Back to Journals » Psychology Research and Behavior Management » Volume 16
Differences in Fertility-Related Quality of Life and Emotional Status Among Women Undergoing Different IVF Treatment Cycles
Authors Ni Y, Shen H, Yao H, Zhang E, Tong C, Qian W, Huang L, Wu X, Feng Q
Received 9 March 2023
Accepted for publication 18 May 2023
Published 22 May 2023 Volume 2023:16 Pages 1873—1882
DOI https://doi.org/10.2147/PRBM.S411740
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Ying Ni,1,2,* Hao Shen,1,2,* Haihui Yao,3,* Enming Zhang,4 Chenye Tong,1 Wen Qian,1 Limin Huang,1 Xian Wu,1 Qing Feng2
1Department of Gynecology and Obstetrics, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 2Department of Nursing, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 3Xianda College of Economics and Humanities, Shanghai International Studies University, Shanghai, People’s Republic of China; 4School of Nursing, Shanghai Jiao Tong University, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qing Feng, Department of Nursing, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China, Email [email protected] Xian Wu, Department of Gynecology and Obstetrics, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China, Email [email protected]
Objective: The present study aimed to provide more insight into the possible differences in the fertility-related quality of life (FertiQoL) and emotional status of women undergoing different cycles of in vitro fertilization (IVF) treatments.
Methods: A prospective cohort study was performed, and a total of 432 women undergoing IVF treatment were recruited. FertiQoL scale, self-rating anxiety scale (SAS), self-rating depression scale (SDS), and perceived social support scale (PSSS) were used to analyze fertility-related QoL and emotional status. Data were analyzed comparing women undergoing different cycles of IVF treatments.
Results: A significant decrease in FertiQoL scores occurred in women with increased cycles of IVF treatment. Both anxiety and depression scores significantly increased with increased cycles of attempting IVF treatment. There was no significant difference detected in perceived social support among groups.
Conclusion: With the increase in the number of IVF treatment cycles, women’s FertiQoL gradually decreased, while the risk of anxiety and depression gradually increased.
Keywords: infertility, quality of life, emotional problems, IVF, treatment failure
Introduction
Infertility is defined as “a reproductive disorder, which is defined as failure to achieve a clinical pregnancy after 12 months or more of unprotected regular sexual intercourse” by the World Health Organization (WHO),1 and it is estimated that approximately 8–12%2 of couples worldwide suffer from infertility. In vitro fertilization (IVF) is one of the most important and final steps of assisted reproductive therapy for infertility, and it has brought hope to many infertile families. Although infertility treatment has achieved success in a considerable percentage of cases,3 it usually has a negative impact on the quality of life (QoL) of patients.
Along with treatment, infertility is one of the biggest stressors in life4 and leads to various physiological, psychological and social consequences, which may have a significant impact on the fertility-related quality of life (FertiQoL) of patients.5–7 The WHO defines QoL as individuals’ perception of their living status in the cultural background and value system of their lives.8 Therefore, FertiQoL refers to individuals’ quality of life in relation to emotional, physical, psychological, marital, social, environmental, and tolerance issues due to fertility problems,9 and it broadly reflects the life status of infertile patients during infertility.
Numerous studies have shown that the FertiQoL of women during infertility is worse than that of women during childbearing.10–12 Women also need to frequently undergo many invasive surgeries and monitor their menstrual cycle daily compared to male spouses. In traditional Chinese culture, women experience the main pressures of infertility. As a result, women experience increased suffering and their FertiQoL is significantly decreased when faced with an infertility crisis.13,14
Assisted reproductive treatments involve a complex and demanding regimen, and the clinical pregnancy rate in each treatment cycle ranges between 28.8% and 33.2%.3 Therefore, to achieve pregnancy, repeated cycles of treatment are usually necessary, and approximately 25% of infertile patients even experienced more than five cycles.15 However, some literature has shown that repeated IVF cycles may significantly increase the risk of ovarian hyperstimulation syndrome, oestrogen-dependent tumors and premature delivery.16–18
Evidence shows that patients who experience repeated IVF failure are more prone to poorer QoL, partly because of the longer duration of conception delay and partly because of the increased IVF medical, emotional and financial burden.19 Our previous study revealed that women with repeated implantation failure had significantly lower levels of FertiQoL, and anxiety and depression were negatively correlated with FertiQoL.20
In addition, some studies have shown that a history of IVF treatment failure may negatively affect women’s emotional health, leading to deterioration of mental health,21 depression,22,23 and anxiety.24,25 These alterations still exist several months after the end of the medical procedure,22 especially in patients with one or more treatment failures. A previous study26 has compared psychological stress in women with different IVF cycles and found that women with repeated treatment failures had significantly higher levels of psychological stress. However, a pilot study27 from Stanford University School of Medicine reported no difference in anxiety and perceived stress among patients with first-time and repeated IVF cycles. A previous study from Turkey28 conducted a survey among infertile couples with and without a history of IVF failure and found that the FertiQoL, anxiety, and depression did not significantly differ. This may be related to the limited sample size of these two studies. Therefore, future studies with different cultural contexts and larger sample sizes are required.
