Back to Journals » International Journal of Women's Health » Volume 14
Do SARS-CoV-2-Infected Pregnant Women Have Adverse Pregnancy Outcomes as Compared to Non-Infected Pregnant Women?
Authors Ahmad SN , Sameen D, Dar MA, Jallu R, Shora TN, Dhingra M
Received 4 June 2022
Accepted for publication 25 August 2022
Published 2 September 2022 Volume 2022:14 Pages 1201—1210
DOI https://doi.org/10.2147/IJWH.S375739
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Syed Nawaz Ahmad,1 Duri Sameen,1 Mansoor Ahmad Dar,2 Romaan Jallu,3 Tajali Nazir Shora,4 Mansi Dhingra5
1Department of Obstetrics and Gynecology, Government Medical College Anantnag, Anantnag, Jammu and Kashmir, India; 2Department of Psychiatry, Government Medical College Anantnag, Anantnag, Jammu and Kashmir, India; 3Department of Microbiology, Government Medical College Srinagar, Srinagar, Jammu and Kashmir, India; 4Department of Community Medicine, Government Medical College Anantnag, Anantnag, Jammu and Kashmir, India; 5Department of Obstetrics and Gynecology, Vaga Hospital, Lucknow, India
Correspondence: Mansoor Ahmad Dar, Department of Psychiatry, Government Medical College, Anantnag, Jammu and Kashmir, Tel +919596010111, Email [email protected] Romaan Jallu, Department of Microbiology, Government Medical College, Srinagar, Jammu and Kashmir, 190010, India, Tel +916006888061, Email [email protected]
Purpose: To determine the feto-maternal outcome in pregnant women infected with SARS-CoV-2 in comparison to non-infected pregnant women and plan management strategies.
Patients and Methods: A retrospective review of case records in the Department of Obstetrics and Gynecology for 1 year was conducted. A total of 6468 case files fulfilling the inclusion criteria were enrolled in the study. Patients who tested positive for SARS CoV-2 and fulfilled inclusion criteria were labeled as cases, whereas patients who tested negative were labeled as controls. Outcome measures including lower segment cesarean section (LSCS) rate, maternal and neonatal intensive care admission and feto-maternal mortality were compared between the two groups.
Results: Our hospital was not an exclusive COVID-19 designated center, and 117 patients infected with SARS-CoV-2 fulfilling the inclusion criteria were enrolled in the study. Fever (67.52%), cough (56.41%), and altered smell (45.29%) were the frequently reported symptoms. Pneumonia affected 16.23% of the cases. LSCS rate was significantly higher in the COVID-19-infected patients (72.41%; OR 2.19; 95% CI 1.46– 3.34; p< 0.001). The rate of maternal ICU admission in COVID-19-infected pregnant women was 11.96% as compared to 0.8% in the non-infected women (OR 16.76; 95% CI 8.72– 30.77; p< 0.001). We observed a significantly higher maternal mortality in COVID-19-infected women (2.56%) [OR 41.61; 95% CI 7.65– 203.5; p< 0.001]. Viral RNA was detected in cord blood and nasopharyngeal swab of one neonate. The neonatal death ratio was high in infected mothers (2.6%) [OR 8.6; 95% CI 1.99– 27.23; p< 0.001].
Conclusion: Significant maternal morbidity, mortality, and neonatal mortality were observed in COVID-19-positive patients.
Keywords: COVID-19, ICU, cesarean, mortality, maternal, neonatal
Introduction
COVID-19 infection, first recognized in December 2019 in Wuhan, China, is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the largest group of RNA viruses.1 SARS-CoV-2 is highly contagious and has caused millions of morbidities and mortalities globally. SARS-CoV-2-infected patients may present with fever, upper or lower respiratory tract infection, and pneumonia in addition to musculoskeletal and gastrointestinal symptoms.2–4 Pregnant women might present with a typical picture or sometimes with non-specific symptoms.5
Contrary to the previous studies, current evidence suggests increased susceptibility of pregnant women to COVID-19 infection because of various physiological changes in respiratory and immune systems.6–8
Our institution, a newly established medical college, and a tertiary care center is located in northern India where not many studies have been conducted on pregnant women infected with COVID-19. Our hospital caters to a population of approximately 2.67 million spread over five districts and two regions. Our hospital has a dedicated record-keeping section and most of the records are well kept. We conducted this study to assess the feto-maternal outcome in COVID-19-infected pregnant women (cases) in comparison to non-infected pregnant women (controls) and to ascertain if the results were any different from world statistics.
