Back to Journals » Cancer Management and Research » Volume 11
Docetaxel, oxaliplatin, leucovorin, and 5-fluorouracil (FLOT) as preoperative and postoperative chemotherapy compared with surgery followed by chemotherapy for patients with locally advanced gastric cancer: a propensity score-based analysis
Authors Wang KS , Ren YX, Ma ZJ, Li F, Cheng XC, Xiao JY, Zhang SZ, Yu ZY, Yang HT, Zhou HN, Li YM, Liu HB, Jiao ZY
Received 8 January 2019
Accepted for publication 15 February 2019
Published 10 April 2019 Volume 2019:11 Pages 3009—3020
DOI https://doi.org/10.2147/CMAR.S200883
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Ahmet Emre Eşkazan
Keshen Wang,1 Yanxian Ren,1 Zhijian Ma,2 Fan Li,1 Xiaocheng Cheng,1 Jingying Xiao,1 Shuze Zhang,1 Zeyuan Yu,1 Hanteng Yang,1 Huinian Zhou,1,2 Yuming Li,1,2 Hongbin Liu,3 Zuo-Yi Jiao1,2
1Department of General Surgery, Lanzhou University Second Hospital, Lanzhou, Gansu 730010, People’s Republic of China; 2Cui-ying Experimental Center, Lanzhou University Second Hospital, Lanzhou, Gansu 730010, People’s Republic of China; 3Department of General Surgery, The 940th Hospital of Joint Logistics Support Force of People’s Liberation Army, Lanzhou 730050, People’s Republic of China
Introduction: Docetaxel, oxaliplatin, leucovorin, and 5-fluorouracil (FLOT) may improve overall survival (OS) in patients with locally advanced gastric cancer (LAGC); however, evidence for its use as a standard treatment has not been established in China. The aim of this study was to investigate the effectiveness, safety, and feasibility of the FLOT regimen as neoadjuvant chemotherapy in Chinese patients with resectable LAGC.
Methods: We conducted an observational study to compare the effectiveness of FLOT regimen consisting of docetaxel (60 mg/m2,), oxaliplatin (85 mg/m2,), leucovorin (200 mg/m2,), and 5-fluorouracil (2,600 mg/m2, as a 24 hr infusion), all given on day 1 and administered every 2 weeks versus initial surgery followed by chemotherapy in patients with clinical T3–4 LAGC. OS was compared by using the Cox proportional hazards regression model and the Kaplan–Meier curve adjusted by inverse probability of treatment weighting (IPTW) and propensity score-matched (PSM) analysis. In addition, we performed subgroup analyses to determine the effectiveness of the FLOT regimen in clinically relevant patient subsets.
Results: Overall, 47 patients who received initial FLOT chemotherapy and 269 patients who received initial surgery were enrolled in this study. In the PSM analysis, the FLOT-first group showed favorable OS compared with the surgery-first group (41 vs 41 [HR, 0.416; 95% CI, 0.218–0.794; P=0.008]), and 3-year survival rates were 58.7% and 30.9% in the FLOT-first group and surgery-first group, respectively. IPTW analysis showed similar results. However, the effect of FLOT was low (HR, 0.868; 95 CI%, 0.215–3.504) in patients without lymph node metastasis.
Conclusion: Our study suggests that preoperative FLOT chemotherapy is safe and feasible. In terms of OS, FLOT may be superior to initial surgery followed by chemotherapy in reducing morbidity with resectable LAGC.
Keywords: gastric cancer, preoperative chemotherapy, propensity score, FLOT, prognosis
Introduction
Gastric cancer (GC) is the fifth most common malignancy worldwide and the third leading cause of cancer-related mortality.1 The mortality rate for GC has continued to increase in the past decade and the high mortality rate reflects the prevalence of advanced stage at presentation, especially in China.2 Currently, for patients with pT1-stage GC, radical surgery (including endoscopic mucosal and submucosal dissection) can be performed to peruse curative outcome, and the postoperative 5-year survival rate can reach 85–95%. However, in China, patients with advanced gastric cancer (AGC) account for nearly 80% of the total number, and the postoperative 5-year survival rate remains only 30–50%. This situation indicates that for most patients with AGC, even if an expanded scope of surgical resection and lymph node dissection were performed, surgery alone or surgery plus chemotherapy cannot achieve the goal of radical cure. Therefore, the concept of preoperative chemotherapy, also known as neoadjuvant chemotherapy (NACT), was proposed to improve the radical resection rate and control preoperative micrometastasis.
