Back to Journals » Patient Preference and Adherence » Volume 12
Distribution characteristics and factors influencing oral warfarin adherence in patients after heart valve replacement
Authors Wang XW, Xu B, Liang HL, Jiang SY, Tan HM, Wang XR, Wang X, Yu SQ, Liu JC
Received 30 April 2018
Accepted for publication 3 July 2018
Published 3 September 2018 Volume 2018:12 Pages 1641—1648
DOI https://doi.org/10.2147/PPA.S172223
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Xiaowu Wang,1,* Bo Xu,1,* Hongliang Liang,1 Shuyun Jiang,1 Hongmei Tan,1 Xinrong Wang,1 Xia Wang,2 Shiqiang Yu,1 Jincheng Liu1
1Department of Cardiovascular Surgery, Xijing Hospital, Fourth Military Medical University, Xi’an 710032, Shaanxi, People’s Republic of China; 2Department of Health Statistics, Faculty of Preventive Medicine, Fourth Military Medical University, Xi’an 710032, Shaanxi, People’s Republic of China
*These authors contributed equally to this work
Purpose: Oral warfarin anticoagulation is a long-term treatment that is required after heart valve replacement. This treatment can prevent serious complications, such as embolism, thereby increasing patients’ postoperative survival rates and quality of life. Patients treated with artificial mechanical heart valve replacement were followed up over the phone at different times after the procedure, which is an effective method for preventing accidents related to postoperative oral warfarin anticoagulation. Our goal was to determine a method for providing theoretical guidance to patients on oral warfarin anticoagulation following heart valve replacement.
Patients and methods: The participants of this study were patients who received artificial mechanical heart valve replacements and were followed up for 2 years after the procedure. Patient adherence to medical advice was calculated, and the distribution characteristics of adherence to prescribed timing, prescribed dose, and regular clinical follow-up among patients of both sexes and of different ages, regions, and educational levels attained were compared.
Results: Univariate and multifactorial logistic regression analyses were used to evaluate the factors influencing adherence. Our analyses showed that adherence to oral warfarin anticoagulation in patients after heart valve replacement is influenced by sex, age, residential location, and educational attainment. The medication habits of patients can be evaluated accordingly via phone follow-up. As such, dose adjustment recommendations can be provided, significantly increasing the adherence to oral warfarin anticoagulation in patients after heart valve replacement.
Conclusion: Adherence to oral warfarin anticoagulation among patients after heart valve replacement is affected by sex, age, type of residence, and educational level, as well as adherence to clinical follow-up over the phone. The follow-up sessions help establish good doctor–patient communication, which is critical for timely medication guidance, thus shortening medication administration delays and decreasing the overall length of therapy.
Keywords: warfarin, artificial mechanical heart valve replacement, AMHVR, telephone follow-up, adherence, distribution characteristics
Introduction
Oral warfarin anticoagulation is a long-term treatment required for patients who have undergone heart valve replacement. Timely and effective anticoagulation treatments can prevent serious complications such as bleeding and embolism, thereby increasing postoperative survival rates and the quality of life among patients.1,2 OAC is the primary method used for oral anticoagulation therapy, and it has been shown to be effective in preventing and treating various thromboembolic diseases.3–5 It is currently widely applied as anticoagulation therapy for various diseases and is the first option for a long-lasting anticoagulant to prevent thromboembolic events related to valvular heart disease, atrial fibrillation, and coronary heart disease, as well as for the prevention of pulmonary embolism, deep vein thrombosis, and other disorders.6–9 However, warfarin must be taken for a long period of time, and compliance is influenced by many factors, including different individual reactions to therapy (eg, genetics, ethnicity, pathological states, pregnancy) and drug interactions, often rendering its anticoagulation properties ineffective.10–13 Dosages must be regularly monitored and adjusted based on the INR,14 and the optimal warfarin dosage varies among patients and changes dynamically. Thus, implementing planned management methods for patients after a heart valve replacement and enhancing patient self-monitoring are effective methods for preventing postoperative anticoagulation accidents.
