Back to Journals » Clinical Interventions in Aging » Volume 16
Development of a Nomogram to Predict Postoperative Transfusion in the Elderly After Intramedullary Nail Fixation of Femoral Intertrochanteric Fractures
Authors Wang J , Zhao Y, Jiang B, Huang X
Received 10 March 2020
Accepted for publication 10 June 2020
Published 6 January 2021 Volume 2021:16 Pages 1—7
DOI https://doi.org/10.2147/CIA.S253193
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Jiqi Wang,1 Youming Zhao,1 Bingjie Jiang,1 Xiaojing Huang2
1Department of Orthopaedics, The Second Affiliated Hospital and Yuying Children’s Hospital of Wenzhou Medical University, Wenzhou 325000, Zhejiang, People’s Republic of China; 2Department of Orthopaedics, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou 325000, Zhejiang, People’s Republic of China
Correspondence: Xiaojing Huang
Department of Orthopaedics, The First Affiliated Hospital of Wenzhou Medical University, Shangcai Village Ouhai District, Wenzhou 325000, Zhejiang, People’s Republic of China
Email [email protected]
Purpose: The aim of our study was to explore the risk factors related to blood transfusion after intramedullary nail fixation of elderly femoral intertrochanteric fracture (FTF) and establish a nomogram prediction model.
Patients and Methods: We conducted a retrospective study including elderly FTF patients treated by intramedullary nail between January 2017 and December 2019. Perioperative information was obtained retrospectively, uni- and multivariate regression analyses were performed to determine risk factors for blood transfusion. A nomogram model was established to predict the risk of blood transfusion, and consistency coefficient (C-index) and correction curve were used to evaluate the prediction performance and consistency of the model.
Results: Of 148 patients, 119 were finally enrolled in the study and and 46 patients (38.7%) received a blood transfusion after the operation. Logistic regression analysis the female, lower preoperative Hb, ASA score > 2, general anesthesia, and higher intraoperative blood loss were independently associated with the blood transfusion. The accuracy of the contour map for predicting transfusion risk was 0.910.
Conclusion: These risk factors are shown on the nomogram and verified. Through the assessment of the risk of blood transfusion and the intervention of modifiable risk factors, we may be able to reduce the blood transfusion rate to a certain extent, so as to further guarantee the safety of the elderly patients during the perioperative period.
Keywords: blood transfusion, femoral intertrochanteric fracture (FTF), elderly, nomograms, risk factors, intramedullary nail fixation
Introduction
Femoral trochanteric fracture (FTF) is one of the common types of hip fracture in elderly patients, which can lead to disability, a decline in quality of life and increased mortality, and has become a serious public health problem.1–3 It is necessary to perform internal fixation for these elderly patients, which will relieve their pain symptoms and improve their quality of life. The choice of internal fixation usually includes a sliding hip screw or intramedullary nail, however, the sliding hip screw cannot provide adequate fixation in unstable fractures, and often leads to malreduction and lag screw cutting.4,5 Thus, in many areas of the world, the intramedullary nail is a more popular method of operation.6
Some patients need blood transfusions after intramedullary nail fixation. A blood transfusion may be a life-saving measure, but it can also lead to transfusion-related complications and increase the risk of bacterial infection and mortality.7–9 Moreover, the hemoglobin threshold of postoperative red cell transfusion is controversial. Foss et al10 reported that there was no significant difference in postoperative rehabilitation score and length of stay between hip fracture patients with a liberal transfusion strategy (a hemoglobin threshold of 10 g per deciliter) or a restrictive transfusion strategy (symptoms of anemia or at physician discretion for a hemoglobin level of <8 g per deciliter), but there were fewer patients with cardiovascular complications and lower mortality in a liberal transfusion strategy. However, Carson et al11 found a liberal transfusion strategy did not reduce the mortality of elderly patients with high cardiovascular risk or could not walk independently or reduce the incidence rate of hospitalization during the 60-day follow-up. Indeed, blood resources are costly and scarce, and are associated with the increased financial burden in the collection, preparation, and administration, thus, our institution adopts a restrictive transfusion strategy. Although elderly patients with FTF cannot completely avoid transfusion after treatment with intramedullary nails, the high-risk factors of postoperative transfusion can be predicted, and the necessary intervention of adjustable risk factors can reduce the demand and rate of postoperative transfusion.
A few studies have explored the risk factors of blood transfusion after intramedullary nail fixation for intertrochanteric fractures in the elderly, but these risk factors are not integrated intuitively. A nomogram is a kind of calculation chart, which can replace complex mathematical formula and integrate more clinical variables to achieve accurate individual prediction. In addition, it provides an easy and reproducible tool to predict the need for blood transfusion, unlike other studies that provided a model that is mathematically more difficult.12 Therefore, we designed this study to explore the risk factors related to blood transfusion after the operation and establish a nomogram prediction model.