Social support may be a key component in a woman’s coping with pain related to infertility and treatment failure.29–31 Social support is often defined as the comfort, care, help, and respect one gets from others, and is an available external resource when an individual is under stress.32,33 Social support makes the individual feel cared for and accepted,34 and it helps reduce individuals’ perceived stress, mitigate the impact of negative emotions, and improve QoL.35 A previous study on the social support of infertile couples has shown that women tend to disclose their infertility to others and are more inclined than men to seek dialogue with relatives and friends.29 Another study has also reported that more disclosure by women may be associated with higher levels of distress.36 Therefore, several authors have claimed that social support should be a variable in studies focusing on women faced with infertility.37
Based on these findings, more specific and definitive studies are needed to explore the differences in emotional status and fertility-related QoL among women undergoing first-time and repeated IVF cycles. Furthermore, it is unclear whether the impact of IVF failure is incremental with increasing cycles of IVF treatment. As far as we know, this is the first exploration undertaken in this respect. Therefore, the purpose of the present study was to provide more insight into the possible differences in the levels of fertility-related quality of life and emotional status of women undergoing different number of attempted cycles of IVF treatment.
Methods
Data and Study Design
The present study was a prospective cohort study performed in the Reproductive Medical Center of Ruijin Hospital in China. Women undergoing IVF treatments at the medical center were recruited from March to June 2021. Ethics approval was granted by the Ethics Committee of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine. Eligible participants included women who had not been affected by preexisting major diseases, had agreed to participate in the study, and were able to complete the survey. Exclusion criteria included women receiving eggs.
Participants were classified into four groups based on the number of attempting IVF cycles as follows: G1 (first cycle), G2 (second cycle), G3 (third cycle), and G4 (fourth and above cycle). The investigation was performed at the last follow-up before embryo transfer in a treatment cycle. After obtaining the written informed consent, the researcher distributed a self-report questionnaire to each eligible participant and collected clinical data from their medical records.
The final cohort consisted of 432 women as follows: 192 women in G1, 80 women in G2, 88 women in G3, and 72 women in G4. Figure 1 shows a flow diagram of the recruitment process.
 |
Figure 1 Flow diagram describing the recruitment process. |
Measures
The demographic characteristics and clinical information, including residence, occupation, education level, age, body mass index (BMI), attribution of infertility, and duration of infertility, were retrieved from medical records.
In the present study, fertility-related QoL was measured by the Chinese version of the fertility quality of life scale (FertiQoL).9 The FertiQoL scale is widely used and has good reliability, validity and sensitivity.7,38 The scale is composed of a core module and an optional treatment module. There are 36 items in total, including 2 independent items and 24 core items (such as emotional, mind-body, marital and social relationships) as well as 10 optional treatment items (such as tolerance and environment). The scale is scored with 5 grades, with each item scoring from 0 to 4. In the present study, the Cronbach’s alpha coefficient of the FertiQoL scale was 0.921.
Social support was assessed using the Chinese version of the Perceived Social Support Scale (PSSS).39 The PSSS scale consists of 12 self-rating items, which are rated on a 7-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree). Higher scores of each dimension and the overall level represent higher social support levels. The scale has been widely used and demonstrated to have good validity and reliability. In the present study, the Cronbach’s alpha coefficient of the PSSS scale was 0.941.
