Back to Journals » Journal of Blood Medicine » Volume 13
Distribution of ABO and Rhesus Types in the Northern Asir Region in Saudi Arabia
Authors Belali TM
Received 22 July 2022
Accepted for publication 3 November 2022
Published 8 November 2022 Volume 2022:13 Pages 643—648
DOI https://doi.org/10.2147/JBM.S383151
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Tareg M Belali
Faculty of Applied Medical Sciences, University of Bisha, Bisha, 67714, Saudi Arabia
Correspondence: Tareg M Belali, University of Bisha, 255, Al Nakhil, Bisha, 67714, Saudi Arabia, Tel +966 17623 8162, Email [email protected]
Background and Objectives: The ABO blood group system is used to denote the presence of one, both, or neither of the A and B antigens on erythrocytes. In humans, this is the most important of the 43 different blood type (or group) classification systems currently recognized. Distribution of ABO and Rh among the Saudi population could affect many factors such as blood transfusion, prognosis, resistance and susceptibility to diseases. The impetus of this study was to develop an understanding of the distribution of the ABO and Rh types of healthy volunteer blood donors in the northern Asir region of Saudi Arabia, comparing the findings to similar studies. Understanding the frequency of different blood types in different populations is imperative.
Subjects and Methods: This study was performed during the period of January 1, 2020, to December 31, 2020, using samples from 4167 voluntary subjects obtained from the blood bank of the King Abdullah Hospital, Bisha. Commercially provided anti-A, anti-B and anti-D antibodies were used for the standard blood grouping procedure.
Results: The findings in this study showed that O was the most prominent ABO blood group, whereas AB was the least so. The frequency of the blood type A was the second highest, followed by the blood group B, whereas Rh positivity was more common than Rh negativity.
Conclusion: O+ > A+ > B+ > O-> AB+> A-> B- > AB- was found to be the order of blood group frequency in the current study.
Keywords: ABO, rhesus, donors, immunoglobulins
Introduction
Landsteiner described the ABO blood group system in the 20th century. Blood cell antigens are inherited from the parents through a single gene and have clinical significance and RBC antigens are a group of structural proteins and carbohydrates that are present on the extracellular surface of the RBC membrane.1–3 To date, there are 43 blood group systems with 360 known antigens according to the ISBT, which are able to stimulate an immune response. These systems include ABO and Rh, which in the case of mismatching could result in severe forms of posttransfusion reactions.2 Antibodies in the ABO system are typically found in the serum of healthy people.4 For example, immunoglobulins such as IgM and IgG against blood groups antigens may very well be present in individuals that express A and B antigens. However, IgM and IgG against ABO antigens are mostly present in individuals that lack the A and B antigens. Individuals are either RhD positive or RhD negative depending on the presence or absence of the RhD phenotype on the surface of the red cells. In blood transfusion therapy, antigens A, B and D are the most important red cell antigens, as donor-patient ABO mismatching could result in severe posttransfusion reactions.2 Except for auto anti-D cases, Individuals whose red cells lack the D antigen cannot have anti-D in their serum unless they have been exposed to a sensitizing event that initiated the production of anti-D antibodies, in contrast to the case of A and B antigens. Overall, blood group compatibility has clinical significance that is essential for blood management in a wide variety of clinical cases. The ABO and Rh phenotype frequencies in given populations in different parts of the world have been studied. Studies that have been conducted in different parts of Saudi Arabia show similar frequencies of the ABO Rh group. For instance, a study that was conducted in the Eastern region found that the O blood group is the most prevalent, followed by A, B and AB respectively. Moreover, Rh-positive blood donors were more prevalent than Rh-negative blood.5 Furthermore, several studies conducted in the Al-Jouf, Hail, Najran and Jazan provinces, showed similar patterns of ABO Rh distribution [Eweidah et al 20116 and Abdullah et al 20107]. Such studies may provide an idea about different hematological conditions, such as hemolytic disease of the fetus and newborn (HDFN). Blood groups are known to have some association with several clinical conditions, such as urinary tract infection and diabetes [Babiker Mohammed 20138, Sinha et al 20159]. The familiarity of the frequencies of ABO and Rh blood groups in the residents of a given regional area is essential for proper operative management at local hospitals and blood banks. Such a study may contribute to the effective management of a blood bank’s inventory and provide safe and reliable blood transfusion services. Thus, this study purposely focused on the population of the Bisha Province in the Asir region.
Objective
This study aimed to screen and determine the frequencies of the occurrence of ABO and Rh blood groups among residents of the northern Asir region in Saudi Arabia. This information will provide an idea about the distribution of particular blood groups in the area. This study included many donors from both the urban and rural populations of the province.