Post-discharge follow-up is the primary method for optimizing pharmacological monitoring in the clinical application of warfarin.15,16 Phone or Internet follow-up can significantly increase patient medication compliance with OAC following heart valve replacement.17 Phone follow-up has become the primary method for clinical surveillance because it is convenient, economical, rapid, and easily received. Phone follow-up allows practitioners to emphasize the effects of interactions between warfarin and other medications, the interactions between Western medications and Chinese herbal medications, and the safe use of warfarin, especially among patients after heart valve replacements who must take a multitude of medications for extended periods of time. It has been shown that the correct combinations of drugs and enhanced monitoring of INR values can decrease the risks of clinical treatment.18–20 For some complex chronic diseases, warfarin use in patients after heart valve replacement carries a risk of exacerbating existing disorders. Therefore, regular follow-up with these patients is highly necessary.21–23 Telephone follow-up can be used to dynamically identify patients’ thrombotic potential and bleeding status, closely monitor coagulation indices, adjust medication dosages, strictly implement individualized regimens, ensure treatment efficacy, and reduce the incidence of adverse reactions.24
In this study, we describe the distribution characteristics of OAC adherence among patients after heart valve replacement. Furthermore, we analyzed the relevant factors influencing adherence, thereby providing effective theoretical guidance for phone follow-up of patients on OAC.
Methods
Study population and design
We selected 2,128 patients who underwent AMHVR and completed 2 years of follow-up through our practice between January 2013 and June 2015. We excluded the data of 59 patients for the reasons that 56 (92%) patients were unable to complete 2 years of follow-up due to loss of contact, and another three (8%) were reluctant to accept the prescribed follow-up. All procedures involving human participants were approved by the medical ethics committee of the Xijing Hospital. All methods were performed in accordance with the approved guidelines, and written informed consent was obtained from the patients who participated in follow-up communications. To evaluate compliance with oral anticoagulants among the patients who received AMHVR, we developed a set of medication adherence evaluation criteria that was based on adherence to the prescribed medication timing, the prescribed medication dosage, and compliance with regular clinical follow-ups. At a given follow-up time point, compliance was judged to be good if the patient adhered to two or three types of the aforementioned medication adherence criteria. Patients who adhered to the two or three types of criteria at three or more of the five follow-up time points were judged as having good adherence. Patients who did not meet the above conditions were judged having poor adherence.
Upon discharge, patients who received AMHVR were given conventional discharge guidance and were required to take warfarin following their doctors’ orders. The doctors’ orders comprised instructions to: 1) adhere to the prescribed medication timing and take warfarin at about 8:00 pm; 2) adhere to the prescribed medication dosage and adjust the dosage according to INR; and 3) attend regular clinical follow-ups once a week during the first month after surgery, once a month during the next 5 months, and once every two or three months after that. If bruising of the skin, bleeding gums, dizziness, or blurred vision occurred, an immediate clinical follow-up was necessary. Phone follow-up, data collection, and immediate online input were conducted at 1 month, 3 months, 6 months, 1 year, and 2 years after the patients were discharged following AMHVR. Follow-up data included warfarin usage, INR, and PT. Patient information collected included name, age, educational level attained (intermediate school or higher vs elementary school or lower), type of residence (urban or rural), and other baseline data, including past medical history (presence of concomitant disorders requiring frequent medication, eg, diabetes, hypertension), type of valve replacement surgery, model number and replacement valve specifications, and other clinical data. Because follow-up work involves a significant amount of time, the task of following up with the participating postoperative patients over the phone was divided among the researchers. The researchers participating in the follow-up work had ample specialized theoretical knowledge and possessed the ability to communicate patiently and in detail. The phone follow-up sought to understand patient adherence to the prescribed medication timing, the prescribed medication dosage, and clinical follow-up of the INRs and PTs. The warfarin dosage was then adjusted on the basis of the values of the PT and INR. The importance of OAC and the possibility of serious complications developing as a result of inappropriate warfarin dosing were emphasized. Any questions that patients had regarding warfarin use were answered fully. Individualized regimens were strictly implemented. In the event that a patient had a special or difficult question, a senior physician or professor was consulted before providing an answer.
Statistical analysis
SPSS 11.0 software (Windows version 11; SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. Numerical data was described using composition ratios, and the chi-squared test was used for comparison between the groups. Logistic regression analysis was used for the multifactorial analysis. P≤0.05 was considered statistically significant.
