Back to Journals » Cancer Management and Research » Volume 11
Differential effects of adjuvant EGFR tyrosine kinase inhibitors in patients with different stages of non-small-cell lung cancer after radical resection: an updated meta-analysis
Authors Lu D, Wang Z, Liu X, Feng S, Dong X, Shi X , Wang H , Wu H , Xiong G, Wang HF, Cai K
Received 18 September 2018
Accepted for publication 8 February 2019
Published 2 April 2019 Volume 2019:11 Pages 2677—2690
DOI https://doi.org/10.2147/CMAR.S187940
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Rituraj Purohit
Di Lu,* Zhizhi Wang,* Xiguang Liu,* Siyang Feng, Xiaoying Dong, Xiaoshun Shi, He Wang, Hua Wu, Gang Xiong, Haofei Wang, Kaican Cai
Department of Thoracic Surgery, Nanfang Hospital, Southern Medical University, Guangzhou, Guangdong, China
*These authors contributed equally to this work
Purpose: A survival improvement was achieved with adjuvant chemotherapy in non-small-cell lung cancer (NSCLC) patients, but its differential effects among patients with different stages remained controversial. This study aimed to compare the beneficial effects of adjuvant tyrosine kinase inhibitor (TKI) therapy with those of traditional therapy on NSCLC patients, specifically on EGFR-mutant and stage II–IIIA patients, who might benefit most from such treatment.
Methods: MEDLINE, Embase, and the Cochrane Library were searched, and the results were screened independently according to certain criteria by two authors. Disease-free survival (DFS) and overall survival (OS) with HRs were used as the summary statistics.
Results: A total of 2,915 publications were identified and screened. Six randomized control trials and three retrospective cohort studies of 2,467 patients with acceptable quality were included. The overall EGFR mutation rate was 48.62%. DFS was significantly improved in all the patients (HR, 0.77; 95% CI, 0.68–0.88) and in the subgroup of EGFR-mutant patients (HR, 0.49; 95% CI, 0.40–0.61). The difference of 5-year OS in the subgroup of EGFR-mutant patients (HR, 0.48; 95% CI, 0.31–0.72) was statistically significant, while in all the patients (HR, 1.01; 95% CI, 0.85–1.19), the difference was not significant. In the subgroups of studies in which <50% of patients were in stage I (HR, 0.46; 95% CI, 0.35–0.60) and >30% of patients were in stage IIIA (HR, 0.46; 95% CI, 0.35–0.60), DFS was significantly improved, while in the subgroups of studies in which <30% of patients were in stage IIIA (HR, 0.90; 95% CI, 0.77–1.04) and >50% of patients were in stage I (HR, 0.90; 95% CI, 0.77–1.04), DFS was not significantly improved.
Conclusion: Stage IIIA NSCLC patients might benefit more from adjuvant TKIs than stage I NSCLC patients after radical resection.
Keywords: non-small-cell lung cancer, EGFR tyrosine kinase inhibitor, adjuvant therapy, meta-analysis
Introduction
Among all the lung cancer cases diagnosed each year, around 20%–25% are resectable NSCLC.1 However, the 5-year survival rates for patients with stages IIIA, IIB, and IIA are only 24%, 36%, and 46%, respectively, while the 5-year survival rates for patients with stages IA and IB are 73% and 58%.2 Several large-scale randomized clinical trials were therefore carried out from 2003 to 2008 to assess the efficacy of adjuvant chemotherapy after radical resection, with the aim of improving long-term survival among these patients.3–5 Although these studies demonstrated an improvement in OS of 4% at 5 years, especially in patients with stage II–IIIA NSCLC,1 the long-term survival rate was largely unchanged, and the adverse effects of the adjuvant agents led to poor compliance with chemotherapy, indicating the need for further studies.
Given the outstanding survival improvement associated with the use of adjuvant EGFR-TKIs in patients with end-stage NSCLC and EGFR mutations compared with traditional chemotherapy,6–13 the efficacy of these agents in NSCLC patients undergoing complete resection has become an attractive topic. However, two early trials that neglected the patients’ EGFR mutation status reported negative results,14,15 while the results of the ADJUVANT and EVAN study that only recruited patients with EGFR mutations showed the great potential benefit of TKIs over chemotherapy.16,17 Additionally, the newly reported studies showed that stage II–IIIA patients might benefit more from TKIs,16,18–20 though this has not been analyzed further. Although a recent pooled analysis showed that adjuvant EGFR-TKI therapy might enhance DFS in patients with EGFR-mutant NSCLC, the study found no significant benefit of TKIs in terms of OS, and differences in their effects among patients with different stages of NSCLC were not further investigated. The potential superiority of EGFR-TKIs over cytotoxic agents in adjuvant therapy in patients with NSCLC thus remains controversial, and the influence of EGFR mutation status and cancer stage still needs to be elucidated.
