Back to Journals » Risk Management and Healthcare Policy » Volume 13
Does Youth-Friendly Service Intervention Reduce Risky Sexual Behavior in Unmarried Adolescents? A Comparative Study in West Gojjam Zone, Northwest Ethiopia
Authors Mekonnen Munea A, Alene GD, Debelew GT
Received 20 March 2020
Accepted for publication 25 June 2020
Published 31 July 2020 Volume 2020:13 Pages 941—954
DOI https://doi.org/10.2147/RMHP.S254685
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Marco Carotenuto
Alemtsehay Mekonnen Munea,1 Getu Degu Alene,1 Gurmesa Tura Debelew2
1School of Public Health, Bahir Dar University, Bahir Dar, Ethiopia; 2Department of Population and Family Health, Institute of Health, Jimma University, Jimma, Ethiopia
Correspondence: Alemtsehay Mekonnen Munea Email [email protected]
Background: Risky sexual behavior established during adolescence adversely affect young people’s health and well-being. Youth-friendly services (YFS) programs are believed to improve the sexual and reproductive health of adolescents. Little is known about the effect of YFS programs on adolescents’ sexual behavior in Ethiopia. Therefore, this study assessed the sexual behavior of unmarried adolescents in YFS-program and nonprogram areas and factors contributing to their sexual behavior in West Gojjam Zone, Northwest Ethiopia.
Methods: This community-based comparative cross-sectional study was conducted among 1,125 randomly selected unmarried adolescents (545 from program areas and 580 from nonprogram areas) in June 2018. Data were collected in face-to-face interviews using a pretested questionnaire and analyzed using SPSS version 21. Between groups, comparisons were made using χ2 and t-tests. A hierarchical logistic regression model was employed to identify important variables explaining risky sexual behavior.
Results: Of all respondents, 305 (27.1%) had risky sexual behavior, which was comparable between the YFS-program and nonprogram areas (25.0% vs 29.1%, p=0.12). Including YFS program-related variables in the hierarchical regression model did not improve the explanation of risky sexual behavior over the individual attributes. On the other hand, including interpersonal-related variables (eg, with parents) significantly improved the explanation of risky sexual behavior over and above individual attributes and YFS program–related variables. A point increase in parent–adolescent communication score reduced risky sexual behavior by 20% (AOR 0.80, 95% CI 0.75– 0.85). Being female, being older, having knowledge on family planning and HIV, out of school, and watching pornography were associated with higher odds of engaging in risky sexual behavior.
Conclusion: Risky sexual behavior was comparable between settings. Parent–adolescent communication about sexual and reproductive health issues is more important in predicting adolescents’ risky sexual behavior than other variables. Therefore, interventions should give emphasis to parent–adolescent communication to reduce adolescents’ risky sexual behavior.
Keywords: risky sexual behavior, parent–adolescent communication, youth-friendly services
Plain Language Summary
Despite the great attention given to the field of adolescent sexual and reproductive health (ASRH), young people are largely affected by SRH problems. Youth-friendly services (YFS) programs are believed to reduce SRH problems through improving knowledge, attitudes, and service utilization. Although risky sexual behavior has been widely investigated, little is known about the effect of YFS programs on adolescents’ sexual behavior in Ethiopia. This study aimed to compare the magnitude of risky sexual behavior and associated factors among 1,125 unmarried adolescents residing in YFS-program (545) and nonprogram areas (580). The descriptive analysis indicates that compared to the nonprogram areas, the proportion of adolescents who had knowledge on family planning, HIV, and positive attitudes toward condom use was higher in the program area. Despite these encouraging findings, the proportion of adolescents with risky sexual behavior in the two settings was comparable, which contradicts the main objective of introducing YFS programs. On hierarchical regression analysis, residing in a YFS-program area was not significantly associated with risky sexual behavior. Also, increased attitude score and knowledge on family planning and HIV increases risky sexual behavior. However, the inclusion of interpersonal-related variables (eg, parent–adolescent communication about SRH) significantly improved the goodness of fit of the model over individual attributes and program-related variables. Parent–adolescent communication on SRH issues decreased the odds of risky sexual behavior by 20%. To improve adolescent sexual behavior, programs should give due emphasis on parent–adolescent communication on sexual issues.
