Back to Journals » Patient Preference and Adherence » Volume 9
Dispensing of non-prescribed antibiotics in Jordan
Authors Almaaytah A, Mukattash T , Hajaj J
Received 2 July 2015
Accepted for publication 19 August 2015
Published 30 September 2015 Volume 2015:9 Pages 1389—1395
DOI https://doi.org/10.2147/PPA.S91649
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Ammar Almaaytah,1 Tareq L Mukattash,2 Julia Hajaj2
1Department of Pharmaceutical Technology, 2Department of Clinical Pharmacy, Faculty of Pharmacy, Jordan University of Science and Technology, Irbid, Jordan
Objective: Current regulations in Jordan state that antibiotics cannot be sold without a medical prescription. This study aimed to assess the percentage of pharmacies that dispense antibiotics without a medical prescription in the Kingdom of Jordan and identify and highlight the extent and seriousness of such practices among Jordanian pharmacies.
Methods: A prospective study was performed, and five different clinical scenarios were simulated at pharmacies investigated including sore throat, otitis media, acute sinusitis, diarrhea, and urinary tract infection in childbearing-aged women. Three levels of demand were used to convince the pharmacists to sell an antibiotic.
Results: A total of 202 total pharmacies in Jordan were visited in the present study. The majority of pharmacies (74.3%) dispensed antibiotics without prescription with three different levels of demand. The percentage of pharmacies dispensing antibiotics without a prescription for the sore throat scenario was 97.6%, followed by urinary tract infection (83.3%), diarrhea (83%), and otitis media (68.4%). The lowest percentage of antibiotic dispensing was for the acute sinusitis simulation at 48.5%. Among the pharmacies that dispensed antibiotics, the pharmacists provided an explanation as the number of times per day the drug should be taken in 95.3% of the cases, explained the duration of treatment in 25.7%, and inquired about allergies prior to the sale of the antibiotic in only 17.3%. Only 52 pharmacies (25.7%) refused to dispense any kind of antibiotics, the majority (61.5%) of this refusal response came from acute sinusitis cases, while the minority (2.4%) came from the sore throat cases.
Conclusion: The results of this study demonstrate that antibiotics continue to be dispensed without prescription in Jordan in violation with national regulations regarding this practice. The findings of this study could provide a layout for governmental health authorities to implement strict enfrorcment of national regulations regarding antibiotic dispensing in order to avoid the serious complications that could arise in the future as a result of such practices.
Keywords: pharmacy, pharmacy practice, non-prescribed antibiotics, microbial resistance, Jordan
Introduction
The discovery of antibiotics is considered as one of the greatest medical achievements of the 20th century.1 Antibiotics had a tremendous impact on improving the life quality of humans as fatal bacterial diseases became treatable and even preventable.
Currently, there is a progressive shrinkage in the range of antimicrobial agents effective against common human pathogens due to the impact of the global health problem of increased antimicrobial resistance, a problem that is mainly attributed to the widespread overuse and systemic misuse of those potent and relatively safe agents that are prescribed by physicians worldwide.2–4 Antibiotics are considered among the most commonly prescribed drugs worldwide with the majority of these prescriptions are being sold and prescribed outside the hospital setting and specifically by community pharmacies.5,6 Antibiotic resistance has been directly linked to high levels of antibiotic consumption within the community.7,8 Additionally, self-medication with antibiotics, a practice performed by individual patients with the intent to treat their infections and relive their clinical symptoms regardless of the causing pathogen, has led to an increased consumption of antibiotics which has contributed significantly to the major global problem of antimicrobial resistance, adverse drug reactions, and higher treatment costs.9,10
Self-medication with antibiotics remains a major global problem as this practice has been reported in several developed countries with high percentages including the European Union.11 Additionally, it has been well documented in several studies that high antibiotic consumption and misuse is closely related to the emergence of resistant bacterial strains.12
In Jordan, self-medication with antibiotics reaches a high percentage of 39.5% within the population.13 Moreover, the main sources of antibiotics intended for self-medication are community pharmacies and medication leftovers from previous prescriptions.13 This reveals that dispensing antibiotics without an official prescription and the lack of awareness regarding the misuse of antibiotics is the main reason behind the uncontrolled practice of self-medication and consequently antibiotic resistance within the Jordanian community. Additionally, several antibiotics dispensed by pharmacists or requested by patients for the purpose of self-medication are intended to treat clinical symptoms that often occur as a result of viral rather than bacterial infections which also contribute heavily to the issue of resistance.14
Due to this global dilemma, several strategies have been investigated to define certain protocols and regulations that could reduce the problem of resistance and these include defining guidelines regarding treatment, public education, marketing policies, and emerging basic regulations restricting antibiotic use.6 The latter strategy has been proven to cause a sharp decrease in antibiotic consumption and when implemented effectively played a significant role in reversing and hampering the rate of emergence of certain resistant microorganisms.15
In many countries, there is a specific regulation/law that prohibits the dispensing of antibiotics without medical prescription.14–18 Here in Jordan, this regulation/law is still inactive, and the practice of self-medication reaches a significant percentage when compared to the overall population while resistance is escalating.13,19–21 All of these factors indicate the need of a quick pronounced action and regulatory policies in order to constrain and retard the health threat of antimicrobial resistance.