In the early 1990s,3 the literature reported the application of neoadjuvant chemotherapy in patients with resectable GC, mostly regimens based on 5-fluorouracil, combined with adriamycin (ADM), mitomycin (MMC), and cisplatin (DDP). In these studies, the median survival time of neoadjuvant chemotherapy was 15–40 months, which was significantly better than that of patients who received surgery alone4–8 In 2006, the MAGIC study (a Phase III, randomized, controlled study) conducted a trial of patients who received three cycles of epirubicin, cisplatin, and fluorouracil (ECF) as chemotherapy before and after surgery and the control group who received surgery alone,9 and found that the overall survival (OS) rate of the perioperative chemotherapy group was significantly better than that of the surgery-alone group (36% vs 23%, HR, 0.75; 95% CI, 0.60–0.93; P=0.0009). In another multicenter randomized controlled trial from France (FNCLCC ACCORD 07-FFCD 9703), preoperative application of 5-FU and cisplatin versus surgery alone resulted in OS rates of 38% and 24%, respectively (P=0.02) and disease-free survival rates of 34% and 19%, respectively (P=0.003).10 Furthermore, the results of the Phase II/III multicenter randomized controlled trial (FLOT4-AIO) showed that the FLOT regimen was significantly superior to the ECF/ECX regimen of the MAGIC trial in terms of OS (HR, 0.0.77; 95% CI, 0.63–0.94; P=0.012).11 The positive impact of preoperative chemotherapy on survival in patients with resectable AGC has been confirmed by many meta-analyses,12,13 although there is no consensus as to the best regimen.
Due to the lack of adequate treatment experience and because the efficacy of NACT has not been clearly verified for Chinese patients, most practitioners still prefer initial surgery once the diagnosis was made. In addition, no study to date has directly compared the efficacy of FLOT as NACT regimen with that of initial surgery followed by adjuvant chemotherapy. Therefore, we designed this study to investigate the relative benefit of FLOT regimen as NACT compared with initial surgery for Chinese patients with resectable locally advanced gastric cancer (LAGC) and investigated the subgroup of patients who would be having better benefits.
Methods
Patients enrollment
From January 2013 to December 2017, clinical data of 341 patients with LAGC who underwent radical gastrectomy were collected at the Department of General Surgery, Lanzhou University Second Hospital.
The eligibility criteria were as follows: 1) preoperative cT3–4; 2) histologically proven adenocarcinoma; 3) underwent D2 or extended D2 lymphadenectomy; 4) complete clinical records; 5) no distant metastasis such as liver, lung or bone; 6) <75 years old; and (7) Eastern Cooperative Oncology Group (ECOG) score 0–2 points.
The exclusion criteria were as follows: 1) previous history of other cancers; 2) gastric stump cancer; and 3) received preoperative radiotherapy. Ultimately, a total of 316 patients who met the criteria were included in this study, representing 92.7% of the total number of patients with LAGC during the same period. The requirement to obtain written informed consent from patients was waived because of the retrospective nature of this study. The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Lanzhou University Second Hospital.
