Back to Journals » Therapeutics and Clinical Risk Management » Volume 18
Discrepancy Between Forceps Biopsy and Resection in Colorectal Polyps: A 1686 Paired Screening-Therapeutic Colonoscopic Finding
Authors Jiang Y, Wang J , Chen Y, Sun H, Dong Z , Xu S
Received 27 January 2022
Accepted for publication 10 May 2022
Published 16 May 2022 Volume 2022:18 Pages 561—569
DOI https://doi.org/10.2147/TCRM.S358708
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Deyun Wang
Yuanxi Jiang, Junwen Wang, Ying Chen, Huihui Sun, Zhiyu Dong, Shuchang Xu
Department of Gastroenterology, Tongji Hospital, Tongji University School of Medicine, Shanghai, People’s Republic of China
Correspondence: Shuchang Xu; Zhiyu Dong, Department of Gastroenterology, Tongji Hospital, Tongji University School of Medicine, No. 389, Xincun Road, Putuo District, Shanghai, People’s Republic of China, Tel +86-136 0199 9711, Email [email protected]; [email protected]
Purpose: To identify pathology discrepancy between forceps biopsies and polypectomy specimens in colorectal polyps, as well as the reliability of biopsy-based treatment strategy.
Methods: All endoscopic polypectomy cases with forceps biopsies performed within 6 months were included in the study. The biopsies were compared with polypectomy specimens in terms of concordance of histological diagnosis. A logistic regression model was used to investigate the independent predictors of upgrade in histological diagnosis compared with concordance in histological diagnosis.
Results: A total of 1686 paired screening-therapeutic colonoscopies and 1739 paired biopsy-polypectomy specimens were enrolled in the study. The grade of dysplasia in 84.5% of biopsy specimens were concordant to polypectomy specimens, but this proportion decreased to 75.4% when the specimens were classified using tubular or villousness structure. 10.1% and 5.4% of biopsy specimens were upgraded and downgraded in assessing grade of dysplasia, respectively, while 14.3% and 10.3% of biopsy specimens were upgraded and downgraded in assessing tubular or villousness structure, respectively. In subgroup analysis stratified by size of polyps, 9.0% and 10.6% of biopsies obtained from polyps smaller than 10 mm were upgraded in assessing dysplasia and tubular or villousness structure, respectively. This proportion increased to 10.7% and 21.3%, respectively, in biopsies obtained from polyps larger than 10 mm. Larger size of polyps and pedunculated polyps were associated with a higher incidence of upgrade in histological diagnosis. Nearly 25% of biopsy specimens with high-grade dysplasia were identified as adenocarcinoma in polypectomy specimens.
Conclusion: The concordance between biopsy and polypectomy specimens is not adequate. The biopsy-based treatment strategy is not reliable and should not be considered as an indicator for further treatment, particularly in large or pedunculated polyps.
Keywords: colorectal polyps, colorectal adenoma, colonoscopy, pathology
Corrigendum for this paper has been published.
Introduction
Colorectal cancer (CRC) is one of the most common types of malignant tumors in the digestive tract.1 With the development of screening and therapeutic colonoscopy, a large number of precursor lesions and CRC can be detected and removed at an early stage, lowering the incidence and improving the prognosis of CRC.2,3
Though optical diagnosis has been attempted to predict the histology of colorectal polyps and is recommended in endoscopic management of polyps in recent guidelines,4 it is still far from popular in many countries, especially in primary care. Instead, endoscopists in many medical units around the world are used to obtaining biopsies of newly detected polyps in screening colonoscopies, which provides histological diagnosis of polyps for subsequent polypectomy. However, this strategy has some limitations. Firstly, the agreement of pathologists in identifying the grade of dysplasia in colorectal lesions has been reported to be poor to moderate.5–8 Furthermore, the biopsy-based treatment strategy considers histological diagnosis of part of lesions as the surrogate for histological diagnosis of entire lesions, which may lead to an overestimation or underestimation of the true diagnosis of entire lesions. Because of these constraints, lesions may be managed in an inappropriate manner.