In this study, we aim to assess the percentage of pharmacies that dispense antibiotics without a medical prescription in the Kingdom of Jordan. We also aim to highlight the seriousness of such problems which hopefully would alert the main health regulatory bodies in the country to implement more rigorous regulations regarding nonprescription antibiotic dispensing, this study will also assess the knowledge of pharmacists in differentiating between the clinical symptoms of viral causes of infections rather than bacterial ones and the percentage of antibiotics that are prescribed for the treatment of viral infections mistakenly, other issues regarding the safety of dispensing antibiotics to certain patient groups (pregnancy) will also be taken into account.
Methodology
Pharmacies
An official list of legal operating pharmacies in the Hashemite Kingdom of Jordan was obtained from the Jordanian Pharmacists Association with a total of 2,045 officially operating pharmacies, from which a randomized sample of 225 pharmacies was chosen using random tables (http://allen.netcom.co.uk/Sampling.htm). In brief, 152 of those pharmacies were in Amman; the capital, and 50 others were in Irbid; the main northern city. The study was conducted in the two main urban cities in Jordan with the highest population as both cities combined account for 71% of the total seven million inhabitants living in Jordan.
Pharmacists were the attendants in 182 (90.1%) of those pharmacies, while pharmacist assistants were in 20 (9.9%) of them. Of this group, 108 (53.5%) were males and 94 (46.5%) were females. The majority (109 [54%]) of the pharmacy staff were in the age ranging between 30 and 50 years.
Each pharmacy was visited once by one of the principal investigators who pretended of having a relative with a complaint predetermined with a specific clinical case scenario with definite information according to simulated-client method pharmacy surveys.22 Any other information was provided only if the pharmacist asked for it and was considered as additional information.
Clinical scenarios
Five different clinical scenarios were chosen: sore throat, acute sinusitis, otitis media, diarrhea, and urinary tract infection (UTI) without complications in childbearing-aged women. The sore throat scenario: a 20-year-old female relative experiencing sore throat with slight fever and headache for 24 hours. The acute sinusitis scenario: a 50-year-old female relative experiencing nasal congestion and facial pain for 24 hours. The otitis media scenario: a 55-year-old male relative experiencing a sharp ear pain with no discharge. The diarrhea scenario: a 20-year-old healthy female relative experiencing a loose bowel motion accompanied by diarrhea with slight fever for 24 hours. The UTI scenario: a 27-year-old female relative experiencing a burning sensation upon urination for 3 consecutive days, where the patient is also pregnant.
Levels of demand
In an attempt to obtain an antibiotic, the investigator pursued three levels of demand starting with asking for something to alleviate the symptoms, then asking for a stronger medication and finally a clear request for an antibiotic was made in the case of not achieving the previous two levels of demand. Immediately after leaving the pharmacy, a note form (Supplementary materials) with predetermined questions and aspects was filled by the same investigator. The note form was divided into three parts; the first part included general information about the pharmacy and the attending pharmacist or pharmacy assistant, name of the pharmacy, its location, the sex of the pharmacist, and the predicted age group (<30, 30–50, >50 years) of the attending pharmacist. The second part included the number of the allocated clinical scenario and the response of the pharmacist either by agreeing or by refusing to dispense an antibiotic. The third part of the note form included specific aspects of the dialogue that were predicted to occur between the pharmacist and the customer (the investigator) regarding the clinical case.