Introduction
Among the 7.8 billion people worldwide, 20% (1.2 billion) are adolescents, and of these, 85% live in developing countries.1 Sub-Saharan Africa is the only region of the world in which the number of young people continues to grow substantially.2 In Ethiopia, nearly 25% of the population is in the adolescent age-group (15–19 years).3
Adolescence is a transition period from childhood to adulthood during which young people become independent individual, begin to form new relationships, and experience their sexuality, and it is characterized by vulnerability and opportunity.4–6 Engagement in risky behavior, such as substance use, violence, and unsafe sexual practices, are common during adolescence and significant public health concerns.6
Risky sexual behavior are defined as an individual’s sexual practices that may increase the vulnerability of a person for the risk of sexually transmitted infections (STIs) including HIV/AIDS and unplanned pregnancy. Some of these behavior include unprotected sexual intercourse, multiple sexual partners, and sexual intercourse with commercial sex workers.7 Risky sexual behavior among adolescents have direct and indirect impact on social and economic well-being, such as an increase in maternal and infant mortality, school dropouts, HIV/AIDS prevalence, substance abuse, and suicidal deaths.8
Every year, an estimated 23 million adolescents become pregnant: half of it is unplanned and ending in unsafe abortion.9–11 Early childbearing is linked with higher maternal morbidity, which leads to intergenerational cycles of ill health and poverty, as well as higher maternal mortality.12 Moreover, young people represent a growing share of age-groups living with HIV in developing countries. In 2018, about 1.6 million adolescents were living with HIV worldwide, of which 1.5 million were in sub-Saharan Africa. This region also had about 70% of new infections, of which youth accounted for the largest proportion.13
Young people in Ethiopia are at risk of a broad range of sexual and reproductive health (SRH) problems, such as unwanted pregnancy, unsafe abortion, pregnancy-related complications, and STIs.14–17 They also have high unmet needs for family-planning utilization and limited awareness of STI prevention.17,18 Although Ethiopia ihas been registered as one of the lowest HIV-prevalence countries in East Africa,19 recent reports have indicated that the incidence is rising again. For example, Girum et al20 reported that HIV prevalence in Addis Ababa, Gambela, and Hareri was 4.8%, 4.5%, and 3%, respectively. With the current prevalence rate, UNICEF has also projected that new infections among adolescents in Ethiopia will have increased by 60% (400,000 annually) by 2030.21 Despite this, knowledge of HIV prevention and condom utilization in Ethiopia is low.22,23 As such, HIV will remain a leading cause of death among adolescents in the country.21
Recognizing that youth are vulnerable to SRH problems and existing health services not ideal for youth, the international community in 1994 recommended services that respect youths’ privacy and confidentiality.24 Since then, the World Health Organization has been promoting YFS programs to improve the SRH of the young generation.25
YFS programs are believed to improve the SRH of adolescents via improving their knowledge, attitudes toward SRH services, and behavior by providing ranges of comprehensive SRH services. These services are information and counseling on SRH issues, promotion of healthy sexual behavior through various methods, including peer education, family-planning information, counseling and methods provision, condom promotion and provision, testing services (pregnancy, HIV counseling and testing), management of STIs, abortion and postabortion care, pregnancy tests, and other maternal-health services with appropriate referral linkage between facilities.26
In Ethiopia, a YFS program was commenced by nongovernmental organizations in line with the government’s policy and strategy in 2005–2006.27 For the effective implementation of the program, standards, delivery guideline, and a minimum service-delivery package on YFS programs were developed and implemented.28,29 The government runs the program, and is implementing an age-driven approach in existing public health facilities. Moreover, peer educators provide community- and school-based SRH information by providing more emphasis on reduction of early sexual initiation, unsafe sex, and its complications, and promotion of SRH-service utilization.26,27 To date, 44.7% and 53.5% of health facilities have implemented YFS programs in Ethiopia overall and the Amhara region, respectively.26,30
Evidence in other countries has indicated that YFS programs are cost-effective and contribute to better health among young people through reducing SRH problems, such as unwanted pregnancies, new HIV infections, STIs, and increased overall service utilization.31–33 Studies in Ethiopia27,34 have reported that YFS programs increase adolescents’ SRH-service utilization. Little is known about the effects of YFS programs on adolescents’ sexual behavior in the country.
A number of studies in Ethiopia35–37 and other countries8,38–40 assessing the sexual behavior of adolescents have reported that parent–adolescent communication has a significant role in reducing adolescents’ risky sexual behavior. Adolescents with good parental communication regarding SRH issues were more likely to engage in safe sexual behavior, including abstinence,8,35,36 delaying first sexual intercourse, fewer lifetime sexual partners, and using condoms,35,38,39 and less likely to experience teenage pregnancy.37 This study elucidates whether YFS programs or parent–adolescent communication are important in explaining adolescents’ sexual behavior. Based on the existing literature, we hypothesized that parent–adolescent communication on SRH issues is more important in predicting adolescents’ sexual behavior than YFS programs and individual attributes.
In this study, ecological framework was employed to understand determinants of adolescent sexual behavior. The framework recognizes multiple influences on health behavior, including factors that operate at the individual, interpersonal, organizational, community, and public-policy levels.40 Therefore, grouping of variables in this study was conceptualized based on this ecological framework. Individual, interpersonal, and organizational (YFS program)–related variables were used for analysis.
Methods
Study Design and Setting
A community-based comparative cross-sectional study was conducted to assess the sexual behavior of unmarried adolescents in West Gojjam, Amhara region, northwest Ethiopia. West Gojjam zone is one of the 15 zones in the Amhara region. It has 13 rural districts and two city administrations, with 362 and 15 rural and urban kebeles (the lowest administrative unit), respectively. There are 104 government health centers in the zone providing basic health services, including SRH. Of all health centers, 59 have YFS programs.41
Study Population and Inclusion Criteria
Unmarried adolescents aged 15–19 years with parents/guardians and residing within a 5 km radius of the selected health facilities (both for YFS-program and nonprogram areas) for at least 1 year were included in the study.
Sample-Size Determination
The sample size was calculated using a two population–proportion formula employing EpiInfo version 7.2.2.2. The proportion of SRH-service use in nonprogram areas (p1=40%) was taken from a previous study,42 and the proportion of SRH-service utilization in program areas (p2) was computed by assuming a 15% additional fraction (f) of respondents in program areas utilizing SRH services:43
p2 = p1 + f (1 – p1)
where p1 is the proportion of adolescents using SRH services in nonprogram area (40%), p2 the proportion of adolescents using SRH services in the program area, and f the assumed additional fraction of respondents utilizing SRH services in program areas (15%). Finally, sample sizes required in each comparison group were calculated:43
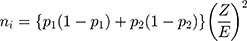
where ni is the sample size required in each group, Z the value of 95% CI (1.96), and E the desired margin of error (5%), with p1 40%, p2 49%, 80% power, and 15% nonresponse rate. A total of 1,204 participants (602 from program areas and 602 from nonprogram areas) were included in the study.
Sampling Procedure
The study was conducted in the catchment areas of two YFS-program and two nonprogram health facilities. There were two major steps in the sampling procedure. The first step was health-center selection. Selection of health centers from the YFS-program area was done based on the quality of services on offer to clients/patients identified by a former study on the quality of YFS programs in the area (the current study is an extension of that one).44 The preceding study identified two health centers providing YFS programs of good quality. These two health centers were considered in the current study. Two health centers where YFS programs were not available (nonprogram areas) were randomly selected for comparison. Further assessment was done on these health centers to ensure whether they were appropriate for comparison. Health centers without provider trained in YFS, any separate room for YFS, or had not introduced a YFS program at all were used as criteria to select nonprogram health facilities.
