 3Nepal Eye Bank, Tilganga Institute of Ophthalmology, Kathmandu, Province No. 3, Nepal
Correspondence: Leena Bajracharya
Tilganga Institute of Ophthalmology, Gaushala, Bagmati Bridge, P. O. Box # 561, Kathmandu, Province No.3, Nepal
Tel +977 1 4493775
Fax +977- 1- 4474937
Email [email protected]
Purpose: Corneal problems is one of the major causes of blindness in developing countries like Nepal. This study intended to analyze donor and tissue profile of Nepal Eye Bank (NEB).
Material and Methods: This was a cross-sectional descriptive type study. Data of corneal tissues collected by NEB from January 2015 to December 2016 were used in the study. Data collected were demographic profile, cause of death, type of corneal donation (whether voluntary or motivated), quality and utilization of tissues. A comparison was made between voluntary and motivated donors.
Results: 1244 corneal tissues were retrieved from 639 donors. Mean age of donors was 49.4 years. 57.7% of the donors were male. There were almost equal number of donor deaths due to cardiovascular disease, 27.2%, and respiratory disease, 26.7%, followed by hanging, 17.8%. Majority of donors were motivated (n = 561, 87.7%). Mean death to preservation time was 5.79 hours (hrs). Of the harvested corneas, 1040 (83.6.%) were suitable for transplant with a mean endothelial cell count of 2850 ± 520 cells/mm 2; 16.4% were of poor tissue quality and 2.7% were seropositive. 76.2% of total tissues were of optical quality. Utilization rate of transplantable tissues was 97%. Tissues from motivated donors were significantly “younger” (p=0.0001), had better endothelial count (p=0.0001), and were of better quality (p=0.026) than those from voluntary donors.
Conclusion: Motivated eye donation is a major and effective source of cornea collection in the eye bank under study with “younger” and better quality corneas compared to voluntary donors.
Keywords: eye donation counselor, hospital corneal retrieval program, HCRP, Tilganga Institute of Ophthalmology, SightLife
Introduction
Diseases affecting the cornea are a major cause of blindness in developing countries like Nepal.1 Corneal blindness encompasses a wide variety of infectious, traumatic, congenital, nutritional and inflammatory eye diseases that cause corneal scarring, for which treatment is corneal transplantation.1 Corneal infection is the main reason for corneal transplant in developing countries like Nepal.2
Nepal Eye Bank (NEB) was established in 1994 with support of International Federation of Eye and Tissue Bank. NEB is a non-profitable organization located in the premises of Tilganga Institute of Ophthalmology, in Kathmandu City. Being the only eye bank in Nepal, it works on the principle of fair and equitable distribution of corneal tissue to surgeons all over the country.
The first years for NEB were challenging. Eye donation was a new concept in society. Various social organizations helped in creating public awareness. Cornea collection depended on voluntary calls from the family of the deceased. But despite continuous eye donation awareness programs in the commubity, cornea collecion could not increase .Then Eye bank staff started to visit crematoriums and got corneas by providing counseling to the family. From time to time, NEB also received corneas from international eye banks as support to treat corneal blindness. With time and growth of population, corneal blindness also increased and it became difficult for NEB to keep up with the demand for tissues and to sustain it.
In 2010, NEB became associated with SightLife, USA. Founded in 1969, SightLife is a non-profit global health organization focused on eliminating corneal blindness, 98% of which is in developing countries. Thereafter, Hospital Corneal Retrieval Program (HCRP) was initiated in the system of NEB. For this program, grief counselors (alternatively called “eye donation counselors”, EDCs) were recruited by NEB and were trained. General hospitals in the city were selected on the basis of high death rates. An agreement was made between the eye bank and the hospitals to allow EDCs to stay full time in the hospitals, who would then keep track of the deaths and counsel the family of the deceased for eye donation. Once consent is received, an eye recovery technician (ERT) is called to retrieve the cornea. A high volume crematorium was also selected for posting of EDCs. The following year after HCRP was started, corneal collection increased more than two fold. This shows the importance of the role of EDCs. HCRP proved to be the appropriate model in NEB.
NEB received a quality certificate in tissue collection and processing in 2015 from SightLife, USA. The current study was intended to find out information related to donors and tissues. It is the first study of this kind in Nepal and will help us to know the status of eye donation and provide data for future reference and studies.