This part was further divided into two sections, where the dialogue can be redirected by the pharmacist and eventually lead to two general outcomes according to the response. If the pharmacist dispensed an antibiotic, the investigator recorded the level of demand at which the antibiotic was dispensed (one, two, or three), the type of antibiotic, and whether the pharmacist explained how to take it, specified the duration of treatment, asked about any drug allergies, other symptoms, concomitant use of other drugs or the pregnancy status of the female patient, and if there was a recommendation to consult a physician. The second outcome that was predicted was if the pharmacist refused to dispense an antibiotic, in this case, the investigator recorded the reason of dispensing refusal (administrative issues, health issues, or both), type of dispensed medication instead of antibiotic if that occurred, and if there was a recommendation to consult a physician.
The investigators
This study included three principal investigators, several rehearsal sessions were conducted to standardize the information provided to the pharmacists. The principal investigators rehearsed each clinical scenario with the aid of a senior clinical pharmacist, in order to convince the pharmacist that the clinical situation presented by the investigator is real and obtain standardization of the simulated clinical scenarios. The investigators visited a number of pharmacies that were not included in the study group, only to experience the event and be more flexible with the real study group.
Ethical approval
The study was approved by the Institutional Review Board (IRB) at Jordan University of Science and Technology (JUST). The research protocol was also approved by the Jordanian Pharmacists Association. Deception and incomplete disclosure to study subjects (pharmacists) were considered ethically acceptable, because this was a minimal risk study and it could not have been performed with complete disclosure of the investigator’s real entity. Data were kept anonymous.
Data collection
Following data collection, responses were coded and entered into a customized database (SPSS version 17). Data are represented as the percentage of pharmacists’ response to each simulated clinical scenario included in this study.
Results
Percentage of dispensing
In all, 252 pharmacies were visited from all different regions of Amman and Irbid in Jordan, of those 152 (75.2%) pharmacies were in Amman, and 50 (24.7%) were in Irbid. Clinical scenarios were equally distributed to the different pharmacies included in this study.
In brief, 150 (74.3%) pharmacies out of the total 202 dispensed antibiotics without prescription with three different levels of demand. The highest percentage of antibiotic dispensing was associated with the sore throat simulation. The percentage of pharmacies dispensing antibiotics without a prescription for the sore throat scenario was 97.6% in Amman and Irbid, followed by UTI (83.3%), diarrhea (83%), otitis media (68.4%), while the lowest percentage of antibiotic sales was for the acute sinusitis simulation was 48.5%. The distribution of the percentage of pharmacies that dispense antibiotics without prescription with different levels of demand for the simulated scenarios is summarized in Table 1. The majority of antibiotics dispensed without a prescription (121 [59.9%]) was associated with level one of demand; this was followed by level three of demand (25 [12.4%]), and finally level two of demand (4 [2%]). This was the case for four of the presented clinical scenarios except for acute sinusitis, where the majority of its dispensing was associated with level three of demand (20.5%), followed by level two (10.3%) then level one (7.7%).
Most pharmacists explained to the principal investigators how to take the antibiotic (143 [95.3%]) of the total pharmacies visited), the duration of treatment was specified by only a small group within the sample (25 [16.7%]), and in some cases, the duration of treatment was never explained to the investigator as in the cases of acute sinusitis and otitis media. The results were relatively similar for other aspects addressed in the study such as drug allergy (26 [17.3%]), the concomitant use of other drugs (8 [5.3%]), and recommending consultation by a physician (6 [4%]).