The second step was participant selection. The 5 km radius (considering distance as a barrier to health-service utilization) from the selected health facilities was estimated by GPS and delineated the area, together with kebele officials. Distance between the selected program and nonprogram areas was considered a buffer zone to minimize information contamination. However, the contribution of the national health program of the country (health-extension program) was assumed to be evenly distributed in both settings. Adolescents aged 15–19 years and living within the delineated catchment areas of the selected health facilities participated in the study.
Household listing was conducted within the 5 km radius from the selected health facilities prior to the survey. Eligible households (with unmarried adolescent/s) were identified and the sampling frame established using a separate sheet. Selection of participants from each setting was done using a computer-generated random-number technique. Accordingly, equal numbers (602) of households from program and nonprogram areas were selected. In households with more than one adolescent, a lottery method was used to select one of them at the time of data collection.
Data-Collection Tool and Procedure
Data were collected using a structured questionnaire developed from the literature.38,45,46 It was first prepared in English, then translated into the local language (Amharic) to ease understanding. The instrument was pilot-tested and reliability of attitudes and parent–adolescent discussion items computed before final administration. Also, based on the pilot result, some items were modified prior to the survey, eg, minimum age of respondents (≥15 years) and alternative wording for sexual intercourse (some people call it “sleeping together”).
Data collectors and supervisors underwent 4 days’ training on the purpose of the study, the content of the questionnaire, and interviewing techniques, such as asking questions, clarifying questions, probing, recording responses, and data quality. Discussion, demonstration, and role-playing techniques were employed during training. Data were collected through face-to-face interviews using the Amharic-version questionnaire at a convenient place for each respondent.Interview were same-sex ones and monitored by supervisors.
Variables and Measurement
Sexual behavior was the outcome variable in this study. Respondents were asked whether they had ever had sexual intercourse or not. Those who had had sexual intercourse were again asked about age at first sexual intercourse, number of sexual partners, and condom utilization. Respondents who had at least one of behavior among sexual debut before age 15 years, inconsistentcondom use (or not using condoms at all) in the last 6 months, and multiple sexual partners were classified as engaging in risky sexual behavior36 and were “1”. The remaining (ever abstained, secondary abstinence or consistent condom use for the last 6 months) were classified as engaging in safe sexual behavior and coded “0”. “Secondary abstinence” referred to unmarried adolescents who were sexually active, but had abstained from sex for the 12 months prior to the survey.
Independent variables in this study comprised individual-related variables (eg, age, sex, current schooling status), YFS program–related variables (eg, knowledge and attitudes toward SRH issues, SRH-service utilization), and interpersonal related variables (eg, parent–adolescent communication on SRH issues and peer influence). The interpersonal variables parent–adolescent communication on SRH issues, parental attitudes toward SRH-service use by unmarried adolescents, and parent knowledge on SRH were taken from data collected for other purposes from parents in the same household (dyadic data). Variables were then assessed.
Consistent condom use was measured based on the question “How often do you use a condom?” Responses were: 1 always, 2 = often, 3 = sometimes, and 4 = never. Respondents who reported always using condoms in the last six months were considered to be using condoms consistently. Peer influence was assessed using four items with binary responses. Respondents were asked to think their three closest friends and whether their friends had ever had sexual intercourse, used condoms, had a positive opinion toward condom use, and whether they approved of premarital sex. The sum value ranged 0–12, and mean values were used to categorize respondents into two groups. Those with totals equal to or above the mean were regarded as having positive peer influence.
For attitudes toward SRH services, eight items were used (eg, whether contraceptive, condom, SIT diagnosis, and treatment service used by unmarried adolescents were acceptable) on a four-point Likert scale: 1 = strongly disagree, 2 = disagree, 3 = agree, and 4 = strongly agree. The items had good internal reliability (Cronbach’s α=0.71). Sums of responses ranged 8–32, where a higher value indicates favorable attitudes toward the service. “Unmarried adolescent” referred to someone in the age-group between 15–19 years and not in a union that had been accepted by the community orconsidered a legal marriage.
With regard to SRH-service utilization, utilization of at least oneSRH service at the nearby health center either for curative (STI diagnosis and treatment, pregnancy test, abortion service) or preventive purposes (condoms, other contraceptives,HIV testing, SRH-related information, counseling on SRH).47 For knowledge on family planning, adolescents were asked to name types of family-planning methods, and if they listed at least three (includes two modern), they were considered knowledgeable,48 while for comprehensive knowledge on HIV, they were asked five questions related to HIV, and those who responded correctly on all items were considered knowledgeable.48
Parent–adolescent communication on SRH issues was measured using eight items (eg, “How often have you ever talked about contraception, HIV/AIDS, or premarital sex with your unmarried adolescent?”) on a four-point Likert scale (1 = never, 2 = sometimes, 3 = many times and 4 = always). The items had good internal consistency (Cronbach’s α=0.79). After centering, sum values ranged 0–24, where higher values indicated good parent–adolescent communication on SRH issues.49,50 For parental knowledge on SRH, eight items, including contraception, HIV, physiology of fertility (eg, menarche year, ovulation time), and STI prevention (eg, condom use), were asked about, and higher scores indicated good knowledge.
Data Analysis
Data were entered, cleaned, and analyzed using SPSS for Windows version 21. Descriptive analysis was used to summarize the data. Between-group comparisons (YFS-program and nonprogram areas) were performed using the χ2 test of independence for categorical variables and independent-sample t-tests for continuous variables. Variables with P<0.2 on bivariate analysis were entered into multivariable logistic regression analysis. Adolescents’ educational level, wealth index, SRH-service utilization, and maternal education status were removed from the analysis, due to multicollinearity with current schooling status, pocket money, adolescents’ knowledge on SRH, and parents’ knowledge on SRH, respectively. Model fitness was checked using the receiver–operating characteristic curve, and the predictive value was significant.
