Back to Journals » International Journal of Women's Health » Volume 14
Differential Diagnosis of Uterine Leiomyoma Torsion Mimicking Ovarian Torsion in a Second Trimester of Pregnancy: A Case Report
Received 9 August 2022
Accepted for publication 13 December 2022
Published 21 December 2022 Volume 2022:14 Pages 1777—1782
DOI https://doi.org/10.2147/IJWH.S385321
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Hee Jeong Kim,1,* Jisun Lee,1,2,* Hyun Jung Lee1,2
1Department of Obstetrics and Gynecology, Kyungpook National University Hospital, Daegu, Republic of Korea; 2Department of Obstetrics and Gynecology, School of Medicine, Kyungpook National University, Daegu, Republic of Korea
*These authors contributed equally to this work
Correspondence: Hyun Jung Lee, Department of Obstetrics and Gynecology, School of Medicine, Kyungpook National University, Daegu, Republic of Korea, Tel +821035328741, Fax +82534237905, Email [email protected]
Abstract: In patients with acute abdomen, especially during pregnancy, it is difficult to suspect myoma torsion initially due to its rarity. However, when these patients have a solid mass in the pelvis, torsion of uterine fibroids or adnexa and large infarct inside leiomyoma are the main diagnoses that must be differentiated. We report a case of uterine myoma torsion mimicking ovarian torsion in the second trimester of pregnancy that was successfully managed by laparoscopic myomectomy. A 31-year-old pregnant woman with severe right lower abdominal pain at 21 + 2 weeks of gestation was transferred. On ultrasonography, the appendix appeared normal but a solid mass (7.0× 4.0 cm) containing a cystic portion was observed on the right side of the uterus. The mass had no blood flow and tenderness appeared on the transducer pressure. Pelvic magnetic resonance imaging revealed a 7 cm edematous mass with low signal intensity on T2-weighted image, instead of a normal-looking right ovary. These findings led to suspicion of right ovarian torsion. One day after admission, the patient’s symptoms worsened with acute elevation in C-reactive protein (CRP) (4.55 mg/dL) and neutrophile-to-lymphocyte ratio (NLR) (10.1), despite the use of analgesics and tocolytics, and uterine contractions were not controlled. Emergency surgery was performed, and the final diagnosis was a uterine leiomyoma torsion. Laparoscopic myomectomy was successfully performed, and symptoms were relieved after operation. She had full term vaginal delivery without complication. The differential diagnosis between myoma torsion and ovarian torsion is challenging in patients with acute abdomen during pregnancy. To exclude ovarian torsion, a comparison with an asymptomatic contralateral normal ovary will be very helpful. When fibroids are found in mothers with an acute abdomen, follow-up of NLR and CRP is related to preterm labor and can be a reference point for considering surgery.
Keywords: ovarian torsion, leiomyoma, pregnancy, laparoscopy, myomectomy
Introduction
Diagnosis of acute abdomen during pregnancy can be complicated by alterations in the clinical presentation due to the anatomical and physiological changes associated with pregnancy and the reluctance to use certain radiologic tools for fear of harm to the fetus. However, delays in diagnosis and treatment can lead to adverse outcomes in the mother and fetus.1 Ultrasonography (USG) is usually considered the first-line imaging modality for evaluating acute abdomen in pregnant women because of its availability, portability, high sensitivity and specificity without ionizing radiation.2 When an acute abdomen is associated with a pelvic mass at the side of the uterus, adnexal torsion and massive infarction or torsion of a leiomyoma are the main diagnoses to be differentiated. The identification of a normal adnexa using imaging modalities can easily exclude the presence of adnexal torsion. However, if a normal ovary is not observed, the diagnosis can be very confusing. Pedunculated leiomyomas may simulate an adnexal mass, especially if the connecting stalk of the tissue and ipsilateral normal ovary are not visualized on imaging. Due to its rarity, it is difficult to initially suspect myoma torsion. Here, we present the case of a patient with pedunculated myoma torsion who was successfully treated with laparoscopic myomectomy in the second trimester of pregnancy.
