Back to Journals » International Journal of Women's Health » Volume 15
Diagnostic Accuracy of Placental Thickness in Lower Uterine Segment Measured by Ultrasound in Prediction of Placenta Accreta Spectrum in Patients with Placenta Previa. A Diagnostic Test Accuracy Study
Authors Elmaraghy AM , Taha Fayed S, Abd ElHamid Ali M, Ali Hassanien M, Mohamed Mamdouh A
Received 2 December 2022
Accepted for publication 3 February 2023
Published 16 February 2023 Volume 2023:15 Pages 311—320
DOI https://doi.org/10.2147/IJWH.S399520
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Ahmed Mohammed Elmaraghy,1 Salah Taha Fayed,1 Mahmoud Abd ElHamid Ali,2 Monira Ali Hassanien,3 Ahmed Mohamed Mamdouh1
1Department of Obstetrics & Gynecology, Faculty of Medicine, Ain Shams University, Cairo, Egypt; 2Department of Obstetrics & Gynecology, Bani Sweif Hospital, Ministry of Health, Bani Sweif, Egypt; 3Obstetrics and Gynecology, Ultrasound and Fetal Care Unit, Ain Shams University Maternity Hospital, Cairo, Egypt
Correspondence: Ahmed Mohammed Elmaraghy, Email [email protected]
Objective: The aim of the study was to evaluate the association between placental thickness and placenta accreta spectrum (PAS) in patients with placenta previa.
Materials and Methods: In this prospective study, 40 patients diagnosed with placenta previa were included. The maximum placental thickness in the lower uterine segment was obtained using a transabdominal scan. For the image to be deemed suitable, a midline sagittal section of the lower uterine segment (with the implanted placenta) and the cervical canal, with the intervening urinary bladder had been required. Intraoperative attendance was ensured for the detection of cases with spontaneous separation and cases with morbid adherence. All specimens removed were sent for histopathology to confirm PAS. The primary outcome of the study was to detect a threshold of placental thickness which can be used as a cut-off value in such screening test. The number of units of packed RBCs transfused during the operation and bladder injury were secondary measures of outcome.
Results: Forty patients were included in the study; 20 patients were ultimately diagnosed with PAS while 20 patients did not have PAS. Mean placental thickness was significantly higher in the PAS patients compared with those with no invasive placentation (61.00 mm Vs 43.00 mm, P value 0.000). Using receiver operating characteristic (ROC) curve, a threshold placental thickness of 58mm was associated with 55% sensitivity, 90% specificity, 84.6% positive predictive value, and 66.7% negative predictive value. Multivariate logistic regression showed that placental thickness more than 58mm and having past history of more than three cesarean sections were independent risk factors for PAS among patients with placenta previa.
Conclusion: Placental thickness in the lower uterine segment is increased in patients with placenta previa with PAS compared to those with no PAS. Such finding can be implemented into clinical practice by using placental thickness as a screening test for PAS in patients with placenta previa.
ClinicalTrials.gov ID: NCT05500404.
Keywords: placental thickness, placenta accreta spectrum, placenta previa, ultrasound, cesarean section
Introduction
Placenta previa is a major obstetric complication that occurs when the placenta occupies lower uterine segment with either partial or complete coverage of the internal os of the cervix.1 The incidence of placenta previa is estimated to be 0.5%. This incidence has increased in recent years. This can be attributed to higher number of cesarean deliveries, in vitro fertilization, previous spontaneous and elective pregnancy terminations, and previous uterine surgery.2
Placenta accreta spectrum (PAS) is one of the most grave conditions associated with pregnancy as it can lead to massive bleeding, which can result in maternal mortality or severe morbidities like multi-organ failure, disseminated intravascular coagulopathy, need for intensive care unit admission and hysterectomy.3 Placenta previa is a risk factor for PAS and there is a lot of overlap in imaging findings between the two processes. PAS problems affect approximately 11% of the people with placenta previa. Differentiating between placenta previa with and without PAS problems is crucial in clinical practice.4
Maternal mortality due to PAS is reduced when the condition is diagnosed at the antenatal period as it allows for proper management of the condition in advance. Ultrasound is the investigation of choice for antenatal diagnosis of abnormally invasive placenta, and the diagnostic accuracy is good both in retrospective and prospective case series.5
Current antenatal diagnosis of morbidly adherent placenta depends on the identification of sonographic findings on grayscale and color Doppler imaging. Such findings are usually subjective with difference in its interpretation by different individuals. While multiple findings have been reported in the literature, even experts provide a range of different descriptions, and efforts are currently underway to provide uniform lexicon and descriptors. When blinded to clinical data, there is significant inter-observer variability in the diagnosis of invasive placentation. While imaging features have increased sensitivity and specificity with experts, developing an objective metric to risk stratify cases even in the hands of less experienced reviewers is useful.2
Maximum placental thickness has a linear correlation with gestational age with a thickness above 50 mm between 32 and 34 weeks of gestation being above the 90th centile.5 Several retrospective studies have stated an association between placental thickness and PAS development in patients with placenta previa.2,6 The cause of this association is not clear but can be attributed to the limited migration of the placenta due to its attachment to the cesarean scar defect with the resulting mushroom-like bulging of the placenta out of the defect.5
The aim of our study was to evaluate placental thickness in lower uterine segment measured by ultrasound in patients with placenta previa regarding its accuracy in prediction of PAS. Defining a cutoff value which can be used for screening purposes of such morbid condition was the ultimate goal of the study.