Patients and Methods
Patients
This study was approved by the Ethics Committee of our institution. The inclusion criteria were as follows: 1) patients who were older than 65 years; 2) OTA/AO classification 31A-1 and 31A-2 FTF;13 3) no polytrauma and pathological fracture; and 4) no history of hematological diseases. From January 2017 to December 2019, 148 consecutive FTF patients underwent intramedullary nail fixation in our hospital. Of these patients, 29 were excluded: 13 patients’ aged less than 65 years, 4 patients with ineligible fracture patterns, 9 patients with combined fracture, 2 patients with tumor metastasis fracture (lung tumor bone metastasis), and 1 patient had a history of hemophilia. Finally, 119 patients met our inclusion criteria and were enrolled in our study.
We collected sex, age, body mass index (BMI), Injury mechanism (low-energy injuries [falls from standing height] and high-energy injuries [such as traffic accidents and falls from greater heights]), comorbid diseases (hypertension and diabetes), anticoagulant history, preoperative hemoglobin (Hb) value (admission day), time to definitive management, American Society of Anesthesiologists (ASA) scores, type of anesthesia (general anesthesia [GA] or spinal anesthesia [SA]), intraoperative blood loss (IBL, recorded by the anesthesiologist, including the blood in the suction bottle (excluding the lavage fluid used in the operation) and the sponge used in the operation), surgical duration, intraoperative reaming or not, postoperative transfusion volume, postoperative hospital stay, and hospitalization expenses from the hospital electronic medical record (EMR) system.
All patients received standard operation and were fixed by an intramedullary nail (InterTAN, Smith and Nephew Richards, Memphis). Previous studies have shown that compared with restrictive strategies, the liberal transfusion strategy did not reduce mortality or reduce the incidence rate of hospitalization in elderly patients with high cardiovascular risk,11 and due to the shortage of blood resources, our institution adopts a restrictive strategy of blood transfusion, i.e., symptoms of anemia or at physiological variation for a hemoglobin level of < 8 g per deciliter.
Statistical Analysis
The statistical analyses were performed using SPSS for Windows software (ver. 19.0; SPSS Inc., Chicago, IL, USA). Means were compared using the independent samples t-test for normally distributed variables; otherwise, the Mann–Whitney U-test was used for group comparisons, and qualitative variables were compared using the chi-square test. Univariate analysis was used to assess the association between different factors and the blood transfusion. Then multivariate logistic regression was performed to control for confounding effects. Predictor exclusion was continued until all predictors had p values less than 0.05, which was then defined as the final prediction model. The final risk factors were incorporated into R3.6.1 software (R Foundation for Statistical Computing, Vienna, Austria) to establish a nomogram prediction model. The consistency index (c-index) was used to evaluate the prediction performance of the model, and the correction curve was used to judge the prediction consistency. The range of C-index value was 0.5 to 1.0, and accuracy was positively correlated with value. The calibration curve included image comparison of predicting risk and patients’ transfer risk. The closer the predicted risk to the standard curve, the better the conformity of the model was. The level of significance was set at 0.05 for all analyses.
Results
In total, 119 patients were included in this study, and 46 patients (38.7%) received a blood transfusion after the operation. The comparison of the baseline characteristics between those patients (see Table 1) revealed that there was no statistical difference with age, comorbid diseases, injury mechanism, surgical duration, and intraoperative reaming. Compared with the patients who did not receive postoperative blood transfusions, the proportion of female, anticoagulant history, ASA score III and received general anesthesia was higher in transfusion group, and the preoperative hemoglobin of patients in the blood transfusion group was lower, the amount of intraoperative blood loss was higher, the time to definitive management, the postoperative hospital stay, and the hospitalization expenses were significantly increased. There was no serious blood transfusion reaction occurred after blood transfusion, and no thrombotic event occurred postoperatively. The number of superficial infection patients were 1 and 5 in non-transfused group and transfused group, respectively, and all of them healed after the use of intravenous antibiotics and wound dressing.
