Back to Journals » International Journal of General Medicine » Volume 14
Diagnostic Values of Epicardial Adipose Tissue Thickness with Right Common Carotid Artery Elasticity and Intima-Media Thickness for Middle-Aged and Elderly Patients with Coronary Heart Disease
Authors Qian C, Sun Y, Jiang J
Received 3 December 2020
Accepted for publication 21 January 2021
Published 25 February 2021 Volume 2021:14 Pages 633—639
DOI https://doi.org/10.2147/IJGM.S292426
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Chengsi Qian1 *,* Yan Sun2 *,* Jun Jiang1
1Department of Cardiology, The Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, 310009, Zhejiang Province, People’s Republic of China; 2Department of Cardiology, Zhejiang Rongjun Hospital, Jiaxing, 314001, Zhejiang Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jun Jiang Email [email protected]
Background: Coronary heart disease (CHD) is the most common cardiovascular disease which greatly threatens the health of middle-aged and elderly people.
Objective: To explore the correlations of epicardial adipose tissue (EAT) thickness with right common carotid artery elasticity and intima-media thickness (IMT) in middle-aged and elderly patients with CHD by ultrasound.
Methods: A total of 132 patients diagnosed with CHD by coronary angiography (CAG) from February 2019 to August 2020 were enrolled and divided into single-vessel disease group (n=38), double-vessel disease group (n=52), and three-vessel disease group (n=42), and 52 healthy subjects were selected as control group. Their general data, biochemical indices, EAT thickness, right common carotid artery elasticity indices, and IMT were compared. The correlations of EAT thickness with right common carotid artery elasticity indices and IMT were studied by Pearson’s analysis. The predictive values of EAT thickness and IMT for CHD were analyzed by receiver operating characteristic curves.
Results: With increasing number of diseased branches, EAT thickness, stiffness parameters β (β), strain elastic modulus (Ep), pulse wave velocity β (PWV-β) and IMT increased, arterial compliance (AC) decreased (P< 0.05), but argumentation index (AI) did not change significantly. EAT thickness had significant positive correlations with β, Ep, PWV-β and IMT, negative correlation with AC, and no significant correlation with AI. The areas under the curves of EAT thickness and IMT for predicting CHD were 0.806 and 0.784, respectively.
Conclusion: EAT thickness is significantly correlated with right common carotid artery elasticity and IMT in middle-aged and elderly patients with CHD, and EAT thickness and IMT have high predictive values. The three indices are crucial for CHD diagnosis.
Keywords: ultrasound, coronary heart disease, epicardial adipose tissue, right common carotid artery elasticity, intima-media thickness
Introduction
With the acceleration of aging, the incidence rate of cardio-cerebrovascular diseases closely related to the middle-aged and elderly population is gradually increasing.1 Coronary heart disease (CHD) is the most common cardiovascular disease which greatly threatens the health of middle-aged and elderly people.2 CHD means that in the case of abnormal lipid metabolism, blood lipids deposit on the artery intima and gradually accumulate to form white plaques that lead to arterial stenosis and obstruction of blood flow, resulting in myocardial ischemia and angina pectoris.3 The incidence, disability and mortality rates of CHD are rising annually.4 Epicardial adipose tissue (EAT) refers to the adipose tissue between the visceral layer of the pericardium and the outer surface of the myocardium, surrounding the coronary arteries, and there is no fascia to separate them.5 EAT is able to secrete multiple inflammatory and anti-inflammatory cytokines to maintain vascular homeostasis,6 but increase in its thickness induces changes in the paracrine function of adipocytes, releasing a large number of inflammatory cytokines to form an inflammatory state.7 The increase in EAT thickness also raises the risk of cardiovascular diseases, which may be a risk factor for atherosclerotic diseases.8 It is easy to detect the common carotid artery that is in a relatively superficial position, which is often used to reflect the degree of arteriosclerosis.9 The common carotid artery intima-media thickness (IMT) is closely associated with CHD.10 Echo-tracking (ET) technique is a new non-invasive ultrasound method that can accurately determine the indices reflecting common carotid artery elasticity and IMT.11 The present study aimed to explore the correlations of EAT thickness with right common carotid artery elasticity and IMT in middle-aged and elderly patients with CHD by ultrasound.