Penicillins and a combination of penicillin/penicillinase inhibitors were the most commonly dispensed antibiotics in cases of the sore throat scenario, while three classes such as penicillins, fluoroquinolones, and macrolides of antibiotics were dispensed for most cases of acute sinusitis with equal percentages. For otitis media, chloramphenicol was the most commonly prescribed antibiotic in that simulated scenario while fluoroquinolones and antiprotozoals were commonly given for UTI and diarrhea cases, respectively. Only one pharmacist asked about the pregnancy status of the patient when presented with a UTI simulated case, and refused to dispense any kind of medicine, while insisting for immediate physician consultation. Table 2 summarizes the main interview aspects and the percentage of dispensed antibiotics across the different case scenarios.
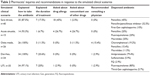  | Table 2 Pharmacists’ inquiries and recommendations in response to the simulated clinical scenarios |
Antibiotic dispensing refusal
Only 52 pharmacies (25.7%) refused to dispense any kind of antibiotics, the majority (61.5%) of this refusal response came from acute sinusitis cases, while the minority (2.4%) came from the sore throat cases. The main reason offered by pharmacists for the refusal of antibiotic dispensing was related to the concern of pharmacists regarding the health issues experienced by the patients (100%) and the possibility of resistance emergence, while administrative issues were not considered in any case.
Recommendation of consulting a physician differed among clinical scenarios; for the sore throat scenario, none of the pharmacists who refused to dispense antibiotics recommended consulting a physician. While the majority of UTI cases (85.7%) and otitis media (75%) in the refusal group recommended consulting a physician. Detailed percentages are shown in Table 3.
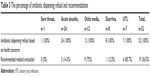  | Table 3 The percentage of antibiotic dispensing refusal and recommendations |
All the pharmacists refusing to dispense antibiotics in the sore throat study group in Amman city (100%) dispensed an anesthetic and a combined therapy product consisting of an analgesic and an antihistamine instead of antibiotics, the majority of pharmacists in the acute sinusitis scenario dispensed (41.7%) decongestants, while anesthetics were dispensed in most cases of otitis media for the refusal group (25%). In the case of diarrhea, the majority of pharmacists dispensed a combination of an antidiarrheal and an anti-spasmodic agent. Finally, 20% of the UTI cases that were refused antibiotics were instead recommended both an analgesic in combination with nutritional advices such as drinking more fluids and juices.
Discussion
The results of our study clearly demonstrate that antibiotics could be easily acquired and sold in Jordan without the need to supply a medical prescription to the pharmacist. Unnecessary and improper dispensing of antibiotics was practiced in 74.3% of the pharmacies included in this study with the different clinical scenarios simulated. Additionally, most clinical scenarios simulated in this study with the exception of UTI and otitis media represent medical conditions that are mainly caused by viral rather than bacterial pathogens. Fluoroquinolones were the most common antibiotics dispensed for UTI in childbearing-aged women without proper assessment of the patient’s pregnancy status highlighting the seriousness of such a practice as fluoroquinolones are classified as category C medications and are contraindicated in pregnancy as they could subject the fetus to serious congenital abnormalities.23 Furthermore, the enquiry of concomitant use of other drugs or other drug allergies that would minimize the risk of side/adverse effects were practiced by a very small group of pharmacists (5.3% and 17.3%, respectively), and only 16.7% of pharmacists provided the patient with the appropriate duration of antibiotic treatment.