Methodology
A cross-sectional study was conducted using blood samples collected from blood donors who belong to different ethnic groups.
The Saudi Ministry of Health’s (MOH) criteria for blood donation was followed in this study.10 As per the MOH criteria, donors were between 18 and 65 years old (male and female) and weighed above 50 kg. The donors met the minimum hemoglobin concentration required for both genders (between 14 and 17 g/dl for males and 12–14 g/dl for females) with normal vital signs, and they were at the blood bank for various reasons. Blood collection from the donors followed a clinical examination that determined their physical wellbeing. Samples were collected over a period of 1 year, from January 1, 2020, to December 31, 2020.
All volunteers donated blood of their own free will and after fulfilling the ethical criteria of the study. All donors provided informed written consent to participate in this study. The study was conducted under the tenets of the Declaration of Helsinki. The Institution Review Board of the University of Bisha approved the study protocols. Blood typing and collection from fit, voluntary donors was performed at the blood bank of the King Abdullah Hospital. The hospital is located in Bisha city, which is an important educational and urban center for the population of the northern Asir region in Saudi Arabia. The city is located in the southern part of Saudi Arabia at altitude of 610 meters above sea level.11 The ABO and Rh statuses of 4167 samples were analyzed by forward blood grouping using commercially acquired anti-A, anti-B and anti-D antisera (Beckman Coulter Inc. Clones; Anti-A 9113D10, Anti-B 9621A8, Anti-D P3X61 + P3X21223B10 +P3X290 + P3X35). Agglutination reactions were observed after mixing the blood and antibodies on the slides, and the results were recorded.
The final ABO and Rh blood groups for each sample were determined based on the presence or absence of agglutination. Using the Microsoft Excel 2019 (Office 17) software, the data on the frequency of ABO and Rh-D blood groups were reported in simple percentages.
Results
In this study, which includes 4167 Saudi and non-Saudi voluntary blood donors, the majority of blood donors within the age range of 18–65 years were male (4058), while (109) were female. The most prominent blood group was O (45.90%), followed by A (27.40%), B (21.71%) and AB (5%) (Table 1).
 |
Table 1 Frequency and Distribution of the ABO System |
The most prominent Rh factor among the donors in this study was Rh positive (89.12%) followed by Rh negative (10.87%) (Table 2).
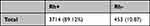 |
Table 2 Frequency and Distribution of Rh Factor |
Upon complete ABO and Rh factor analysis for all donors, it was noted that the blood group O+ was the most prevalent blood type (38.68%), followed by types A+ (24.81%), B+ (20.90%), O- (7.22%), AB+ (4.72%), A- (2.59%), B- (0.81%) and AB- (0.23%) (Table 3).
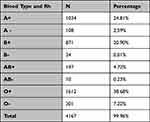 |
Table 3 Distribution of ABO System and Rh Factor |
Discussion
The current study determined the distribution of ABO and Rh types in the northern Asir region. The vast majority of the participants were male, which is consistent with similar studies in other parts of the Arabian Peninsula.12 The reason behind the low number of female participants according to,13 was an inability to reach the blood donation centers and a fear of anemia, according to Al-Johar et al.14 The most prominent hurdle preventing them from donating was the difficulty of reaching the blood bank, as they could not drive cars or use public transport alone.15,16 Due to the infrequent donations from females, the ABO/Rh distribution might not be an accurate assessment of the true frequency.