Treatment
Patients in the NACT group received at least 1 week of preoperative chemotherapy with the FLOT regimen consisting of docetaxel (60 mg/m2), oxaliplatin (85 mg/m2), leucovorin (200 mg/m2), and 5-fluorouracil (2,600 mg/m2 as a 24 hr infusion), all given on day 1. This procedure was performed every 2 weeks and surgery was followed 3 weeks after chemotherapy was completed. Patients underwent imaging evaluation (computed tomography [CT] or magnetic resonance imaging [MRI]) after receiving FLOT neoadjuvant. If the tumor resolved, the patients finished three cycles of preoperative chemotherapy. If the imaging evaluation revealed the chemotherapy ineffective or the tumor progressed, surgery was performed directly. Patients in the two groups all received at least one cycle of adjuvant chemotherapy after surgery, and we preferred to use FLOT. If the FLOT regimen was not tolerated due to toxic reaction, then it was replaced by XELOX (oxaliplatin 130 mg/m2 on day 1; xeloda 1,000 mg/m2 twice a day, on day 1–14), SOX (oxaliplatin 130 mg/m2 on day 1; tegafur 40 mg/m2 twice a day, on day 1–14), or FOLFOX6 (oxaliplatin 85 mg/m2, leucovorin 200 mg/m2 on, and 5-fluorouracil 2,600 mg/m2) regimens. All patients in our study underwent total, subtotal, or distal gastrectomy based on the primary tumor size and location. The strategy for lymph node dissection was taken by standard D2 or extended D2 lymphadenectomy.
Data collection
After reviewing medical records, we obtained data on age, sex, time of diagnosis, tumor location, preoperative ECOG score, clinical TNM stage, Lauren classification, style of operation, regimen of adjuvant chemotherapy, depth of tumor invasion, and number of positive lymph nodes in all patients. Depth of tumor invasion was utilized to stage tumors according to the 7th edition AJCC guidelines.14 The primary endpoint in this study was OS, which was calculated from the time of the any form of treatment since diagnosis to the date of death (for any reason) or the most recent follow-up. The secondary endpoint was response, which was evaluated by CT scan in each cycle according to RECIST criterion v 1.1, and compared with the baseline CT scan performed before treatment.
Statistical analysis
Associations between treatment modality and patients’ demographic, clinical, and facility characteristics were assessed using Pearson χ2 or Fisher’s exact test for categorical data and independent-sample t test for continuous variables, respectively. To reduce bias from nonrandom treatment assignments, two models of the association between OS and treatment modality based on propensity score analysis were constructed: propensity score-matched (PSM) and weighting by inverse probability of treatment (IPTW). The propensity score analysis of receipt of NACT was used to take into account all baseline covariates into a nonparsimonious manner and was constructed using a multivariable logistic regression model, which contained age, gender, tumor location, clinical TNM stage, Lauren classification, and year of diagnosis. The Hosmer and Lemeshow goodness-of-fit statistics and the area under the receiver operating characteristic curve (AUC) were calculated to evaluate the adequacy of the model.
For the matched-patient analysis, patients treated with NACT were matched 1:1 to patients who received initial surgery on propensity score with a caliper of 0.05. We also assessed the heterogeneity of treatment effects with tests of interaction and subgroup analysis that explored the effect of age, gender, clinical TNM stage, and tumor location. Moreover, based on the propensity score, an IPTW analysis was conducted. Patients who received first-line FLOT were weighted by 1/propensity score, whereas patients who underwent first-line surgery were weighted by 1/(1− propensity score).
In both models, Kaplan–Meier curves with the log-rank tests were used to calculate the overall cumulative probability. Univariate and multivariate Cox models were performed to compare the groups in the PSM analysis. A P-value <0.05 was considered statistically significant. Statistical analyses were conducted using Statistical Product for Social Sciences (SPSS) software (version 23.0; Inc, Chicago, IL, USA) and Empower-Stats (
Results
Patients’ characteristics
From 2013 to 2017, a total of 316 LAGC patients were included in this study, of whom 47 patients received preoperative FLOT regimen chemotherapy and 269 patients received initial surgery after diagnosis. The baseline data of the patients are shown in Table 1. As shown in Table 1, there was a significant difference between the two groups in the clinical TNM stage and the time of diagnosis. The propensity score obtained by multivariate logistic regression analysis showed an AUC of 0.75 and a P-value of the Hosmer–Lemeshow test of 0.414, which suggested a reasonable data model.