Materials and Methods
Objective: To determine the obstetric outcome of the SARS-CoV-2-infected pregnant women as compared to non-infected pregnant women.
Study design: A retrospective case–control study.
Methods: We conducted a retrospective review of records of pregnant women who were admitted and delivered in our hospital from June 2020 to June 2021. Our hospital was not an exclusive COVID-19-dedicated center and only a small percentage of infected patients were managed at our center. A total of 7008 case files were reviewed. Most of the patients who visited our facility had been subjected to COVID-19 rapid antigen testing, and the patients who tested positive on rapid COVID-19 card test had been subjected to COVID-19 rt-PCR (reverse transcriptase polymerase chain reaction) for confirmation of diagnosis. In addition, patients who had symptoms consistent with COVID-19 infection at presentation and tested negative on the rapid card test had been subjected to COVID-19 rt-PCR. A total of 6468 patients who visited and delivered in our facility were finally enrolled in the study. Patients lost to follow-up, and incomplete case records were excluded from the study. COVID-19-positive patients with other reasons for elevated serum liver transaminases and CRP were also excluded from the study. Outcome measures including lower segment cesarean section rate, maternal intensive care unit (ICU) admission, maternal mortality, neonatal intensive care unit (NICU) admission, and neonatal mortality in the COVID-19-positive pregnant women were compared with that of the COVID-19-negative pregnant women. The data thus collected were compiled, tabulated and statistical analysis was done using SPSS 26. Odds ratios with 95% CI were calculated, and their respective p values were estimated.
Approval for conduction of the study was sought from the Institutional Ethics Committee (IEC), GMC Anantnag. Patient consent to review their medical record was not required by the institutional review board (IRB) because all patients admitted to our hospital consent for treatment, and use of their data for teaching and/or research purposes at the time of admission. Patient identification data, sensitive information, hospital ID numbers, or any other data revealing the identity of the patient was kept confidential. The procedures followed, were in accordance with the ethical standards of the responsible committee on human experimentation (institutional) and with the Helsinki Declaration of 1975, revised in 2013.
Results
One hundred and seventeen patients infected with SARS-CoV-2 fulfilling the inclusion criteria were taken as cases against the control of 6351 COVID-19-negative patients. Most of the COVID-19-positive pregnant women presented in the last trimester of pregnancy (Table 1).
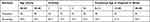 |
Table 1 Patient Profile at the Time of Diagnosis of COVID-19 |
Anemia, gestational diabetes, and hypothyroidism were the commonest co-morbidities present in the COVID-19-positive study population (Figure 1).
 |
Figure 1 Co-morbidities present in COVID-19-infected mothers. |
Fever (67.52%), cough (56.41%), and altered smell (45.29%) were the frequently reported symptoms. Pneumonia was encountered in 16.23% of the COVID-19-positive population (Table 2).
 |
Table 2 Symptomatology of SARS-CoV-2-Infected Pregnant Women |
In addition to elevated serum liver transaminases, most of the COVID-19 infected patients had raised CRP (c-reactive protein) levels (57.26%) and lymphocytopenia (average lymphocyte count=0.84×109 cells/liter) (Table 3). None of the patients had undergone a chest roentgenogram at less than 12 weeks of gestation and none of the patients had undergone a computed tomogram while still pregnant. Sixty-three COVID-19-positive patients had undergone chest X-ray and 88.9% showed findings consistent with SARS-CoV-2 infection. Fourteen patients out of 19 who had been subjected to computed tomogram demonstrated findings in line with SARS-CoV-2 infection (Table 4). CRP and chest imaging were either not ordered or ordered in a small number of COVID-19-negative patients for different reasons like lower respiratory tract infection not attributable to COVID-19 infection, congestive cardiac failure, prolonged leaking, etc. Most of the patients (81.2%) delivered at more than 37 weeks of gestation (Table 5). Out of 65 COVID-19-positive near-term patients who underwent vaginal fluid SARS-CoV-2 testing, none tested positive. Cord blood and nasopharyngeal swab were sent for rt-PCR SARS-CoV-2 only in those neonates who were born while their mothers were still positive for SARS-CoV-2 and only one tested positive (Table 6). Out of 115 neonates born to COVID-positive women 26 (22.6%) were admitted to NICU as compared to 1545 among 5806 (26.60%) (OR 0.80; 95% CI 0.51–1.22; p<0.33) (Table 7). Review of case records revealed a high elective as well as emergency caesarean section rate in COVID-19-positive women (72.41%) as opposed to COVID-19 negative mothers (54.49%) [OR 2.19; 95% CI 1.46–3.34; p<0.001]. Maternal ICU admission was significantly higher in COVID-positive women (11.96%) as compared to COVID-negative women (0.8%) (OR 16.76; 95% CI8.72–30.77; p<0.001) (Tables 8 and 9). Maternal death was significantly higher in SARS-CoV-2-infected pregnant women (OR 41.61; 95% CI 7.65–203.5; p<0.001) There was higher neonatal mortality in the COVID-19-positive group (2.6%) in comparison to COVID-19-negative group (0.31%) (OR 8.60; 95% CI 1.99–27.23; p<0.001) (Tables 7 and 9).