The recent release of a few new studies led us to perform a meta-analysis to compare the beneficial effects of adjuvant TKI therapy with those of traditional chemotherapy in NSCLC patients undergoing radical resection, aimed specifically at identifying those subgroups of patients, such as EGFR-mutant and stage II–IIIA patients, who might benefit most from such treatment. The results could thus provide information and guidance for clinicians and researchers in this field.
Methods
Strategy for literature search
MEDLINE (PubMed interface), Embase, and the Cochrane Library were searched without any restrictions on publication status, type, date, or language to identify eligible studies. The following search terms were used: (“pulmonary neoplasms” OR “lung cancer” OR “lung neoplasm” OR “pulmonary cancer”) AND (“EGFR tyrosine kinase inhibitors” OR “EGFR TKI” OR “gefitinib” OR “erlotinib” OR “icotinib” OR “afatinib” OR “dacomitinib” OR “neratinib” OR “vandetanib” OR “canertinib” OR “pelitinib” OR “AZD9291” OR “CO-1686” OR “HM61713” OR “EGF816” OR “ASP8273”) AND (“adjuvant” OR “ancillary” OR “auxiliary” OR “appurtenant” OR “accessory” OR “adjunct” OR “intercalated” OR “alternative”). The latest search was conducted on September 12th, 2017.
Study selection
Studies were included according to the following criteria: 1) involving adult patients diagnosed with pathological stage I–IIIA NSCLC suitable for adjuvant chemotherapy or chemoradiotherapy; 2) assessing the efficacy of adjuvant EGFR-TKIs vs chemotherapy or placebo, or adjuvant combination of TKIs and chemotherapy vs chemotherapy alone; 3) reporting at least one pertinent clinical outcome such as DFS or OS with long-term follow-up; and 4) containing original data sufficient for calculating the HR or P-value. The included studies were published in English, with no restriction on publication type.
The exclusion criteria were: 1) single-arm study reporting adjuvant EGFR-TKI outcomes; 2) studies with irretrievable or insufficient data for statistical analysis; 3) duplicates; and 4) original articles with unavailable full text.
Outcomes and data extraction
The outcomes of interest included DFS, OS at different time points from 1 to 5 years, and adverse effects of TKIs and cytotoxic agents such as rash, acne, diarrhea, dyspnea, fatigue, nausea, and vomiting.
All the publications identified through the literature search were reviewed independently by two investigators (D Lu and Z Wang) to assess their eligibility at the level of title and/or abstract, and disagreements were documented and resolved by discussion with a third reviewer (K Cai). Additionally, the full text of identified related meta-analyses and reviews was investigated in detail to detect any additional hidden data.
Data extraction was carried out using a spreadsheet, as described previously,21 to improve efficiency and avoid possible mistakes. In addition to the outcomes, other basic information was extracted as follows: first author, affiliation, published date, study design, number of enrolled patients, gender percentage, EGFR mutation percentage, usage of TKIs, number of patients in each stage, median treatment duration, and control group therapy.
Quality assessment
The methodological quality of the included studies was assessed independently by the two investigators above as we mentionedbefore.21 A rating system called Newcastle–Ottawa scale22 was used for non-randomized cohort studies, which consists of three domains: selection, comparability, and outcome. Total score achieved from the scores of the three sections (selection 0–4, comparability 0–2, outcome 0–3) ranged from zero star to nine stars, which was positively correlated with the study’s quality. Studies awarded with more than five stars were considered to be of acceptable quality. The detailed scores of the included studies are given in Table S1. Quality of the included RCTs was evaluated according to the Cochrane Collaboration’s tool for assessing risk of bias (5.3.0)23 with the following methodological items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other potential source of bias. Each item was classified as low risk, high risk, or unclear risk, which determined the general quality when taken together. The risk-of-bias graph and summary are presented in a figure from in Figure S1. Disagreement was resolved through discussion with the third reviewer.
Statistical analysis
The outcomes of DFS and OS at different years after radical surgery were treated as dichotomous variables, and the HR and 95% CI were used as the summary statistics. Data were extracted from the included studies according to the methods of Tierney et al24 and Parmar et al.25 c2 tests and I2 statistic were used to measure heterogeneity for each pooled analysis to estimate the percentage of total variation across the included studies that was due to heterogeneity rather than chance. Significant heterogeneity was defined as Phet ≤0.1 and I2≥50%. In the event of significant heterogeneity, a random-effects model was used, and sensitivity analyses were performed by deselecting studies sequentially to identify the sources of the heterogeneity. In the absence of significant heterogeneity, a fixed-effects model was used. The pooled statistics are presented as forest plots, and publication bias was evaluated visually by funnel plots and statistically by Egger’s and Begg’s tests. Specific analyses considering confounding factors could not be conducted due to the unavailability of adequate original data. All P-values were two-sided and the significance level was set at 0.05, except for Phet. All the pooled analyses, related plots, and Egger’s and Begg’s tests were managed using Stata/SE version 12.0 (StataCorp, College Station, TX, USA).