Case Presentation
A 31-year-old pregnant woman with severe right lower abdominal pain at 21 + 2 weeks’ gestation was transferred to the emergency room. Her pain began three days before the visit and was accompanied by vomiting and diarrhea. She had a history of hydatidiform mole and ectopic pregnancy, and due to infertility, she became pregnant through in vitro fertilization (IVF) and embryo transfer (ET). Before the onset of the pain, her pregnancy had been uneventful. On physical examination, vital signs were normal, and she had right-lower quadrant pain and tenderness with palpable uterine contractions. A non-stress test revealed regular uterine contractions (10 contractions in 20 min). The amniotic fluid was normal, and fetal well-being was conserved (fetal heart rate, 152 beats per minute: fetal weight, 404 g).
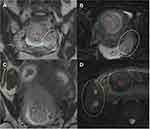
The first impression was acute appendicitis; however, transabdominal ultrasonography (USG) revealed a normal appendix. The USG revealed a solid mass (7.0 × 4.0 cm) containing a cystic portion suspected of being a follicle on the right side of the uterus and the left ovary appeared normal. The mass considered as an enlarged right ovary was characterized by central edema and peripherally displaced follicles (Figure 1A). There was no blood flow in the mass (Figure 1B) and tenderness appeared on the transducer pressure. Pelvic magnetic resonance imaging (MRI) revealed an intrauterine pregnancy and 5 cm sized normal-looking left ovary (Figure 2A and B). Instead of the normal right ovary, a 7 cm edematous mass with low signal intensity was observed on the right lateral side of the uterus on T2-weighted imaging, suggesting right ovarian torsion (Figure 2C and D). Furthermore, the patient had a history of IVF-ET, which could be a risk factor for normal ovarian torsion due to enlarged ovary related with hyperstimulation. These findings led to suspicion of right ovarian torsion. While a pedunculated fibroid was listed as a possible diagnosis, no stalk with uterus was visualized and there was no history of myomas during the antenatal period.
 |
Figure 1 Ultrasonography revealed a solid mass (7.0 cm × 4.0 cm) containing cystic portion (A) without blood flow (B). |
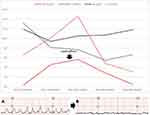
Initial laboratory studies (Day 1 of admission) revealed elevated levels of white blood cell counts (WBCs) (13.2x103/µL), segmented neutrophils (81.6%), neutrophile-to-lymphocyte ratio (NLR) (6.6), but C-reactive protein (CRP) (0.28 mg/dL) was within normal range. One day after admission (Day 2 of admission), the patient’s symptoms worsened with acute elevation in CRP (4.55 mg/dL) and NLR (10.1) (Figure 3), despite the use of analgesics, antibiotics and tocolytics, and uterine contractions were not controlled (Figure 3A). Emergent laparoscopic surgery was planned at 21 + 3 weeks of gestation (Day 2 of admission). After general anesthesia, a multichannel single-port laparoscopic trocar (Uni-portTM, Dalim, Seoul, Korea) was inserted through the patient’s umbilicus, and an additional trocar was placed horizontally on the left side of the umbilicus. A 25 to 30 mm long vertical incision was made on the umbilicus, extending to the peritoneum. The abdominal wall was elevated using Army-Navy retractors inserted into the incision opening. A wound retractor was inserted into the covering of the peritoneal cavity from the skin to the peritoneum, and the port cap was fixed to the wound retractor. The pressure of the pneumoperitoneum was maintained at 12 mmHg. A second trocar was inserted for the laparoscopic fan retractor to push the uterus to the left without traumatizing the uterus. Contrary to expectations, during laparoscopy, a pedunculated subserosal myoma was revealed in the torsion state with complete necrosis on the right side of the uterus (Figure 4A). Myomectomy was performed using LigaSure™ (Medtronic, Dublin, Ireland), a 5-mm blunt-tip piece. Bleeding control was performed using bipolar cautery. The myoma was pedunculated and subserosal myoma. The dissected myoma was removed through the umbilical port by the in-bag hand morcellation method. The pathologic diagnosis was uterine myoma with infarction. Hematoxylin and eosin stain of specimen showed well demarcated spindle cell tumor with infarction and hemorrhage (Figure 4B). After laparoscopic myomectomy, her laboratory results were improved, and her abdominal pain and uterine contraction disappeared (Figure 3B). Following discharge, the patient underwent routine obstetric evaluation. She had full term vaginal delivery without complication. Writing and publishing this case report was approved by institutional review board of Kyungpook National University Hospital (IRB file No. 2022–07-003). Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Discussion
Acute abdominal pain during pregnancy could be occurred due to obstetric as well as non-obstetric causes. In right lower quadrant of abdomen, cecum, appendix, ascending colon, terminal ileum, lower ureter, urinary bladder, right ovary and adnexa and uterus are located.1 Therefore, as non-obstetric etiologies of acute pain in right lower quadrant of abdomen, gastrointestinal disorder such as appendicitis, urinary stone, uterine myoma degeneration or torsion, and right adnexal torsion should be considered. As obstetric causes of acute abdomen are ectopic pregnancy, abruption, uterine rupture and abdominal pregnancy.