A hierarchical regression model was used to test whether YFS programs or parent–adolescent communication were important in predicting the sexual behavior of adolescents. This model shows if variables of interest explain a statistically significant amount of variance in the dependent variable after controlling for all other variables. In the analysis, several regression models can be built by adding variables to a previous model at each step. Of importance is to determine whether the newly added variables show a significant improvement in R2 (proportion of variance explained in the dependent variables by the model).51
Based on the ecological framework, the first model (model I) included demographic information, such as age, sex, and schooling status. Model II consisted of program-related variables, such as program/nonprogram area, knowledge on family planning, and comprehensive knowledge on HIV. In the final model (model III), interpersonal-related variables, such as parent–adolescent communication on SRH, and peer influence, were added. Difference in R2 between models II and III and −2LL were used to assess model improvement in explaining the sexual behavior of adolescents. P≤0.05 was considered the cutoff for significance.
Ethical Considerations
Ethical clearance was obtained from the Institutional Review Board (IRB) of Bahir Dar University College of Medicine and Health Sciences. Before the household listing, a support letter was obtained from the Amhara Public Health Institute and submitted to the Zonal Health Office. Offices were communicated with using the post. Verbal informed assent and consent was acceptable and approved by the IRB of Bahir Dar University, and this study was conducted in accordance with the Declaration of Helsinki. All data were given an identification number and anonymously processed.
Results
Sociodemographic Characteristics
Of the total 1,125 (545 from program areas and 580 from the nonprogram areas) unmarried adolescents included in the analysis, 625 (55.6%) were males. A majority, 652, 58), were aged 18–19 years (mean 17.6±1.4 years). Amhara was the predominant ethnic group, (1,103, 98%). The leading religion was Orthodox Christian (1,111, 98.7%). More than a third (385, 34.2%) of respondentswere out of school at the time of data collection. (Table 1).
 |
Table 1 Distribution of Sociodemographic Characteristics of Respondents by Program and Nonprogram Areas in West Gojjam Zone, Northwest Ethiopia, June 2018 |
Behavior-Related Characteristics
Respondents were asked about how frequently they attended religious services, and375 (68.4%) from program areas and 347 (64.5%) from nonprogram areas attended sometimes. Nearly three quarters (71.9%) of participants from program areas and 541 (93.3%) from nonprogram areas ever consumed alcohol. More than a quarter of respondents (28.3%) from program areas and 184 (31.7%) from nonprogram areas ever watched pornography (Table 2).
 |
Table 2 Distribution of Behavior-Related Characteristics of Unmarried Adolescents by Program/Nonprogram Areas in West Gojjam Zone, Northwest Ethiopia, June 2018 |
SRH-Related Knowledge and Attitudes
Compared to nonprogram areas, the proportion of adolescents who had knowledge on family planning, HIV, and SRH-service use was significantly higher in program areas. More than a quarter (158, 28.7%) of adolescents in program areas and 109 (18.8%) in nonprogram areas approved of premarital sex, and the difference was statistically significant (P<0.001. The proportion of adolescents with favorable attitudes toward condom use was also significantly higher in program areas (40.0% vs 19.7%, P=<0.001). Parent–adolescent communication on SRH issues was significantly higher inprogram areas (t1,123=−3.5, pP<0.001; Table 3).
 |
Table 3 Distribution of Unmarried Adolescents by SRH-Related Knowledge and Attitudes Between Program/Nonprogram Areas in West Gojjam Zone, Northwest Ethiopia, June 2018 |
Sexual Behavior of Unmarried Adolescents
Of all respondents, 409 (36.4%) had had sexual intercourse. The mean age of sexual debut was 16.9±1.2 years and 254 (62.0%) had started before the age of 18 years. proportions of adolescents who had had sex and for age at first sex were comparable between program and nonprogram areas. A total of 72 adolescents (17.6%) — 39 (20.6%) in program areas and 33 (15%) in nonprogram areas — had had two sexual partners. Of those adolescents who had ever had sex (327, 80%), 165 (83.7%) in program areas and 162 (73.6%) in nonprogram areas had had sex in the past 12 months. Only 98 (24.0%) respondents had ever used condoms. Condoms were used consistently by 13 (8.1%) in program areas and 9 (5.4%) in nonprogram areas while having sex in the last 6 months (Table 4). As indicated in Table 5, proportions for all sexual behavior were comparable between settings. The overall prevalence of risky sexual behavior was 305 (27.1%, 95% CI 24.7%−29.7%), which was divided comparably between program (25.0%) and nonprogram (29.1%) areas (P=0.12, Table 5).
 |
Table 4 Distribution of Unmarried Adolescents’ Sexual Behavior Between Program/Nonprogram Areas in West Gojjam Zone, Northwest Ethiopia, June 2018 |
 |
Table 5 Distribution of Unmarried Adolescents by Sexual Behavior Risk Between Program/Nonprogram Areas in West Gojjam Zone, Northwest Ethiopia, June 2018 (n=1,125) |
Factors Associated with Risky Sexual Behavior
As indicated in model I, sex, age, schooling, religious attendance, and watching pornographic film significantly predicted risky sexual behavior in unmarried adolescents. Compared to those attending school, adolescents who had left school were 2.5 (95% CI 1.59–2.98, P<0.001) times more likely to engage in risky sexual behavior. A 1-year increase in age, increases risky sexual behavior nearly two-fold (95% CI 1.59–2.12, P<0.001). Among the four program-related factors considered in model II, adolescentknowledge on family planning had significant associations with sexual behavior. Adolescents who had poor knowledge on family planning were 0.39 times less likely to engage in risky sexual behavior (95% CI 0.27–0.57, P<0.001).
The final model (model III) added five interpersonal-related variables. The results indicated that individual-related variables (sex, age, schooling status, and watching pornography), program-related variables (knowledge on family planning, knowledge on HIV/AIDS, and attitudes on SRH-service use), interpersonal-related variables (parent–adolescent communication on SRH and parental attitudes toward SRH-service use) were significantly associated with risky sexual behavior.