This meta-analysis was performed in accordance with the PRISMA standards.
Results
Eligible studies
A total of 2,915 publications were identified by combining the results from MEDLINE (609), Embase (2,542), and the Cochrane Library (116), and removing duplicates (Figure 1). After reviewing the titles and abstracts of these articles, the full text of 31 studies was subsequently reviewed for eligibility. Nine studies of acceptable quality were finally included in the meta-analysis according to the inclusion and exclusion criteria, of which six were RCTs and three were RCSs.
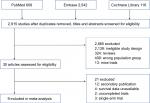  | Figure 1 Flowchart presenting study selection. |
A total of 2,467 patients were involved in the pooled analysis, including 1,248 in the adjuvant TKI group and 1,209 in the control group, with 76.26% of the involved patients from RCTs. All of the cases in seven studies were diagnosed with EGFR-mutated NSCLC.17–19,26–29 The other two studies (BR19 and RADIANT)14,15 also reported detailed data for EGFR-mutant subgroups, though the proportions were relatively low (4% and 16.5%, respectively). Information on pathological stage was available for all nine studies, and patients with stage I NSCLC were not included in three studies.17,26,27 Two studies18,27 referred to the sixth edition of TNM staging system released by the American Joint Committee on Cancer/Union for International Cancer Control, and seven studies14,15,17,19,26,28,29 consulted the seventh edition. The control groups in four studies14,15,28,29 were treated with placebo, while the control groups in the other five studies17–19,26,27 received chemotherapy. The characteristics of all the nine included studies are shown in Table 1.
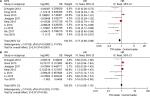
Effects of adjuvant TKIs on DFS and OS in NSCLC patients
DFS was analyzed in six RCTs14,15,17,18,26,27 and three RCSs19,28,29 (Figure 2A). Compared with the control arm, adjuvant EGFR-TKIs improved DFS (HR, 0.77; 95% CI, 0.68–0.88; Figure 2A). Built on a random-effects model, significant heterogeneity was noted across the studies involved (Phet <0.00001, I2=79%), and Egger’s and Begg’s tests showed significant publication bias in terms of DFS (Egger’s P=0.040; Begg’s P=0.754). In contrast, four RCTs14,15,17,27 and three RCSs19,28,29 were included in the quantitative analysis of OS, which showed no significant beneficial effect of EGFR-TKI treatment (HR, 1.01; 95% CI, 0.85–1.19; Figure 2B) and no significant publication bias (Egger’s P=0.408; Begg’s P=0.548). Although there was significant heterogeneity (Phet =0.003, I2=70%), no single trial notably affected the pooled results for DFS or OS according to the sensitivity analyses.
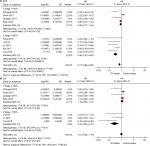
Effects of adjuvant TKIs on DFS and OS in NSCLC patients with EGFR mutations
As noted above, six RCTs14,15,17,18,26,27 and three RCSs19,28,29 were used to evaluate DFS, and two RCTs17,27 and three RCSs19,28,29 to assess OS (Figure 3). EGFR-TKIs demonstrated a significant beneficial effect on DFS in patients with mutant EGFR (HR, 0.49; 95% CI, 0.40–0.61; Figure 3A). There was no significant heterogeneity (Phet =0.37, I2=7%) but significant publication bias existed (Egger’s P=0.035; Begg’s P=0.072) among the included studies. TKIs also had a similar beneficial effect on OS in the EGFR mutation group (HR, 0.48; 95% CI, 0.32–0.71; Figure 3B), with no significant heterogeneity (Phet =0.44, I2=0%) or publication bias (Egger’s P=0.110; Begg’s P=0.221).
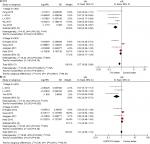
Effects of adjuvant TKIs on DFS and OS in NSCLC patients in relation to proportion of stage I disease
According to Table 2, the above studies were separated into two subgroups according to the different percentages (30%, 40%, and 50%) of patients with stage I NSCLC. TKIs were associated with significantly better DFS in the subgroups of studies in which >30% and >40% of patients were diagnosed with stage I NSCLC (HR, 0.85; 95% CI, 0.47–0.99), while in the subgroup of studies in which >50% of patients were diagnosed with stage I NSCLC, there was no beneficial effect of TKI with statistical significance (HR, 0.90; 95% CI, 0.77–1.04). In this way, the cutoff value of 50% was used for further pooled analyses of the effects of adjuvant TKIs in relation to proportion of stage I disease.