 |
Table 1 Comparison of Baseline Characteristics of Two Groups |
In the univariate analyses the following were significantly associated with blood transfusions: sex, anticoagulant history, preoperative Hb, time to definitive management, ASA score, type of anesthesia, and intraoperative blood loss (Table 2). Multivariate logistic regression analysis the female, lower preoperative Hb, ASA score > 2, general anesthesia, and higher intraoperative blood loss were independently associated with the blood transfusion and constituted the final model (Table 3). A nomogram was established to predict the risk of blood transfusion (Figure 1). The total score of the prognosis index is obtained by the sum of the scores of every single item, while the probability of postoperative blood transfusion is obtained by the total score. For example, for a female patient, the preoperative hemoglobin value was 120 g/L, the preoperative ASA score was level II, she received general anesthesia during the operation, and the intraoperative blood loss was about 300 mL. According to our nomogram evaluation, the probability of receiving a blood transfusion was approximately 80%. The C-index of the model was 0.910 after 1000 bootstrap self-sampling replicates, which indicated that the consistency between the predicted value and the actual observation value is in accordance with the standard and has standard resolution. Figure 2 shows the calibration curve. The average absolute error of the coincidence between the predicted value and real value was 0.054. The predicted risk is close to the actual risk and in good coincidence.
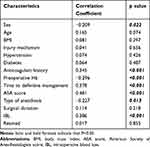 |
Table 2 Univariate Analysis Results Related to Blood Transfusion |
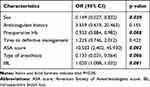 |
Table 3 Multivariate Analysis Results Related to Blood Transfusion |
 |
Figure 1 A nomogram to predict the incidence of blood transfusions after intramedullary nail fixation of femoral intertrochanteric fractures. |
 |
Figure 2 Calibration curve for nomogram prediction of blood transfusions after intramedullary nail fixation of femoral intertrochanteric fractures. |
Discussion
It has been known for a long time that blood transfusions have a down-regulation effect on the immune system, resulting in low reactivity and alloimmunity to various blood cells or plasma antigens.14 Down regulation of immune response usually leads to an increase in postoperative infection rate, such as superficial wound infection and urinary tract infection.15,16 In addition, blood transfusions may also cause transfusion reaction (such as shivering and high fever), prolong the length of stay, increase the cost of treatment, and possibly increase mortality rates.17 The influence of allogeneic transfusion on the patients has been reported in a large number of literatures, and it is more serious in the elderly patients with poor general conditions. FTF is a common hip fracture in elderly patients, and a large number of patients need a blood transfusion after an intramedullary nail fixation.18,19 Therefore, it is necessary to explore the risk factors of blood transfusions after internal fixation of the FTF, establish an intuitive and accurate prediction model, and give reasonable perioperative intervention, so as to reduce the blood transfusion rate to a certain extent.
Our preliminary data showed a correlation between blood transfusion requirement and sex, preoperative Hb, ASA score, type of anesthesia, and intraoperative blood loss. Our results were consistent with previous research reports,20 preoperative Hb was an independent risk factor for postoperative blood transfusion, and was negatively related to the risk of blood transfusion. In our study, preoperative Hb was 108.00 ± 16.92 g/L in the transfused group and 121.40 ± 13.49 g/L in the non-transfused group (p < 0.001). Adunsky et al21 studied the clinical data of 302 patients with hip fracture and believed that preoperative Hb value lower than 120 g/L would increase the risk of postoperative blood transfusion by 5 times. Previous studies have debated whether the ASA score affects postoperative blood transfusion. On the one hand, Desai et al7 believed that the higher the ASA score, the higher the postoperative blood transfusion rate, while some studies indicated that there was no correlation between the ASA score and the postoperative blood transfusion rate.20 Our results showed that ASA was an independent risk factor for blood transfusion, and was positively correlated with the risk of blood transfusion. We believe that only elderly patients over 65-years-old were included in our study, their general conditions were relatively poor, and the corresponding basic diseases were also more. On this basis, the ASA score had clinical significance in predicting the risk of blood transfusion. Patients who received general anesthesia during the operation had an increased risk of blood transfusion, which was consistent with the results of Basques et al22 who believed that general anesthesia was a high-risk factor for blood transfusion. We considered that this might be related to the following factors. First, there was a difference in hemodynamics between general anesthesia and spinal anesthesia. Patients with high blood pressure during general anesthesia surgery might increased blood loss and blood transfusion risk.23 Secondly, anesthetic gas used in general anesthesia (mixed with nitrous oxide) might inhibit erythrocyte production during the endogenous recovery of erythrocytes.24 Finally, hypothermia during general anesthesia might lead to coagulation disorders and might increased the patient’s blood transfusion needs.25 In addition, we found that the larger the intraoperative blood loss, the higher the risk of postoperative transfusion. Intramedullary nail implantation usually required reaming, which would lead to blood loss and red blood cell destruction. However, there was no significant relationship between blood transfusion risk and reaming. We considered that the blood transfusion demand after an operation might be related to the effective blood volume lost by patients, including the intraoperative blood loss and the hidden blood loss during the perioperative period.26,27 Under the standard operation, more intraoperative blood loss might lead to the increase of the effective blood volume loss, thus increasing the blood transfusion risk after operation.