Adolescents who had no knowledge on family planning were 0.36 times less likely to engage in risky sexual behavior (95% CI 0.24–0.53, P<0.001) than their counterparts. A one-point increase in adolescents’ attitudes toward SRH-service use (eg, agreed with condom and other contraceptive use by unmarried adolescents) meant they were 1.09 times more likely to engage in risky sexual behavior (95% CI 1.04–1.14, P<0.01). On the other hand, a one-point increase in parent–adolescent communication decreased the risk of engaging in risky sexual behavior by 20% (P<0.001).
The inclusion of interpersonal-related variables in model III significantly improved its goodness of fit compared to model II (χ215=338, P<0.001). While model II explained 31% of variance in risky sexual behavior (Nagelkerke’s R2=0.31), model III explained 38% of variance in risky sexual behavior (Nagelkerke’s R2=0.38). The data indicated that relational variables explained an additional 7% of variance in risky sexual behavior (Table 6).
 |
Table 6 Hierarchical Logistic Regression Model of Unmarried Adolescents’ Individual Attributes, Program, and Interpersonal-Related Variables, West Gojjam Zone, Northwest Ethiopia, June 2018 (n=1,125) |
The results indicated that there was a statistically significant improvement in predicting sexual behavior of unmarried adolescents with parent–adolescent communication on SRH after controlling for other variables. As we hypothesized, parent–adolescent communication on SRH issues better predicts the sexual behavior of unmarried adolescents than their individual attributes or YFS program–related variables alone.
Discussion
This study demonstrated that a significant number of unmarried adolescents engaged in risky sexual behavior. More than a quarter (27.1%, 95% CI 24.7%−29.7%) of adolescents had risky sexual behavior in the past 12 months preceding the survey. This finding was lower than other studies in Ethiopia (62%, 49.1%, and 43.1%) and Zambia (72.2%).16,53–55 The difference might be related to characteristics of the study population, methods employed, and study settings. Those studies cited were conducted in institutions, among students, in an urban setting, and used self-administered questionnaires, which may minimize underreporting of adolescent sexual behavior.
On the other hand, our finding was slightly higher than another studies conducted in northwest Ethiopia — Jiga (14.7%).16 This difference may be attributed to the approaches used to measure risky sexual behavior. In previous research, risky sexual behavior has been measured with the notion that having premarital sex with full protection is not a big problem.8 Respondents who had had their sexual debut before age 15 years were not considered a risky group (though they are actually risky). Our finding was consistent with other studies conducted in northern Ethiopia (22.6%) and Wollega (25.3%).56,57
This study investigated the sexual behavior of unmarried adolescents in YFS-program and nonprogram areas and assessed whether YFS programs or parent–adolescent communication on SRH issues are important in predicting the sexual behavior of unmarried adolescents. The findings indicated that risky sexual behavior was comparable between the two settings (25.0% in program areas and 29.1% in nonprogram areas). A similar study in Malawi reported that the sexual behavior of adolescents between YFS-program areas and nonprogram areas did not show a statistically significant difference.58
The literatures has documented that YFS reduces risky sexual behavior in youths via improving their knowledge on and attitudes toward SRH use. In this study, the proportion of adolescents with family-planning knowledge, knowledge on HIV, and favorable attitudes toward condom use was significantly higher in program areas. Despite these supportive results, the proportion of adolescents with risky sexual behavior in the two settings was comparable, which contradicts the main intent of introducing YFS programs.24 Our regression analysis revealed that increased attitude scores (favoring contraceptive and condom use) increased risky sexual behavior among unmarried adolescents. In the same way, knowledge on family planning and HIV increased risky sexual behavior in this sample of adolescents.
These unexpected relationships between family planning and HIV knowledge and risky sexual behavior observed in our study could be explained by the cross-sectional nature of the study, where causal relationships could not be established. Respondents may acquire knowledge after receiving services for their risky sexual behavior (service utilization was significantly higher in program areas: 40.2% vs 23.8%; P<0.001). In addition, having knowledge only may not be a sufficient condition to bring behavioral change.59,60 Besides, these findings may be attributed to the implementation strategy employed following the program. In YFS programs, peer education is the main approach believed to improve adolescentSRH behavior through enhancing their knowledge and attitudes toward the service.29 In the current study, the peer-education strategy may have provided inadequate SRH information (intensity and duration), resulting in limited or temporary effects in promoting SRH behavior and improving adolescents’ sexual health.61 In line with this, researchers have reported that a peer-education intervention was ineffective in facilitating young people’s behavioral change or influencing social norms concerning adolescent SRH.62
In this study, a significant difference was observed between program and nonprogram areas for attitudes of adolescents toward SRH issues. For example, premarital sexual-practice approval was reported by 28.7% of adolescents in program area and 18.8% in nonprogram areas. Additionally, adolescents with a more favorable attitude toward SRH services used were more likely to have risky sexual behavior (P<0.01). This finding may be attributed to the YFS-program strategy. A nonrandomized controlled trial conducted in Rwanda on the effect of peer education on SRH indicated that YFS using a peer-education program was effective in reducing stigma and creating a more positive climate that pulled the adolescent out of the “taboo” sphere.63
As we hypothesized, analyses of factors for sexual behavior demonstrated that sexual behavior of unmarried adolescents was predicted better by parent–adolescent communication on SRH issues than the individual- or program-related attributes alone. The result in this sample of unmarried adolescents indicated that with each unit increase in parent–adolescent communication score reduced the risk of engaging in risky sexual behavior by 20%. This finding is in line with other studies in Ethiopia reporting that youths who had parent–adolescent communication were less likely to commence sexual activity or have multiple sexual partners than their counterparts.35–37 Similarly, studies conducted on the role of parents on adolescent SRH behavior in sub-Saharan Africa have also indicated that good family communication has been associated with less engagement in risky sexual behavior. Adolescents who engaged in conversations about sex-related topics with their parents were less likely to report being sexually experienced, reported fewer lifetime sex partners, and were more likely to report using condoms.8,40,64
The importance of parent–adolescent communication on adolescent sexual behavior has been well described in different kinds of literature. Parents are the first socializing agents for their children, and one of the key areas of socialization is communication on SRH issues. Parents are sources of knowledge, beliefs, attitudes, and values for children and young people. These values, likely to shape adolescents’ behavior, can be transmitted from parents to children directly or indirectly through processes of communication and actions with their children.65 Such a pathway has been reported by overseas research, reporting that parent–adolescent communication about sex predicts changes in adolescents’ sexual attitudes and perceived norms, which in turn can influence their sexual intentions and/or behavior.66 Therefore, our finding supplements the growing body of literature suggesting that parents are key agents in the promotion of healthy sexual behavior through communication about SRH issues with their adolescents.