Many previous studies have found a histological difference between biopsies and resected specimens in gastric lesions.9–13 However, studies on the discrepancy in histological diagnosis between biopsy and polypectomy specimens in colorectal polyps are scarce. A recent study in Sweden with 485 colorectal lesions pointed out the inconsistencies between biopsy and polypectomy specimens.14 However, due to the small sample size and the lack of data from polyps smaller than 10 mm, the results were limited. A comprehensive evaluation of the clinical value of biopsy-based treatment strategy for colorectal polyps is required.
The aim of this study was to demonstrate the agreement between biopsy and polypectomy specimens and investigate the factors associated with concordance and discordance between biopsy and polypectomy specimens. The grade of dysplasia, tubular or villousness structure and serrated structure were considered as primary outcome measures. The logistic regression model was used to explore the independent factors associated with discordance between biopsy and polypectomy specimens.
Methods
Data were collected from endoscopic procedure database and histological information database at our hospital and analyzed retrospectively between January 1, 2012 and June 30, 2019. This study was approved by the Ethics Committee of Tongji Hospital (K-W-2020-011) and performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. All patients signed an informed consent. The basic information of patients, bowel preparation quality, endoscopic manifestation and histological information were all documented. The location, size and lesion type of polyps were extracted from endoscopic reports.
All endoscopic resection cases with forceps biopsies within 6 months, as well as corresponding biopsy specimens and polypectomy specimens were enrolled in our study. Specimens without corresponding biopsy specimens or polypectomy specimens, as well as those with polyps in the same bowel segment or less than 10 cm apart in neighboring segments were excluded. The cases with rare benign or malignant lesions such as leiomyoma, fibroma and neuroendocrine tumors were also excluded. The inclusion and exclusion criteria, the number of cases and the number of biopsy specimens and polypectomy specimens are shown in a study flow diagram (Figure 1). Both the characteristics of the included and excluded resected polyps without biopsy results were listed to assess the selection bias (Supplementary Table 1).
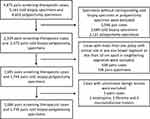 |
Figure 1 Study flow diagram. |
Histopathology
All biopsy and polypectomy specimens were embedded for histological examination in accordance with the Vienna classification of gastrointestinal neoplasia.15 All specimens were examined by pathologists at our hospital. However, the pathologists who examined the biopsy and polypectomy specimens from the same lesion might be different. In our hospital, the pathologist reviewing the second sample was encouraged to be blind to the first sample report. In order to verify the implementation effect of blindness method, the concordance of dysplasia as well as villousness examined by each pathologist was calculated and listed (Supplementary Table 2).
According to the discrepancy between biopsy and polypectomy specimens, lesions were classified as concordance (no difference between biopsy and polypectomy specimen) or discordance, and further classified as upgrade (higher histological grade in polypectomy specimen compared with biopsy) or downgrade (lower histological grade in polypectomy specimen compared with biopsy).
Statistical Analysis
The logistic regression model was used to investigate the independent factors associated with upgrade, a more clinically significant measure, in histological diagnosis compared with concordance in histological diagnosis. The discrepancy in grade of dysplasia and tubular or villousness structure were used as outcome measures of the logistic regression model. Polyp characteristics including location, size and lesion type, as well as patient characteristics consisting of age, gender, sedation and bowel preparation were entered into the model. Whether the same pathologist examined the biopsy and polypectomy specimen from the same lesion, as well as the time period between biopsy and resection were also included in the model.
All reported P values were two-sided with P <0.05 defined as statistical significance. All analysis was performed using R (R foundation for Statistical Computing, Vienna, Austria).
Results
A total of 4875 pairs of screening-therapeutic colonoscopies and corresponding 5161 cold biopsy specimens and 4603 polypectomy specimens were retrieved from our database and only 1686 pairs of screening-therapeutic colonoscopies and 1739 pairs of biopsy-polypectomy specimens were used for further analysis, as shown in the study flow diagram (Figure 1). 1739 pairs of biopsy-polypectomy specimens were classified as 1629 conventional class pairs and 110 serrated class pairs. Among all the polyps included in our analysis, 50.2% (873/1739) were smaller than 10 mm, 43.8% (762/1739) were between 10–20 mm and 6% (104/1739) were larger than 20 mm. In terms of the excluded polyps, the above sizes of polyps separately accounted for 73.4% (2103/2864), 24.7% (707/2864) and 1.9% (54/2864). The pedunculated polyps accounted for 28.9% (502/1739) and 27.5% (788/2864) in included and excluded polyps, respectively, with sessile polyps accounting for the remainder (Supplementary Table 1). The overall consistency rate of each pathologist was within a reasonable range, which indicates they did not refer to the previous report when making a diagnosis (Supplementary Table 2).