Uterine leiomyoma is the most common benign gynecological tumor, but it has been known to be relatively rare with an estimated incidence rate of 0.1% to 3.9% during pregnancy, and most cases are asymptomatic.3,4 Therefore, in the case of acute abdominal pain during pregnancy, it is difficult to suspect that subserosal leiomyoma torsion is the main cause.5,6 The torsion of pedunculated leiomyomas requires emergency surgery because if left untreated, it can lead to acute abdomen due to myoma necrosis, infection, resultant inflammatory peritoneal reaction, and peritonitis, requiring a precise and prompt diagnosis to avoid significant morbidity caused by the progression of the condition to tissue necrosis.3,7 Due to its high diagnostic accuracy without ionizing radiation, ultrasonography (USG) is the first-line imaging modality for pelvic organ examination as well as for acute abdominal diagnosis such as appendicitis and cholecystitis in pregnant women.2 In patients with acute abdomen, adnexal torsion should be considered first when pelvic lesions on the lateral side of the uterus are involved, and the identification of normal adnexa using imaging modalities can easily rule out the presence of adnexal torsion. USG was reported to have a high diagnostic rate, with an overall accuracy of 96.0%, a sensitivity of 72.1%, and a specificity of 99.6% in the diagnosis of ovarian torsion.8 However, as in our patient, if the ipsilateral ovary with the pain location was not found, the differential diagnosis between ovarian torsion and myoma torsion would be difficult. The most common finding in ovarian torsion is unilateral ovarian enlargement (>4 cm). Other findings suggestive of ovarian torsion are interrupted blood flow, decreased echogenicity of the stroma centrally secondary to edema, and the peripheral arrangement of follicles.9 In our case, a normal ovary was not seen, and the mass looked very similar to the ovary, showing enlargement (7 cm) and a peripheral cyst considered as follicle; therefore, ovarian torsion was suspected first. However, it should be noted that there was no significant ovarian enlargement compared to the contralateral normal ovary (5 cm), considering that the normal ovary may have been enlarged by hyperstimulation due to the history of IVF-ET. The computed tomography and MRI findings of ovarian torsion are nonspecific. MRI are useful imaging modalities in cases of myoma torsion during pregnancy; however, in acute situations, they may unnecessarily delay the management of the condition.
Pregnant women with fibroids are significantly more likely to develop preterm labor and to deliver preterm than women without fibroids. However, the confirmation of myoma alone cannot provide evidence for surgery to remove the myoma. In this case, CRP and NLR were monitored together with labor pain, and the medical staff decided to operate when the NLR exceeded upper limit of normal range. To the best of our knowledge, there is no report using NLR to monitor the course of myoma torsion during pregnancy. Immediately after surgery, NLR and CRP decreased rapidly, and pain associated with preterm labor was not observed.
Open surgery is the preferred treatment modality for pregnant women. However, over the years, various studies have shown an increasing trend towards the acceptance of laparoscopy as a feasible, safe, and effective therapeutic option during pregnancy. Laparoscopic myomectomy has recently evolved as a feasible and minimally invasive surgical option to manage acute leiomyoma torsion, replacing the traditional open approach.10–12 We used a multichannel, single-port laparoscopic trocar as the primary port, which has several advantages. First, it requires an open technique for inserting the primary trocar, so that the surgeon can avoid uterine injury during blind insertion of the trocar and adjust the insertion site according to the height of the uterus. Second, it is convenient to remove the specimen by in-bag manual morcellation through a 25–30-mm relatively long trans-umbilical incision and avoids the dissemination of mass particles. In addition, the multichannel port reduces the number of trocars required, resulting in cosmetic advantages and pain reduction.