Consistently with earlier researchs, in this study, being female, older, watching pornography, and being in school were significantly associated with risky sexual behavior. As the age of the respondents increased by 1 year, the odds of being in risky sexual behavior doubled. This finding is in line with a study conducted among high school students in West Gojjam Zone and Zambia.16,53 This could be because of increasing physical maturity and sexual awareness and/or that unmarried adolescents may discover more opportunities to experiment.
Also, being in school was a consistent predictor that significantly reduced adolescents’ risky sexual behavior. Being in school had a role in reducing risky sexual behavior by 64% in this study. This is attributed to the fact that being at school improves one’s knowledge and level of understanding. In school settings, people’s exposure to various modes (“gender clubs”, anti-HIV clubs) of information about sex and sexual behavior, which in the long term have a significant impact on improving the use of condoms and abstinence from sex. A related study conducted in Malawi reported that adolescents with more formal education tended to be more likely to possess positive health-seeking behavior, including increased use of condoms.58
Additionally, exposure to sexually explicit materials is associated with increased risky sexual behavior among adolescents. In our study, watching pornography was associated with risky sexual behavior, consistent with previous studies in Ethiopia.56,67 A possible explanation for this may be adolescents who watch pornography are curious to try out and indulge in sexual acts that could result in risky sexual behavior.68
Limitations
Although the current study represents a better examination of the cumulative effects of sociodemographic characteristics, YFS, and interpersonal-related variables, several limitations need to be considered. The use of face-to-face interviews may have resulted in underestimation of the risky sexual behavior. Since sexuality is a very sensitive topic, there may have been the possibility of deliberate hiding of information in relation to communities’ unacceptable behavior. To minimize underreporting, same-sex interviews for data collection on an individual basis at a location convenient for the respondent were considered. Also, because adolescents are not controlled in their movements between program and nonprogram areas, they might have had opportunities to come into contact with ASRH activities, regardless of area. Though this study addressed this limitation by using criteria for area selection and leaving a buffer zone between settings, the results should be interpreted with these limitations in mind. Another limitation of the study was the lack of involvement of unmarried adolescents aged < 15 years. This was as a result of their shyness to provide detailed accounts of what was being investigated. This means that their sexual behavior was not represented in this study. Limitations related to the cross-sectional nature of the study were also observed. Some variables, such as knowledge on family planning, might not be causally connected to the outcome variable.
Conclusion
More than a quarter of respondents reported that they had risky sexual behavior. The magnitude was comparable between areas that had YFS programs and those without. Parent–adolescent communication on SRH issues is more important in predicting adolescents’ sexual behavior than YFS program–related and individual attributes. The results of this assessment would not suggest replicating the YFS programs with the existing approach, but rather undertaking alternative approaches that give due emphasis to parent–adolescent communication to improve adolescent sexual behavior.
Abbreviations
YFS, youth-friendly service; SRH, sexual and reproductive health.
Data-Sharing Statement
All the raw data supporting the findings can be obtained from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The study was approved by the Institutional Review Board (IRB) of Bahir Dar University College of Medicine and Health Sciences (protocol 089/18-04). Verbal informed assent and consent was acceptable and approved by the IRB of Bahir Dar University, and this study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
Our heartfelt thanks go to Bahir Dar University for providing financial support and ethical clearance. We would also like to thank the Amhara Regional Health Bureau and West Gojjam Zone officials, study participants, data collectors, and supervisors for their unreserved support during data collection.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, took part in revising the article critically for important intellectual content, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
1. United Nations. World population prospects 2019. Available at: https://population.un.org/wpp/.
2. UNICEF. Progress for children: a report card on adolescents. 2012. UNICEF progress for Children: a report card for adolescents. 2015. 10.
3. Ethiopian Central Statistical Agency (CSA). Single age projections (2008–2037). CSA. Projections for 2016In: CSA E, editor. In: Addis Ababa; 2016.
4. WHO. Helping parents in developing countries improve adolescents’ health. 2007.
5. WHO. Adolescents: health risks and solutions.
6. WHO. A period adolescence: needing special attention. 2014.
7. Glen-Spyron C. Risky Sexual Behavior in Adolescence. Namibia: BeliaVida Centre; 2015.
8. Shrestha RB. Premarital sexual behaviour and its impact on health among adolescents. J Health Promot. 2019;7:43–52. doi:10.3126/jhp.v7i0.25496
9. Darroch JE, Woog V, Bankole A, Ashford LS, Points K. Costs and Benefits of Meeting the Contraceptive Needs of Adolescents. Guttmacher İnstitute; 2016.