 |
Table 3 Laboratory Findings of the COVID-19-Infected Pregnant Mothers |
 |
Table 4 Image Findings of the COVID-19-Positive Pregnant Women |
 |
Table 5 Mode of Delivery of COVID-19-Positive Pregnant Women |
 |
Table 6 rt-PCR Test Results of Various Fluids in COVID-19-Positive Pregnant Women |
 |
Table 7 Outcome of Neonates Born to COVID-19-Positive Pregnant Mothers |
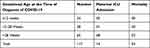 |
Table 8 Maternal Outcome of COVID-19-Infected Pregnant Mothers |
 |
Table 9 Comparison of Maternal and Neonatal Outcome in COVID-19-Positive and -Negative Women |
Discussion
SARS-CoV-2 led to a global pandemic with 486.7 million cases and 6.14 million deaths reported by WHO with increasing daily numbers. India reported 43 million cases and half a million deaths due to novel coronavirus infection. Till November 2021, five variants of SARS-CoV-2 were labeled as variants of concern (VOC) which include alpha (B.1.1.7), beta (B.1.351), gamma (P.1), delta (B.1.617.2), and Omicron (B.1.1.529). Delta (B.1.617.2) was first reported in India in December 2020 and was the predominant strain during our study period.9 This virus can be readily transmitted through respiratory secretions, feces, and fomites.10–17 The chances of contracting the infection depend upon the duration of contact with the infected person, viral load, and immunity of an individual.18,19 Severe manifestations of the infection like pneumonia and marked hypoxia due to SARS-CoV-2 occur more commonly in people with pre-existing co-morbid conditions like diabetes, respiratory disorders, suppressed immune status, etc.20 COVID-19-positive pregnant women might be at an increased risk of developing a severe or critical disease like pneumonia and respiratory failure because of the suppressed immune response, altered hormone milieu and reduced residual lung capacity.21,22 We observed lymphocytopenia in COVID-19-infected pregnant women in addition to elevated CRP and liver transaminases across all gestations in our study, and our findings were supported by the available literature on the subject.23–26 Inflammatory markers like, procalcitonin, interleukin 6, interleukin 2, interleukin 12, serum amyloid A, and serum ferritin, produced by monocytes and macrophages involved in disease pathogenesis were not routinely done in our institute due to cost issues.27–36 Previous evidences suggested against the presence of SARS-CoV-2 in body fluids like urine, amniotic fluid or breast milk.26,37–40 No cases of vertical transmission with sudden acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS) viruses, that are similar to SARS CoV2, have been reported in the past.41,42 But recent research suggests a possible vertical transmission as was found in one of our cases where viral RNA was detected in cord blood and later in the nasopharyngeal swab of the neonate.43,44 The neonate expired later in the neonatal intensive care unit. Vertical transmission of the virus could be possible because of the expression of angiotensin-converting enzyme receptor 2 (ACE2) in placental tissue, uterus, and ovaries and the affinity of the virus for it.45–48 Presence of IgM antibodies against SARS CoV2 in some neonates born to mothers infected with this virus further adds to the possibility of vertical transmission as IgM cannot cross placenta.49,50 Further, it is yet to be established which neonates would have an adverse outcome and what management strategies need to be adopted to prevent such adverse events.
There are controversial results regarding the risk of miscarriage in women infected with SARS-CoV-2, although SARS and MERS viruses have been linked with an increased risk of miscarriage in humans. Although we found a statistically significant risk of miscarriage in COVID-19-infected women as compared to the control group (p=0.001), we are not sure about the actual association between SARS-CoV-2 infection and miscarriage because of the small size of the case sample and further studies to establish or refute the association are needed. We had only one twin intrauterine death in SARS-Co-2-infected population, and the association was statistically insignificant (p=0.22).