The above studies were divided into two subgroups according to the proportion of patients with stage I NSCLC (>50% or <50%). The use of EGFR-TKIs was associated with higher DFS among five studies17–19,26,27 including <50% of patients diagnosed with stage I NSCLC (HR, 0.46; 95% CI, 0.35–0.60; Figure 4A), with no significant heterogeneity (Phet =0.39, I2=4%) but significant publication bias (Egger’s P=0.049; Begg’s P=0.027). However, there was no significant difference in DFS between the two arms in the subgroup of four studies14,15,28,29 including >50% of patients diagnosed with stage I NSCLC (HR, 0.90; 95% CI, 0.77–1.04; Figure 4A), with significant heterogeneity (Phet =0.002, I2=80%) but no publication bias (Egger’s P=0.186; Begg’s P=0.734). No single study had any notable effect on the pooled results according to sensitivity analyses for DFS in the subgroup of studies including >50% of patients with stage I NSCLC. Among the four RCTs and three RCSs evaluated for OS, EGFR-TKIs were more effective than the control in the subgroup of three studies17,19,27 including <50% of patients diagnosed with stage I NSCLC (HR, 0.42; 95% CI, 0.24–0.73; Figure 4B), with no significant heterogeneity (Phet =0.21, I2=37%). However, there was no significant difference between the TKI and control groups among four studies14,15,28,29 including >50% of patients diagnosed with stage I NSCLC, and significant heterogeneity was indicated (Phet =0.09, I2=53%). In the subgroup among studies including >50% of patients diagnosed with stage I NSCLC, the study of D’Angelo28 might be the source of heterogeneity according to sensitivity analyses for the pooled results of OS.
Effects of adjuvant TKIs on DFS in NSCLC patients in relation to proportion of stage III disease
Similarly, in the subgroups of studies in which <40% and <50% of patients were diagnosed with stage III NSCLC, the differences of beneficial effect of TKI were significant (HR, 0.49; 95% CI, 0.36–0.67), while the difference became insignificant in the subgroups of studies in which <30% of patients were diagnosed with stage III NSCLC (HR, 0.92; 95% CI, 0.79–1.07). Therefore, the cutoff value of 30% was used for further pooled analyses of the effects of adjuvant TKIs in relation to the proportion of stage III NSCLC.
Among the subgroup of five studies17–19,26,27 in which >30% of patients were diagnosed with stage III NSCLC, TKIs were associated with significantly better DFS (HR, 0.46; 95% CI, 0.35–0.60; Figure 5A), with significant heterogeneity (Phet =0.39, I2=4%) and no significant publication bias (Egger’s P=0.186; Begg’s P=0.734). However, no such benefit was found in the subgroup of four studies14,15,28,29 including <30% of patients with stage III NSCLC (HR, 0.90; 95% CI, 0.77–1.04; Figure 5A), with significant heterogeneity (Phet =0.002, I2=80%) and no significant publication bias (Egger’s P=0.11; Begg’s P=0.806). Among the four RCTs and three RCSs evaluated for OS, EGFR-TKIs were more effective than the control in the subgroup of three studies17,19,27 including >30% of patients diagnosed with stage III NSCLC (HR, 0.42; 95% CI, 0.24–0.73; Figure 5B), with no significant heterogeneity (Phet =0.21, I2=37%). Sensitivity analyses for DFS and OS showed that no individual trials obviously modified the results. However, there was no significant difference between the TKI and control groups among four studies14,15,28,29 including <30% of patients diagnosed with stage III NSCLC (HR, 1.10; 95% CI, 0.92–1.31; Figure 5B), and significant heterogeneity was indicated (Phet =0.09, I2=53%). In this subgroup among studies including <30% of patients diagnosed with stage III NSCLC, the study of D’Angelo28 might be the source of heterogeneity according to sensitivity analyses for the pooled results of OS.
Ongoing clinical trials
As shown in Table 3, six ongoing clinical trials involving 1,770 patients were all developed in parallel assignment for the intervention model. Two studies are collecting single-stage patients, including one (NCT02264210) collecting stage IB and one collecting stage IIIA patients (NCT01410214). Three of the studies are based on patients with stage I–III NSCLC, and one trial was designed for patients with stage II–III disease. Four of the studies were recruiting, one was active but not recruiting (NCT01746251), and the status of the other was unknown (NCT01410214) at the time of the current meta-analysis. All these trials are expected to be completed before 2021.
  | Table 3 Characteristics of patients in ongoing studies Abbreviations: A, afatinib; AZ, AZD9291; E, erlotinib; I, icotinib. |
Discussion
From a clinical perspective, patients with NSCLC with EGFR mutation tend to benefit from adjuvant EGFR-TKI treatment in terms of both DFS and OS. Notably, the results of the current meta-analysis indicated that, although EGFR-TKIs significantly improved DFS and OS among patients with stage II–IIIA NSCLC,17,26 EGFR-TKI treatment was not justified in patients with stage I NSCLC.