10. Wado YD, Sully EA, Mumah JN. Pregnancy and early motherhood among adolescents in five East African countries: a multi-level analysis of risk and protective factors. BMC Pregnancy Childbirth. 2019;19(1):59. doi:10.1186/s12884-019-2204-z
11. Ganatra B, Gerdts C, Rossier C, et al. Global, regional, and subregional classification of abortions by safety, 2010–14: estimates from a Bayesian hierarchical model. Lancet. 2017;390(10110):2372–2381. doi:10.1016/S0140-6736(17)31794-4
12. Kiani MA, Ghazanfarpour M, Saeidi M. Adolescent pregnancy: a health challenge. Int J Pediatr. 2019;7(7):9749–9752.
13. UNICEF and UNAIDS. Global AIDS monitoring and UNAIDS estimates in adolescents-young-people hduoth, editor. 2019.
14. Muche AA, Kassa GM, Berhe AK, Fekadu GA. Prevalence and determinants of risky sexual practice in Ethiopia: systematic review and meta-analysis. Reprod Health. 2017;14(1):113. doi:10.1186/s12978-017-0376-4
15. Agajie M, Belachew T, Tilahun T, Amentie M. Risky sexual behavior and associated factors among high school youth in Pawe Woreda, Benishangul Gumuz Region. Sci J Clin Med. 2015;4(4):67–75. doi:10.11648/j.sjcm.20150404.11
16. Kassa GM, Degu G, Yitayew M, et al.Risky sexual behaviors and associated factors among Jiga high school and preparatory school students, Amhara Region, Ethiopia. International scholarly research notices. 2016;2016.
17. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey. Addis Ababa Ethiopia,and Rockville, Maryland, USA: CSA and ICF; 2016.
18. Tebekaw Y, Aemro B, Teller C. Prevalence and determinants of unintended childbirth in Ethiopia. BMC Pregnancy Childbirth. 2014;14(1):326. doi:10.1186/1471-2393-14-326
19. Central Statistical Agency. Ethiopia mini-demographic and health survey 2014. Addis Ababa, Ethiopia. 2014. 1.
20. Girum T, Wasie A, Worku A. Trend of HIV/AIDS for the last 26 years and predicting achievement of the 90-90-90 HIV prevention targets by 2020 in Ethiopia: a time series analysis. BMC Infect Dis. 2018;18(1):320. doi:10.1186/s12879-018-3214-6
21. UNICEF Ethiopia. New HIV infections among adolescents projected. NEW YORK/JOHANNESBURG/ADDIS ABABA. 2016.
22. Central Statistical Agency. Ethiopia demographic and health survey 2016. Addis Ababa, Ethiopia. 2016.
23. ICF. CSACEa. Ethiopia Demographic and Health Survey 2016: HIV Report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF; 2018.
24. United Nations.
25. Worled Health Organization. Making health services adolescent friendly: developing national quality standards for adolescent friendly health services. In: Department of Maternal N. Geneva, Switzerland: Child and Adolescent Health editor; 2012.
26. Federal Dimocratic of Ethiopia Ministry of Health. National adolescent and youth health strategy 2016–2020. Addis Ababa. 2016.
27. Jain A, Ismail H, Tobey E, Erulkar A Understanding adolescent and youth sexual and reproductive health-seeking behaviors in Ethiopia: implications for youth friendly service programming. 2017.
28. Ministry of Health of Federal Democratic Republic of Ethiopia Addis. Standards on youth friendly reproductive health services service delivery guideline minimum service delivery package on YFRH services. Ababa, Ethiopia. 2007. 1.
29. Federal Democratic reoublic of Ethiopia Ministry of Health. National adolescent and youth sexual and reproductive health strategy (2006–2015). Addis Ababa, Ethiopia. 2005.
30. Ministry of Health of Ethiopia. ETHIOPIAN Emergency Obstetric and Newborn Care (EmONC) assessment 2016. Addis Abab. 2016.
31. Organization WH. Adolescent Friendly Health Services: An Agenda for Change. Geneva: World Health Organization; 2003.
32. Kempers J, Ketting E, Lesco G. Cost analysis and exploratory cost-effectiveness of youth-friendly sexual and reproductive health services in the Republic of Moldova. BMC Health Serv Res. 2014;14(1):316. doi:10.1186/1472-6963-14-316
33. Denno DM, Hoopes AJ, Chandra-Mouli V. Effective strategies to provide adolescent sexual and reproductive health services and to increase demand and community support. J Adolesc Health. 2015;56(1):S22–S41. doi:10.1016/j.jadohealth.2014.09.012
34. Fikree FF, Abshiro WK, Mai MM, Hagos KL, Asnake M. Strengthening youth friendly health services through expanding method choice to include long-acting reversible contraceptives for Ethiopian youth. Afr J Reprod Health. 2017;21(3):37–48. doi:10.29063/ajrh2017/v21i3.3
35. Negeri EL. Assessment of risky sexual behaviors and risk perception among youths in Western Ethiopia: the influences of family and peers: a comparative cross-sectional study. BMC Public Health. 2014;14(1):301. doi:10.1186/1471-2458-14-301
36. Yimer B, Ashebir W. Parenting perspective on the psychosocial correlates of adolescent sexual and reproductive health behavior among high school adolescents in Ethiopia. Reprod Health. 2019;16(1):66. doi:10.1186/s12978-019-0734-5
37. Gebregzabher TG, Hailu TT, Assefa BA. Determinants of teenage pregnancy in Degua Tembien District, Tigray, Northern Ethiopia: a community-based case-control study. PLoS One. 2018;13(7):1–15.
38. Widman L, Choukas-Bradley S, Noar SM, Nesi J, Garrett K. Parent-adolescent sexual communication and adolescent safer sex behavior: a meta-analysis. JAMA Pediatr. 2016;170(1):52–61. doi:10.1001/jamapediatrics.2015.2731
39. Hannah Lantos H, Manlove J, Wildsmith E, Faccio B, Guzman L, Moore K. Parent-teen communication about sexual and reproductive health: cohort differences by race/ethnicity and nativity. Int J Environ Res Public Health. 2019;16(5):833. doi:10.3390/ijerph16050833.
40. Bronfenbrenner U. The Ecology of Human Development. Harvard university press; 1979.
41. ANRS Health Burea. The 2016/17 fiscal year annual performance report of Amhara regional state health bureau. Bahir Dar. 2017.