Knowing the ABO-Rh D frequency in a given population helps to predict the prevalence of ABO and Rh HDFN.4,17,18 Moreover, the essential interaction among blood groups, organ transplantation and transfusion therapy make identifying the patient’s blood type one of the vital sources of information in any clinical patient’s report.19
The heterozygosity of blood types is attributed to the pattern of the ABO group and Rh mode of inheritance. A and B alleles are inherited in an autosomal codominant fashion, whereas the O allele is autosomal recessive. On the other hand, the Rh factor is inherited through autosomal dominant pattern.3,20
There is a well-known correlation between ABO and some diseases such as cancer, hematologic disorders, cardiovascular diseases and malaria, but there are also many factors that affect the outcome of the disease.21–24 Furthermore, several studies have linked blood groups to certain clinical conditions, such as stomach cancer,25 and infectious diseases, such as COVID-19, HBSAg, HCV, HIV and syphilis. For example, in patients who are suffering from stomach cancer, the prevalence of blood group A was greater than that of blood group O.26 Most recently, a relationship between COVID-19 and blood groups has been established. The number of COVID-19 patients with blood group A was significantly higher than patients with other blood groups. On the other hand, the number of COVID-19 patients with blood group O was much lower than that of other individuals. This finding suggests that individuals with the blood group A are at higher risk of COVID-19 infection and more severe clinical symptoms than individuals with the blood group O.27 Among blood donors, a study that analyzed the association of blood groups to HBsAg has described the blood group O as the most prevalent blood group associated with HBsAg, followed by the blood groups B, AB and A.28 Another study that was conducted in Northern India has found that HBsAg is highly associated with individuals with the B blood group but is less prevalent in AB blood group donors. However, it has been concluded that ABO blood groups are not statistically associated with HBsAg positivity among their cohort.29 A recent study in Pakistan found that Individuals with the blood group O and Rh-negative factor had a strong association with HCV viremia compared to other blood types.30 Interestingly, patients with β- Thalassemia demonstrated a higher association between A and B blood types while those with O blood groups appeared to have less vulnerability to the virus. Moreover, HCV was more prevalent in patients with the Rh D positive factor. Furthermore, a higher correlation between the blood group O and HIV infection was described by Sayal et al (1996).31 However, participants with the blood group B demonstrated a lower prevalence of HIV in the same study. A more recent study32 also described a higher incidence of HIV infection among O blood group donors compared to other blood types. On the other hand,33 Mohammadali et al (2014) failed to establish a significant association between syphilis infection and blood groups, however, a high prevalence of syphilis was noted among Rh D positive participants. Another study failed to link blood groups to obesity.34 An earlier study that was conducted in the eastern region of Saudi Arabia estimated the frequency of ABO blood groups and its findings relate to the results of the present study.5 The O blood group was determined to be the most prominent blood group in the current study (45%) and in the eastern region at large (51%). In both studies, the blood group A was the second most common blood type (27% and 26.5% in this study and the eastern region, respectively). Similarly, the B blood group was the third most common in both regions (21% and 18%, respectively). AB was the least dominant blood group in the eastern region (4%) and the northern Asir region (5%). Individuals who were rhesus negative in the eastern region accounted for only 8%, whereas Rh positive blood donors accounted for 92%. This finding is consistent with the findings in this study.
A study that described the allele frequency at the ABO locus in Middle Eastern countries has shown a high frequency of the blood group A in the northern region of the Arabian Peninsula, whereas the frequency of the same blood group was lower in the southern part and at a minimum in the central region of Saudi Arabia. In the northeastern part of the Arabian Peninsula, the blood group B was the most prevalent blood type. A high frequency of the blood group O was noted in the southwestern Arabian Peninsula, which is in general agreement with the findings in the current study. Nevertheless, the O blood group is considerably less frequent in the northeastern part of the region of interest.12
Several studies have found that the B blood group is the most prominent in central and western Africa, whereas O is the most common blood group in southern and eastern Africa.27 According to one study, the blood group B is the most common in Nepal. The most common blood group in the United Kingdom is O, and the least common is AB.27 Another study in Morocco showed a different ABO Rh frequency from this study.35 Benahadi et al (2013) have found the A blood group to be the most prominent, followed by B, AB and O at 32.86%, 15.80%, 4.53% and 46.80%, respectively. Similar to the findings in the current study, the Rh-negative factor was less prevalent (0.09%) than the Rh-positive factor (91.00%) among the participants. In disagreement with the findings in the current study, in Greece,36 found that the blood group A was the most prevalent (36.11%), followed by O (35.13%), B (15.53%) and AB (4.64%). However, most of the donors were Rh-positive (91.41%), while the Rh-negative factor was less common (8.59%) among the participants, which is in agreement with the current study. These geographical differences can be interpreted using factors such as genetic mapping, ethnic background and migration frequency of a given population.
The findings of this study define the frequency of blood groups in the kingdoms north of the southwest regions. This area of the kingdom is not known to have a prevalence of diseases that are related to the blood, such as thalassemia and sickle cell anemia.25,37
Furthermore, this study had grouped the donors based on their gender because some studies have indicated that the variation in blood group inheritance between men and women could be attributed to some sex determining genes alongside the mode of inheritance of ABO-Rh genes.38–40
Conclusion
The current study provides a better understanding of the ABO and Rh distribution among the residents of the northern Asir region, Saudi Arabia. This study identified the O+ blood group to be the most prevalent and AB- to be the least so in the studied area. The findings of this study contribute to the improvement of resource management and efficient health planning. Given the recognized connection between certain clinical conditions and blood groups, such studies could be helpful in the prediction of disease prognosis in certain geographical regions.
Limitations of the Study
Overall, since this study was conducted during the COVID-19 pandemic, the participants experienced some difficulties in reaching the collection site to donate blood. The other limitation of this study is the limited number of female participants in comparison to male donors.