There was no correlation found with anticoagulant history or time to definitive management in our study. However, Kadar et al12 reviewed the possibility of blood transfusion within 72 hours after admission in 1484 patients with hip fracture, and found that there was a correlation between blood transfusion and coagulation status. We think that the reason for this deviation may be that in our institution, for patients with a long history of oral anticoagulants, we routinely follow the consultation advice of anesthesiologists, stopping anticoagulants before the operation and injecting low molecular weight heparin (LMWH) sodium subcutaneously for 5–7 daysmight affect the patient’s blood coagulation status. Prolonged time to definitive management has been shown to increase mortality, postoperative infection, and hospital stay.28–30 However, there was no relationship between the time to definitive management and the requirement of blood transfusion in our study, which might be related to the stability of hematoma at the fracture site and the reduction of preoperative active hemorrhage to the greatest extent.
There are few reports about the risk factors of blood transfusion after intramedullary nail fixation of FTF in the literature, and no studies have shown the visual manifestation of these risk factors in the nomogram. Compared with the traditional multiple regression model, the nomogram can display all the key prediction factors in a graphical way. Our nomogram can enable clinicians to better assess the risk of patients receiving blood transfusion postoperatively, so as to make necessary interventions (such as improving the Hb of patients before operation, giving spinal anesthesia as often as possible, and minimizing intraoperative blood loss, etc.), so as to reduce the incidence of blood transfusion.
There are limitations to our study that should be considered. Firstly, we performed a retrospective analysis, and the samples in our study were relatively small, which cannot rule out the effect of other potential factors on the results (i.e., osteoporosis and bone mineral density), thus, further prospective study with larger samples are required to validate our findings; Secondly, early functional outcomes and long-term follow-up data were lacking, inclusion of such data would have improved our study; Finally, our nomogram model has only been validated internally, and still needs to be validated externally.
Conclusion
We found a correlation between blood transfusion requirement and sex, preoperative Hb, ASA score, type of anesthesia, and intraoperative blood loss. Moreover, these risk factors are shown on the nomogram and verified. Through the assessment of the risk of blood transfusion and the intervention of modifiable risk factors, we may be able to reduce the blood transfusion rate to a certain extent, so as to further guarantee the safety of the elderly patients during the perioperative period.
Data Sharing Statement
The datasets analyzed in the study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This retrospective study was approved by the Ethics Committee of Second Affiliated Hospital of Wenzhou Medical University, and all participants provided informed consent prior to data collection.
Acknowledgments
The authors thank all the colleagues for their valuable assistance during the implementation of this study.
Funding
There is no funding to report.
Disclosure
All authors report no conflicts of interest in this work.
References
1. Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord. 2018;19:369. doi:10.1186/s12891-018-2276-3
2. Hartholt KA, van Beeck EF, Polinder S, et al. Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. J Trauma. 2011;71:748–753. doi:10.1097/TA.0b013e3181f6f5e5
3. Lobo-Escolar A, Joven E, Iglesias D, Herrera A. Predictive factors for cutting-out in femoral intramedullary nailing. Injury. 2010;41:1312–1316. doi:10.1016/j.injury.2010.08.009
4. Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American board of orthopaedic surgery database. J Bone Joint Surg. 2008;90:700–707. doi:10.2106/jbjs.g.00517
5. Dunn J, Kusnezov N, Bader J, et al. Long versus short cephalomedullary nail for trochanteric femur fractures (OTA 31-A1, A2 and A3): a systematic review. J Orthop Traumatol. 2016;17:361–367. doi:10.1007/s10195-016-0405-z
6. Matre K, Havelin LI, Gjertsen J-E, et al. Sliding hip screw versus IM nail in reverse oblique trochanteric and subtrochanteric fractures. A study of 2716 patients in the Norwegian hip fracture register. Injury. 2013;44:735–742. doi:10.1016/j.injury.2012.12.010