Materials and Methods
This diagnostic accuracy test study was carried out during the period from January to August 2022 at Ain Shams university maternity hospital. The study participants were 40 pregnant women with ultrasound proven diagnosis of placenta previa and past history of at least one cesarean section. Using PASS 15 sample size program for sample size calculation, setting the power at 80% and alpha error at 0.05, it was estimated that sample size of 40 patients was needed to detect the diagnostic accuracy of placental thickness for diagnosis of PAS assuming that the area under ROC curve = 0.75 and the proportion of patients with PAS diagnosed by histopathology among studied patients = 58%.2
The age of the included participants ranged from 20 to 45 years and at the time of recruitment, their gestational age was ≥26 weeks. Hemodynamically unstable women, those with repeated attacks of antepartum hemorrhage were excluded from the study. Moreover, patients with medical disorders leading to uteroplacental insufficiency such as systemic lupus erythematosus or antiphospholipid antibody syndrome or enlarged placenta such as cases with fetal hydrops or multiple pregnancy were also excluded from the study.
After obtaining informed consent, patients included in the study underwent measurement of placental thickness. The maximum placental thickness in the lower uterine segment was obtained using transabdominal ultrasound scan by obstetrics and gynecology consultant with special interest in obstetric ultrasound. Ultrasound was performed at the ultrasound and fetal care unit of Ain Shams University Maternity Hospital. For the image to be deemed suitable, a midline sagittal section of the lower uterine segment (with the implanted placenta) and the cervical canal, with the intervening urinary bladder was required.5 The measurement was made by a researcher who was blinded to the final diagnosis. Intraoperative attendance of the cesarean section to document intraoperative findings of morbidly adherent placenta was ensured. Cases with spontaneous placental separation without any attempts of manual extraction, ie, no evidence of invasion were documented and recorded, while cases that underwent cesarean hysterectomy due morbidly adherent placenta or myometrial resection due to focal invasion were documented and the removed specimens were sent for histopathology to document PAS and to determine the depth of invasion. The primary outcome of the study was the threshold of placental thickness which can be used as a cut-off level with appropriate sensitivity and specificity so it can be used as a screening test for such morbid condition. The number of units of packed RBCs transfused intraoperatively and intraoperative complications as bladder injury were secondary measures of outcome.
This study was done after approval of the Ethical Committee of the Faculty of Medicine, Ain Shams University. Informed consent was taken from all participants before recruitment in the study, and after explaining the purpose and procedures of the study. The investigator retained the original signed informed consent form. The data were collected confidentially. The study was based on the investigator self-funding. Quantitative variables were presented using mean and SD. Qualitative variables were presented using count and percentage. Student’s t-test was used to compare quantitative variables between two independent groups and Chi square test was used for qualitative variables. ROC curve analysis was used to compare the predictive ability of the two measures and determine the best cut-off value with the highest sensitivity and specificity for each measure. Logistic regression analysis was done to measure the ability of different factors to predict PAS. P value less than or equal to 0.05 will be considered statistically significant.
Results
The study included 40 pregnant women with ultrasound proven diagnosis of placenta previa. The age of the study participants ranged from 20 to 43 years (Table 1). Table 1 presents the baseline characteristics of the studied participants.