Methodology
This was a cross-sectional study. All corneal tissues retrieved and registered in NEB over the course of 24 months from Jan 2015 to Dec 2016 were enrolled. Data were collected from NEB about demographic profile and cause of death of donors; type of corneal donation (whether voluntary or motivated), quality and utilization of tissues. Voluntary donation is the type of eye donation in which family members themselves call the eye bank to retrieve corneas of the deceased, most of whom had pledged eye donation during their lives. In motivated donation, an EDC approaches family members of the deceased and provide counseling to get consent for eye donation. EDCs work full time in hospitals or crematoriums, wait for death notification and proceed. In this study, a comparison was made between voluntary and motivated donors with respect to age of donor, death to preservation time (DPT), tissue quality and positive serology. For statistical analysis, chi-squared value was calculated. Chi-squared p value was obtained for statistical significance for all variables except for serology, in which p value was calculated from Fisher's extact test. All procedures like screening of donors, legal consent for eye donation, recovery of tissue, processing, evaluation and distribution of tissues were done by trained technicians in accordance with standard operating procedures of NEB. Tissues were stored in Cornisol media (Aurolab, Madurai, India) which has a storage time of 14 days at 2 to 8 degrees Celsius. Quality of tissues was ascertained on the basis of slit lamp (SL) biomicroscopy, specular microscopy (cannon eka 10), and endothelial cell density (ECD). Tissue evaluation was done at the beginning of storage. At least 100 cells were selected during specular microscopy for endothelial cell evaluation. Tissues were then regarded as “suitable” or “not suitable” for transplantation. The suitable tissues were further classified as optical (good to excellent grade tissues on SL evaluation with ECD of 2000/mm2 or above) or therapeutic (fair grade tissues on SL evaluation or ECD between 1500 to 2000/mm2). Unsuitable tissues are those with one or more of following: a) ECD less than 1500/mm2, b) poor quality in SL evaluation, c) positive serology for one or more of tests for human immunodeficiency virus (HIV) 1 and 2, Hepatitis B virus (HBV), Hepatitis C virus (HCV) or syphilis (Treponema pallidum haemagglutination test), d) inadequate donor blood sample for serology, e) any other reasons deemed unsuitable.
Ethical Consideration
Ethical approval was obtained from Institutional Review Board of Tilganga Institute of Ophthalmology.
Results
Number and Type of Corneal Donations
Total number of donors in the study period was 639. 561 (87.7%) donors were motivated and 78 (12.3%) were voluntary donors. In total, 1244 tissues were collected in the study period (1092 tissues from motivated and 152 from voluntary donors).
Motivation of donor families had been done through grief counseling in three hospitals and a crematorium (Table 1). The consent rate (number of families that gave consent divided by total number of families counseled) was 57%. All HCRP based hospitals and the crematorium are within 10 kilometer distance of NEB. Tribhuvan University Teaching Hospital and Pashupati Crematorium were major sources of tissues.
 |
Table 1 Source of corneal donors in Nepal Eye Bank |
Age and Sex
The mean age of donors was 49.4 years (range: 5–80 years). 33.6% of donors were below 40 years of age. 37.4% of donors were above 60 years (Figure 1), 57.7% were male.
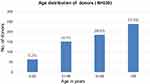 |
Figure 1 Age distribution of donors in years (N=639). Note: N= Number of Donors. |
Cause of Death
Most of the donors had died of cardiovascular diseases, closely followed by respiratory diseases. Considering hanging and poisoning together, suicidal cases made up 23.8%. Trauma was the cause of death for mostly male donors, 7.7 times more than in female donors (Table 2).
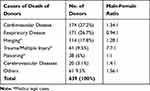 |
Table 2 Cause of death of corneal donors |
Ethnicity and Religion
Out of 639 donors, 29.2% were Newar ethnicity followed by Brahmins (27.2%) and Chhetris (21.4%). The remaining 22% constituted donors from ethnic groups of Mongol origin like Tamang, Limbu, Rai, Sherpa, Magar, and Gurung. Most of the donors belonged to Hindu religion (63.2%) followed by Buddhists (31%). 5.8% were of Muslim, Christian or Kirant religion.