 | Table 1 Demographic and clinical characteristics before and after PSM analysis |
Survival analysis
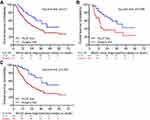
The median follow-up time for the entire study was 41 months (12–67 months). In the unmatched study, the median survival time for patients in the initial FLOT group and that in the initial surgery group was 44 months and 23 months (P=0.01), respectively. The 3-year survival rates in the initial FLOT group and that in the initial surgery group were 60.1% and 36.5%, respectively; the 5-year survival rates were 43.8% and 26.8%, respectively (Figure 1A, Table 2). The results of the multivariate analyses showed that treatment approach and clinical TNM stage were independent factors affecting patients’ survival. In addition, the adjusted HR of FLOT-first compared with surgery-first for OS was 0.417 (95% CI, 0.23–0.755, P=0.004) (Table S1). In the head-to head PSM analysis, 41 patients treated with FLOT-first and 41 patients treated with surgery-first were successfully matched, and the age, sex, tumor location, Lauren classification, clinical TNM stage, and time of diagnose were balanced between the two groups (Table 1). The results of the multivariate analysis indicated that initial FLOT was associated with a significant OS benefit compared with initial surgery (HR, 0.416; 95% CI, 0.218–0.794; P=0.008) (Table 3). The median survival time for patients in the FLOT-first group and that in the surgery-first group was 44 months and 15 months (P=0.008), respectively. The 3-year survival rate in the FLOT-first group and surgery-first group was 58.7% and 30.9%, respectively (Figure 1B, Table 2). The IPTW analysis showed a similar result; The 3-year survival rate in the FLOT-first group and the surgery-first group was 68.6% and 35.4% (P<0.001), respectively (Figure 1C, Table 2). In the exploratory subgroup analysis of the matched cohort, there were no significantly different effects of FLOT on OS across all subgroups examined (Figure 2). However, in stage II subgroup, patients who received FLOT-first treatment did not show a beneficial survival (HR, 0.868; 95% CI, 0.215–3.504).
 | Table 2 Overall survival for FLOT-first versus surgery-first in patients with locally advanced gastric cancer |
 | Table 3 Univariate and multivariate analysis of survival in PSM analysis (n=82) |
 | Figure 2 Subgroup analysis in the propensity score-matched analysis.Abbreviation: FLOT, docetaxel, oxaliplatin, leucovorin, and 5-fluorouracil. |
Response and toxicity analysis
In this study, only 1 (2.1%) patient achieved CR, 15 (42.6%) patients achieved PR, 17 (44.7%) patients were in SD, and 3 (6.4%) patients were in progressive disease (PD) according to CT contrast before and after chemotherapy. Two patients’ data were lost. After surgery, 1 (2.1%) patient was not found to have cancer tissue (PCR), and the R0 resection rate was 91% in the FLOT-first cohort (Table 4). In the FLOT-first cohort, the results of multivariate analysis showed that the response to chemotherapy (HR, 8.21; 95% CI, 1.66–40.56, P=0.005) and gender (HR, 6.322; 95% CI, 1.75–22.91; P=0.01) were independent factors associated with survival (Table S2). Throughout the course of chemotherapy, the main grade 3–4 toxicities were mainly leukopenia (36%), dizziness (9%), nausea (25%), and vomiting (3%). No patient dropped out due to severe toxic reactions. In addition, G-CSF was administered in 23 patients and no treatment-related death occurred.
 | Table 4 Tumor response according to RECIST 1.1 criteria |
Postoperative pathology results
The extent of resection, surgical complications, pT stage of tumor invasion, and pN stage of lymph node according to the 7th edition AJCC guidelines are summarized in Table 5.14 We can conclude that in the unmatched study, the R0 resection rate was 88.4% in the FLOT group and 86.4% in the surgery group. In the PSM analysis, the R0 resection rate was 89.2% in the FLOT group and 84.6% in the surgery group (all P>0.05). After surgery, there was significant difference only in the pN stage between the two groups after PSM (P=0.006), and percentage of patients without lymph node metastasis was slightly high in the FLOT-first cohort.
 | Table 5 Postoperative pathology report |
Discussion
The positive impact of neoadjuvant chemotherapy on survival in patients with locally advanced gastric adenocarcinoma has become clearer over time, although there is no consensus as to the best approach. The best chemotherapy regimen for neoadjuvant therapy is not established, and practice is variable. Although the FLOT regimen demonstrated higher 5-year survival and disease-free survival rates in the treatment of GC and gastroesophageal junction cancer than the previous regimen,11 whether this regimen can achieve similar results in GC patients in China has not been reported.