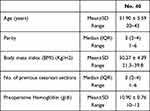 |
Table 1 Baseline Characteristics of the Studied Patients |
Placental thickness was measured at the third trimester and the results ranged from 15mm to 110mm (Table 2); such measurements were compared with the histopathological examination of removed specimens which is the gold standard diagnostic test for PAS. Fifty percent of the study participants had PAS (Table 3). Table 4 illustrates the depth of invasion detected by histopathology.
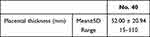 |
Table 2 Placental Thickness Among the Studied Patients |
 |
Table 3 Incidence of PAS and Pathological Results Among the Studied Patients: (Total Number: 40) |
 |
Table 4 Operative Complications in the Study Participants:(Total Number: 40 Patients) |
Operative complications are presented in Table 4. There were neither ureteric injuries nor vascular injuries. No intestinal injuries were reported as well.
The distribution of blood groups among study participants is presented in Table 5.
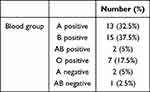 |
Table 5 Blood Group Distribution Among the Studied Patients |
The final outcome has divided study participants into two groups: patients with placenta previa with PAS and patients with placenta previa with no morbid adherence. Table 6 shows the comparison between the two groups regarding demographic data with age, parity and number of previous cesarean sections being significantly higher in PAS patients. Placental thickness had a significant correlation with PAS in patients with placenta previa (Table 7).
 |
Table 6 Comparison Between Patients with PAS and Those with No PAS Regarding Demographic Data |
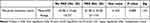 |
Table 7 Comparison Between Patients with PAS and Patients with No PAS Regarding Placental Thickness |
Hysterectomy is the standard treatment for cases of PAS; 85% of the PAS group (17 patients) underwent cesarean hysterectomy, while only 3 patients underwent partial myometrial resection due to focal invasion. None of the patients with no morbid adherence underwent a hysterectomy. Regarding blood transfusion, requirements were significantly higher in the PAS group. There was no significant difference between the two groups regarding bladder injury (Table 8).
 |
Table 8 Comparison Between Patients with PAS and Patients with No PAS Regarding Operative Complications |
Table 9 shows that there was no significant correlation between certain blood groups and PAS development among study participants.
 |
Table 9 Comparison Between Patients with PAS and Those with No PAS Regarding Different Blood Groups |
The multivariate logistic regression model showed that having more than three previous cesarean sections and placental thickness more than 58mm were independent risk factors for having PAS in patients with placenta previa (Table 10).
 |
Table 10 Univariate and Multivariate Logistic Regression Analyses for Factors Associated with Placenta Accreta Spectrum |
The ROC curve of placental thickness showed that a cutoff value of 58mm was associated with 55% sensitivity, 90% specificity, 84.6 positive predictive value and 66.7 negative predictive value (Table 11).
 |
Table 11 Data Interpreted from ROC Curve |
Discussion
To our knowledge, this is the first prospective study assessing the value of placental thickness as a screening tool for the detection of placenta accreta spectrum in patients with placenta previa.
The study included 40 pregnant patients with ultrasound proven diagnosis of placenta previa or low-lying placenta; 20 patients (50%) were diagnosed with PAS which was confirmed by histopathology while 20 patients (50%) did not have PAS and their placenta were separated completely at CS (Figure 1). Eighty-five percent of the patients with PAS (17/20) underwent cesarean hysterectomy, which is the standard treatment for morbidly adherent placenta, while the remaining 15% (3/20) had focal invasion and underwent conservative surgery in the form of partial myometrial resection. None of the patients with no PAS underwent a cesarean hysterectomy (Figure 2).
 |
Figure 1 Incidence of placenta accrete spectrum among study participants. |
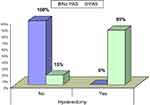 |
Figure 2 Incidence of cesarean hysterectomy among PAS and no PAS patients. |
Our study showed that age was significantly higher among patients with PAS compared with patients with placenta previa but no PAS. The univariate logistic regression model showed that age above 35 years increased the aOR for developing PAS by 5.7 (95% CI: 1.254–25.606) for every 1-year increase in age. RCOG guideline discussing placenta previa and placenta accreta spectrum reported a similar association with an increase in the aOR by 1.3 (95% CI 1.13–1.50) for every 1-year increase in age in women without previous cesarean delivery.4 Such higher aOR in our study could be attributed to the fact that all the study participants had at least one previous cesarean delivery.