In the present study, the Chinese version of the Self-Rating Anxiety Scale (SAS)40 and the Self-Rating Depression Scale (SDS)41 were used to assess the levels of anxiety and depression. Both scales contain 20 items and are scored on a 4-point Likert scale, ranging from 1 (none or seldom) to 4 (most or all of the time). Higher scores indicate more serious anxiety or depression. In the present study, the Cronbach’s alpha coefficients of the SAS and SDS were 0.897 and 0.885, respectively.
Statistical Analysis
SPSS software version 23.0 was used to perform all statistical analyses. The measured data were expressed as the mean (M) and standard deviation (SD), and the counting data were presented as the frequency and composition ratio (%). Pearson’s chi-squared test and univariate analysis of variance (ANOVA) were performed to explore the differences in demographic characteristics, clinical characteristics, depression, anxiety, and social support among the groups. P<0.05 was considered statistically significant.
Results
In the present study, 432 women were included, and they were classified into the following four groups: women who were undergoing the first-time IVF cycle (G1; n=192), undergoing the second cycle (G2; n=80), undergoing the third cycle (G3; n=88), and undergoing the fourth or later cycle (G4; n=72). The average number of IVF cycles in G4 was 4.65, SD=0.87.
Table 1 shows the demographic and clinical characteristics of the women in the four groups. There were no significant differences detected among groups (p>0.05), except for age and infertility duration (p<0.001), with G4 women reporting a higher frequency of infertility duration of more than six years compared to the other groups.
 |
Table 1 Demographic Characteristics of Women Undergoing IVF |
The FertiQoL, PSSS, SAS, and SDS results for the four groups are shown in Table 2. The total FertiQoL score in all four groups was 64.43±11.19, and the scores of PSSS, SAS and SDS scores were 60.79±13.08, 49.24±10.31, and 52.48±10.50 respectively. Significant differences were found in FertiQoL, SAS, and SDS among the four groups (p<0.05). The total scores together with the core module scores of FertiQoL of women in G1 were the highest, and decreased progressively with increasing numbers of IVF treatment cycles. However, the treatment module scored the highest in G2, and then progressively decreased with increasing numbers of IVF treatment cycles (see Figure 2). The PSSS scores were generally higher in G3 than those in any other group (see Figure 3), but this difference was not statistically significant (p>0.05). However, the PSSS scores of the family and friend support domains in G3 were significantly higher than those in any other group (p<0.05). The SAS and SDS scores both increased with increasing numbers of IVF treatment cycles (see Figures 4 and 5).
 |
Table 2 FertiQoL, PSSS, SAS and SDS Scores of Women Undergoing IVF |
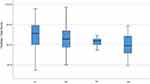 |
Figure 2 Box plot of fertility-related QoL levels for each group. |
 |
Figure 3 Box plot of social support levels for each group. |
 |
Figure 4 Box plot of anxiety levels for each group. |
 |
Figure 5 Box chart of depression levels for each group. |
Discussion
There is growing evidence that infertility is a significant psychological burden, as it may negatively impact the QoL as well as the emotional and social well-being of affected individuals or couples.42–46 Kahyaoglu et al demonstrated an inverse correlation of mind-body, tolerance, and total FertiQoL scores with the number of IVF failures in infertile women.47 Understanding whether there are specific differences in fertility-related QoL and emotional status is important for optimal support of infertile women during different IVF cycles. To the best of our knowledge, this is the first cohort study exploring the incremental impact of attempting IVF cycles on the levels of fertility-related QoL, social support, anxiety, and depression in a well-characterized population of women undergoing IVF treatment.