Reliability of Cold Biopsy in Assessing Dysplasia
84.5% (1469/1739) of biopsy specimens were concordant with polypectomy specimens in assessing dysplasia. 10.1% (176/1739) and 5.4% (94/1739) of biopsy specimens were upgraded and downgraded in assessing dysplasia, respectively (Table 1).
 |
Table 1 Concordance or Discordance of Dysplasia Between Cold Biopsy Specimen and Polypectomy Specimen |
Among 176 upgrade cases, 43.8% (106/242), 1.2% (3/242) cases judged as negative for dysplasia in biopsy specimens were assessed to be LGD and HGD, respectively. 3.4% (49/1461) and 0.6% (9/1461) LGD in biopsy were examined to be HGD and carcinoma respectively. 25.0% (9/36) cases judged as HGD were identified as carcinoma in polypectomy specimens.
As for 94 downgrade cases, 5.8% (85/1461) LGD in biopsy specimens were assessed to be no dysplasia in polypectomy specimens. 5.6% (2/36) and 19.4% (7/36) cases judged as HGD were identified as no dysplasia and LGD respectively.
In subgroup analysis stratified by size of polyps, 84.2% (962/1143) and 9.0% (103/1143) of biopsies obtained from polyps smaller than 10 mm were concordant with polypectomy specimens and upgraded in assessing dysplasia, respectively. Among 103 upgrade cases, 45.8% (87/190) of biopsies with no dysplasia, 1.5% (14/947) of biopsies with LGD and 33.3% (2/6) of biopsies with HGD were upgraded in assessing dysplasia. As for biopsies obtained from polyps larger than 10 mm, 85.1% (507/596) and 10.7% (64/596) of biopsies were concordant with polypectomy specimens and upgraded in assessing dysplasia, respectively. Among 64 upgrade cases, 42.3% (22/52) of biopsies with no dysplasia, 6.8% (35/514) of biopsies with LGD and 23.3% (7/30) of biopsies with HGD were upgraded in assessing dysplasia (Table 3).
 |
Table 2 Concordance or Discordance of Tubular or Villousness Status Between Cold Biopsy Specimen and Polypectomy Specimen |
 |
Table 3 Subgroup Analysis of Concordance or Upgrade of Dysplasia and Tubular or Villousness Status Stratified by Size of Polyps |
Reliability of Biopsy in Assessing Tubular or Villousness Structure and Adenocarcinoma
75.4% (1229/1629) biopsy specimens were concordant to polypectomy specimens in assessing tubular or villous structure and adenocarcinoma. 14.3% (232/1629) and 10.3% (168/1629) biopsy specimens were upgraded and downgraded in assessing tubular or villous structure and adenocarcinoma, respectively (Table 2).
Among 232 upgrade cases, 37.1% (75/202) and 4.0% (8/202) cases judged as hyperplastic or inflammatory polyps in biopsy specimens were assessed to be tubular adenoma and villous/tubulovillous adenoma in polypectomy specimens, respectively. 9.6% (116/1207) and 2% (24/1207) tubular adenoma in biopsy were examined to be villous/tubulovillous adenoma and adenocarcinoma, respectively. 4.2% (9/216) cases judged as villous/tubulovillous adenoma were identified as adenocarcinoma in polypectomy specimens.
As for 168 downgrade cases, 6.6% (80/1207) tubular adenoma in biopsy specimens were assessed to be non-neoplastic in polypectomy specimens. 0.9% (2/216) and 39.8% (86/216) cases judged as villous/tubulovillous adenoma were identified as non-neoplastic and tubular adenoma respectively.