All epidemiological studies in the past 20 years have shown a direct association between the increase in cesarean deliveries and the incidence of PAS.4 Our results showed that there is a significant association between the number of cesarean deliveries and the development of PAS in patients with placenta previa. Moreover, the multivariate regression model showed that among the study participants, the presence of more than three previous cesarean deliveries was associated with OR of 17.7 for developing PAS. Regarding parity, the significant association between the increase in parity and PAS seemed to be a consequence to the increase in the number of cesarean deliveries since having at least one previous cesarean delivery was one of the inclusion criteria of the study.
Body mass index was not significantly associated with the development of PAS; this is consistent with the results of the cohort study obtained by Vieira et al, which showed that obesity by itself was not strongly correlated with PAS and that the apparent association seems to be confounded by the high incidence of CS among patients with high BMI.7
The maximum placental thickness in the lower uterine segment was directly correlated with the presence of PAS disorder as evidenced by the significant linear association between the placental thickness and histological confirmation of PAS in either the hysterectomy specimens or the resected myometrial segments in cases who underwent conservative surgery. The ROC curve of placental thickness revealed an area under the curve of 0.734. The maximum placental thickness of 58mm was determined as the cut-off point in the screening for PAS disorder with 55% sensitivity, 90% specificity, 84.6% PPV, and 66.7 NPV (Figure 3). The multivariate logistic regression analysis showed that the cut-off point of 58mm was associated with an odds ratio of 18.519 for developing PAS among patients with placenta previa. These findings were similar to that obtained by Bhide et al in their retrospective analysis which showed that for each 1mm increase in placental thickness above the normal median, the odds of PAS increase by 1.051. However, the study did not define an optimal threshold which can be used as a cutoff point for screening purposes. The ROC curve analysis revealed an area under the curve of 0.826 which could be due higher sample size.5 Li et al obtained similar results as well where 45mm was determined as a threshold for PAS screening with 50% sensitivity and 96% specificity.2 Such higher specificity compared to our study was attributed to a higher proportion of PAS (67.9% of cases) compared to our study (50% of cases). Every effort was made to predict the possible adverse outcomes of PAS before intervention to achieve optimum preoperative preparations. Shazly et al created two models named Middle-East Obstetrics and Gynecology Graduate Education placenta accreta risk-antepartum score (MOGGE PAR-A) and peri-partum score (MOGGE PAR-P) to predict massive blood loss, prolonged hospitalization, and maternal ICU admission associated with PAS by using antenatal and peripartum data from the Placenta accreta spectrum international database (PAS-ID). The diagnostic accuracy of these two models ranged between 80 and 90%.8 The higher AUC compared to our study can be attributed to the higher prevalence of the condition in their study population which is due to its retrospective nature. Moreover, the primary focus of our study was the prediction of PAS in high-risk patients using a simple test which is the placental thickness which differs from the aim of the study conducted by Shazly et al which is the prediction of clinical outcomes in an already diagnosed PAS patients.8
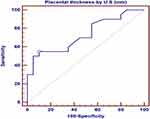 |
Figure 3 ROC curve of placental thickness by ultrasound as a predictor of placenta accreta spectrum. |
There was no significant difference between patients with PAS and patients with no PAS regarding preoperative hemoglobin; this finding indicates that intra-operative blood transfusion was entirely dependent on the haemodymanics and the vital data of the patient during the cesarean section. The number of transfused units of packed RBCs per patient was significantly higher among patients with PAS disorder compared with cases with complete placental separation; we included only intra-operative transfusion as it was guided by the anesthesiologist in charge with a low risk of bias, while postoperative transfusion is usually affected by the vital data of the patient and the surgeon’s preference. Bhide et al showed similar results with 39.3% of the PAS patients required blood transfusion. However, the number of transfused units for each patient was not reported, ie, only qualitative assessment.5 Our results were also similar to those obtained by Kim et al, who developed a scoring system to predict massive hemorrhage in patients with placenta previa totalis; The presence of pathological placental adhesion was significantly associated with massive transfusion i.e. more than 8 units of packed RBCs.9 There was no correlation between certain blood groups and PAS development among the study participants.