The rate of cesarean delivery in SARS-COV-2-infected pregnant women in our study was higher when compared with the non-infected patients (72.41%vs54.49%; OR 2.19; 95% CI 1.46–3.34; p<0.001) particularly if they were hospitalized with pneumonia. Global literature shows controversial results regarding the mode of delivery in COVID-19-infected women, some studies depict an increased cesarean rate while others showed no difference.38,51–54 Most of the cesarean sections upon COVID-19-positive patients in our study were elective in nature, planned and performed during morning hours. In addition to obstetric indications, emergency cesarean sections were performed for worsening respiratory status of COVID-19-infected women, non-availability of individual and isolated birthing suites, and lack of manpower to adequately monitor labor in SARS-CoV-2-infected patients as a large proportion of staff was infected with COVID-19. Pregnancy termination decisions and mode of delivery should be guided by feto-maternal condition, gestational age, and other relevant obstetric factors. Delaying induction of labor just because of COVID-19 infection should be avoided.22 Instrumental delivery can be offered to the laboring mother if she feels exhausted or dyspneic.55–57 In cases of extreme prematurity and deteriorating maternal condition, a quick multidisciplinary team review for the continuation of labor versus emergency cesarean section to facilitate effective cardio-pulmonary resuscitation, should be undertaken.55 Statistically significant proportion of COVID-19 infected women (11.96%) were admitted to the intensive care unit with or without the need for mechanical ventilation in the antepartum period or within 2 weeks after delivery as compared to non-infected pregnant women (0.80%) [OR 16.76; 95% CI8.72–30.77; p<0.001]. Indications for ICU admission in COVID-19-infected women were pneumonia and/or deterioration of respiratory function whereas a myriad of causes was responsible for ICU admission in non-infected mothers, which mainly included obstetric hemorrhage, hypertensive crisis, sepsis, and multi-organ dysfunction syndrome in that order. Diabetes and asthma increased the need for admission to ICU in SARS-CoV-2-infected mothers. In the study by DeBolt et al and Nana et al, the control group comprised of non-pregnant women, and pregnancy was found to be a risk factor for increased morbidity.58,59 The results however might not represent the actual picture because pregnant women not infected with COVID-19 would make a more appropriate control group. Among the 14 women admitted to ICU approximately 50% needed mechanical ventilation and three women died despite mechanical ventilation and other supportive measures. Of these three women, one woman had twin intra-uterine death. Maternal mortality rate was significantly higher in the COVID-19-infected women (2.56%) when compared with non-infected women (0.06%) [OR 41.61; 95% CI 7.65–203.5; p<0.001]. In a multinational cohort study, a mortality rate of 1.6% was observed.60 Morbidity and mortality in our study were higher in second and third trimesters and the pattern is supported by many studies.61 Higher mortality rates in COVID-19-positive women in our study could be attributed to the lesser-equipped ICU in our institution because of its relatively new inception. However, the comparison could be more valid in our study because of a very large COVID-19-negative control sample. We observed a statistically significant increase in neonatal death rate in COVID-19-positive patients compared to the COVID-19-negative control group (OR 8.60; 95% CI 1.99–27.23; p<0.001). Iatrogenic prematurity in women with severe coronavirus infection leads to lower APGAR scores and birthweight and higher admission to NICU. In the INTERCOVID study, pyrexia and breathlessness in the mother, irrespective of the time duration of symptoms were associated with increased neonatal morbidity and mortality. Breastfeeding was not seen to pose any additional risk to the neonate.60 Neonatal intensive care admission rate was not any different in the two groups in our study (p<0.33).
COVID-19 vaccination in pregnant women though widely practiced worldwide for the last year was newly introduced during the study period and was not widely available during that period. In addition, the acceptance for the vaccination was very low because of a multitude of reasons which included inconsistency in data regarding COVID-19 vaccine safety in the pregnant population and the possibility of harm to the fetus. Goncu Ayhan et al documented a low acceptance for COVID-19 vaccination in pregnant women in their study.62 Due to the lack of standard pharmacological treatments for SARS-CoV-2 disease, WHO recommended universal vaccination in an attempt to attain herd immunity for prevention of the disease like other viral infections.63,64 Vaccination has been shown to bring down hospital admission and the severity of the disease. Booster doses of the vaccine are advised to improve immunity against the virus and its variants.65 Due to the above-cited reasons, the percentage of the vaccinated study population was very low and hence prior vaccination status was not taken into consideration in the study.