In subgroup analysis stratified by size of polyps, 78.0% (840/1076) and 10.6% (114/1076) of biopsies obtained from polyps smaller than 10 mm were concordant with polypectomy specimens and upgraded in assessing tubular or villousness structure, respectively. Among 114 upgrade cases, 42.9% (69/161) of biopsies with non-neoplastic, 5.1% (43/836) of biopsies with tubular adenoma and 2.5% (2/79) of biopsies with villous/tubulovillous adenoma were upgraded in assessing tubular or villousness structure. As for biopsies obtained from polyps larger than 10 mm, 69.9% (387/553) and 21.3% (118/553) of biopsies were concordant with polypectomy specimens and upgraded in assessing dysplasia, respectively. Among 61 upgrade cases, 34.1% (14/41) of biopsies with non-neoplastic, 26.0% (97/373) of biopsies with tubular adenoma and 5.1% (7/137) of biopsies with villous/tubulovillous adenoma were upgraded in assessing tubular or villousness structure (Table 3).
Variables Affecting Reliability of Biopsy in Assessing Dysplasia, Tubular or Villousness Structure and Adenocarcinoma
Larger size of polyps was an independent factor associated with a higher proportion of underestimating dysplasia in multivariate logistic regression analysis (Table 4). The polyps larger than 20 mm significantly increased the risk of underestimating to 2.45 times.
 |
Table 4 Results of Logistic Regression Model Using Underestimating Dysplasia and Tubular or Villousness Status in Biopsy Specimens as Outcome Measures |
In addition, larger size of polyps and pedunculated polyps were significantly associated with a higher proportion of underestimating tubular or villousness status and adenocarcinoma. Polyps between 10–20 mm and polyps larger than 20 mm significantly increased the risk of underestimating to 1.94 times and 2.89 times, respectively, compared with polyps smaller than 10 mm. And sessile polyps significantly decreased the risk of underestimating to 0.67 times compared with pedunculated polyps.
Overview of Underestimating the Villousness Structure and Carcinoma as Well as Mistaking Serrated Class for Conventional Class
In overview of villousness structure (Table 5), the proportion of underestimating in polyps between 10–20 mm and polyps larger than 20 mm was significantly higher than that in polyps smaller than 10 mm (10~20 mm vs <10 mm, 11.9% vs 2.2%, Adjusted P <0.001; >20 mm vs <10 mm, 13.3% vs 2.2%, Adjusted P <0.001). The incidence of underestimating was higher in pedunculated polyps compared with sessile polyps (12.2% vs 4.9%, Adjusted P <0.001). The villousness structure was underestimated in 3.7% (8/219) of polyps with non-neoplastics and 9.6% (116/1213) of tubular adenomas.
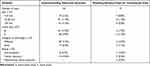 |
Table 5 Overview of Underestimating Villousness Status in Biopsy Specimens |
In overview of 17 cases mistaking serrated class for conventional class (Table 5), the serrated class polyps were mistaken for conventional class polyps in 0.8% (7/873) of polyps smaller than 10 mm and 1.3% (10/762) of polyps between 10–20 mm. Only 1.0% of sessile polyps (12/1215) and pedunculated polyps (5/525) were mistaken for conventional class polyps. 5.0% (11/219) of polyps with non-neoplastic, 0.3% (4/1213) of tubular adenomas and 0.9% (2/221) of tubulovillous/villous adenomas were mistaken for conventional class polyps.
In overview of underestimating carcinoma (Table 6), the proportion of underestimating in polyps larger than 20 mm was significantly higher than that in polyps smaller than 10 mm and polyps between 10–20 mm (>20 mm vs <10 mm, 6.7% vs 0.1%, Adjusted P <0.001; >20 mm vs 10–20 mm, 6.7% vs 1.3%, Adjusted P = 0.006). The carcinoma was underestimated in 0.6% (9/1402) lesions with LGD and 25.0% (9/36) lesions with HGD.