Results
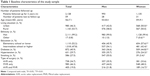
Construction of a health follow-up profile for a patient after heart valve replacement
The age, sex, ethnicities, types of residence, educational levels attained, diabetes and hypertension status, smoking status, and types of heart valve replacement of the participating patients were recorded (Table 1). There were significant gender-related differences between the patients living in urban residences, of specific ethnic backgrounds, with a prevalence of diabetes and hypertension, with specific smoking status, and after specific types of surgery.
  | Table 1 Baseline characteristics of the study sample |
Distribution characteristics of oral warfarin adherence in patients 2 years after AMHVR
Adherence rate
Patients after AMHVR were categorized on the basis of their adherence to medical advice during oral warfarin treatment. This was used as a basis for comparing the adherence to medical advice at the 2-year follow-up point among patients of both sexes, and different ages, types of residence, educational attainment levels, and other characteristics. The data showed that 86.8% of patients successfully adhered to all three types of medical advice and 7.5% of patients adhered to two types of medical advice. Adherence to prescribed timing and regular clinical follow-up were shown in the 7.5% of patients adhering to two types of medical advice; however, dosage could not be accurately adjusted on the basis of the INR values. In addition, 5.7% of patients adhered to only one type of medical advice, adhered to prescribed timing, and had no regular clinical follow-ups or dosage adjustments based on INR values (Table 2).
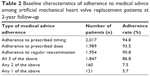  | Table 2 Baseline characteristics of adherence to medical advice among artificial mechanical heart valve replacement patients at 2-year follow-up |
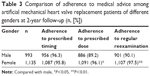
Distribution by gender
There was no significant difference in the rate of adherence to prescribed timing between male and female patients after AMHVR, but the rate of adherence to prescribed dosages and regular clinical follow-ups was significantly higher in women than in men (all P<0.05; Table 3).
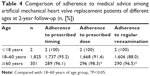
Distribution by age
The medication adherence behavior of patients aged 18 years or less after AMHVR reached 100%. This group adhered to prescribed timing and regular clinical follow-up, and the dosage was adjusted on the basis of thrombin monitoring indices. There was no significant difference in the rate of adherence to the prescribed timing between the age≥60 and age 18–60 groups; however, the rates of adherence to prescribed dosages and regular clinical follow-ups were significantly lower in the age≥60 group compared to the age 18–60 group (P<0.05; Table 4).
Distribution by educational attainment
There was no significant difference in the rate of adherence to prescribed timing of the medication among patients of different educational levels, but the rate of adherence to the prescribed dosage and regular clinical follow-up was significantly higher in patients with higher educational attainment (P<0.05, P<0.01; Table 5).
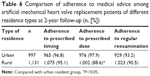
Distribution by type of residence
The rate of adherence to prescribed timing was significantly higher in urban residents than in rural residents (P<0.05), but there was no significant difference in the rate of adherence to the prescribed dosage or regular clinical follow-ups between urban and rural residents (Table 6).
Analysis of factors influencing oral warfarin adherence in patients at 2 years after AMHVR
Chi-squared testing was used for the univariate analysis. The results showed that there were significant differences in gender, age, type of residence, and other influential factors between the good adherence and poor adherence groups (P<0.01). Educational attainment also differed between the two groups (P<0.01). There was no significant difference in ethnicity, smoking status, or valve replacement type between the two groups (Table 7).
Multifactorial analysis
A multifactorial logistic regression model was used for the multifactorial analysis. The independent variable had a binary variable value and was represented by one or 0. The dependent variable was whether medical advice was followed, and the independent variables were the factors from the univariate analysis that were statistically significant (Table 8). After substitution in the regression equation and elimination of confounding factors, the results showed that sex, age, type of residence, and educational attainment were independent factors influencing adherence (Table 9).
  | Table 8 Variable coding |
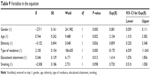  | Table 9 Variables in the equation |
Discussion
On the basis of previous studies, we analyzed the factors influencing oral warfarin adherence in patients after heart valve replacement who completed 2 years of follow-up. Our results showed that gender, age, place of residence, and educational level attained were the independent factors affecting oral warfarin adherence. This indicates that we can provide personalized counseling for different groups of patients in future follow-up and also provide comprehensive theoretical guidance for prescribing oral warfarin after valve replacement. Adherence to medication advice among women was significantly greater than in men. This is because of the manner in which men and women manage such issues and may be related to the way in which the question was asked. In addition, this finding was also related to a large extent to the societal roles and lifestyle habits of patients of different genders. After recovery from surgery, most younger male patients reenter the workforce, and work stress trivializes the awareness of self-care to different degrees. This leads to insufficient emphasis on regular clinical follow-up of the hematological indices and warfarin use, which results in lower medication adherence in men than in women. Because warfarin anticoagulation acts by interfering with the recycling of vitamin K in the liver,24 long-term alcohol and tobacco use can affect metabolic activity in the liver, thereby significantly lowering the effectiveness of warfarin anticoagulation and causing relatively large fluctuations in coagulation among some male patients. Therefore, the effects of tobacco and alcohol use on warfarin are emphasized to patients who smoke and/or drink and are also emphasized to their family members during follow-up. They are recommended to quit smoking or drinking or reduce tobacco and alcohol consumption and facilitate the stabilization of thrombin-related indices, thereby reducing fluctuations in warfarin dosage. The maintenance dose of warfarin within the acceptable range of coagulation indices is significantly lower in female patients compared to male patients due to the effects of estrogen.8,24 During follow-up, approximately 10% of female patients stated that warfarin use led to significantly increased menstrual flow and extension of the menstrual period by 2–3 days. Our general recommendation is that the warfarin dosage can be appropriately reduced during the menstrual period, which reduces patient anxiety and also alleviates clinical symptoms to some extent by reducing physical discomfort. Oral contraceptives affect INR, and we will focus on the effect of oral contraceptives on INR in women of childbearing age during future follow-ups.