Conclusions
In summary, the authors presented a pregnant woman with acute abdomen, confirmed as myoma torsion. To exclude ovarian torsion, a comparison with an asymptomatic contralateral normal ovary would be very helpful. If the mass resembles an ovary without significant ovarian enlargement compared to the contralateral normal ovary, a diagnosis of myoma torsion must still be considered. Although it is supported by imaging, there are limitations in differential diagnosis due to diagnostic limitations due to pregnancy and imaging similarity between cystic degeneration of myoma and ovary follicle. In this case, it was necessary to consider NLR and CRP to consider surgical indications. In some cases of subserosal fibroids that induce preterm pain, laparoscopic myomectomy using manual excision in the bag may be a feasible and safe minimally invasive surgical option.
Abbreviations
MRI, magnetic resonance imaging; CRP, C-reactive protein; NLR, neutrophile-to-lymphocyte ratio; IVF, in vitro fertilization; ET, embryo transfer; USG, ultrasonography; WBCs, white blood cell counts.
Ethical Approval
Ethical approval was granted by institutional review board of Kyungpook National University Hospital (IRB file No. 2022-07-003).
Declaration of Patient Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Hee Jeong Kim, Jisun Lee are co-first authors for this study. The authors report no conflicts of interest in this work.
References
1. Zachariah SK, Fenn M, Jacob K, Arthungal SA, Zachariah SA. Management of acute abdomen in pregnancy: current perspectives. Int J Womens Health. 2019;11:119–134. doi:10.2147/IJWH.S151501
2. Lee HJ, Norwitz ER, Shaw J. Contemporary management of fibroids in pregnancy. Rev Obstet Gynecol. 2010;3(1):20–27.
3. Basso A, Catalano MR, Loverro G, et al. Uterine fibroid torsion during pregnancy: a case of laparotomic myomectomy at 18 weeks’ gestation with systematic review of the literature. Case Rep Obstet Gynecol. 2017;2017:4970802. doi:10.1155/2017/4970802
4. Vitale SG, Tropea A, Rossetti D, Carnelli M, Cianci A. Management of uterine leiomyomas in pregnancy: review of literature. Updates Surg. 2013;65(3):179–182. doi:10.1007/s13304-013-0198-z
5. Cerdeira AS, Tome M, Moore N, Lim L. Seeing red degeneration in uterine fibroids in pregnancy: proceed with caution. Lancet. 2019;394:10212. doi:10.1016/S0140-6736(19)32322-0
6. Gupta S, Manyonda IT. Acute complications of fibroids. Best Pract Res Clin Obstet Gynaecol. 2009;23(5):609–617. doi:10.1016/j.bpobgyn.2009.01.012
7. Roy C, Bierry G, El Ghali S, Buy X, Rossini A. Acute torsion of uterine leiomyoma: CT features. Abdom Imaging. 2005;30(1):120–123. doi:10.1007/s00261-004-0240-1
8. Rostamzadeh A, Mirfendereski S, Rezaie MJ, Rezaei S. Diagnostic efficacy of sonography for diagnosis of ovarian torsion. Pak J Med Sci. 2014;30(2):413–416.
9. Chang HC, Bhatt S, Dogra VS. Pearls and pitfalls in diagnosis of ovarian torsion. Radiographics. 2008;28(5):1355–1368. doi:10.1148/rg.285075130
10. Currie A, Bradley E, McEwen M, Al-Shabibi N, Willson PD. Laparoscopic approach to fibroid torsion presenting as an acute abdomen in pregnancy. JSLS. 2013;17(4):665–667. doi:10.4293/108680813X13794522666400
11. Kosmidis C, Pantos G, Efthimiadis C, Gkoutziomitrou I, Georgakoudi E, Anthimidis G. Laparoscopic excision of a pedunculated uterine leiomyoma in torsion as a cause of acute abdomen at 10 weeks of pregnancy. Am J Case Rep. 2015;16:505–508. doi:10.12659/AJCR.893382
12. Tsai YJ, Yeat SK, Jeng CJ, Chen SC. Torsion of a uterine leiomyoma. Taiwan J Obstet Gynecol. 2006;45(4):333–335. doi:10.1016/S1028-4559(09)60254-0
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.