Cesarean hysterectomy remains the most widely accepted and preferred approach to PAS according to an Obstetric Care Consensus document developed jointly by the American College of Obstetricians and Gynecologists (ACOG) and the Society for Maternal-Fetal Medicine (SMFM) and endorsed by The Society of Gynecologic Oncology (SGO).10 Among our study participants, only 15% of the patients of the PAS arm underwent conservative management in the form of myometrial resection. The study conducted by Shazly et al included 587 patients with a diagnosis of PAS; uterine conservation was successful in 469 cases (79.9%).10 This high success rate because that most of the study participants had only one previous cesarean section (The median number of previous CS was 1) which is much lower than the median number of previous CS in our PAS patients, which was 4. Besides, 290 out of 587 patients (49.9%) had placenta accreta,11 while among our study participants, 40% of the PAS arm had placenta increta and another 40% had placenta percreta at the histopathological analysis of the hysterectomy specimens. Cırpan et al conducted a retrospective study that evaluated the segmental resection technique in the management of PAS; 21 out of 23 cases (91.3%) were successfully managed with segmental resection. Such a high rate of conservative surgery compared to our study can be attributed to a lower number of previous cesarean sections (the mean number was 1.87). Moreover, the technique was applied to cases where the myometrium is extremely thin with protrusion of the placenta through the defective thin area; this means that cases were carefully selected before performing the technique12 while in our study, the such selection was not present because our primary aim was the prediction of PAS, while the management was influenced by surgeons’ preference and expertise.
Regarding bladder injury, there was no significant difference between patients with PAS and patients without PAS; this might be a reflection of the high experience of the surgeons who performed the procedure. Such experience is due to the high number of cases admitted to our hospital, which is a tertiary centre for referral of such cases from all over Egypt. However, a higher sample size is needed for a better assessment of possible significant difference regarding such complication.
Patients included in the study were asked about the site where previous cesarean section or sections were performed; 80% of the patients with no PAS stated that their past cesarean sections were performed at private hospitals, 5% reported university hospitals, 10% at teaching hospitals and 5% reported both university and private hospitals. Similar percentages were reported by patients having PAS with 80% stated that their sections were carried out at private hospitals, 5% reported teaching hospitals, 10% at both private and teaching hospitals and 5% at both university and private hospitals. Such findings reveal the huge role played by the private sector in providing obstetric services in Egypt and the fact that much more follow-up of obstetric interventions which are carried out at this important sector is needed by health authorities.
Conclusion
Our study showed that there was a significant increase in placental thickness at the lower uterine segment in patients with placenta previa and PAS compared to those with placenta previa but no morbid adherence. Measuring placental thickness is simple and easy to implement. So, it can be used as a screening test for patients with placenta previa, particularly those with a past history of cesarean section and no other uterine surgeries.
Abbreviations
PAS, placenta accreta spectrum; ROC curve, receiver operating characteristic; RBCs, red blood cells; SD, standard deviation; BMI, body mass index; CS, cesarean section; AUC, area under curve; PPV, positive predictive value; NPV, negative predictive value; RCOG, Royal College of Obstetrics and Gynecology; aOR, adjusted Oodds ratio; MOGGE PAR-A, Middle-East Obstetrics and Gynecology Graduate Education placenta accreta risk – antepartum score; MOGGE PAR-P, Middle-East Obstetrics and Gynecology Graduate Education placenta accreta risk – peri-partum score; PAS-ID, Placenta Accreta Spectrum – International Database.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author (A.M. Elmaraghy).
Ethics Approval and Informed Consent
Informed consent was obtained from study participants prior to the initiation of the study. Prior to initiation of publishing process, the study was registered in ClinicalTrials.gov, ID: NCT05500404; and was approved by the Research Ethics Committee, Faculty of Medicine, Ain Shams University (FWA 000017585), approval number: MS 719/2021. All procedures were carried out in accordance with the ethical rules and the principles of the Declaration of Helsinki.
Acknowledgments
We would like to show our gratitude to Professor Dr Amr Elshalakany; Professor of Obstetrics and Gynecology at the Faculty of Medicine, Ain Shams University, for his comments that greatly improved the manuscript. We would also like to thank Dr. Mahmoud Ghaleb and Dr Mohammed Abd ElRazeq who performed the surgeries.