Based on the symptomatology, oxygen saturation, need for ICU, presence or absence of respiratory failure, septic shock, and multiple organ dysfunction, patients are categorized into having mild, moderate, severe, and critical disease.66
Asymptomatic or mildly symptomatic pregnant women can be provided home-based care using telehealth, video-conferencing, etc. Patients with severe, critical disease, co-morbidities, or immune-compromised disorders need to be taken care of at a COVID-19-designated facility, equipped to take care of such patients.
Molnupiravir, paxlovid, sotrovimab, remdesivir, antisera, and immune-modulatory agents like corticosteroids are being used for the treatment of COVID-19 infection in non-pregnant population with varied results. The use of chloroquine and its hydroxyl derivative, lopinavir, ritonavir, and ivermectin for the treatment of COVID-19 is not supported by contemporary research.66 We could not find any literature where pregnant women were included in clinical trials for testing the efficacy and safety of various available pharmacotherapies. Anticoagulants, remdesivir, and azithromycin have been listed as pregnancy category B by the FDA. The safety of other agents has not been established yet.67
Where testing capacity allows, universal testing of all labor admissions should be undertaken to avoid admission of asymptomatic COVID-19-positive mothers to COVID-19-negative facilities/wards. Labor presents a unique challenge in this COVID-19 pandemic. Social isolation for about 2 weeks starting at the onset of the 37th week of pregnancy in addition to COVID appropriate behavior can be advised in planned labor admissions.22
Hypercoagulability of pregnancy and COVID-19 may put patients at a high risk of venous thromboembolism. Low molecular weight heparins (LMWH) should be started as soon after delivery as practically feasible keeping in view that there is no postpartum hemorrhage and at least 4 hours have elapsed since between regional analgesia/anesthesia or removal of an epidural catheter. Regional anesthesia/analgesia should be delayed for at least 12 hours after the last dose of LMWH (RCOG).
Currently, it is less known whether breast milk poses the risk of transmission from mother to the infant; however, transmission from mother to the infant during breastfeeding due to respiratory droplets has been established.68 Presently, most research institutions allow breastfeeding with standard universal precautions.69,70
Conclusion
COVID-19 infection during pregnancy is associated with a high propensity for maternal morbidity and mortality. Close monitoring is required, especially in the third trimester and labor. Continuous and ongoing mutations in the viral genome and hence the spike protein limit the possibility of developing a single pharmacological agent, antisera, or vaccine against all the virus strains. Earlier confirmation of COVID-19 infection status, a clear understanding of all possible symptoms of infection during pregnancy, highly trained and dedicated staff, and proper management are important to prevent adverse outcomes. Vaccination, a high index of suspicion, and timely intervention seem to be the key. Recruitment of pregnant women in clinical trials to test the safety and efficacy of various pharmacological agents should be done by researchers, to plan better management strategies. In the absence of any definitive therapy, management of COVID-19 symptomatic pregnant women remains challenging.
Acknowledgments
All the authors acknowledge the contribution of Mr Suheel Ahmad working as a data entry operator in the Department of Obstetrics and Gynecology, Government Medical College Anantnag, in planning the statistical analysis of this study.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Shwartz DA, Graham AL. Potential maternal and infant outcomes from (Wuhan) coronavirus 2019 nCov infecting pregnant women: lessons from SARS, MERS and other human coronavirus infections. Viruses. 2020;12:194. doi:10.3390/v12020194
2. Lai CC, Liu YH, Wang CY, et al. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): facts and myths. J MicrobiolImmunol Infect. 2020. doi: 10.1016/j.jmii.2020.02.012