In the present study, the FertiQoL scores of women who had repeated IVF cycles were significantly lower than that of those who were undergoing IVF treatment for the first time, and they progressively decreased with increasing numbers of attempting cycles. This may partly be because of the longer duration of conception delay and partly because of the increased IVF medical, emotional and financial burden, which is consistent with other studies.20,24,35,48 Current data also reported that the treatment module scored the highest in women undergoing the second IVF attempt and then progressively decreased, which may be explained by the fact that women who underwent the second IVF cycle have become more familiar with the treatment process from the first cycle, or have a strong desire to have children, thereby increasing their tolerance for the treatment environment. However, this tolerance is also limited and fragile, and it may decrease due to another failure, which also explains why the treatment module scores decreased after the second cycle. A previous study from Turkey28 compared FertiQoL between women undergoing first-time and repeated IVF cycles, reporting no differences in total FertiQoL scores between the two groups, but the study demonstrated that the scores of treatment module in women with repeated cycles were significantly higher than those in women with first IVF cycle. We were unable to eliminate random factors that stem in part from the nature of such research. Additional multi-centered research with a larger sample size or an extended enrollment is expected to provide more evidence.
In the present study, the perceived social support of women undergoing different IVF cycles did not significantly differ, but was generally higher in women undergoing the third cycle, especially for family and friend support. This is somewhat similar to the treatment module of FertiQoL in the present study, and may be explained by the experience of unsuccessful treatment arousing more sympathy and support from family and friends, but as the failure continues, perceived social support declines accordingly. Thus, the continual failure of IVF cycles may also reduce the confidence and patience of the partners and family members, resulting in less support. Ching-Yu Cheng et al reported that the relationship between an infertile woman and her partner and family members may affect the woman’s psychological stress and QoL during assisted reproductive treatment.49 A study by Takaki and Hibino et al also indicated that the lack of family support of infertile women can result in stress and significantly increase their psychological pressure.50 In our previous study,35 social support was found positively correlated with FertiQoL. Adequate social support enables infertile women to obtain more emotional support and care, improving their QoL and ability to cope with psychological stress.
Moreover, the present study also revealed that women had more risk factors for developing emotional problems with increased IVF attempting cycles. The levels of anxiety and depression progressively increased with increasing numbers of IVF cycles, which was consistent with other studies.48,51 A study by Li et al52 found that the incidence of anxiety and depression was significantly higher among infertile couples with IVF treatment than among normal fertile couples. A previous study has reported that 11.8% of women exhibit depressive symptoms prior to IVF treatment and that this value increases to 25.4% after unsuccessful IVF attempts.53 These findings can be interpreted as the impact of cumulative trauma, which may be attributed to the interaction of many stress events, including infertility and long-term psychological and physical problems associated with repeated failures of IVF treatment. Women who have experienced more than one IVF cycle often suffer from the dual pressures of family and society, and they have a variety of psychological problems. Repeated IVF failure can easily lead to adverse psychological problems, such as anxiety and depression.54 Proper psychological care can help relieve tension, anxiety, and other negative emotions, as well as increase the success rate of assisted reproductive treatment.55 In line with this idea, Seyedi et al screened women undergoing IVF treatment and reported improvements in life satisfaction following positive psychotherapy for women presenting with mild to moderate depressive symptoms.56
Limitations
This study had several limitations. First, the present study focused on female partners only. Second, self-report questionnaires were used, which may have reflected subjective evaluations rather than diagnosis. Moreover, specific moments in the treatment cycle, such as ovarian stimulation and oocyte retrieval, may be closely related to the increase in depression and anxiety levels,57,58 which are not further distinguished in this study. Therefore, future research aimed at expanding the research results should take these limitations into account.
Conclusion
In summary, with the increase in the number of attempting cycles, women undergoing IVF treatment seem to have a progressively decreasing level of fertility-related quality of life and are at a progressively increasing risk of anxiety and depression. Therefore, current clinical practice should develop intervention and prevention programs in which the impact of IVF failure on women’s emotional experience in future IVF treatment cycles is taken into account, so as to help women develop realistic expectations of parenthood.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
All participants provided their informed written consent. The study was approved by the Ethics Committee of Shanghai Ruijin Hospital and was conducted in accordance with the principles of the Declaration of Helsinki.
Acknowledgment
The authors would like to thank all the participants who voluntarily participated in this study and research assistants who performed the data collection. Ying Ni, Hao Shen and Haihui Yao are co-first authors for this study.