A recommendation offered by pharmacists to consult a physician was not frequently advised. Only 4% of the pharmacists in the study group did recommend that, while most of the pharmacists in the study group (95.3%) explained to the patient how to take the dispensed antibiotic. Additionally, the majority of pharmacists (61.3%) inquired about other symptoms to confirm or further investigate the case. These results are in agreement with previous studies conducted in Jordan regarding antibiotic misuse and emerging bacterial resistance.24 In one study, pharmacy customers who were seeking antibiotics were randomly interviewed by the investigators in order to assess the ease of acquiring non-prescribed antibiotics within the Jordanian population, the study demonstrated that non-prescribed antibiotics were acquired by patients and dispensed by pharmacists without any prescription in approximately one-half (46%) of the studied pharmacies due to either recommendation by the pharmacist (23.1%) or as a result of a self-medication practice individually performed by the patient (23.2%). The extent of self-medication with antibiotics within the Jordanian population was also estimated by another study that concluded that the prevalence of self-medication with antibiotics was alarmingly high as 39.5% had used antibiotics without a prescription within a 1-month study period.13 Globally, there has been a clear link between antibiotic overuse and misuse and the emergence of bacterial resistance.12 In Jordan, bacterial resistance against antibiotics has been reported with most different classes of antibiotics including penicillins, cephalosporins, monobactams, tetracyclines, aminoglycosides, fluoroquinolones, and sulfonamides.20,21
The problem of bacterial resistance has stimulated governmental and health regulatory bodies to implement strict legal limitations on antibiotic dispensing within community and hospital pharmacies worldwide.17,24 A law prohibiting the sale and dispensing of non-prescribed antibiotics exists in Jordan without being enforced by the regulatory bodies. This reveals the lack of national guidelines controlling the inappropriate use and dispensing of antibiotics that is closely related to the emergence of antibiotic resistance.12 The Jordanian situation is similar to many other developing countries as dispensing antibiotics without prescription is considered illegal but the lack of regulatory enforcment and governmental neglegence stimulates this practice in these different countries.4,16–18,24–26 Several factors could be responsible for the dispensing and sale of non-prescribed antibiotics in Jordan, in addition to the lack of enforcment of national regulations, the financial interest of community pharmacists along with suboptimal levels professionality and non-abidment to the code of ethics could be the main reasons behind the significant number of pharmacists adopting this practice. Furthermore, this practice could also be attributed to the high demand of antibiotics by the Jordanian population as self-medication with antibiotics according to recent studies in this field is significantly high. All these factors should urge the governmental and nongovernmental local health organizations to pursue the devolpment of several programs with the aim of increasing the awareness of pharmacists and the local population regarding this issue through providing up-to-date training courses offered to pharmacists and local civil societies highlighting the seriousness of this practice on the overall population in general.
Conclusion
The results of this study demonstrate that antibiotics are dispensed without prescription in Jordan with relative ease and in violation with national regulations regarding this practice. The findings of this study could provide a layout for governmental health authorities to implement strict enfrorcment of national regulations regarding dispensing of non-prescribed antibiotics in order to avoid the serious complications that could arise in the future as a result of such unregulated practices. Adittionally, local nongovernmental organizations working in the field of medical public awarness should put more emphasis on this isssue in their national policies and programs across the country. Future national policies should address this problem and its serious impact on the overall health of its its citizines with the aim of fulfilling the health intersts of the future generations of Jordanian citizens.
Acknowledgment
The present research was funded by the deanship of Research at the Jordan University of Science and Technology.
Disclosure
The authors report no conflicts of interest in this work.
References
Chopra I. The 2012 Garrod Lecture: discovery of antibacterial drugs in the 21st century. J Antimicrob Chemother. 2012;68(3):496–505. | ||