Ethical Statement
This study was approved by the ethical committee at the University of Bisha.
Acknowledgments
The author extends their appreciation to the Deputyship of Research & Innovation, Ministry of Education in Saudi Arabia, for funding this research work.
Funding
This research work was funded through Promising Program under Grant Number (UB- Promising - 1- 1443).
Disclosure
The author declares no conflicts of interest in relation to this work.
References
1. Bodmer W. Genetic characterization of human populations: from ABO to a genetic map of the British people. Genetics. 2015;199(2):267–279. doi:10.1534/genetics.114.173062
2. National Center for Biotechnology Information (U.S.); Dean L. Blood Groups and Red Cell Antigens. Bethesda, Md.: NCBI /z-wcorg/; 2005.
3. Reid M, Mohandas N. Red blood cell blood group antigens: structure and function. Semin Hematol. 2004;41(2):93–117. doi:10.1053/j.seminhematol.2004.01.001
4. Singh A, Srivastava RK, Deogharia KS, Singh KK. Distribution of ABO and Rh types in voluntary blood donors in Jharkhand area as a study conducted by RIMS, Ranchi. J Fam Med Prim Care. 2016;5(3):631–636. doi:10.4103/2249-4863.197319
5. Bashwari LA, Al-Mulhim AA, Ahmad MS, Ahmed MA. Frequency of ABO blood groups in the Eastern Region of Saudi Arabia. Saudi Med J. 2001;22(11):1008–1012.
6. Eweidah MH, Rahiman S, Ali MDH, Al-Shamary A. Distribution of ABO and rhesus (RHD) blood groups in Al-Jouf Province of the Saudi Arabia. Null. 2011;13(2):99–102.
7. Abdullah S. Frequency of ABO and Rh blood groups in the Jazan region of Saudi Arabia. Pak J Med Sci. 2010;26:818–821.
8. Mohammed. B. ABO Blood Group and Susceptibility to Urinary Tract Infection in Children. sudan academy of science; 2013.
9. Sinha A, Jain A, Shukla A, et al. Association of ABO blood groups with type-2 diabetes mellitus and its complications. Int J Diabetes Dev Ctries. 2015;35:S579. doi:10.1007/s13410-016-0469-6
10. Blood Donation. Facts and guidelines; June 8, 2014. Available from: https://www.moh.gov.sa/en/HealthAwareness/EducationalContent/Blog/1435/Pages/Artical-2014-06-08.aspx.
11. Al Arabiya English. Exploring Saudi Arabia: how Asir’s Bisha became the ‘town of Palm Dates’; May 20, 2020. Available from: https://english.alarabiya.net/life-style/travel-and-tourism/2018/07/11/Exploring-Saudi-Arabia-How-Asir-s-Bisha-became-The-town-of-palm-dates.
12. Alsuhaibani ES, Kizilbash NA, Afshan K, Malik S. Distribution and clinical trends of the ABO and Rh genes in select Middle Eastern Countries. Genet Mol Res. 2015;14(3):10729–10742. doi:10.4238/2015.September.9.12
13. Abolfotouh MA, Al-Assiri M, Al Askar A, et al. Public awareness of blood donation in Central Saudi Arabia. Int J Gen Med. 2014;7:401–410. doi:10.2147/IJGM.S67187
14. Al-Johar AW, Al-Saud A, Abalkhail Y, et al. Why do-Saudi women refrain donating their blood? --a study on the attitude, belief and motivation of Saudi female university students towards blood donation. Clin Lab. 2016;62(5):771–779. doi:10.7754/clin.lab.2015.150718
15. Bani M, Giussani B. Gender differences in giving blood: a review of the literature. Blood Transfus. 2010;8(4):278–287. doi:10.2450/2010.0156-09
16. Prados Madrona D, Fernández Herrera MD, Prados Jiménez D, et al. Women as whole blood donors: offers, donations and deferrals in the province of Huelva, South-Western Spain. Blood Transfus. 2014;12(Suppl 1):s11–s20. doi:10.2450/2012.0117-12
17. Akanmu AS, Oyedeji OA, Adeyemo TA, Ogbenna AA. Estimating the risk of ABO Hemolytic disease of the newborn in Lagos. J Blood Transfus. 2015;2015:560738. doi:10.1155/2015/560738
18. Mbalibulha Y, Muwanguzi E, Mugyenyi GR, Natukunda B. Occurrence of anti-D alloantibodies among pregnant women in Kasese District, Western Uganda. J Blood Med. 2015;6:125–129. doi:10.2147/JBM.S80977