Patients and Methods
General Information
A total of 132 patients diagnosed with CHD by coronary angiography (CAG) from February 2019 to August 2020 in our hospital were enrolled. According to the number of diseased branches, the patients were divided into single-vessel disease group (n=38), double-vessel disease group (n=52), and three-vessel disease group (n=42). In single-vessel disease group, there were 18 males and 20 females aged 45–73 years old, with an average age of 62.41±8.12 years. In the double-vessel disease group, there were 24 males and 28 females aged 46–75 years old, with an average age of 64.35±7.23 years. In the three-vessel disease group, there were 19 males and 23 females aged 46–78 years old, with an average age of 63.58±6.95 years. Meanwhile, 52 healthy subjects physically examined in our hospital were selected as control group, including 18 males and 24 females aged 45–76 years old, with an average age of 63.74±8.26 years.
Inclusion criteria: a) patients who were diagnosed with CHD by CAG, b) those with at least one diseased coronary artery stenosis of more than 50%, c) those who had quit smoking for more than 5 years or had no history of smoking, d) those aged 45–80 years old, and e) those with complete clinical data.
Exclusion criteria: a) patients with unclear ultrasound images, b) those whose pericardial effusion or EAT could not be identified, c) those with congenital heart disease, thyroid disease, severe liver or kidney insufficiency, or diseases in vital organs, d) those with common carotid artery stenosis, e) those who were pregnant or had endocrine disorders, f) those with mental disorders or infectious diseases, g) those with poor compliance, or h) presence of morphologic/functional EAT changes such as aortic valve stenosis, atrial fibrillation or heart failure.
This study was approved by the Ethics Committee of The Second Affiliated Hospital of Zhejiang University School of Medicine and was conducted in accordance with the Declaration of Helsinki. All patients and their families signed the informed consent.
Collection of Baseline Clinical Data
The general data of patients were collected through electronic medical records. After admission, gender and age (years old) were recorded, height (m) and weight (kg) were measured to calculate body mass index (BMI=weight/height2), and systolic blood pressure (mmHg) and diastolic blood pressure (mmHg) were measured.
Measurement of Biochemical Indices
In the early morning of the next day after admission, 5 mL of fasting venous blood was drawn from every patient and placed in a serum separation tube, followed by centrifugation at 3000 rpm for 10 min. Subsequently, the serum was collected to detect fasting blood glucose (FBG), total cholesterol (TC), triacylglycerol (TG), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C) levels.
Measurement of EAT Thickness
Voluson E8 color Doppler ultrasound system (USA) was utilized to measure EAT thickness (frequency: 2.5 MHz) according to previous literature.12 EAT thickness between the free wall of right ventricle and the visceral layer of pericardium was measured as follows (Figure 1): an M5S probe was positioned on the parasternal long-axis section, the image was frozen at end-diastole, and then the sampling line was perpendicular to the free wall of the right ventricle and fixed at the aortic valve annulus. Besides, the M5S probe was positioned at the level of the papillary muscle, the image was frozen at end-diastole, and then the sampling line was perpendicular to the interventricular septum. Three dynamic images of the cardiac cycle were captured to obtain the average, and the average of EAT thicknesses of the two sections was calculated.
 |
Figure 1 EAT measurement. EAT of the anterior wall of the right ventricle appears as a hypoechoic zone between the epicardium (red arrow below) and pericardium visceral layer (red arrow above). |
Measurement of Right Common Carotid Artery Elasticity and IMT
The vascular elasticity of right common carotid artery was determined by L11-3 probe with a frequency of 7–13 MHz combined with ET technique. Firstly, after resting for 5–10 min, blood pressure was measured from the right upper limb of the patient. The patient was kept in a supine position, with the neck fully exposed. Subsequently, the morphology and thickness of the intima-media of right common carotid artery were examined by ultrasound, and IMT was measured in the middle of right common carotid artery. Then ECG was connected, and M-type sampling line was adjusted to be perpendicular to the common carotid artery wall. At 2.0 cm below the lower edge of right carotid sinus, the sampling gates were placed at the junctions of the anterior and posterior walls of the common carotid artery, respectively, avoiding the internal jugular vein as much as possible. The trajectory of the anterior and posterior walls of the blood vessel was tracked in real time and recorded during systole and diastole, and then more than five continuous change curves of the inner diameter of the common carotid artery were obtained. Next, the systolic and diastolic blood pressures were loaded, and the clear images of 5–6 cardiac cycles were selected for offline analysis. Finally, the indices reflecting right common carotid artery elasticity were determined and calculated, including stiffness parameters (β), strain elastic modulus (Ep), pulse wave velocity β (PWV-β), arterial compliance (AC), and argumentation index (AI). All data were measured 3 times to obtain the average. Ep (kPa) = (SP-DP)/[(Ds-Dd)/Dd]; β = ln(SP/DP)/[(Ds-Dd)/Dd]; AC (mm2/kPa) = π(Ds2-Dd2)/[4(SP-DP)]; PWV-β (m/s) = (β×DP/2p)1/2; AI (%) = Dp/PP. Where SP is the systolic pressure, DP is the diastolic pressure, PP is the pulse pressure, Dp is the difference between the peak systolic pressure and the pressure at break point, Ds is the maximum diameter of the carotid artery, Dd is the minimum diameter of the carotid artery, and p is the blood density.13
Statistical Analysis
SPSS 19.0 software was adopted to conduct one-way analysis of variance. GraphPad Prism 5.0 software was utilized for plotting. The differences between two groups were compared by t-test, and the differences among multiple rates or constituent ratios were compared by Chi-squared test. The correlations of EAT thickness with right common carotid artery elasticity indices and IMT were studied by Pearson’s analysis. The predictive values of EAT thickness and IMT for CHD were analyzed by receiver operating characteristic (ROC) curves. P<0.05 indicated that the difference was statistically significant.