3. Guan WJ, Ni ZY, Hu Y, et al; China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi:10.1056/NEJMoa2002032
4. Wong HY, Lam HY, Fong AH, et al. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2019;296:E72–E78.
5. Afshar Y, Gaw SL, Flaherman VJ. on behalf of the Pregnancy Coronavirus Outcomes Registry (PRIORITY) study clinical presentation of coronavirus disease 2019 (COVID-19) in pregnant and recently pregnant people. Obstet Gynecol. 2020;136(6):1117–1125. doi:10.1097/AOG.0000000000004178
6. Liu H, Wang LL, Zhao SJ, Kwak-Kim J, Mor G, Liao AH. Why are pregnant women susceptible to COVID-19? An immunological viewpoint. J Reprod Immunol. 2020;139:103122. doi:10.1016/j.jri.2020.103122
7. Zhao X, Jiang Y, Zhao Y, et al. Analysis of the susceptibility to COVID-19 in pregnancy and recommendations on potential drug screening. Eur J Clin Microbiol Infect Dis. 2020;39(7):1209–1220. doi:10.1007/s10096-020-03897-6
8. Ellington S, Strid P, Tong VT, et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status—United States, January 22–June 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:769–775. doi:10.15585/mmwr.mm6925a1
9. Aleem A, Akbar Samad AB, Slenker AK. Emerging variants of SARS-CoV-2 and novel therapeutics against coronavirus (COVID-19). In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. PMID: 34033342.
10. Cheng VCC, Wong SC, Chen JHK, et al. Escalating infection control response to the rapidly evolving epidemiology of the coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect Control Hosp Epidemiol. 2020;41:493–498. doi:10.1017/ice.2020.58
11. Chia PY, Coleman KK, Tan YK, et al. Detection of air and surface contamination by SARS-CoV-2 in hospital rooms of infected patients. Nat Commun. 2020;11:2800. doi:10.1038/s41467-020-16670-2
12. Faridi S, Niazi S, Sadeghi K, et al. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci Total Environ. 2020;725:138401. doi:10.1016/j.scitotenv.2020.138401
13. Guo Z-D, Wang Z-Y, Zhang S-F, et al. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis. 2020;26:1583–1591. doi:10.3201/eid2607.200885
14. Santarpia JL, Rivera DN, Herrera V, et al. Transmission potential of SARS-CoV-2 in viral shedding observed at the University of Nebraska Medical Center (Preprint). MedRxiv. 2020. doi:10.1101/2020.03.23.20039446
15. Wong SCY, Kwong RTS, Wu TC, et al. Risk of nosocomial transmission of coronavirus disease 2019: an experience in a general ward setting in Hong Kong. J Hosp Infect. 2020;105:119–127. doi:10.1016/j.jhin.2020.03.036
16. Hui DSC, Zumla A. Severe acute respiratory syndrome: historical, epidemiologic, and clinical features. Infect Dis Clin North Am. 2019;33:869–889. doi:10.1016/j.idc.2019.07.001
17. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi:10.1056/NEJMoa2001316
18. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, evaluation and treatment coronavirus (COVID-19); 2020. Available from: https://www.ncbi.nlm.nih.gov/pubmed/32150360.
19. Yu N, Li W, Kang Q, et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. Lancet Infect Dis. 2020;20:559–564. doi:10.1016/S1473-3099(20)30176-6
20. Ejaz H, Alsrhani A, Zafar A, et al. COVID-19 and comorbidities: deleterious impact on infected patients. J Infect Public Health. 2020;13(12):1833–1839. PMID: 32788073; PMCID: PMC7402107. doi:10.1016/j.jiph.2020.07.014
21. Zhou Y, Fu B, Zheng X, et al. Pathogenic T-cells and inflammatory monocytes incite inflammatory storms in severe COVID-19 patients. Natl Sci Rev. 2020;7:998–1002. doi:10.1093/nsr/nwaa041
22. Boelig RC, Manuck T, Oliver EA, et al. Labor and delivery guidance for COVID-19. Am J ObstetGynecol MFM. 2020;2(2):100110. doi:10.1016/j.ajogmf.2020.100110
23. Wu C, Yang W, Wu X, et al. Clinical manifestation and laboratory characteristics of SARS-CoV-2 infection in pregnant women. VirologicaSinica. 2020;35(3):305–310. doi:10.1007/s12250-020-00227-0
24. Pereira A, Cruz-Melguizo S, Adrien M, Fuentes L, Marin E, Perez-Medina T. Clinical course of coronavirus disease-2019 in pregnancy. Acta Obstetricia et GynecologicaScandinavica. 2020;99(7):839–847. doi:10.1111/aogs.13921
25. Blitz MJ, Rochelson B, Meirowitz N, et al. Maternal mortality among women with coronavirus disease 2019. Am J Obstetr Gynecol. 2019. doi:10.1016/j.ajog.2020.06.020
26. Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi:10.1016/S0140-6736(20)30360-3
27. Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi:10.1016/S0140-6736(20)30628-0
28. Stebbing J, Phelan A, Griffin I, Tucker C, Oechsle O, Smith D. COVID-19: combining antiviral and anti-inflammatory treatments. Lancet Infect Dis. 2020;20(4):400–402. doi:10.1016/S1473-3099(20)30132-8
29. Tay MZ, Poh CM, Renia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:1–12. doi:10.1038/s41577-019-0258-9
30. Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi:10.1016/S2213-2600(20)30076-X
31. Cheng K, Wei M, Shen H, Wu C, Chen D, Xiong W. Clinical characteristics of 463 patients with common and severe type coronavirus disease (In Chinese). Shanghai Med J. 2020;3:1–15.
32. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934. doi:10.1001/jamainternmed.2020.0994
33. Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin Infect Dis. 2020;71:762–768. doi:10.1093/cid/ciaa248
34. Xiang T, Liu J, Xu F, Cheng N, Liu Y, Qian K. Analysis of clinical characteristics of 49 patients with Novel Coronavirus Pneumonia in Jiangxi province (In Chinese). Chin J Respir Crit Care Med. 2020;19(2):1–7.
35. Chen L, Liu HG, Liu W, Liu J, Liu K, Shang J. Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia (In Chinese). Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(3):203–208. doi:10.3760/cma.j.issn.1001-0939.2020.03.013
36. Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy Eur J Allergy Clin Immunol. 2020;75:1730–1741. doi:10.1111/all.14238
37. Fan C, Lei D, Fang C. Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? Clin Infect Dis. 2020;23:45.
38. Della Gatta AN, Rizzo R, Pilu G, Simonazzi G. Coronavirus disease 2019 during pregnancy: a systematic review of reported cases. Am J Obstet Gynecol. 2020;223:36–41. doi:10.1016/j.ajog.2020.04.013
39. Yang Z, Wang M, Zhu Z, Liu Y. Coronavirus disease 2019 (COVID-19) and pregnancy: a systematic review. J Matern Fetal Neonatal Med. 2020;35:1619–1622.
40. Yang Z, Liu Y. Vertical transmission of severe acute respiratory syndrome coronavirus 2: a systematic review. Am J Perinatol. 2020;37:1055–1060. doi:10.1055/s-0040-1712161
41. Principi N, Bosis S, Esposito S. Effects of coronavirus infections in children. Emerg Infect Dis. 2010;16:183–188. doi:10.3201/eid1602.090469
42. Zumla A, Hui DS, Perlman S. Middle East respiratory syndrome. Lancet. 2015;386:995–1007. doi:10.1016/S0140-6736(15)60454-8
43. Kotlyar AM, Grechukhina O, Chen A, et al. Vertical transmission of coronavirus disease 2019: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224(1):35–53.e3. PMID: 32739398; PMCID: PMC7392880. doi:10.1016/j.ajog.2020.07.049
44. Vivanti AJ, Vauloup-Fellous C, Prevot S, et al. Transplacental transmission of SARS-CoV-2 infection. Nat Commun. 2020;11:3572. doi:10.1038/s41467-020-17436-6
45. Levy A, Yagil Y, Bursztyn M, Barkalifa R, Scharf S, Yagil C. ACE2 expression and activity are enhanced during pregnancy. Am J PhysiolRegulIntegr Comp Physiol. 2008;295:R1953–R1961. doi:10.1152/ajpregu.90592.2008
46. Valdés G, Neves LA, Anton L. Distribution of angiotensin-(1–7) and ACE2 in human placentas of normal and pathological pregnancies. Placenta. 2006;27:200–207. doi:10.1016/j.placenta.2005.02.015
47. Jing Y, Run-Qian L, Hao-Ran W. Potential influence of COVID-19/ACE2 on the female reproductive system. Mol Hum Reprod. 2020;26:367–373. doi:10.1093/molehr/gaaa030
48. Li M, Chen L, Zhang J, Xiong C, Li X. The SARS-CoV-2 receptor ACE2 expression of maternal-fetal interface and fetal organs by single-cell transcriptome study. PLoS One. 2020;15:e0230295.