19. Rydberg L. ABO-incompatibility in solid organ transplantation. Transfus Med. 2001;11(4):325–342. doi:10.1046/j.1365-3148.2001.00313.x
20. Canizalez-Román A, Campos-Romero A, Castro-Sánchez JA, et al. Blood groups distribution and gene diversity of the ABO and Rh (D) Loci in the Mexican population. Biomed Res Int. 2018;2018:1925619. doi:10.1155/2018/1925619
21. Abegaz SB, Erg n S. Human ABO blood groups and their associations with different diseases. Biomed Res Int. 2021;2021:6629060. doi:10.1155/2021/6629060
22. Amoroso A, Magistroni P, Vespasiano F, et al. HLA and AB0 polymorphisms may influence SARS-CoV-2 infection and COVID-19 severity. Transplantation. 2021;105(1):193–200. doi:10.1097/TP.0000000000003507
23. Dahlén T, Clements M, Zhao J, et al. An agnostic study of associations between ABO and RhD blood group and phenome-wide disease risk. eLife. 2021;10. doi:10.7554/eLife.65658
24. Krog GR, Donneborg ML, Hansen BM, et al. Prediction of ABO hemolytic disease of the newborn using pre- and perinatal quantification of maternal Anti-A/Anti-B IgG titer. Pediatr Res. 2021;90(1):74–81. doi:10.1038/s41390-020-01232-5
25. Kalokola FM, Kumar A, Lema RA, et al. Sickle cell-thalassemia associated with G6PD deficiency in an African Girl in Tanzania. East Afr Med J. 1983;60(7):512–514.
26. Aird I, Bentall HH, Roberts JAF. A relationship between cancer of stomach and the ABO blood groups. Br Med J. 1953;1(4814):799–801. doi:10.1136/bmj.1.4814.799
27. Zhao J, Yang Y, Huang H, et al. Relationship between the ABO blood group and the COVID-19 susceptibility. medRxiv. 2020;2020:20031096. doi:10.1101/2020.03.11.20031096
28. Saadoon IH. The Frequency of HBsAg in blood donors in Tikrit city. Med J Tikrit Univ. 2016;21(1):200–204.
29. Behal R, Jain R, Behal KK, et al. Seroprevalence and risk factors for hepatitis B virus infection among general population in Northern India. Arq Gastroenterol. 2008;45(2):137–140. doi:10.1590/S0004-28032008000200009
30. Mahnoor M, Noreen M, Imran M, et al. Association of blood groups with hepatitis C viremia. Saudi J Biol Sci. 2021;28(9):5359–5363. doi:10.1016/j.sjbs.2021.05.062
31. Sayal SK, Das AL, Nema SK. Study of blood groups in HIV seropositive patients. Indian J Dermatol Venereol Leprol. 1996;62(5):295–297.
32. Siransy LK, Nanga ZY, Zaba FS, et al. ABO/Rh blood groups and risk of HIV infection and hepatitis B among blood donors of Abidjan, Côte D’Ivoire. Eur J Microbiol Immunol. 2015;5(3):205–209. doi:10.1556/1886.2015.00029
33. Mohammadali F, Pourfathollah A. Association of ABO and Rh blood groups to blood-borne infections among blood donors in Tehran-Iran. Iran J Public Health. 2014;43(7):981–989.
34. Alwasaidi TA, Alrasheed SK, Alhazmi RA, et al. Relation between ABO blood groups and obesity in a Saudi Arabian Population. J Taibah Univ Med Sci. 2017;12(5):407–411. doi:10.1016/j.jtumed.2017.05.011
35. Benahadi A, Alami R, Boulahdid S, et al. Distribution of ABO and Rhesus D blood antigens in Morocco. Internet J Biol Anthropol. 2013;6:16.:16.
36. Lialiaris T, Digkas E, Kareli D, et al. Distribution of ABO and Rh blood groups in Greece: an update. Int J Immunogenet. 2011;38:1–5. doi:10.1111/j.1744-313X.2010.00958
37. Castro O. Sickle cell thalassemia, thrombocytosis, and erythrocytosis. South Med J. 1981;74(3):380–381. doi:10.1097/00007611-198103000-00042
38. Allan TM. ABO and Rh blood groups in relation to sex ratio, mean number and mortality of Sibs. Hum Hered. 1977;27(2):108–113. doi:10.1159/000152858
39. Allan TM. ABO blood groups and human sex ratio at birth. J Reprod Fertil. 1975;43(2):209–219. doi:10.1530/jrf.0.0430209
40. Allan TM. ABO and Rh blood groups in relation to sex ratio of Sibs. Hum Hered. 1972;22(5–6):578–583. doi:10.1159/000152541
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