Results
General Information and Biochemical Indices
The four groups had similar age, gender, BMI, systolic blood pressure, diastolic blood pressure, as well as FBG, TC, TG, HDL-C, and LDL-C levels (P>0.05) (Table 1).
 |
Table 1 General Information and Biochemical Indices |
EAT Thickness
EAT thickness was significantly higher in the three-vessel disease group than those in double-vessel disease group, single-vessel disease group, and control group in turn (P<0.05) (Table 2).
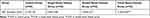 |
Table 2 EAT Thickness |
Right Common Carotid Artery Elasticity Indices and IMT
With increasing number of diseased branches, right common carotid artery elasticity indices β, Ep, PWV-β and IMT significantly increased, and AC decreased (P<0.05). No significant difference was found in AI among the four groups (P>0.05) (Table 3).
 |
Table 3 Right Common Carotid Artery Elasticity Indices and IMT |
Correlation Analysis Results
The results of Pearson’s correlation analysis displayed that EAT thickness had significant positive correlations with β, Ep, PWV-β, AC and IMT (P<0.05), negative correlation with AC (P<0.05), and no significant correlation with AI (P>0.05) (Table 4 and Figure 2).
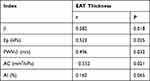 |
Table 4 Correlations Between EAT Thickness and Right Common Carotid Artery Elasticity Indices |
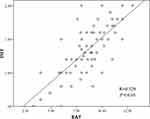 |
Figure 2 Correlation between EAT thickness and IMT. |
ROC Curve Analysis Results
To assess the predictive values of EAT thickness and IMT for CHD, the optimal cut-off values were obtained by plotting ROC curves. The optimal cut-off values of EAT thickness and IMT for predicting CHD were 4.28 and 0.73, respectively. The areas under the curves were 0.806 [95% confidence interval (CI): 0.735–0.863, P<0.001] and 0.784 (95% CI: 0.716–0.824, P<0.001), respectively, suggesting high predictive values (Table 5 and Figure 3).
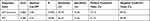 |
Table 5 Predictive Values of EAT Thickness and IMT for CHD |
 |
Figure 3 ROC curve analysis of predictive values of EAT thickness and IMT for CHD. |
Discussion
CHD is a common cardiovascular disease in middle-aged and elderly people, which is mainly caused by coronary atherosclerosis which is the most common type of arteriosclerosis.14 Possibly, CHD occurs because the branches of coronary arteries are multi-directional and close to the ventricle, and bear huge blood flow shear stress and systolic pressure impact.15 Considerable complex carbohydrates and lipids are deposited in the intima of the involved artery, inducing fibrous tissue hyperplasia and calcium deposition, and even vascular occlusion and wall rupture and bleeding.16 As the gold standard for CHD diagnosis, CAG is an invasive and expensive examination method.17 Thus, it is necessary to find non-invasive and highly predictive diagnostic indices. EAT thickness has a close relationship with CHD and has high predictive value for it.18 Besides, it is easy to detect the common carotid artery which is in a relatively superficial position, so related indices have often been utilized to reflect the degree of arteriosclerosis in recent years.19
EAT accumulates on the surface of the heart and originates from brown adipose tissue together with visceral adipose tissues such as the greater omentum and mesentery.20 About 80% of the surface of an adult heart is covered by EAT, mostly covering the right ventricle.21 As an independent risk factor for CHD, the increase in EAT thickness can reflect severity.22 Given the fact that the echo of EAT notably differs from those of surrounding tissues during ultrasound examination, it is easy to accurately measure EAT thickness through echocardiography.23 Moreover, due to non-invasiveness, simple operation and no economic burden to patients, echocardiography for EAT examination is well-accepted by patients. In the present study, EAT thickness was significantly higher in the three-vessel disease group compared with double-vessel disease group, single-vessel disease group, and control group in turn. The common carotid artery, a crucial blood vessel that supplies blood to the head and neck, is superficial and convenient for detection, so it has always been considered as a “window” to reflect the degree of arteriosclerosis. ET is a non-invasive ultrasound technique to examine vascular function, which can accurately measure common carotid artery elasticity indices including β, Ep, PWV-β, AC, and AI as well as IMT.24 Ren et al reported that common carotid artery elasticity and IMT were closely associated with CHD.10 In this study, with increasing number of diseased branches, β, Ep, PWV-β, and IMT significantly increased, and AC decreased. No significant difference was found in AI.