Two previous meta-analyses showed that EGFR-mutant patients benefited from adjuvant TKI treatment,30,31 and the current updated analysis included two more clinical trials accounting for an additional 269 patients and 29.3% more patients with EGFR-mutant status. This study therefore strengthened the evidence for the efficacy of adjuvant EGFR-TKI treatment in terms of DFS in EGFR-mutant patients with NSCLC. Furthermore, the results notably suggested that NSCLC patients with mutant EGFR may benefit from adjuvant EGFR-TKI treatment in terms of OS.
The ability of adjuvant chemotherapy to improve the prognosis of patients with resected stage IB NSCLC remains controversial. A previous meta-analysis proposed that adjuvant chemotherapy could increase long-term DFS and OS among patients with postoperative stage IB NSCLC.32 However, an RCT designed specifically for stage IB NSCLC concluded that routine adjuvant chemotherapy was not justified in all patients with stage IB NSCLC.33 Furthermore, another study suggested that adjuvant chemotherapy was associated with improved DFS in patients with stage I NSCLC with high-risk clinicopathologic characteristics such as poorly differentiated tumor, vascular invasion, wedge resection, tumor >4 cm, visceral pleural involvement, and incomplete lymph node sampling.34 However, even among the studies showing that adjuvant chemotherapy was effective in patients with early stage (IB–III) NSCLC, the absolute survival improvements were only 4% at 5 years.1 In the current meta-analysis, we compared the efficacies of adjuvant EGFR-TKI treatment among patients with different stages of NSCLC to determine which stages benefited from EGFR-TKI treatment after radical resection. We showed that patients with stage II or IIIA NSCLC benefited more from adjuvant EGFR-TKI than those with stage I NSCLC. We therefore divided the included studies into subgroups according to the percentage of patients with stage I, and showed that the subgroup containing a higher percentage of patients with stage I disease (ie, outcomes of patients with stage I contributed more to the overall outcome) benefited less from EGFR-TKI treatment. In contrast, the subgroup with fewer cases of stage I compared with stages II and III showed a more effective outcome following EGFR-TKI treatment, with improvements in both DFS and OS. Compared with the previous meta-analyses, the current study included 117 more patients with stage I NSCLC, accounting for 11% of all stage I patients, thus strengthening the evidence for a differential benefit of EGFR-TKIs according to the stage of NSCLC. The current results therefore do not support the routine use of adjuvant EGFR-TKIs as standard treatment for patients with stage IB NSCLC. Radical surgery has been considered as a standard treatment for improving survival in patients with early-stage NSCLC, especially those without metastasis to distant lymph nodes, with 5-year survival rates approaching 80% in stage I and a median survival approaching 5.71 years after curative resection.35 Patients with stage IB NSCLC thus have a better prognosis compared with N1- or N2-positive patients, suggesting that adjuvant chemotherapy may contribute less in these patients. The recent American Society of Clinical Oncology guidelines asserted that “For individuals with stage IB, adjuvant cisplatin-based chemotherapy is not recommended for routine use”.36 This conclusion is supported by our current study.33
Although adjuvant chemotherapy has demonstrated benefits in patients with resected early-stage NSCLC, the absolute survival improvement was only 4% at 5 years, even in stage II–IIIA patients.1 However, two recent clinical trials notably demonstrated absolute benefits in terms of 3-year DFS of 7.1% in N1-positive patients26 and 25% in N2-positive patients.17 Furthermore, we analyzed stage III patients in a similar way to stage I patients and found that patients in the subgroup of studies including fewer cases of stage III NSCLC benefited less from adjuvant EGFR-TKI treatment, while those in the subgroup with more stage III NSCLC cases showed a benefit of TKIs in terms of DFS, but not OS. Compared with the previous meta-analyses, the current analysis included an additional 127 patients with stage III NSCLC, accounting for 24% of stage III patients, thus strengthening the evidence for a benefit of adjuvant EGFR-TKI treatment in patients with certain stages of NSCLC.
Several studies found that high copy numbers of ctDNA were associated with shorter OS and DFS.37–39 High levels of ctDNA could be indicative of higher overall tumor burden in patients with stage II–III compared with patients with stage IB disease.40 One study proposed that patients with detectable ctDNA had a poorer prognosis than patients with undetectable ctDNA, and that a poorer prognosis was associated with the detection of ctDNA and extrathoracic lymph node metastasis.41 Given that TKI and chemotherapy represent systematic therapies while radical resection is a local therapy, and that ctDNA is not scavenged after R0 surgery, adjuvant therapy (TKI or chemotherapy) could be beneficial in NSCLC patients postoperatively. On the other hand, the fact that EGFR-TKI treatment was more effective in patients with stage II–III compared with stage IB disease may be expected given that tumor burden was positively related to the amount of ctDNA.