Rolain JM, Canton R, Cornaglia G. Emergence of antibiotic resistance: need for a new paradigm. Clin Microbiol Infect. 2012;18(7):615–616. | ||
Wright GD, Poinar H. Antibiotic resistance is ancient: implications for drug discovery. Trends Microbiol. 2012;20(4):157–159. | ||
Spellberg B, Powers JH, Brass EP, Miller LG, Edwards JE Jr. Trends in antimicrobial drug development: implications for the future. Clin Infect Dis. 2004;38:1279–1286. | ||
Col NF, O’Connor RW. Estimating world wide current antibiotic usage: report of Task Force 1. Rev Infect Dis. 1987;9(3):232–243. | ||
Carbon C, Bax RP. Regulating the use of antibiotics in the community. BMJ. 1998;317:663–665. | ||
Austin DJ, Kristinsson KG, Anderson RM. The relationship between the volume of antimicrobial consumption in human communities and the frequency of resistance. Proc Natl Acad Sci U S A. 1998;96:1152–1156 | ||
J Linares (1998) Community-acquired resistance: is it controllable. Int J Clin Pract. 1998;95(Suppl):23–26. | ||
Chretien JH, McGarvey M, Destwolinski A, Esswein JG. Abuse of antibiotics. A study of patients attending a university clinic. Arch Intern Med. 1975;135:1063–1065. | ||
Bax RP. Antibiotic resistance: a view from the pharmaceutical industry. Clin Inf. 24(Suppl 1):S151–S153. | ||
Grigoryan L, Haaijer-Ruskamp FM, Burgerhof JG, et al. Self-medication with antimicrobial drugs in Europe. Emerg Infect Dis. 2006;12(3):452. | ||
English BK, Gaur AH. The use and abuse of antibiotics and the development of antibiotic resistance. Adv Exp Med Biol. 2010;659:73–82. | ||
Al-Azzam SI, Al-Husein BA, Alzoubi F, Masadeh MM, Al-Horani MA. Self-medication with antibiotics in Jordanian population. Int J Occup Med Environ Health. 2007;20(4):373–380. | ||
Bin Abdulhak AA, Altannir MA, Almansor MA, et al. Non prescribed sale of antibiotics in Riyadh, Saudi Arabia: a cross sectional study. BMC Public Health. 2011;11:538. | ||
Seppala H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. N Engl J Med. 1997;337:441–446. | ||
Plachouras D, Kavatha D, Antoniadou A, et al. Dispensing of antibiotics without prescription in Greece, 2008: another link in the antibiotic resistance chain. Euro Surveill. 2010;15(7):19488. | ||
Llor C, Cots JM. The sale of antibiotics without prescription in pharmacies in Catalonia, Spain. Clin Infect Dis. 2009;48:1345–1349. | ||
Dameh M, Green J, Norris P. Over-the-counter sales of antibiotics from community pharmacies in Abu Dhabi. Pharm World Sci. 2010;32(5):643–650. | ||
Nimri LF, Batchoun R. Community-acquired bacteraemia in a rural area: predominant bacterial species and antibiotic resistance. J Med Microbiol. 2004;53:1045–1059. | ||
Battikhi MN. Epidemiological study on Jordanian patients suffering from diarrhoea. New Microbiol. 2002;25:405–412. | ||
Abu Shaqra Q. Occurrence and antibiotic sensitivity of Enterobacteriaceae isolated from a group of Jordanian patients with community acquired urinary tract infections. Cytobios. 2000;101:15–21. | ||
Madden JM, Quick JD, Ross Degnan D, Kafle KK. Undercover care-seekers: simulated clients in study health provider behavior in developing countries. Social Sci Med. 1997;45:1465–1482. | ||
Sá del Fiol F, Gerenutti M, Groppo FC. Antibiotics and pregnancy. Pharmazie. 2005;60(7):483–493. | ||
Chalker J, Ratanawijitrasin S, Chuc NT, Petzold M, Tomson G. Effectiveness of a multi-component intervention on dispensing practices at private pharmacies in Vietnam and Thailand – a randomized controlled trial. Soc Sci Med. 2005;60(1):131–141. | ||
Volpato DE, Souza BV, Rosa LGD, et al. Use of antibiotics without prescription. Braz J Infect Dis. 2005;9(3):288–291. | ||
Lansang MA, Lucas-Aquino R, Tupasi TE, et al. Purchase of antibiotics without prescription in Manila, the Philippines. Inappropriate choices and doses. J Clin Epidemiol. 1990;43:61–67. | ||
Matuz M, Benko R, Doro P, Hajdu E, Soos G. Non-prescription antibiotic use in Hungary. Pharm World Sci. 2007;29(6):695–698. |
Supplementary materials
Sale of non-prescribed antibiotics
Name of pharmacy: Location:
Sex: (male/female) Age group (years): (<30) – (30–50) – (>50)
Clinical presentation:
Was an antibiotic prescribed: (Yes/No)
If yes complete the following data:
- Which level of demand (1) – (2) – (3)
- Type of antibiotic
- Did the pharmacist?
- Explain how to take the antibiotic (Yes/No)
- Give the duration of treatment (Yes/No)
- Asked about drug allergy (Yes/No)
- Asked about other symptoms (Yes/No)
- Recommended consulting a physician (Yes/No)
- Asked about contaminant use of other drugs (Yes/No).
If no antibiotics were dispensed, complete the following data:
- Reason for not selling the antibiotic: administrative/health issues/both
- Type of alternative medication dispensed
- Did the pharmacist recommend consulting a physician (Yes/No)
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