Death to Preservation Time and Storage Media
Mean DPT was 5.79 hrs. 990 (79.5%) tissues were collected within 8 hrs of death (Figure 2). All corneas were retrieved by in-situ excision. 85% of the tissues were stored in Cornisol media, which is the intermediate term media and 15% in short term, McCarey-Kaufman (MK) media (LV Prasad, Hyderabad, India).
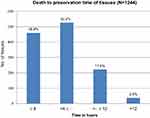 |
Figure 2 Distribution of Death to Preservation time of tissues (N=1244). Note: N= Number of Tissues. |
Quality of Tissues
Out of the total 1244 tissues collected, 1040 (83.6%) were suitable for transplantation. The transplantable tissues were graded as optical quality (76.2%) or therapeutic quality (7.3%). 204 (16.4%) were unsuitable for surgery. Table 3 shows the reasons why tissues are considered not suitable for transplantation. Majority (67%) of transplantable corneal tissues had ECD ≥ 2500 cells/mm2 (Figure 3). Mean ECD of transplantable tissues was 2857± 551 cells/mm2.
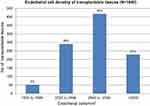 |
Figure 3 Distribution of Endothelial cell density of transplantable tissues (N=1040). Note: N= Number of transplantable tissues. |
Distribution and Utilization of Tissues
Out of 1040 transplantable tissues, 82% were used by corneal surgeons working in various parts of our country. Surplus corneas in NEB at any point of time (15%) are distributed to foreign countries as humanitarian support to South Asia region, where there has been a lack of corneal tissues. This made our utilization rate 97%.
Comparison of Motivated/HCRP and Voluntary Donation
Average age of voluntary donors was 61.3 years and that of HCRP was 48.1 years. Mean DPT for voluntary donor was 5.07 hrs and that of HCRP donor was 5.89 hrs. Table 4 shows that motivated donors provided younger tissues having higher ECD with statistical significance. Although tissue suitability rate between motivated and voluntary donors was the same, motivated donors provided significantly better quality (optical) corneas. It was found that voluntary donors' corneas were collected significantly earlier than those of motivated donors. Difference in the seropositivity rate was not significant in the two groups.
Discussion
The main source of corneal donors in NEB is through counseling the family of the deceased. This type of motivated eye donation collected corneas from three major hospitals of the Kathmandu city and a crematorium and accounted for 87.7% of total donors (Table 1). NEB has maintained a good relationship with hospitals and crematorium both at managerial and staff level to have their support in getting death notification, screening of donors, and continuity of the program. Besides working hours, EDCs and ERTs are available on call afterhours and on weekends. NEB also maintains community awareness about eye donation by liaising with social organizations. Before the initiation of HCRP, the eye bank used to rely mostly on voluntary donors, whose proportion has currently decreased. The motivated collection of cornea in eye banks in various parts of India ranges from 69 to 86% which is similar to our studies.3–5 Some eye banks in India rely mostly on home deaths with collections from 71 to 75.2% of the tissues.6–8 In our study, all HCRP donors (87.7%) were within 10 kilometers of the eye bank (Table 1) unlike in the study of Desar et al, where the distance to travel to get corneas was more than 60 km in one third of the donors.6 NEB is in a favorable location, which is an advantage for shorter tissue excision and preservation time.
In our study, average DPT was 5.7 hrs (Figure 2), which is similar to that reported by Sharma et al.5 Other reports mentioned averageDPT of 2.8 to 3.9 hrs.3,7,9 Cunningham et al10 mentioned longer DPT of 18.5 hrs. DPT varies with the climate and ambient temperature. Hence, it varies from one geographic region to another. Our DPT, in the climate of Kathmandu city, has been within 8 hrs (in summer with average maximum temperature of 30° Celsius) to 15 hrs (in winter with average maximum temperature of 20° Celsius) after death.