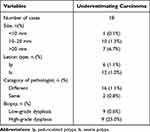 |
Table 6 Overview of Underestimating Carcinoma in Biopsy Specimens |
Discussion
The optimal management of polyps depends on the pretherapeutic diagnosis of lesions. Endoscopic evaluation of size, morphological characteristics, surface type and pit pattern of colorectal lesions for pretherapeutic diagnosis are strongly recommended in recent guidelines.4 Unlike these well-defined indicators, the role of biopsy in pretherapeutic diagnosis has not been thoroughly investigated, despite the fact that histological diagnosis of biopsy has been used for pretherapeutic diagnosis of colorectal lesions in many medical units around the world. In order to comprehensively illustrate the agreement between biopsy and polypectomy specimens, we used grade of dysplasia, tubular or villousness structure and serrated structure as primary outcome measures.
In our study, grade of dysplasia in 84.5% of biopsy specimens was concordant to polypectomy specimens, but this proportion decreased to 75.4% when the specimens were classified using tubular or villousness structure. 9.0% and 14.3% biopsy specimens were underestimated in assessing grade of dysplasia and tubular or villousness structure, respectively. The villousness structure was underestimated in 3.7% of non-neoplastic lesions and 9.6% of tubular adenomas identified in biopsy specimens. As for serrated structure, only 17 cases identified as serrated class polyps in polypectomy specimens were mistaken for conventional class polyps in biopsy specimens. In total 18 carcinomas were mistaken for precancerous lesions in biopsy. Notably, the malignancy was underestimated in 25% of high-grade dysplasia identified in biopsy specimens, indicating a high possibility of incorrect treatment selection when the biopsy-based treatment strategy was considered as the primary indicator for treatment. Our findings are consistent with other relevant studies. A prospective study demonstrated that biopsy-based diagnosis underestimated histological diagnosis in about 10% of colorectal adenomas, and this proportion increased to more than 60% in advanced neoplasia.16 According to a recent retrospective study, only about 60% of biopsies of large colorectal lesions provided the correct grade of dysplasia when compared with final resected specimens and biopsies underestimated the grade of dysplasia in about 30% of large colorectal lesions.14 Both of these studies, as well as ours, indicate that the clinical effectiveness of a biopsy-based treatment strategy is questionable and neither negative results (hyperplastic or inflammatory polyps) nor cancer-negative results in biopsy specimens are reliable in assessing colorectal lesions referred for further endoscopic treatment.
In order to explore the independent factors associated with upgrade between biopsy and polypectomy specimens, we used a logistic regression model and considered the grade of dysplasia and tubular or villousness structure as the outcome measures. In our results, the size of polyps was the only independent factor associated with underestimating the grade of dysplasia. As for assessing the tubular or villousness structure, larger size of polyps and pedunculated polyps were significantly associated with a higher incidence of underestimating. The size of polyps has been found to play an important role in discrepancy between biopsy and resected specimens in studies on gastric and colorectal lesions.9–11,13 The decreased relative tissue volume obtained by biopsy in larger polyps might lead to more frequent underestimating. The relationship between type of lesions and discordance between biopsy and resected specimens still remained uncertain. Only one study on colorectal lesions found no significant difference in proportion of discordance in grade of dysplasia between polyps with different lesion types.14 Our study confirmed the previous results in grade of dysplasia and we also found that the proportion of underestimating tubular or villousness structure was significantly higher in pedunculated polyps compared with sessile polyps, which had never been investigated in previous studies.
One of the major limitations of our study is that this is a retrospective study, and all paired biopsy-polypectomy specimens were obtained retrospectively based on the information from endoscopic procedure database, which may lead to mismatched biopsy-polypectomy specimens. To minimize the possibility of mismatch, we excluded the biopsy or polypectomy specimens with polyps in the same bowel segment or less than 10 cm apart in neighboring segments in our study. Furthermore, it was obvious that the size of the polyps had significantly influenced the decision to perform biopsy prior to endoscopic resection, resulting in a selection bias ((Supplementary Table 1).
In conclusion, our findings demonstrated that neither negative results (hyperplastic or inflammatory polyps) nor other cancer-negative results for biopsies are reliable in assessing the colorectal lesions referred for further endoscopic treatment. The size of polyps was associated with discordance in assessing grade of dysplasia and tubular or villousness structure, while pedunculated polyps were associated with a higher incidence of underestimating tubular or villousness structure. As a result, the histological diagnosis of biopsy should be treated cautiously, particularly in large or pedunculated colorectal polyps, and the biopsy-based strategy should not be considered as an indicator for further treatment.