EAT thickness, right common carotid artery elasticity, and IMT are all measured by ultrasound, so the procedure is non-invasive and simple. Since the three indices are closely related to CHD, they can work as predictors for early CHD and reflect the severity and therapeutic effect.10 EAT thickness has significant correlations with right common carotid artery elasticity and IMT.25 In the present study, EAT thickness had significant positive correlations with β, Ep, PWV-β and IMT, negative correlation with AC, and no significant correlation with AI. With high predictive values for CHD, EAT thickness and IMT are crucial for diagnosing and evaluating the therapeutic effects of CHD.5 Herein, the optimal cut-off values of EAT thickness and IMT for predicting CHD were 4.28 and 0.73, respectively, and the areas under the curves were 0.806 and 0.784, respectively, suggesting their high predictive values.
Conclusion
In conclusion, given the high correlations of EAT thickness with right common carotid artery elasticity and IMT in middle-aged and elderly patients with CHD and the high predictive values of EAT thickness and IMT for CHD, the three indices are of significance in CHD diagnosis.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Zeng T, Cui H, Tang D, et al. Short-term dietary restriction in old mice rejuvenates the aging-induced structural imbalance of gut microbiota. Biogerontology. 2019;20(6):837–848. doi:10.1007/s10522-019-09830-5
2. Jin K, Khonsari S, Gallagher R, et al. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review and meta-analysis. Eur J Cardiovasc Nurs. 2019;18(4):260–271. doi:10.1177/1474515119826510
3. Muscella A, Stefàno E, Marsigliante S. The effects of exercise training on lipid metabolism and coronary heart disease. Am J Physiol Heart Circ Physiol. 2020;319(1):H76–H88. doi:10.1152/ajpheart.00708.2019
4. Bacquer DD, Smedt DD, Kotseva K, et al. Incidence of cardiovascular events in patients with stabilized coronary heart disease: the EUROASPIRE IV follow-up study. Eur J Epidemiol. 2018;34(3):247–258. doi:10.1007/s10654-018-0454-0
5. Hruskova J, Maugeri A, Podroužková H, et al. Association of cardiovascular health with epicardial adipose tissue and intima media thickness: the kardiovize study. J Clin Med. 2018;7(5):113–125. doi:10.3390/jcm7050113
6. Nabati M, Salehi A, Hatami G, Dabirian M, Yazdani J, Parsaee H. Epicardial adipose tissue and its association with cardiovascular risk factors and mitral annular calcium deposits. Ultrasound. 2019;27(4):217–224. doi:10.1177/1742271X19846159
7. Cicek Y, Durakoglugil ME, Rakici H, Balcioglu AS, Duman H, Erdogan T. The effect of epicardial adipose tissue thickness with irritable bowel syndrome. J Pak Med Assoc. 2018;68(10):1456–1460.