Adherence to medical advice in patients aged 18 years or below was 100%. These patients adhered to prescribed timing and regular clinical follow-up and had their dosage adjusted dynamically based on the thrombin monitoring indices. This was primarily due to the patient’s parents or guardians strongly emphasizing medical advice adherence. This phenomenon further demonstrated that the degree of emphasis by patients and their family members could significantly affect adherence to medical advice. Among on-campus university students and young people who did not grow up with their parents, adherence to medical advice was affected by excessive academic pressure and work pace. Approximately 12% of patients missed doses or did not undergo regular clinical follow-ups. Adherence to medical advice was relatively high among married, middle-aged patients, reaching 95% and above. Further, the degree of awareness of medication and the ability to implement it was highest in this age group. Reminders and monitoring by spouses significantly increased medication adherence. However, this age group also included individual patients of the other extreme, that is, who rejected medication-related information provided to them and were resistant to phone follow-up. These patients were generally not easily convinced, and follow-up personnel could only indirectly understand the situation through the patient’s family members.
Warfarin use among elderly patients is steadily increasing, especially to prevent stroke in chronic atrial fibrillation. Although warfarin is most beneficial to elderly patients, it carries the highest risk of adverse outcomes and difficulties in anticoagulation therapy.25 Adherence to medical advice among elderly patients aged 60 years and above is determined by the level of attention given by the patient and also to a large extent by the attention given by the spouse and children of the patient. Especially among elderly patients with limited mobility issues, low educational attainment, and remote residence, medication adherence is generally completely determined by the awareness and attitudes of the patient’s children. Thus, direct communication with the patient’s children by phone follow-up not only allows more frequent, comprehensive information to be obtained, but also permits better solutions to medication-related problems and ensures the responsibility of the children during the interaction.
In medication follow-up actions, there were significantly lower numbers of rural patients than urban patients who took their medications on time. That is primarily because many county-level hospitals can measure coagulation-related indices and also because primary care physicians specializing in cardiovascular-related specialties have undergone training in recent years to solve certain medication-related problems faced by rural patients at local hospitals. Phone follow-up and consultation can allow for immediate and dynamic medication-related guidance among patients for whom local physicians may not be available to provide medication-related guidance. Thus, phone follow-up can increase medication adherence among patients to a large degree, especially among patients living in rural areas. However, approximately 1.4% of those patients did not adhere to the prescribed timing of clinical follow-up of hematological indices and therefore did not have their dosages adjusted. This could be because of the patient or their family members giving insufficient attention to medical advice because of remote residence, low educational attainment, or other factors. Through routine follow-up reminders in which the importance of regular blood work and dynamic dosing is explained, the medication adherence of patients can be improved.
The degree of understanding of individualized warfarin regimens increases with increasing educational level attained among patients after AMHVR; these patients have greater subjective initiative when medication-related questions arise. Among this type of patient and their family members, some may ask about the effects of their other medications on warfarin’s activity or stability. Our follow-up personnel explained the interactions between warfarin and piperacillin sodium, sulbactam sodium, azithromycin, and atorvastatin with respect to changing INR values.26 The strength of anticoagulation therapy following heart valve replacement is related to the incidence of complications.24 After AVR, the target INR for an aortic valve is 2–3 and for a mitral or dual prosthetic valve it is 2.5–3.5.27 Thus, relevant points of emphasis are also different for patients and family members at different educational levels.