Funding
Shanghai Jiao Tong University School of Medicine: Nursing Development Program.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Zegers-Hochschild F, Adamson GD, de Mouzon J, et al. International committee for monitoring assisted reproductive technology; world health organization. International committee for monitoring assisted reproductive technology (ICMART) and the world health organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92(5):1520–1524. PMID: 19828144. doi:10.1016/j.fertnstert.2009.09.009
2. Schmidt L, Holstein B, Christensen U, Boivin J. Does infertility cause marital benefit? An epidemiological study of 2250 women and men in fertility treatment. Patient Educ Couns. 2005;59(3):244–251. PMID: 16310331. doi:10.1016/j.pec.2005.07.015
3. Human Fertilisation and Embryology Authority. Fertility treatment in 2014 - trends and figures; 2016. Available from: https://www.hfea.gov.uk/media/1783/fertility-treatment-2014-trends-and-figures.pdf.
4. Omani-Samani R, Ghaheri A, Navid B, Sepidarkish M, Maroufizadeh S. Prevalence of generalized anxiety disorder and its related factors among infertile patients in Iran: a cross-sectional study. Health Qual Life Outcomes. 2018;16(1):129. PMID: 29914527; PMCID: PMC6006936. doi:10.1186/s12955-018-0956-1
5. Lakatos E, Szigeti JF, Ujma PP, Sexty R, Balog P. Anxiety and depression among infertile women: a cross-sectional survey from Hungary. BMC Womens Health. 2017;17(1):48. PMID: 28738833; PMCID: PMC5525318. doi:10.1186/s12905-017-0410-2
6. Jansen NA, Saint Onge JM. An internet forum analysis of stigma power perceptions among women seeking fertility treatment in the United States. Soc Sci Med. 2015;147:184–189. PMID: 26584236. doi:10.1016/j.socscimed.2015.11.002
7. Namavar Jahromi B, Mansouri M, Forouhari S, Poordast T, Salehi A. Quality of life and its influencing factors of couples referred to an infertility center in Shiraz, Iran. Int J Fertil Steril. 2018;11(4):293–297. PMID: 29043705; PMCID: PMC5641461. doi:10.22074/ijfs.2018.5123
8. Whoqol Group. The world health organization quality of life assessment (WHOQOL): position paper from the world health organization. Soc Sci Med. 1995;41(10):1403–1409. PMID: 8560308. doi:10.1016/0277-9536(95)00112-k
9. Boivin J, Takefman J, Braverman A. The fertility quality of life (FertiQoL) tool: development and general psychometric properties. Fertil Steril. 2011;96(2):409–415.e3. PMID: 21458806; PMCID: PMC7094343. doi:10.1016/j.fertnstert.2011.02.046
10. Namdar A, Naghizadeh MM, Zamani M, Yaghmaei F, Sameni MH. Quality of life and general health of infertile women. Health Qual Life Outcomes. 2017;15(1):139. PMID: 28701163; PMCID: PMC5508693. doi:10.1186/s12955-017-0712-y
11. Aduloju OP, Olaogun OD, Aduloju T. Quality of life in women of reproductive age: a comparative study of infertile and fertile women in a Nigerian tertiary centre. J Obstet Gynaecol. 2018;38(2):247–251. PMID: 28920515. doi:10.1080/01443615.2017.1347916
12. Masoumi SZ, Garousian M, Khani S, Oliaei SR, Shayan A. Comparison of quality of life, sexual satisfaction and marital satisfaction between fertile and infertile couples. Int J Fertil Steril. 2016;10(3):290–296. PMID: 27695611; PMCID: PMC5023039. doi:10.22074/ijfs.2016.5045
13. Massarotti C, Gentile G, Ferreccio C, Scaruffi P, Remorgida V, Anserini P. Impact of infertility and infertility treatments on quality of life and levels of anxiety and depression in women undergoing in vitro fertilization. Gynecol Endocrinol. 2019;35(6):485–489. PMID: 30612477. doi:10.1080/09513590.2018.1540575