Acknowledgments
The authors wish to acknowledge Tingting Zhan for her invaluable assistance. She re-analyzed the original data to complete Tables 3, 4 and Supplementary Table 2. She also wrote the responses point-by-point and helped revise the manuscript.
Disclosure
The authors declared that they have no conflicts of interest in this work.
References
1. Brody H. Colorectal cancer. Nature. 2015;521:S1.
2. Zauber AG, Winawer SJ, O’Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366:687–696. doi:10.1056/NEJMoa1100370
3. Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977–1981. doi:10.1056/NEJM199312303292701
4. Kaltenbach T, Anderson JC, Burke CA, et al. Endoscopic Removal of Colorectal Lesions-Recommendations by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology. 2020;158:1095–1129. doi:10.1053/j.gastro.2019.12.018
5. Rex DK, Alikhan M, Cummings O, et al. Accuracy of pathologic interpretation of colorectal polyps by general pathologists in community practice. Gastrointest Endosc. 1999;50:468–474. doi:10.1016/S0016-5107(99)70067-2
6. Lederer PC. Response to: properties of different pancreatin preparations used in pancreatic exocrine insufficiency. Eur J Gastroenterol Hepatol. 2009;21(9):1024–1031. doi:10.1097/MEG.0b013e328328f414
7. Foss FA, Milkins S, McGregor AH. Inter-observer variability in the histological assessment of colorectal polyps detected through the NHS Bowel Cancer Screening Programme. Histopathology. 2012;61:47–52. doi:10.1111/j.1365-2559.2011.04154.x
8. Osmond A, Li-Chang H, Kirsch R, et al. Interobserver variability in assessing dysplasia and architecture in colorectal adenomas: a multicentre Canadian study. J Clin Pathol. 2014;67:781–786. doi:10.1136/jclinpath-2014-202177
9. Kim YJ, Park JC, Kim JH, et al. Histologic diagnosis based on forceps biopsy is not adequate for determining endoscopic treatment of gastric adenomatous lesions. Endoscopy. 2010;42:620–626. doi:10.1055/s-0030-1255524
10. Cho SJ, Choi IJ, Kim CG, et al. Risk of high-grade dysplasia or carcinoma in gastric biopsy-proven low-grade dysplasia: an analysis using the Vienna classification. Endoscopy. 2011;43:465–471. doi:10.1055/s-0030-1256236
11. Lim H, Jung HY, Park YS, et al. Discrepancy between endoscopic forceps biopsy and endoscopic resection in gastric epithelial neoplasia. Surg Endosc. 2014;28:1256–1262. doi:10.1007/s00464-013-3316-6
12. Maekawa A, Kato M, Nakamura T, et al. Incidence of gastric adenocarcinoma among lesions diagnosed as low-grade adenoma/dysplasia on endoscopic biopsy: a multicenter, prospective, observational study. Dig Endosc. 2018;30:228–235. doi:10.1111/den.12980
13. Noh CK, Jung MW, Shin SJ, et al. Analysis of endoscopic features for histologic discrepancies between biopsy and endoscopic submucosal dissection in gastric neoplasms: 10-year results. Dig Liver Dis. 2019;51:79–85. doi:10.1016/j.dld.2018.08.027
14. Ronnow CF, Uedo N, Stenfors I, et al. Forceps Biopsies Are Not Reliable in the Workup of Large Colorectal Lesions Referred for Endoscopic Resection: should They Be Abandoned? Dis Colon Rectum. 2019;62:1063–1070. doi:10.1097/DCR.0000000000001440
15. Dixon MF. Gastrointestinal epithelial neoplasia: Vienna revisited. Gut. 2002;51:130–131. doi:10.1136/gut.51.1.130
16. Gondal G, Grotmol T, Hofstad B, et al. Biopsy of colorectal polyps is not adequate for grading of neoplasia. Endoscopy. 2005;37:1193–1197. doi:10.1055/s-2005-921031
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