Telephone follow-up is a practical and effective method for clinical postoperative follow-up, as it not only fulfills the health needs of patients, but also improves patients’ self-awareness regarding adherence to medical advice and increases medication adherence in patients.28 Regular postoperative follow-up of patients after heart valve replacement by phone assesses warfarin adherence, immediately identifies incorrect understandings, increases patient awareness and implementation of adherence to medical advice, and increases patient adherence to warfarin anticoagulation. Phone follow-ups can allow the medical provider to impart relevant medical knowledge and alleviate patient worries, thereby eliminating the fear and anxiety that some clinical symptoms cause in patients.29,30 Providing phone follow-up for oral warfarin anticoagulation that is targeted to individual patients after heart valve replacement can establish communication channels between the patient, the primary care physician, and the clinical specialist and improve oral warfarin adherence in patients.
We are improving the follow-up system gradually, and now, we connect patients via E-mail and Wechat in addition to telephone. During follow-up, we collect relevant information; provide consulting services; give individualized, rational guidance on warfarin usages based on each unique patient’s situation; and improve compliance among patients who do not take their warfarin as prescribed by the doctor.
This study exposed some limitations to warfarin use, which should be considered for future follow-up: 1) oral warfarin can prevent complications such as embolism in patients after heart valve surgery, but at the same time, it can increase arterial stiffness;31 2) to monitor oral warfarin dosing more effectively, follow-up INR should be obtained monthly at minimum; and 3) estrogen use decreases the warfarin effect, so more attention should be paid to the effect of oral contraceptives on INR in younger women during menses.
Conclusion
In summary, adherence to oral warfarin anticoagulation among patients after heart valve replacement is affected by gender, age, type of residence, and educational attainment level, as well as adherence to clinical follow-up, which is determined through appropriate follow-up over the phone.
On the one hand, personalized phone follow-up can significantly increase adherence to oral warfarin anticoagulation, further providing patients with the following benefits: scientifically rational guidance for warfarin use, reinforced efficacy of surgical treatment, reduced incidence of postoperative complications, and improved postoperative quality of life. On the other hand, these follow-ups help to establish good doctor–patient communication, which is critical for timely medication guidance, thus shortening medication administration delays and decreasing the overall length of therapy.
Abbreviations
AMHVR, artificial mechanical heart valve replacement; AVR, aortic valve replacement; INR, International Normalized Ratio; MVR, mitral valve replacement; OAC, oral anticoagulation; PT, prothrombin time.
Acknowledgment
This study was supported by the Natural Science Foundation of China: No 81570330 (JC Liu) and No 81470500 (HL Liang).
Disclosure
The authors report no conflicts of interest in this work.
References
Tiede DJ, Nishimura RA, Gastineau DA, et al. Modern management of prosthetic valve anticoagulation. Mayo Clin Proc. 1998;73(7):665–680. | ||
Eikelboom JW, Wallentin L, Connolly SJ, et al. Risk of bleeding with 2 doses of dabigatran compared with warfarin in older and younger patients with atrial fibrillation: an analysis of the randomized evaluation of long-term anticoagulant therapy (RE-LY) trial. Circulation. 2011;123(21):2363–2372. | ||
Tran A, Cheng-Lai A. Dabigatran etexilate: the first oral anticoagulant available in the United States since warfarin. Cardiol Rev. 2011;19(3):154–161. | ||
Liew A, Douketis J. Initial and long-term treatment of deep venous thrombosis: recent clinical trials and their impact on patient management. Expert Opin Pharmacother. 2013;14(4):385–396. | ||
Arendt CJ, Hong JH, Daly RC, et al. Time to achieving therapeutic international normalized ratio increases hospital length of stay after heart valve replacement surgery. Am Heart J. 2017;187:70–77. | ||