Furthermore, the differences in prognoses among patients with different NSCLC stages after R0 resection suggest that radical surgery is necessary but not sufficient, especially in patients with stage II–IIIA NSCLC, according to a study of adjuvant chemotherapy.42 The present pooled analysis similarly showed that patients with stage II–IIIA NSCLC benefited more from postoperative TKIs than stage I patients, supporting the existence of differential beneficial effects of postoperative chemotherapy among NSCLC patients with different stages. We hypothesized that cellular or molecular tumor residues, such as circulating tumor cells or ctDNA, which might be positively related to TNM stage or time of tumor growth or development, could not be eradicated by surgery and might respond to systematic therapy.
There are a few limitations in this pooled analysis. Firstly, several of the included studies were retrospective in design, and some characteristics, including the use of chemotherapy, were therefore not balanced. However, the slow processes of recruitment and follow-up in clinical trials mean that the survival results of currently ongoing trials will not be available for several years, and a comprehensive meta-analysis of currently available data was therefore urgently required. Secondly, there was significant heterogeneity among the studies in terms of the outcomes assessed, though we used random-effects models and sensitivity analyses to attempt to control for this heterogeneity. Thirdly, the current study was not based on individual patient’s data and it was therefore hard to analyze the influence of NSCLC stage accurately, and to evaluate the differences in beneficial effects among each subtype of EGFR mutations such as the exon 19 deletion, exon 21 L858R point mutation, and other uncommon mutations. We attempted to determine the impact of cancer stage by dividing the studies into groups according to the percentage of patients with a certain stage. Despite these limitations, the results of the current study have significant implications for future research and the management of NSCLC patients, especially patients with early-stage NSCLC.
Conclusion
This meta-analysis indicated that postoperative adjuvant EGFR-TKI treatment may provide significant benefits in terms of DFS and OS in patients with EGFR-mutated NSCLC, especially those with regional lymph node metastasis (N1 and N2), but may not be beneficial in patients with stage I NSCLC.
Abbreviations
ctDNA, circulating tumor DNA; DFS, disease-free survival; NSCLC, non-small-cell lung cancer; OS, overall survival; RCS, retrospective cohort study; RCT, randomized controlled trial; TKI, tyrosine kinase inhibitor.
Data sharing statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
This work was supported by the Dean Research Funding of Nanfang Hospital, Southern Medical University, China (2016B018). The funding bodies had no role in the design of the study, in collection, analysis, and interpretation of data, and in writing the manuscript. The abstract of this paper was presented at the 2018 ASCO Annual Meeting on June 1–5, 2018 (“Effects of TKI on Patients with Non-small Cell Lung Cancer of Different Stages: A Meta-analysis)”, as an online publication. The online publication’s abstract was published in “Meeting Abstracts” in the Journal of Clinical Oncology titled “Effects of TKI on patients with non-small cell lung cancer of different stages: a meta-analysis” (DOI: 10.1200/JCO.2018.36.15_suppl.e20503).
Disclosure
The authors report no conflicts of interest in this work.
References
Burdett S, Pignon JP, Tierney J, et al. Adjuvant chemotherapy for resected early-stage non-small cell lung cancer. Cochrane Database Syst Rev. 2015;7(Suppl):CD011430. | ||
Goldstraw P, Crowley J, Chansky K, et al. The IASLC lung cancer staging project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM classification of malignant tumours. J Thorac Oncol. 2007;2(8):706–714. | ||
Arriagada R, Bergman B, Dunant A, et al. Cisplatin-based adjuvant chemotherapy in patients with completely resected non-small-cell lung cancer. N Engl J Med. 2004;350(4):351–360. | ||
Winton T, Livingston R, Johnson D, et al. Vinorelbine plus cisplatin vs. observation in resected non-small-cell lung cancer. N Engl J Med. 2005;352(25):2589–2597. | ||
Douillard J-Y, Rosell R, de Lena M, et al. Adjuvant vinorelbine plus cisplatin versus observation in patients with completely resected stage IB-IIIA non-small-cell lung cancer (Adjuvant Navelbine International Trialist Association [ANITA]): a randomised controlled trial. Lancet Oncol. 2006;7(9):719–727. | ||
Mok TS, Wu Y-L, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–957. | ||
Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362(25):2380–2388. | ||
Mitsudomi T, Morita S, Yatabe Y, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11(2):121–128. | ||
Zhou C, Wu Y-L, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (optimal, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12(8):735–742. | ||
Han J-Y, Park K, Kim S-W, et al. First-SIGNAL: first-line single-agent Iressa versus gemcitabine and cisplatin trial in never-smokers with adenocarcinoma of the lung. J Clin Oncol. 2012;30(10):1122–1128. | ||
Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13(3):239–246. | ||
Wu Y-L, Zhou C, Hu C-P, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15(2):213–222. | ||
Yang JC, Wu Y-L, Schuler M, et al. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol. 2015;16(2):141–151. | ||
Goss GD, O’Callaghan C, Lorimer I, et al. Gefitinib versus placebo in completely resected non-small-cell lung cancer: results of the NCIC CTG BR19 study. J Clin Oncol. 2013;31(27):3320–3326. | ||
Kelly K, Altorki NK, Eberhardt WEE, et al. Adjuvant erlotinib versus placebo in patients with stage IB-IIIA non-small-cell lung cancer (radiant): a randomized, double-blind, phase III trial. J Clin Oncol. 2015;33(34):4007–4014. | ||
WuYL, Zhong W, Wang Q, et al. Gefitinib (G) versus vinorelbine+cisplatin (VP) as adjuvant treatment in stage IIIIIA (N1-N2) non-small-cell lung cancer (NSCLC) with EGFR-activating mutation (adjuvant): a randomized, phase III trial (CTONG 1104). J Clin Oncol. 2017;35(15):8500. | ||
Yue D, Xu S, Wang Q, et al. Erlotinib versus vinorelbine plus cisplatin as adjuvant therapy in Chinese patients with stage IIIA EGFR mutation-positive non-small-cell lung cancer (Evan): a randomised, open-label, phase 2 trial. Lancet Respir Med. 2018;6(11):863–873. | ||
Feng S, Wang Y, Cai K, et al. Randomized adjuvant chemotherapy of EGFR-mutated non-small cell lung cancer patients with or without Icotinib consolidation therapy. PLoS One. 2015;10(10):e0140794. | ||
Lv C, An C, Feng Q, et al. A retrospective study of stage I to IIIA lung adenocarcinoma after resection: what is the optimal adjuvant modality for patients with an EGFR mutation? Clin Lung Cancer. 2015;16(6):e173–e181. | ||
Neal JW, Na P, Govindan R, et al. The select study: a multicenter phase II trial of adjuvant erlotinib in resected epidermal growth factor receptor (EGFR) mutation-positive non-small cell lung cancer (NSCLC). J Clin Oncol. 2012;30(15_suppl):7010. | ||
Lu D, Nie X, Wan J, et al. Is off-pump coronary artery bypass grafting superior to drug-eluting stents for the treatment of coronary artery disease? A meta-analysis of randomized and nonrandomized studies. Int J Cardiol. 2014;174(3):640–653. | ||
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–605. | ||
Higgins JPT, Green S; Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Hoboken, NJ: Wiley-Blackwell; 2008. | ||
Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 2007;8:16. | ||
Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17(24):2815–2834. | ||
Zhong W-Z, Wang Q, Mao W-M, et al. Gefitinib versus vinorelbine plus cisplatin as adjuvant treatment for stage II-IIIA (N1-N2) EGFR-mutant NSCLC (ADJUVANT/CTONG1104): a randomised, open-label, phase 3 study. Lancet Oncol. 2018;19(1):139–148. | ||
Li N, Ou W, Ye X, et al. Pemetrexed-carboplatin adjuvant chemotherapy with or without gefitinib in resected stage IIIA-N2 non-small cell lung cancer harbouring EGFR mutations: a randomized, phase II study. Ann Surg Oncol. 2014;21(6):2091–2096. | ||
D’Angelo SP, Janjigian YY, Ahye N, et al. Distinct clinical course of EGFR -Mutant resected lung cancers: results of testing of 1118 surgical specimens and effects of adjuvant gefitinib and erlotinib. J Thorac Oncol. 2012;7(12):1815–1822. | ||
Janjigian YY, Park BJ, Zakowski MF, et al. Impact on disease-free survival of adjuvant erlotinib or gefitinib in patients with resected lung adenocarcinomas that harbor EGFR mutations. J Thorac Oncol. 2011;6(3):569–575. | ||
Yuan Y, Huang Q, Gu C, Chen H. Disease-free survival improved by use of adjuvant EGFR tyrosine kinase inhibitors in resectable non-small cell lung cancer: an updated meta-analysis. J Thorac Dis. 2017;9(12):5314–5321. | ||
Huang Q, Li J, Sun Y, Wang R, Cheng X, Chen H. Efficacy of EGFR tyrosine kinase inhibitors in the adjuvant treatment for operable non-small cell lung cancer by a meta-analysis. Chest. 2016;149(6):1384–1392. | ||
He J, Shen J, Yang C, et al. Adjuvant chemotherapy for the completely resected stage IB nonsmall cell lung cancer: a systematic review and meta-analysis. Medicine. 2015;94(22):e903. | ||