In our study, donor deaths were mostly due to cardiovascular disease, 27.2%, closely followed by respiratory disease, 26.7% (Table 2). In eye banks of India, Brazil, and New Zealand also, cardiovascular morbidity was the major cause for donor deaths ranging from 34% to 50.5%.3,5,9,11 Respiratory disease accounted for 7%, as reported by Patel et al11 in New Zealand. In our community, lack of timely treatment of chest infections in elderly people could be the reason for high proportion of respiratory disease. In our study as well as in that of Sharma et al,5 hanging accounted for 18% of deaths and was the third cause of donor death. Road traffic accident was the cause of death in 12% to 30% of donors in other eye banks, compared to 9.5% in our study.3,5,11 Medico legal cases (hanging, poisoning, and trauma) accounted for 33.3% of all donor deaths because we have counselors posted in the high volume autopsy department of a donor hospital. This could be one reason for the “young” corneas in our study.
In our study, average age of donors was 49.7 years (Figure 1), which is less than in developed countries with a range of 56.8 to 69 years.9,10,12 In India, it ranged from 52 years to 69 years in different eye banks.3,4,7 Age is one criteria for good quality corneas.
Male donors made up 57.7% in our study. There has been male preponderance in many eye banks (57 to 68%).4–6,8,10,12,13 This could be because cardiovascular diseases and trauma were important causes of donor deaths in most eye banks, which could have occurred more in the male gender, like in our study (Table 2).
29% of donors belonged to Newar ethnic community who are the natives of Kathmandu valley followed by Brahmins and Chhetries. 63% belonged to Hindu religion and 31% were Buddhists. This is explained by Nepal being a Hindu predominant country.
In the past, in NEB, all tissues were stored in short term MK media but recently it is being replaced by Cornisol for all tissues. Preservation in Cornisol, which is an intermediate term media, has given more flexibility to the eye bank in terms of distribution and tissue utilization. In India, most eye banks use MK media followed by Cornisol and Optisol media (Bausch and Lomb, St Louis Missouri).3,8 Longer term storage media like organ culture is used in New Zealand.10
NEB has trained EDCs and ERTs who thoroughly screen the donors for any contraindications and also carefully examine the tissues prior to harvesting them. This could be the reason why 83.6% of total tissues collected were suitable for transplantation. Other studies reported rates of 71% to 90%.10,11 Dasar et al6 and Gohel et al7 reported suitability rate of 36% to 43%, where voluntary donation was the main source of cornea donation.
In our study, 2.7% of tissues were found to be seropositive (Table 3). In the studies of Basak et al,4 Raj et al,13 and Sharma et al,5 2.2% to 3.8% of donors had shown positive serology for either HIV, HBV, HCV or syphilis. Some eye banks exclude syphilis in screening tests of corneal donors and reported seropositivity (HIV/HBV/HCV) of 3.9 to 5.6%.10,11,14
 |
Table 3 Tissues not suitable for surgery |
Mean ECD of transplantable tissues was 2850±520 cells/mm2 in our study (Figure 3), which is comparable to those reported by other eye banks of 2857 to 3024 cells/mm2.3,11 In our study, 76.2% of tissues were optical grade. Sharma et al8 mentioned cumulative proportion of optical grade tissue in India as 59.6%.
97% of transplantable tissues were used for surgery in our eye bank, compared to 88% reported by Cunningham et al.10 In India, utilization rate in various eye banks varied from 50.5% to 75%.3,8,15 NEB distributes tissues to surgeons within the country on a fair and equitable basis. They can get tissues from NEB without much waiting time. It is mandatory that NEB gives priority to Nepali surgeons and patients. If there are surplus tissues and if there has not been any request from surgeons within or if patients want to postpone the surgery, then in such situations, tissues are sent for use outside the country. This explains our high utilization rate.
In comparison with voluntary donors (Table 4), HCRP had a significantly higher proportion of younger donors and higher ECD (p=0.0001 for both variables). Although suitability rates of tissues collected were similar in both the groups (p= 0.829), the proportion of optical tissues was significantly higher in motivated donors (p= 0.026). Sharma et al also drew a similar conclusion about HCRP and voluntary donors, with statistical significance.5 Voluntary donors are mostly from highly motivated communities and the eye bank is contacted as soon as a death occurs. Whereas in HCRP, some time is spent waiting for the right moment to approach the family, and the family could also take some time to decide. Time is also taken up in case of medico legal cases, waiting for the release of the body. These could be the reasons why DPT was statistically shorter in voluntary donors (p=0.0001). Sharma et al5 also found shorter DPT in voluntary donors in her study, with statistical significance.
 |
Table 4 Comparison of Motivated (or HCRP) and Voluntary Eye Donation |
Conclusion and Recommendation
Motivated eye donation provides “younger” corneas with better quality. The increase in cornea collection in recent years is attributed to the success of HCRP and trained grief counselors. A good, strong relationship between donor hospitals and the eye bank is necessary for success and continuity of HCRP. For the eye bank’s growth, HCRP can be extended to more hospitals. There should be regular training for eye bank staff, not only for better performance, but also for good quality corneas which are very important for better surgical outcomes. Community awareness also has to be maintained.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ. 2001;79:214–221.