Our head-to-head study based on the propensity score, for the first time, directly compared the survival benefit of preoperative FLOT chemotherapy with initial surgery followed by adjuvant chemotherapy. We found that patients who received neoadjuvant chemotherapy with the FLOT regimen had a lower mortality rate and a median survival time of approximately 10 more months compared with patients who underwent initial surgery. This benefit profile is consistent with that obtained in the IPTW study, and the consistency of the results from these two analyses can further support our conclusions.
For patients with potentially resectable AGC, randomized trials and meta-analyses indicate a significant survival benefit over surgery alone for the number of approaches, including neoadjuvant chemotherapy. At least four trials have directly compared surgery alone with neoadjuvant or perioperative chemotherapy, three of which demonstrated a survival benefit for this approach. In the Phase III MAGIC trial,9 the HR of the ECF regimen compared with surgery for OS was 0.75 (95% CI, 0.60–0.93). In the large multicenter randomized controlled trial 07-FFCD 9703 in France,10 the HR was 0.69 (95% CI, 0.50–0.95) in the DCF regimen compared with the surgery alone. Fiteni et al15 conducted a large retrospective study based on the propensity score. In Fiteni’s study, the DCF regimen was compared with the surgery group, and the 5-year survival rate was 0.293 (95% CI, 0.135–0.636) in the treatment of gastroesophageal junction cancer. In these three studies, R0 resection rates were 69%, 84%, and 90.32%. These results illustrate the potential superiority of docetaxel in the neoadjuvant chemotherapy regimen. In our study, the adjusted HR was 0.417 (95% CI, 0.23–0.755) for the FLOT-first compared with surgery-first, and the 3-year survival rate was 60.1%. The 3-year survival rate was similar to the 57% result in the stage III FLOT-AIO4 trial and 60% in the Fiteni study and is superior to the 45% in the MAGIC trial and 50% in FFCD trial.9,10,16 Although the biological behavior of gastroesophageal junction cancer and distal GC included in these studies are different, the results may indicate the potential advantages of FLOT as a neoadjuvant chemotherapy regimen. In addition, the R0 resection rate in our study was 88.4%, which is similar to the result of 86% reported in a Phase II clinical study (Neo-FLOT) in Germany, where the patients included were (consistent with our study) all in cT3–4 stage.17 Furthermore, there was a significant difference in postoperative lymph node N stage between the two groups in the PSM analysis, and the number of patients without lymph node metastasis was slightly high in the FLOT-first cohort, which may mean that the number of lymph node metastases can be reduced by the FLOT regimen to achieve the goal of downstage treatment. A meta-analysis conducted by Coccolini F also reached a similar conclusion.13 In addition, in the further subgroup analysis, we found that for stage II patients, preoperative FLOT chemotherapy did not show a better benefit (HR, 0.868, 95% CI, 0.215–3.504). This indicated that the FLOT regimen might not be effective in patients without lymph node metastasis, because only cT3–4 patients were included in our study, and those with stage II had no lymph node metastasis.
Previous findings have confirmed that response to chemotherapy is closely related to the prognosis of patients with GC and gastroesophageal junction cancer,18,19 and this conclusion is also consistent with the results of our research. In the Neo-FLOT study,17 PCR in the FLOT regimen reached 20% and RR reached 40%. In the FLOT4 trial, PCR reached 15% and 16% in gastric and gastroesophageal junction cancers, respectively.11 In addition, PCR was 5% in the study by Simon, and the response rate was even higher at 66%.20 Although only 1 patient in our study achieved PCR (7%), which is lower than the above study, the overall response rate reached 44.7% and is better than the overall response rate of 37% in the V325 study,21 which also included a docetaxel-containing DCF regimen. Although limited by the fact that this comparison was made between different trials, we cannot directly conclude that the FLOT regimen is superior to other docetaxel-containing chemotherapy regimens; however, this result still demonstrates the potential superiority of FLOT over DCF and other docetaxel-containing chemotherapy regimens in terms of chemotherapy effectiveness.