Strauss GM, Herndon JE, Maddaus MA, et al. Adjuvant paclitaxel plus carboplatin compared with observation in stage IB non-small-cell lung cancer: CALGB 9633 with the cancer and leukemia group B, radiation therapy Oncology group, and North Central cancer Treatment Group study groups. J Clin Oncol. 2008;26(31):5043–5051. | ||
Woodard GA, Wang SX, Kratz JR, et al. Adjuvant chemotherapy guided by molecular profiling and improved outcomes in early stage, non-small-cell lung cancer. Clin Lung Cancer. 2018;19(1):58–64. | ||
Agarwal M, Brahmanday G, Chmielewski GW, Welsh RJ, Ravikrishnan KP. Age, tumor size, type of surgery, and gender predict survival in early stage (stage I and II) non-small cell lung cancer after surgical resection. Lung Cancer. 2010;68(3):398–402. | ||
Kris MG, Gaspar LE, Chaft JE, et al. Adjuvant systemic therapy and adjuvant radiation therapy for stage I to IIIA completely resected non-small-cell lung cancers: american Society of clinical Oncology/Cancer care Ontario clinical practice guideline update. J Clin Oncol. 2017;35(25):2960–2974. | ||
Nygaard AD, Holdgaard PC, Spindler K-LG, Pallisgaard N, Jakobsen A. The correlation between cell-free DNA and tumour burden was estimated by PET/CT in patients with advanced NSCLC. Br J Cancer. 2014;110(2):363–368. | ||
Alegre E, Fusco JP, Restituto P, et al. Total and mutated EGFR quantification in cell-free DNA from non-small cell lung cancer patients detects tumor heterogeneity and presents prognostic value. Tumour Biol. 2016;37(10):13687–13694. | ||
Xm Y, Yc W, Liu X, et al. Cell-free RNA content in peripheral blood as potential biomarkers for detecting circulating tumor cells in non-small cell lung carcinoma. Int J Mol Sci. 2016;17(11):E1845. | ||
Wei Z, Wang W, Shu Z, Zhou X, Zhang Y. Correlation between circulating tumor DNA levels and response to tyrosine kinase inhibitors (TKI) treatment in non-small cell lung cancer. Med Sci Monit. 2017;23:3627–3634. | ||
Lee Y, Park S, Kim WS. et al. Correlation between progression-free survival, tumor burden, and circulating tumor DNA in the initial diagnosis of advanced-stage EGFR -mutated non-small cell lung cancer. Thorac Cancer. 2018;9(9):1104–1110. | ||
Zhong W-Z, Zhai H-R, Wu Y-L. Clinical trials in lung cancer surgery and research cooperation. Chin Clin Oncol. 2014;3(4):46. |
Supplementary materials
  | Figure S1 Risk-of-bias graph and summary for the included randomized control trials. |
  | Table S1 Newcastle–Ottawa scale for quality assessment of non-randomized cohort studies |
References
Feng S, Wang Y, Cai K, et al. Randomized adjuvant chemotherapy of EGFR-mutated non-small cell lung cancer patients with or without Icotinib consolidation therapy. PLoS One. 2015;10(10):e0140794 | ||
Goss GD, O’Callaghan C, Lorimer I, et al. Gefitinib versus placebo in completely resected non-small-cell lung cancer: results of the NCIC CTG BR19 study. J Clin Oncol. 2013;31(27):3320–3326. | ||
Kelly K, Altorki NK, Eberhardt WEE, et al. Adjuvant erlotinib versus placebo in patients with stage IB-IIIA non-small-cell lung cancer (radiant): a randomized, double-blind, phase III trial. J Clin Oncol. 2015;33(34):4007–4014. | ||
Li N, Ou W, Ye X, et al. Pemetrexed-carboplatin adjuvant chemotherapy with or without gefitinib in resected stage IIIA-N2 non-small cell lung cancer harbouring EGFR mutations: a randomized, phase II study. Ann Surg Oncol. 2014;21(6):2091–2096 | ||
Wu YL, Zhong W, Wang Q, et al. Gefitinib (G) versus vinorelbine+cisplatin (VP) as adjuvant treatment in stage IIIIIA (N1-N2) non-small-cell lung cancer (NSCLC) with EGFR-activating mutation (adjuvant): a randomized, phase III trial (CTONG 1104). J Clin Oncol. 2017;35(15):8500. | ||
Yue D, Xu S, Wang Q, et al. Erlotinib versus vinorelbine plus cisplatin as adjuvant therapy in Chinese patients with stage IIIA EGFR mutationpositive non-small-cell lung cancer (Evan): a randomised, open-label, phase 2 trial. Lancet Respir Med. 2018;6(11):863–873. | ||
D’Angelo SP, Janjigian YY, Ahye N, et al. Distinct clinical course of EGFR -Mutant resected lung cancers: results of testing of 1118 surgical specimens and effects of adjuvant gefitinib and erlotinib. J Thorac Oncol. 2012;7(12):1815–1822. | ||
Janjigian YY, Park BJ, Zakowski MF, et al. Impact on disease-free survival of adjuvant erlotinib or gefitinib in patients with resected lung adenocarcinomas that harbor EGFR mutations. J Thorac Oncol. 2011;6(3):569–575. | ||
Lv C, An C, Feng Q, et al. A retrospective study of stage I to IIIA lung adenocarcinoma after resection: what is the optimal adjuvant modality for patients with an EGFR mutation? Clin Lung Cancer. 2015;16(6):e173–e181. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.