7. Desai SJ, Wood K, Marsh J, et al. Factors affecting transfusion requirement after hip fracture: can we reduce the need for blood? Can J Surg. 2014;57:342–348. doi:10.1503/cjs.030413
8. Hill GE, Frawley WH, Griffith KE, Forestner JE, Minei JP. Allogeneic blood transfusion increases the risk of postoperative bacterial infection: a meta-analysis. J Trauma. 2003;54:908–914. doi:10.1097/01.ta.0000022460.21283.53
9. Vincent JL, Baron JF, Reinhart K, et al. Anemia and blood transfusion in critically ill patients. JAMA. 2002;288:1499–1507. doi:10.1001/jama.288.12.1499
10. Foss NB, Kristensen MT, Jensen PS, et al. The effects of liberal versus restrictive transfusion thresholds on ambulation after hip fracture surgery. Transfusion. 2009;49:227–234. doi:10.1111/j.1537-2995.2008.01967.x
11. Carson JL, Terrin ML, Noveck H, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365:2453–2462. doi:10.1056/NEJMoa1012452
12. Kadar A, Chechik O, Steinberg E, Reider E, Sternheim A. Predicting the need for blood transfusion in patients with hip fractures. Int Orthop. 2013;37:693–700. doi:10.1007/s00264-013-1795-7
13. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium - 2007: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma. 2007;21:S1–133. doi:10.1097/00005131-200711101-00001
14. Johnston P, Wynn-Jones H, Chakravarty D, Boyle A, Parker MJ. Is perioperative blood transfusion a risk factor for mortality or infection after hip fracture? J Orthop Trauma. 2006;20:675–679. doi:10.1097/01.bot.0000249435.25751.e8
15. Brunskill SJ, Millette SL, Shokoohi A, et al. Red blood cell transfusion for people undergoing hip fracture surgery. Cochrane Database Syst Rev. 2015;4:Cd009699. doi:10.1002/14651858.CD009699.pub2
16. Gregersen M, Damsgaard EM, Borris LC. Blood transfusion and risk of infection in frail elderly after hip fracture surgery: the TRIFE randomized controlled trial. Eur J Orthop Surg Traumatol. 2015;25:1031–1038. doi:10.1007/s00590-015-1609-2
17. Hart A, Khalil JA, Carli A, et al. Blood transfusion in primary total hip and knee arthroplasty. Incidence, risk factors, and thirty-day complication rates. J Bone Joint Surg. 2014;96:1945–1951. doi:10.2106/jbjs.n.00077
18. Sellan M, Bryant D, Tieszer C, et al. Short versus long interTAN fixation for geriatric intertrochanteric hip fractures: a multicentre head-to-head comparison. J Orthop Trauma. 2019;33:169–174. doi:10.1097/bot.0000000000001409
19. Temiz A, Durak A, Atici T. Unstable intertrochanteric femur fractures in geriatric patients treated with the DLT trochanteric nail. Injury. 2015;46(Suppl 2):S41–46. doi:10.1016/j.injury.2015.05.031
20. Dillon MF, Collins D, Rice J, et al. Preoperative characteristics identify patients with hip fractures at risk of transfusion. Clin Orthop Relat Res. 2005;439:201–206. doi:10.1097/01.blo.0000173253.59827.7b
21. Adunsky A, Lichtenstein A, Mizrahi E, Arad M, Heim M. Blood transfusion requirements in elderly hip fracture patients. Arch Gerontol Geriatr. 2003;36:75–81. doi:10.1016/s0167-4943(02)00059-6
22. Basques BA, Bohl DD, Golinvaux NS, Samuel AM, Grauer JG. General versus spinal anaesthesia for patients aged 70 years and older with a fracture of the hip. Bone Joint J. 2015;97-b:689–695. doi:10.1302/0301-620x.97b5.35042
23. Modig J. Regional anaesthesia and blood loss. Acta Anaesthesiol Scand. 1988;32(Supplementum 89):44–48. doi:10.1111/j.1399-6576.1988.tb02842.x
24. Borghi B, Casati A, Iuorio S, et al. Frequency of hypotension and bradycardia during general anesthesia, epidural anesthesia, or integrated epidural-general anesthesia for total hip replacement. J Clin Anesth. 2002;14:102–106. doi:10.1016/s0952-8180(01)00362-2
25. Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. 2008;109:318–338. doi:10.1097/ALN.0b013e31817f6d76
26. Sehat KR, Evans RL, Newman JH. Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg. 2004;86:561–565. doi:10.1302/0301-620X.86B4.14508
27. Sehat KR, Evans R, Newman JH. How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee. 2000;7:151–155. doi:10.1016/s0968-0160(00)00047-8
28. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg. 2005;87:483–489. doi:10.2106/jbjs.d.01796
29. Verbeek DO, Ponsen KJ, Goslings JC, Heetveld MJ. Effect of surgical delay on outcome in hip fracture patients: a retrospective multivariate analysis of 192 patients. Int Orthop. 2008;32:13–18. doi:10.1007/s00264-006-0290-9
30. Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291:1738–1743. doi:10.1001/jama.291.14.1738
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