14. El Kissi Y, Romdhane AB, Hidar S, et al. General psychopathology, anxiety, depression and self-esteem in couples undergoing infertility treatment: a comparative study between men and women. Eur J Obstet Gynecol Reprod Biol. 2013;167(2):185–189. PMID: 23298895. doi:10.1016/j.ejogrb.2012.12.014
15. Simonstein F, Mashiach-Eizenberg M, Revel A, Younis JS. Assisted reproduction policies in Israel: a retrospective analysis of in vitro fertilization-embryo transfer. Fertil Steril. 2014;102(5):1301–1306. PMID: 25150392. doi:10.1016/j.fertnstert.2014.07.740
16. Talaulikar VS, Arulkumaran S. Maternal, perinatal and long-term outcomes after assisted reproductive techniques (ART): implications for clinical practice. Eur J Obstet Gynecol Reprod Biol. 2013;170(1):13–19. PMID: 23759305. doi:10.1016/j.ejogrb.2013.04.014
17. Hilbert SM, Gunderson S. Complications of assisted reproductive technology. Emerg Med Clin North Am. 2019;37(2):239–249. PMID: 30940369. doi:10.1016/j.emc.2019.01.005
18. Richards A, Boogert T, Livingstone M, Dalrymple C. Endometrioid ovarian carcinoma in a woman with a history of infertility and multiple in-vitro fertilization treatment cycles. Ultrasound Obstet Gynecol. 2012;40(1):112–114. PMID: 21674660. doi:10.1002/uog.9077
19. Maroufizadeh S, Ghaheri A, Omani Samani R. Factors associated with poor quality of life among Iranian infertile women undergoing IVF. Psychol Health Med. 2017;22(2):145–151. PMID: 26892628. doi:10.1080/13548506.2016.1153681
20. Ni Y, Tong C, Huang L, Zhou W, Zhang A. The analysis of fertility quality of life and the influencing factors of patients with repeated implantation failure. Health Qual Life Outcomes. 2021;19(1):32. PMID: 33494768; PMCID: PMC7831164. doi:10.1186/s12955-021-01666-3
21. Nelson CJ, Shindel AW, Naughton CK, Ohebshalom M, Mulhall JP. Prevalence and predictors of sexual problems, relationship stress, and depression in female partners of infertile couples. J Sex Med. 2008;5(8):1907–1914. PMID: 18564149. doi:10.1111/j.1743-6109.2008.00880.x
22. Verhaak CM, Smeenk JM, van Minnen A, Kremer JA, Kraaimaat FW. A longitudinal, prospective study on emotional adjustment before, during and after consecutive fertility treatment cycles. Hum Reprod. 2005;20(8):2253–2260. PMID: 15817584. doi:10.1093/humrep/dei015
23. Agostini F, Monti F, Fagandini P, Duncan De Pascalis LL, La Sala GB, Blickstein I. Parental mental representations during late pregnancy and early parenthood following assisted reproductive technology. J Perinat Med. 2009;37(4):320–327. PMID: 19290854. doi:10.1515/JPM.2009.062
24. Agostini F, Monti F, Andrei F, Paterlini M, Palomba S, La Sala GB. Assisted reproductive technology treatments and quality of life: a longitudinal study among subfertile women and men. J Assist Reprod Genet. 2017;34(10):1307–1315. PMID: 28733802; PMCID: PMC5633563. doi:10.1007/s10815-017-1000-9
25. Gameiro S, van den Belt-Dusebout AW, Smeenk JM, Braat DD, van Leeuwen FE, Verhaak CM. Women’s adjustment trajectories during IVF and impact on mental health 11–17 years later. Hum Reprod. 2016;31(8):1788–1798. PMID: 27282775. doi:10.1093/humrep/dew131
26. Coughlan C, Walters S, Ledger W, Li TC. A comparison of psychological stress among women with and without reproductive failure. Int J Gynaecol Obstet. 2014;124(2):143–147. PMID: 24290538. doi:10.1016/j.ijgo.2013.08.006
27. Turner K, Reynolds-May MF, Zitek EM, Tisdale RL, Carlisle AB, Westphal LM. Stress and anxiety scores in first and repeat IVF cycles: a pilot study. PLoS One. 2013;8(5):e63743. PMID: 23717472; PMCID: PMC3662783. doi:10.1371/journal.pone.0063743