We would also like to thank our colleagues from the Department of Obstetrics and Gynecology at the Faculty of Medicine, Ain Shams University, who provided insight and experience that greatly assisted the research.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was based on the investigator's self-funding.
Disclosure
All authors declare that:
- In the past 3 years, they had not received any funding from any organization that may have a financial interest in the manuscript.
- They do not hold any stock holdings or options in an organization that may have a financial interest in the publication of this manuscript.
- The content of the manuscript is not related to any patents they hold or currently applied for.
- They have not received any funding or salary from organizations that hold or have applied for patents relating to the content of the manuscript.
- They do not have any other financial competing interests.
- They have not received any equipment from an entity that might benefit or be at an advantage financially or reputationally from the published findings.
- They do not hold a position on an industry board or private company that might benefit or be at an advantage financially or reputationally from the published findings.
- They do not have any personal, political, religious, ideological, academic and intellectual competing interests which are perceived to be relevant to the published content.
References
1. Zhang L, Bi S, Du L, et al. Effect of previous placenta previa on outcome of next pregnancy: a 10-year retrospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):212. doi:10.1186/s12884-020-02890-3
2. Li Y, Choi HH, Goldstein R, Poder L, Jha P. Placental thickness correlates with placenta accreta spectrum (PAS) disorder in women with placenta previa. Abdom Radiol. 2021;46(6):2722–2728. doi:10.1007/s00261-020-02894-9
3. Silver RM, Branch DW. Placenta Accreta Spectrum. N Engl J Med. 2018;378(16):1529–1536. doi:10.1056/NEJMcp1709324
4. Jauniaux E, Alfirevic Z, Bhide AG, et al.; Royal College of Obstetricians and Gynaecologists. Placenta praevia and placenta accreta: diagnosis and management: green-top guideline no. 27a. BJOG. 2019;126(1):e1–e48. doi:10.1111/1471-0528.15306
5. Bhide A, Laoreti A, Kaelin Agten A, et al. Lower uterine segment placental thickness in women with abnormally invasive placenta. Acta Obstet Gynecol Scand. 2019;98(1):95–100. doi:10.1111/aogs.13422
6. Jha P, Li Y, Choi HH, Sugi MD, Goldstein R, Poder L. VP46.30: placental thickness as a screening tool for placenta accreta spectrum disorder in women with placenta previa. Ultrasound Obstet Gynecol. 2020;56:275. doi:10.1002/uog.23095
7. Vieira MC, Rijken MJ, Braun T, et al. International Society for Placenta accreta spectrum (IS-PAS). The relation between maternal obesity and placenta accreta spectrum: a multinational database study. Acta Obstet Gynecol Scand. 2021;100(Suppl 1):50–57. doi:10.1111/aogs.14075
8. Shazly SA, Hortu I, Shih JC, et al.; and Middle East Obstetrics and Gynecology Graduate Education (MOGGE), foundation – Artificial intelligence (AI) unit. Prediction of clinical outcomes in women with placenta accreta spectrum using machine learning models: an international multicenter study. J Matern Fetal Neonatal Med. 2022;35(25):6644–6653. doi:10.1080/14767058.2021.1918670
9. Kim JW, Lee YK, Chin JH, et al. Development of a scoring system to predict massive postpartum transfusion in placenta previa totalis. J Anesth. 2017;31(4):593–600. doi:10.1007/s00540-017-2365-8
10. Zuckerwise LC, Craig AM, Newton JM, Zhao S, Bennett KA, Crispens MA. Outcomes following a clinical algorithm allowing for delayed hysterectomy in the management of severe placenta accreta spectrum. Am J Obstet Gynecol. 2020;222(2):179.e1–179.e9. doi:10.1016/j.ajog.2019.08.035
11. Shazly SA, Hortu I, Shih JC, et al. Prediction of success of uterus-preserving management in women with placenta accreta spectrum (CON-PAS score): a multicenter international study. Int J Gynaecol Obstet. 2021;154(2):304–311. doi:10.1002/ijgo.13518
12. Cırpan T, Akdemir A, Okmen F, Hortu I, Ekici H, Imamoglu M. Effectiveness of segmental resection technique in the treatment of placenta accreta spectrum. J Matern Fetal Neonatal Med. 2021;34(19):3227–3233. doi:10.1080/14767058.2019.1702019
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