42. Ayehu A, Kassaw T, Hailu G, Ciccozzi M. Level of young people sexual and reproductive health service utilization and its associated factors among young people in Awabel District, Northwest Ethiopia. PLoS One. 2016;11(3):e0151613. doi:10.1371/journal.pone.0151613
43. Fleiss JL, Levin B, Paik MC. Statistical Methods for Rates and Proportions. john wiley & sons; 2013.
44. Munea AM, Alene GD, Debelew GT. Quality of youth friendly sexual and reproductive health services in West Gojjam Zone, north West Ethiopia: with special reference to the application of the Donabedian model. BMC Health Serv Res. 2020;20(1):1–12. doi:10.1186/s12913-020-05113-9
45. Awoke Derbie MA, Daniel M, Fantahun B. Risky sexual behaviour and associated factors among students of Debre Tabor University, Northwest Ethiopia: a cross-sectional study. Ethiop J Health Dev. 2016;30(1):11–18.
46. World Health Organization. Global Standards for Quality Health-Care Services for Adolescents: A Guide to Implement a Standards-Driven Approach to Improve the Quality of Health Care Services for Adolescents. World Health Organization; 2015.
47. Organization WH. Making health services adolescent friendly: developing national quality standards for adolescent friendly health services. 2012.
48. Organization WH. Global standards for quality health-care services for adolescents: a guide to implement a standards-driven approach to improve the quality of health care services for adolescents. 2015.
49. Sales JM, Milhausen RR, Wingood GM, DiClemente RJ, Salazar LF, Crosby RA. Validation of a parent-adolescent communication scale for use in STD/HIV prevention interventions. Health Educ Behav. 2008;35(3):332–345. doi:10.1177/1090198106293524
50. Dessie Y, Berhane Y, Worku A, Wallander JL. Parent-adolescent sexual and reproductive health communication is very limited and associated with adolescent poor behavioral beliefs and subjective norms: evidence from a community based cross-sectional study in eastern Ethiopia. PLoS One. 2015;10(7):e0129941. doi:10.1371/journal.pone.0129941
51. Lewis M Stepwise versus HIERARCHICAL REGRESSION: pros and cons. Online Submission. 2007.
52. FDRE Ministry of Science and Technology. National Research Ethics Review Guideline.
53. Yang X-H, Yuan S, Zhang R, et al. Risky sexual behaviors and associated factors among college students in Lusaka, Zambia. Arch Sex Behav. 2019;48:1–7.
54. Obo CS, Sori LM, Abegaz TM, Molla BT. Risky sexual behavior and associated factors among patients with bipolar disorders in Ethiopia. BMC Psychiatry. 2019;19(1):313. doi:10.1186/s12888-019-2313-2
55. Fetene N, Mekonnen W, Price MA. The prevalence of risky sexual behaviors among youth center reproductive health clinics users and non-users in Addis Ababa, Ethiopia: a comparative cross-sectional study. PLoS One. 2018;13(6):e0198657. doi:10.1371/journal.pone.0198657
56. Tolera FH, Girma E, Mamo A, Babure ZK Risky sexual behaviors and associated factors among high and preparatory school youth, East Wollega, Ethiopia, 2017: a cross-sectional study design. 2019.
57. Abrha K, Worku A, Lerebo W, Berhane Y. Sexting and high sexual risk-taking behaviours among school youth in northern Ethiopia: estimating using prevalence ratio. BMJ Sex Reprod Health. 2019;45:200–206.
58. Maonga BB, Gondwe TS, Machira K Determinants of risky sexual behavior among the youth in Malawi. 2018.
59. Okpokumoku S, Nwose E, Nwajei S. Sexual behaviour, knowledge and use of contraceptives among undergraduate students. J Health Sci Res. 2018;2(2):10–17. doi:10.18311/jhsr/2017/18113
60. González RP, Kadengye DT, Mayega RW. The knowledge-risk-behaviour continuum among young Ugandans: what it tells us about SRH/HIV integration. BMC Public Health. 2019;19(1):604. doi:10.1186/s12889-019-6809-y
61. Rose-Clarke K, Bentley A, Marston C, Prost A, Das JK. Peer-facilitated community-based interventions for adolescent health in low-and middle-income countries: a systematic review. PLoS One. 2019;14(1):e0210468. doi:10.1371/journal.pone.0210468
62. Chandra-Mouli V, Lane C, Wong S. What does not work in adolescent sexual and reproductive health: a review of evidence on interventions commonly accepted as best practices. Global Health: Sci Pract. 2015;3(3):333–340.
63. Michielsen K, Beauclair R, Delva W, Roelens K, Van Rossem R, Temmerman M. Effectiveness of a peer-led HIV prevention intervention in secondary schools in Rwanda: results from a non-randomized controlled trial. BMC Public Health. 2012;12(1):729. doi:10.1186/1471-2458-12-729
64. Seif SA, Kohi TW, Moshiro CS. Sexual and reproductive health communication intervention for caretakers of adolescents: a quasi-experimental study in Unguja-Zanzibar. Reprod Health. 2019;16(1):92. doi:10.1186/s12978-019-0756-z
65. Viner RM, Ozer EM, Denny S, et al. Adolescence and the social determinants of health. Lancet. 2012;379(9826):1641–1652. doi:10.1016/S0140-6736(12)60149-4
66. Rogers AA. Parent–adolescent sexual communication and adolescents’ sexual behaviors: a conceptual model and systematic review. Adolesc Res Rev. 2017;2(4):293–313. doi:10.1007/s40894-016-0049-5
67. Waktole ZD, Dalby AR. Sexual behaviors and associated factors among youths in Nekemte town, East Wollega, Oromia, Ethiopia: a cross-sectional study. PLoS One. 2019;14(7):e0220235. doi:10.1371/journal.pone.0220235
68. Hardani R, Hastuti D, Yuliati LN. Pornography behavior of junior high school student. J Child Dev Stud. 2018;3(1):15–27. doi:10.29244/jcds.3.1.15-27
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