There is no doubt that chemotherapy regimens including docetaxel increase the risk of hematologic toxicities and nonhematologic side effects. In the FLOT4 trial,11 chemotherapy-related grade 3–4 adverse effects were mainly leukopenia (36%), dizziness (9%), and vomiting (3%). In our study, to ensure safety and avoid unnecessary drug reductions during FLOT administration, we used prophylactic antiemetics in each patient. Additionally, granulocyte-colony stimulating factor (G-CSF) was used for patients with fewer than 4 × 109 leukocytes. Leukopenia and vomiting remained the most predominant side effects of chemotherapy with results similar to those observed in the FLOT4 trial, but these were clinically acceptable grade 3–4 toxicities.22 In the present study, no patient dropped out due to unbearable or severe side effects and no treatment-related deaths occurred.
Our study has some limitations and deficiencies. First, there were only 47 patients in the FLOT-first group, and the effect of FLOT for patients without lymph node metastasis still needs to be verified by a larger sample; second, as a retrospective study, although the statistical method based on the propensity score can effectively eliminate observed confounders, it cannot control for unobserved confounders; thus, it is impossible to reach the level of evidence of randomized controlled studies. However, the efficacy of the FLOT regimen for patients with LAGC within the tolerable toxicity levels is consistent with the results of previous studies. Furthermore, tumor staging and efficacy evaluation were all conducted through CT, gastroscopy, or MRI. Similar to many previous studies, these traditional methods can only evaluate tumors and tumor changes from a morphological point of view. It is difficult to achieve an accurate evaluation, and a high degree of consistency cannot be maintained with pathological findings, which may affect the matching and comparison of the two groups of patients.
Conclusion
Our study demonstrated that preoperative FLOT regimen chemotherapy was superior to initial surgery for patients with LAGC in terms of OS. We suggest that the use of the FLOT regimen as neoadjuvant chemotherapy should be taken into consideration during the comprehensive treatment of patients with LAGC. Rigorous randomized studies are needed to determine the role of FLOT and optimal patient selection in the Chinese population.
Ethical statement
To preserve patient privacy and data confidentiality, patient data have been identified before analysis. All analyses in this retrospective study were performed based on the data from anonymized patients. Due to the retrospective nature of this study, the Ethics Committee of Lanzhou University Second Hospital approved the study and determined that written informed consent was not required.
Acknowledgment
This study was funded by the National Natural Science Foundation of China (Grant No.31670847) and Gansu Provincial Key Research and Development Program (No.17YF1FA127). Dr Keshen Wang and Yanxian Ren are co-first authors.
Disclosure
The authors report no conflicts of interest in this study.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
2. Patru CL, Surlin V, Georgescu I, Patru E. Current issues in gastric cancer epidemiology. Rev Med Chir Soc Med Nat Iasi. 2013;117(1):199–204.
3. Ajani JA, Ota DM, Jessup JM, et al. Resectable gastric carcinoma. An evaluation of preoperative and postoperative chemotherapy. Cancer. 1991;68(7):1501–1506.
4. Ajani JA, Mansfield PF, Ota DM. Potentially resectable gastric carcinoma: current approaches to staging and preoperative therapy. World J Surg. 1995;19(2):216–220.
5. Ajani JA, Mayer RJ, Ota DM, et al. Preoperative and postoperative combination chemotherapy for potentially resectable gastric carcinoma. J Natl Cancer Inst. 1993;85(22):1839–1844.