Akhtar RP, Abid AR, Zafar H, Khan JS. Aniticoagulation in patients following prosthetic heart valve replacement. Ann Thorac Cardiovasc Surg. 2009;15(1):10–17. | ||
Dzeshka MS, Lip GY. Warfarin versus dabigatran etexilate: an assessment of efficacy and safety in patients with atrial fibrillation. Expert Opin Drug Saf. 2015;14(1):45–62. | ||
Wu L, Chang Q, Wang T, Zhang Z, Lou Y. Clinical observation of postoperative warfarin anticoagulation in 300 patients undergoing mitral valve replacement with a carbomedics mechanical valve. Heart Surg Forum. 2015;18(2):63–66. | ||
Liedtke MD, Rathbun RC. Drug interactions with antiretrovirals and warfarin. Expert Opin Drug Saf. 2010;9(2):215–223. | ||
Kucera T, Maly R, Urban K, Sponer P. Venous Thromboembolism Prophylaxis after Total Hip Arthroplasty. Acta Chir Orthop Traumatol Cechoslov. 2011;78:101–105. | ||
Leite PM, Martins MAP, Castilho RO. Review on mechanisms and interactions in concomitant use of herbs and warfarin therapy. Biomed Pharmacother. 2016;83:14–21. | ||
Yinon Y, Siu SC, Warshafsky C, et al. Use of low molecular weight heparin in pregnant women with mechanical heart valves. Am J Cardiol. 2009;104(9):1259–1263. | ||
Nadkarni A, Oldham M, Howard M, Lazar HL, Berenbaum I. Detrimental effects of divalproex on warfarin therapy following mechanical valve replacement. J Card Surg. 2011;26(5):492–494. | ||
Wen MS, Lee MT. Warfarin Pharmacogenetics: New Life for an Old Drug. Acta Cardiol Sin. 2013;29(3):235–242. | ||
Craig JA, Chaplin S, Jenks M. Warfarin monitoring economic evaluation of point of care self-monitoring compared to clinic settings. J Med Econ. 2014;17(3):184–190. | ||
Fritzsche D, Schenk S, Eitz T, et al. Patient self-monitoring of prosthetic heart valve function. J Heart Valve Dis. 2007;16(5):558–566. | ||
Aucar JA, Doarn CR, Sargsyan A, et al. Use of the Internet for long-term clinical follow-up. Telemed J. 1998;4(4):371–374. | ||
Shalansky S, Lynd L, Richardson K, Ingaszewski A, Kerr C. Risk of warfarin-related bleeding events and supratherapeutic international normalized ratios associated with complementary and alternative medicine: a longitudinal analysis. Pharmacotherapy. 2007;27(9):1237–1247. | ||
Nutescu EA, Shapiro NL, Ibrahim S, West P. Warfarin and its interactions with foods, herbs and other dietary supplements. Expert Opin Drug Saf. 2006;5(3):433–451. | ||
Wong RS, Cheng G, Chan TY. Use of herbal medicines by patients receiving warfarin. Drug Saf. 2003;26(8):585–588. | ||
Fanola CL, Mooney D, Cowan AJ, et al. Incidence of severe renal dysfunction among individuals taking warfarin and implications for non-vitamin K oral anticoagulants. Am Heart J. 2017;184:150–155. | ||
Ihaddadene R, Carrier M. The use of anticoagulants for the treatment and prevention of venous thromboembolism in obese patients: implications for safety. Expert Opin Drug Saf. 2016;15(1):65–74. | ||
Chuai JB, Shi L, Ma XY, et al. Curative effect of mechanical heart valve replacement and anticoagulant therapy after surgery. J Biol Regul Homeost Agents. 2016;30(1):141–146. | ||
Zivelin A, Rao LV, Rapaport SI. Mechanism of the anticoagulant effect of warfarin as evaluated in rabbits by selective depression of individual procoagulant vitamin K-dependent clotting factors. J Clin Invest. 1993;92(5):2131–2140. | ||
Bereznicki LR, Peterson GM, Jackson SL, Jeffrey EC. The risks of warfarin use in the elderly. Expert Opin Drug Saf. 2006;5(3):417–431. | ||
Clark NP, Delate T, Riggs CS, et al. Warfarin interactions with antibiotics in the ambulatory care setting. JAMA Intern Med. 2014;174(3):409–416. | ||
Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC Focused Update of the 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017;135(25):e1159–e1195. | ||
Lanas-Gimeno A, Lanas A. Risk of gastrointestinal bleeding during anticoagulant treatment. Expert Opin Drug Saf. 2017;16(6):673–685. | ||
Cruess DG, Localio AR, Platt AB, et al. Patient attitudinal and behavioral factors associated with warfarin non-adherence at outpatient anticoagulation clinics. Int J Behav Med. 2010;17(1):33–42. | ||
El-Gatit AM, El-Gatit AS, Haw M. Relationship between depression and non-adherence to anticoagulant therapy after valve replacement. East Mediterr Health J. 2003;9(1–2):12–19. | ||
Mozos I, Stoian D, Luca CT. Crosstalk between Vitamins A, B12, D, K, C, and E Status and Arterial Stiffness. Dis Markers. 2017;2017: 8784971. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.