28. Karaca N, Karabulut A, Ozkan S, et al. Effect of IVF failure on quality of life and emotional status in infertile couples. Eur J Obstet Gynecol Reprod Biol. 2016;206:158–163. PMID: 27693938. doi:10.1016/j.ejogrb.2016.09.017
29. Agostini F, Monti F, De Pascalis L, Paterlini M, La Sala GB, Blickstein I. Psychosocial support for infertile couples during assisted reproductive technology treatment. Fertil Steril. 2011;95(2):707–710. PMID: 20643403. doi:10.1016/j.fertnstert.2010.06.011
30. Mahajan NN, Turnbull DA, Davies MJ, Jindal UN, Briggs NE, Taplin JE. Adjustment to infertility: the role of intrapersonal and interpersonal resources/vulnerabilities. Hum Reprod. 2009;24(4):906–912. PMID: 19106176. doi:10.1093/humrep/den462
31. Martins MV, Peterson BD, Almeida V, Mesquita-Guimarães J, Costa ME. Dyadic dynamics of perceived social support in couples facing infertility. Hum Reprod. 2014;29(1):83–89. PMID: 24218401. doi:10.1093/humrep/det403
32. Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–357. PMID: 3901065. doi:10.1037/0033-2909.98.2.310
33. Ladin K, Daniels A, Osani M, Bannuru RR. Is social support associated with post-transplant medication adherence and outcomes? A systematic review and meta-analysis. Transplant Rev. 2018;32(1):16–28. PMID: 28495070; PMCID: PMC5658266. doi:10.1016/j.trre.2017.04.001
34. Dreyer J, Schwartz-Attias I. Nursing care for adolescents and young adults with cancer: literature review. Acta Haematol. 2014;132(3–4):363–374. PMID: 25228562. doi:10.1159/000360213
35. Ni Y, Huang L, Zhang E, et al. Psychosocial correlates of fertility-related quality of life among infertile women with repeated implantation failure: the mediating role of resilience. Front Psychiatry. 2022;13:1019922. PMID: 36440419; PMCID: PMC9691643. doi:10.3389/fpsyt.2022.1019922
36. Slade P, O’Neill C, Simpson AJ, Lashen H. The relationship between perceived stigma, disclosure patterns, support and distress in new attendees at an infertility clinic. Hum Reprod. 2007;22(8):2309–2317. PMID: 17580298. doi:10.1093/humrep/dem115
37. Schmidt L. Social and psychological consequences of infertility and assisted reproduction - what are the research priorities? Hum Fertil. 2009;12(1):14–20. PMID: 19330608. doi:10.1080/14647270802331487
38. Kahyaoglu Sut H, Balkanli Kaplan P. Quality of life in women with infertility via the FertiQoL and the hospital anxiety and depression scales. Nurs Health Sci. 2015;17(1):84–89. PMID: 25263133. doi:10.1111/nhs.12167
39. Zimet GD, Dahlem NW, Zimet SG, et al. The multidimensional scale of perceived social support. J Pers Assess. 1988;52(1):30–41. doi:10.1207/s15327752jpa5201_2
40. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. PMID: 5172928. doi:10.1016/S0033-3182(71)71479-0
41. Zung WW. A Self-Rating Depression Scale. Arch Gen Psychiatry. 1965;12:63–70. PMID: 14221692. doi:10.1001/archpsyc.1965.01720310065008
42. Chachamovich JR, Chachamovich E, Ezer H, Fleck MP, Knauth D, Passos EP. Investigating quality of life and health-related quality of life in infertility: a systematic review. J Psychosom Obstet Gynaecol. 2010;31(2):101–110. PMID: 20443659. doi:10.3109/0167482X.2010.481337
43. Domar A, Gordon K, Garcia-Velasco J, La marca A, Barriere P, Beligotti F. Understanding the perceptions of and emotional barriers to infertility treatment: a survey in four European countries. Hum Reprod. 2012;27(4):1073–1079. PMID: 22313869. doi:10.1093/humrep/des016
44. Huppelschoten AG, van Dongen AJ, Verhaak CM, Smeenk JM, Kremer JA, Nelen WL. Differences in quality of life and emotional status between infertile women and their partners. Hum Reprod. 2013;28(8):2168–2176. PMID: 23748487. doi:10.1093/humrep/det239