2. Bajracharya L, Gurung R, DeMarchis EH, Oliva M, Ruit S, Tabin G. Indications for keratoplasty in Nepal: 2005–2010. Nepal J Ophthalmol. 2013;5:207–214. doi:10.3126/nepjoph.v5i2.8730
3. Ranjan A, Das S, Sahu SK. Donor and tissue profile of a community eye bank in Eastern India. Indian J Ophthalmol. 2014;62:935–937. doi:10.4103/0301-4738.138298
4. Basak S, Basak SK, Biswas B. Comparison of seropositivity of human immunodeficiency virus, hepatitis B virus, hepatitis C virus, and syphilis among Hospital Cornea Retrieval Programme-Donors versus voluntary cornea donors at a large eye bank in Eastern India. Indian J Ophthalmol. 2017;65:1138–1142. doi:10.4103/ijo.IJO_472_17
5. Sharma N, Agrawal N, Maharana PK, Agrawal T, Vanathi M, Vajpayee RB. Comparison of hospital cornea retrieval and voluntary eye donation program in eye banking. Eye Contact Lens. 2018;44:S54–S58. doi:10.1097/ICL.0000000000000320
6. Dasar LV, Jayashree MP, Gill KS. Demographic profile of eye-donors of southern India. J Pharm Biomed Sci. 2012;16:1–7.
7. Gohel DJ, Kamath MA, Bhosale DA, Gadhavi BN. Donor and tissue profiling at the time of eye donation at a tertiary care hospital in western India. Int J Community Med Public Health. 2018;5:2349–2351. doi:10.18203/2394-6040.ijcmph20182156
8. Sharma N, Arora T, Singhal D, et al. Procurement, storage and utilization trends of eye banks in India. Indian J Ophthalmol. 2019;67:1056–1059. doi:10.4103/ijo.IJO_1551_18
9. Adán CB, Diniz AR, Perlatto D, Hirai FE, Sato EH. Ten years of corneal donation to the Hospital São Paulo Eye Bank: characteristics of cornea donors from 1996 to 2005. Arq Bras Oftalmol. 2008;71:176–181. doi:10.1590/s0004-27492008000200009
10. Cunningham WJ, Brookes NH, Twohill HC, et al. Trends in the distribution of donor corneal tissue and indications for corneal transplantation: the New Zealand National Eye Bank Study 2000–2009. Clin Exp Ophthalmol. 2012;40:141–147. doi:10.1111/ceo.2012.40.issue-2
11. Patel HY, Brookes NH, Moffatt L, et al. The New Zealand National Eye Bank study 1991–2003: a review of the source and management of corneal tissue. Cornea. 2005;24:576–582. doi:10.1097/01.ico.0000155035.55751.b2
12. Chopra GK, De Vincentis F, Kaufman D, Collie D. Effective corneal retrieval in a general hospital. The royal Melbourne Hospital Eye Bank. Aust N Z J Ophthalmol. 1993;21:251–255. doi:10.1111/ceo.1993.21.issue-4
13. Raj A, Mittal G, Bahadur H. Factors affecting the serological testing of cadaveric donor cornea. Indian J Ophthalmol. 2018;66:61–65. doi:10.4103/ijo.IJO_656_17
14. Mahalakshmi B, Madhavan HN, Pushpalatha R, Margarita S. Seroprevalence of human immunodeficiency virus, hepatitis B virus and hepatitis C virus among eye donors. Indian J Ophthalmol. 2004;52:61–62.
15. Gogia V, Gupta S, Agarwal T, Pandey V, Tandon R. Changing pattern of utilization of human donor cornea in India. Indian J Ophthalmol. 2015;63:654–658. doi:10.4103/0301-4738.169790
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