6. Leichman L, Silberman H, Leichman CG, et al. Preoperative systemic chemotherapy followed by adjuvant postoperative intraperitoneal therapy for gastric cancer: a University of Southern California pilot program. J Clin Oncol. 1992;10(12):1933–1942. doi:10.1200/JCO.1992.10.12.1933
7. Yoshikawa T, Sasako M, Yamamoto S, et al. Phase II study of neoadjuvant chemotherapy and extended surgery for locally advanced gastric cancer. Br J Surg. 2009;96(9):1015–1022. doi:10.1002/bjs.6665
8. Persiani R, Rausei S, Pozzo C, et al. 7-Year survival results of perioperative chemotherapy with epidoxorubicin, etoposide, and cisplatin (EEP) in locally advanced resectable gastric cancer: up-to-date analysis of a phase-II study. Ann Surg Oncol. 2008;15(8):2146–2152. doi:10.1245/s10434-008-9982-2
9. Cunningham D, Allum WH, Stenning SP, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20. doi:10.1056/NEJMoa055531
10. Ychou M, Boige V, Pignon JP, et al. Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol. 2011;29(13):1715–1721. doi:10.1200/JCO.2010.33.0597
11. Al-Batran SE, Hofheinz RD, Pauligk C, et al. Histopathological regression after neoadjuvant docetaxel, oxaliplatin, fluorouracil, and leucovorin versus epirubicin, cisplatin, and fluorouracil or capecitabine in patients with resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4-AIO): results from the phase 2 part of a multicentre, open-label, randomised phase 2/3 trial. Lancet Oncol. 2016;17(12):1697–1708. doi:10.1016/S1470-2045(16)30531-9
12. Xu AM, Huang L, Liu W, Gao S, Han WX, Wei ZJ. Neoadjuvant chemotherapy followed by surgery versus surgery alone for gastric carcinoma: systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9(1):e86941. doi:10.1371/journal.pone.0086941
13. Coccolini F, Nardi M, Montori G, et al. Neoadjuvant chemotherapy in advanced gastric and esophago-gastric cancer. Meta-analysis of randomized trials. Int J Surg. 2018;51:120–127. doi:10.1016/j.ijsu.2018.01.008
14. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–1474. doi:10.1245/s10434-010-0985-4
15. Fiteni F, Paget-Bailly S, Messager M, et al. Docetaxel, cisplatin, and 5-fluorouracil as perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma. Cancer Med. 2016;5(11):3085–3093. doi:10.1002/cam4.885
16. Al-Batran SE, Pauligk C, Homann N, et al. LBA-008Docetaxel, oxaliplatin, and fluorouracil/leucovorin (FLOT) versus epirubicin, cisplatin, and fluorouracil or capecitabine (ECF/ECX) as perioperative treatment of resectable gastric or gastro-esophageal junction adenocarcinoma: the multicenter, randomized phase 3 FLOT4 trial (German Gastric Group at AIO). Ann Oncol. 2017;28(suppl_3). doi:10.1093/annonc/mdx075.
17. Schulz C, Kullmann F, Kunzmann V, et al. NeoFLOT: multicenter phase II study of perioperative chemotherapy in resectable adenocarcinoma of the gastroesophageal junction or gastric adenocarcinoma-very good response predominantly in patients with intestinal type tumors. Int J Cancer. 2015;137(3):678–685. doi:10.1002/ijc.29403
18. Fields RC, Strong VE, Gonen M, et al. Recurrence and survival after pathologic complete response to preoperative therapy followed by surgery for gastric or gastrooesophageal adenocarcinoma. Br J Cancer. 2011;104(12):1840–1847. doi:10.1038/bjc.2011.175
19. Becker K, Langer R, Reim D, et al. Significance of histopathological tumor regression after neoadjuvant chemotherapy in gastric adenocarcinomas: a summary of 480 cases. Ann Surg. 2011;253(5):934–939. doi:10.1097/SLA.0b013e318216f449
20. Pernot S, Mitry E, Samalin E, et al. Biweekly docetaxel, fluorouracil, leucovorin, oxaliplatin (TEF) as first-line treatment for advanced gastric cancer and adenocarcinoma of the gastroesophageal junction: safety and efficacy in a multicenter cohort. Gastric Cancer. 2014;17(2):341–347. doi:10.1007/s10120-013-0266-6
21. Van Cutsem E, Moiseyenko VM, Tjulandin S, et al. Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line therapy for advanced gastric cancer: a report of the V325 Study Group. J Clin Oncol. 2006;24(31):4991–4997. doi:10.1200/JCO.2006.06.8429
22. Al-Batran SE, Hartmann JT, Hofheinz R, et al. Biweekly fluorouracil, leucovorin, oxaliplatin, and docetaxel (FLOT) for patients with metastatic adenocarcinoma of the stomach or esophagogastric junction: a phase II trial of the Arbeitsgemeinschaft Internistische Onkologie. Ann Oncol. 2008;19(11):1882–1887. doi:10.1093/annonc/mdn403
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.