8. Lu C, Jia H, Wang Z. Association between epicardial adipose tissue and adverse outcomes in coronary heart disease patients with percutaneous coronary intervention. Biosci Rep. 2019;39(5):BSR20182278. doi:10.1042/BSR20182278
9. Jain PK, Gupta S, Bhavsar A, Nigam A, Sharma N. Localization of common carotid artery transverse section in B-mode ultrasound images using faster RCNN: a deep learning approach. Med Biol Eng Comput. 2020;58(3):471–482. doi:10.1007/s11517-019-02099-3
10. Ren L, Shi M, Wu Y, et al. Correlation between hypertension and common carotid artery intima-media thickness in rural China: a population-based study. J Hum Hypertens. 2018;32(8–9):548–554. doi:10.1038/s41371-018-0074-x
11. Yeh YC, Fang KM, Hsu WL, Liao LJ. The effectiveness of high-resolution ultrasound in the assessment of the carotid intima–media thickness for postirradiated neck. Eur Arch Otorhinolaryngol. 2019;276(4):1167–1173. doi:10.1007/s00405-019-05302-1
12. Iacobellis G, Willens HJ. Echocardiographic epicardial fat: a review of research and clinical applications. J Am Soc Echocardiogr. 2009;22(12):1311–1319. doi:10.1016/j.echo.2009.10.013
13. Ozisler C, Kaplanoglu H. Evaluation of subclinical atherosclerosis by ultrasound radiofrequency data technology in patients with primary Sjogren's syndrome. Clin Rheumatol. 2019;38(3):709–717. doi:10.1007/s10067-018-4330-9
14. Vuorio A, Kovanen PT. Decreasing the cholesterol burden in heterozygous familial hypercholesterolemia children by dietary plant stanol esters. Nutrients. 2018;10(12):1842–1851. doi:10.3390/nu10121842
15. Koksungnoen S, Rattanadecho P, Wongchadakul P. 3D numerical model of blood flow in the coronary artery bypass graft during no pulse and pulse situations: effects of an anastomotic angle and characteristics of fluid. J Mech Sci Technol. 2018;32(9):4545–4552. doi:10.1007/s12206-018-0851-z
16. Herr JE, Hétu MF, Li TY, Ewart P, Johri AM. Presence of calcium-like tissue composition in carotid plaque is indicative of significant coronary artery disease in high-risk patients. J Am Soc Echocardiogr. 2019;32(5):633–642. doi:10.1016/j.echo.2019.01.001
17. Vallée A, Zhang Y, Protogerou A, Safar ME, Blacher J. Added value of aortic pulse wave velocity index for the detection of coronary heart disease by elective coronary angiography. Blood Press. 2019;28(6):375–384. doi:10.1080/08037051.2019.1641400
18. Sinha SK, Thakur R, Jha MJ, et al. Epicardial adipose tissue thickness and its association with the presence and severity of coronary artery disease in clinical setting: a cross-sectional observational study. J Clin Med Res. 2016;8(5):410–419. doi:10.14740/jocmr2468w
19. Nerlekar N, Brown AJ, Muthalaly RG, et al. Association of epicardial adipose tissue and high-risk plaque characteristics: a systematic review and meta-analysis. J Am Heart Assoc. 2017;6(8):e006379. doi:10.1161/JAHA.117.006379
20. Cho DH, Joo HJ, Kim MN, Lim DS, Shim WJ, Park SM. Association between epicardial adipose tissue, high-sensitivity C-reactive protein and myocardial dysfunction in middle-aged men with suspected metabolic syndrome. Cardiovasc Diabetol. 2018;17(1):95–103. doi:10.1186/s12933-018-0735-7
21. Senoo A, Kitagawa T, Torimaki S, et al. Association between histological features of epicardial adipose tissue and coronary plaque characteristics on computed tomography angiography. Heart Vessels. 2018;33(8):827–836. doi:10.1007/s00380-018-1129-1
22. Rhee TM, Kim HL, Lim WH, et al. Association between epicardial adipose tissue thickness and parameters of target organ damage in patients undergoing coronary angiography. Hypertens Res. 2019;42(4):549–557. doi:10.1038/s41440-018-0180-8
23. Quisi A, Şentürk SE, Harbalıoğlu H, Baykan AO. The relationship between echocardiographic epicardial adipose tissue, P-wave dispersion, and corrected QT interval. Turk Kardiyol Dern Ars. 2018;46(6):471–478. doi:10.5543/tkda.2018.01578
24. Liang H, Wang D, Che G, Su Y. Evaluation of carotid artery elasticity in patients with uremia by echo tracking. J Med Ultrason. 2018;45(4):591–596. doi:10.1007/s10396-018-0868-z
25. Sag S, Yildiz A, Gullulu S, et al. Early atherosclerosis in normotensive patients with autosomal dominant polycystic kidney disease: the relation between epicardial adipose tissue thickness and carotid intima-media thickness. Springerplus. 2016;5(1):211. doi:10.1186/s40064-016-1871-8
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