45. Ramezanzadeh F, Aghssa MM, Abedinia N, et al. A survey of relationship between anxiety, depression and duration of infertility. BMC Womens Health. 2004;4(1):9. PMID: 15530170; PMCID: PMC534113. doi:10.1186/1472-6874-4-9
46. Tan S, Hahn S, Benson S, et al. Psychological implications of infertility in women with polycystic ovary syndrome. Hum Reprod. 2008;23(9):2064–2071. PMID: 18583330. doi:10.1093/humrep/den227
47. Wdowiak A, Anusiewicz A, Bakalczuk G, Raczkiewicz D, Janczyk P, Makara-Studzińska M. Assessment of quality of life in infertility treated women in Poland. Int J Environ Res Public Health. 2021;18(8):4275. PMID: 33920638; PMCID: PMC8073613. doi:10.3390/ijerph18084275
48. Chan CH, Lau HP, Tam MY, Ng EH. A longitudinal study investigating the role of decisional conflicts and regret and short-term psychological adjustment after IVF treatment failure. Hum Reprod. 2016;31(12):2772–2780. PMID: 27664215. doi:10.1093/humrep/dew233
49. Cheng CY, Stevenson EL, Yang CT, Liou SR. Stress and quality of life for Taiwanese women who underwent infertility treatment. J Obstet Gynecol Neonatal Nurs. 2018;47(4):498–508. PMID: 29715441. doi:10.1016/j.jogn.2018.03.005
50. Takaki J, Hibino Y. Family-related opinions and stressful situations associated with psychological distress in women undergoing infertility treatment. Int J Environ Res Public Health. 2014;11(9):9068–9081. PMID: 25184788; PMCID: PMC4199007. doi:10.3390/ijerph110909068
51. Agostini F, Monti F, Paterlini M, Andrei F, Palomba S, La Sala GB. Effect of the previous reproductive outcomes in subfertile women after in vitro fertilization (IVF) and/or intracytoplasmic sperm injection (ICSI) treatments on perinatal anxious and depressive symptomatology. J Psychosom Obstet Gynaecol. 2018;39(1):29–37. PMID: 28635535. doi:10.1080/0167482X.2017.1286474
52. Kong L, Shao Y, Xia J, et al. Quantitative and qualitative analyses of psychological experience and adjustment of in vitro fertilization-embryo transfer patients. Med Sci Monit. 2019;25:8069–8077. PMID: 31656309; PMCID: PMC6836641. doi:10.12659/MSM.916627
53. Newton CR, Hearn MT, Yuzpe AA. Psychological assessment and follow-up after in vitro fertilization: assessing the impact of failure. Fertil Steril. 1990;54(5):879–886. PMID: 2226921. doi:10.1016/s0015-0282(16)53950-8
54. Durgun Ozan Y, Okumuş H. Effects of nursing care based on watson’s theory of human caring on anxiety, distress, and coping, when infertility treatment fails: a randomized controlled trial. J Caring Sci. 2017;6(2):95–109. PMID: 28680864; PMCID: PMC5488674. doi:10.15171/jcs.2017.010
55. Li J, Long L, Liu Y, He W, Li M. Effects of a mindfulness-based intervention on fertility quality of life and pregnancy rates among women subjected to first in vitro fertilization treatment. Behav Res Ther. 2016;77:96–104. PMID: 26742022. doi:10.1016/j.brat.2015.12.010
56. Seyedi Asl ST, Sadeghi K, Bakhtiari M, Ahmadi SM, Nazari Anamagh A, Khayatan T. Effect of group positive psychotherapy on improvement of life satisfaction and the quality of life in infertile woman. Int J Fertil Steril. 2016;10(1):105–112. PMID: 27123207; PMCID: PMC4845519. doi:10.22074/ijfs.2016.4775
57. Knoll N, Schwarzer R, Pfüller B, Kienle R. Transmission of depressive symptoms: a study with couples undergoing assisted-reproduction treatment. Eur Psychol. . 2009;14:7–17. doi:10.1027/1016-9040.14.1.7
58. Verhaak CM, Smeenk JM, Evers AW, Kremer JA, Kraaimaat FW, Braat DD. Women’s emotional adjustment to IVF: a systematic review of 25 years of research. Hum Reprod Update. 2007;13(1):27–36. PMID: 16940360. doi:10.1093/humupd/dml040
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