49. Dong L, Tian J, He S. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. 2020;323:1846–1848. doi:10.1001/jama.2020.4621
50. Zeng H, Xu C, Fan J. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA. 2020;323:1848–1849. doi:10.1001/jama.2020.4861
51. Cavalcante MB, De Melo Bezerra cavalcante CT, Cavalcante ANM, Sarno M, Barini R, Kwak-Kim J. COVID-19 and miscarriage: from immunopathological mechanisms to actual clinical evidence. J Reprod Immunol. 2021;148:103382. PMID: 34534878; PMCID: PMC8429080. doi:10.1016/j.jri.2021.103382
52. Di Mascio D, Khalil A, Saccone G, et al. Outcome of coronavirus spectrum infections (SARS, MERS, COVID-19) during pregnancy: a systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2020;2(2):100107. PMID: 32292902; PMCID: PMC7104131. doi:10.1016/j.ajogmf.2020.100107
53. Chen L, Li Q, Zheng D, Jiang H, Yuan Y, Zou L. Clinical characteristics of pregnant women with Covid-19 in Wuhan, China. N Engl J Med. 2020;382(25). doi:10.1056/nejmc2009226
54. Malhotra Y, Miller R, Bajaj K, et al. No change in cesarean section rate during COVID-19 pandemic in New York City. Eur J Obstet Gynecol Reprod Biol. 2020;253:328–329. doi:10.1016/j.ejogrb.2020.06.010
55. World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance; 2020. Available from: https://apps.who.int/iris/bits.
56. The Royal College of Obstetricians and Gynecologists. Royal College of Midwives. Coronavirus (COVID-19) infection in pregnancy: information for healthcare professionals; 2020. Available from: https://www.rcog.org.uk/global.
57. Giaxi P, Maniatelli E, Vivilaki VG. Evaluation of mode of delivery in pregnant women infected with COVID-19. Eur J Midwifery. 2020;4(July). doi:10.18332/ejm/123888
58. DeBolt CA, Bianco A, Limaye MA, et al. Pregnant women with severe or critical coronavirus disease 2019 have increased composite morbidity compared with nonpregnant matched controls. Am J Obst Gynecol. 2019. doi:10.1016/j.ajog.2020.11.022
59. Nana M, Nelson-Piercy C. COVID-19 in pregnancy. Clin Med. 2021;21(5):e446–e450. PMID: 34507928; PMCID: PMC8439502. doi:10.7861/clinmed.2021-0503
60. Villar J, Ariff S, Gunier RB, et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection: the INTERCOVID Multinational Cohort Study. JAMA Pediatr. 2021;175(8):817–826. PMID: 33885740; PMCID: PMC8063132. doi:10.1001/jamapediatrics.2021.1050
61. Hantoushzadeh S, Shamshirsaz AA, Aleyasin A, et al. Maternal death due to COVID-19 disease. Am J ObstetGynecol. 2020;223:
62. Goncu Ayhan S, Oluklu D, Atalay A, et al. COVID-19 vaccine acceptance in pregnant women. Int J Gynaecol Obstet. 2021;154(2):291–296. PMID: 33872386; PMCID: PMC9087778. doi:10.1002/ijgo.13713
63. Hinman AR. The eradication of Polio: have we succeeded? Vaccine. 2017;35(42):5519–5521. PMID: 28890190. doi:10.1016/j.vaccine.2017.09.015
64. Durrheim DN, Crowcroft NS, Strebel PM. Measles - The epidemiology of elimination. Vaccine. 2014;32(51):6880–6883. PMID: 25444814. doi:10.1016/j.vaccine.2014.10.061
65. Andrews N, Stowe J, Kirsebom F, et al. Effectiveness of COVID-19 booster vaccines against COVID-19-related symptoms, hospitalization and death in England. Nat Med. 2022;28:831–837. doi:10.1038/s41591-022-01699-1
66. Cascella M, Rajnik M, Aleem A, et al. Features, evaluation, and treatment of coronavirus (COVID-19). In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022
67. Arco-Torres A, Cortés-Martín J, Tovar-Gálvez MI, Montiel-Troya M, Riquelme-Gallego B, Rodríguez-Blanque R. Pharmacological treatments against COVID-19 in pregnant women. J Clin Med. 2021;10(21):4896. PMID: 34768416; PMCID: PMC8584594. doi:10.3390/jcm10214896
68. Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus Disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. 2020;222(5):415–426. doi:10.1016/j.ajog.2020.02.017
69. Poon LC, Yang H, Lee JCS, et al. ISUOG Interim Guidance on 2019 novel coronavirus infection during pregnancy and puerperium: information for healthcare professionals. Ultrasound Obstet Gynecol. 2020;55(5):700–708. doi:10.1002/uog.22013
70. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J ThrombHaemost. 2020;18(5):1094–1099. doi:10.1111/jth.14817
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
