Back to Journals » International Journal of Women's Health » Volume 14
Development of a Nomogram for Predicting Intravasation Before Transvaginal 4-Dimensional Hysterosalpingo-Contrast Sonography
Authors Jin Y , Huang W, Qv Q, Liu S
Received 23 January 2022
Accepted for publication 14 April 2022
Published 21 April 2022 Volume 2022:14 Pages 583—591
DOI https://doi.org/10.2147/IJWH.S359467
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Everett Magann
Yi Jin, Wendi Huang, Qinhong Qv, Shuling Liu
Department of Ultrasound Imaging, the First People’s Hospital of Wenling, Wenling City, Zhejiang Province, People’s Republic of China
Correspondence: Yi Jin, Department of Ultrasound Imaging, the First People’s Hospital of Wenling, No. 333, Chuan’an South Road, Chengxi Street, Wenling, Zhejiang Province, People’s Republic of China, Post Code: 317500, Tel +86-13586226622, Email [email protected]
Background: Intravasation during transvaginal 4-dimensional hysterosalpingo-contrast sonography (TVS 4D-HyCoSy) may lead to false-negative results in tubal patency evaluation. Although the influencing factors associated with intravasation have been investigated, some factors are only identified during 4D-HyCoSy, thus currently no studies on preventing intravasation. However, several preprocedural features can be collected in advance, which may be valuable in predicting intravasation.
Objective: The purpose of this study is to establish a nomogram incorporating the preprocedural features to predict the risk of intravasation before TVS 4D-HyCoSy.
Methods: The data of 276 infertile women with patent fallopian tubes were analyzed retrospectively. They were assigned to the study group (n = 62) and the control group (n = 214) according to the development of intravasation. The preprocedural characteristics were collected to investigate the predictors independently associated with intravasation, which were then served as the construction of a nomogram. The performance of the nomogram was verified internally.
Results: History of uterine curettage (OR = 2.341, P = 0.009), endometrial thickness (OR = 0.587, P < 0.001), and examination schedule (OR = 0.790, P = 0.024) were found to be the independent influencing factors associated with intravasation. The established nomogram incorporating these preprocedural features was useful for predicting the risk of intravasation prior to 4D-HyCoSy. It yielded net benefits when the predicted probability was less than 50%.
Conclusion: The nomogram incorporating the preprocedural characteristics achieved a net benefit for clinical decision-making when the estimated risk was less than 50%. It is recommended to change the examination schedule for patients with an estimated risk greater than 50% and perform 4D-HyCoSy when the risk is less than 50%.
Keywords: intravasation, TVS 4D-HyCoSy, nomogram, preprocedural characteristics, tubal patency
Introduction
Fallopian tube injury is a prevalent cause of female infertility, which affects roughly 20% of infertile women.1 Tubal patency test is critical for determining the reasons of infertility and choosing the optimal treatment. Transvaginal 4-dimensional hysterosalpingo-contrast sonography (TVS 4D-HyCoSy), a multi-dimensional imaging method that observes ultrasound contrast agents filling in the uterine cavity and fallopian tubes, and then diffusing in the pelvic cavity in real time, is proved to effectively assess tubal patency without requiring hospitalization.2–5 Because of its safety and non-radiation, s4D-HyCoSy is growing to be an attractive screening technique for fallopian occlusion as an alternative to hysterosalpingography.6 However, due to the tiny volume of ultrasonic contrast agents, they tend to diffuse to the myometrium and pelvic venous plexus via abnormal routes to affect the display of uterine cavity and fallopian tubes, which is called intravasation.7,8 Intravasation will result in reticular patterns and multiple thin lines that ultimately lead to false assumptions in diagnosis.9–11 According to the latest published studies, the incidence of intravasation ranged from 13.04% to 26.28% in the process of TVS 4D-HyCoSy,10,12 which was much higher than that in hysterosalpingography (6.9% to 7.2%).13,14 Thus, prevention of intravasation is critical for the assessment of tubal patency in women presenting with infertility.
To the best of our knowledge, intravasation is associated with endometrial thickness, examination schedule, secondary infertility, clinical history (such as abortion, intrauterine surgery, and ectopic pregnancy), fallopian occlusion, pain, and improper operation.10,12,13 However, understanding the influencing factors has no effect on the prevention of intravasation. This is due to the lack of studies currently available to predict the risk of intravasation prior to 4D-HyCoSy. Although fallopian occlusion, which has been demonstrated to be the most important influencing factor, cannot be determined before 4D-HyCoSy, several preprocedural features such as endometrial thickness, examination schedule, and clinical history can be collected in advance.
To avoid the impact of fallopian occlusion, the purpose of this study was to analyze the characteristics of patients with intravasation but patent fallopian tubes, and to establish a nomogram model to predict the risk of intravasation prior to TVS 4D-HyCoSy. It may provide more individual strategies to avoid the occurrence of intravasation.
Materials and Methods
This study was approved by the institutional review board of the First People’s Hospital of Wenling (KY-2021-1016-01). Informed consents were obtained from all participants. It was planned in accordance with the Declaration of Helsinki.
Patients
The medical records of 416 infertile patients who underwent TVS 4D-HyCoSy between April 2019 and December 2021 in our center were retrospectively analyzed. Infertility is defined as the inability to achieve a clinical pregnancy in 12 months of unprotected relationships. The included patients were free of contraindications for HyCoSy, including vaginal hemorrhage, acute sexually transmitted disease, genital system inflammation, sulphur hexafluoride allergy, and abnormal fallopian tubes caused by hydrosalpinx or ectopic pregnancy. Patients with occluded fallopian tubes (unilaterally or bilaterally) were excluded due to the requirement of the study design.
Finally, 276 women with patent fallopian tubes were enrolled in this study. Women whose fallopian tubes were unobstructed but the contrast agents do not move through the tube smoothly were included as well.2 Women without intravasation (n = 214) were assigned to the control group, while those with intravasation were assigned to the study group (n = 62). Clinical data prior to TVS 4D-HyCoSy including age, infertility duration, infertility type (primary/secondary), endometrial thickness, examination schedule (clean day after menstruation), intrauterine lesions, and history of uterine curettage, pelvic surgery, and pelvic inflammatory disease were collected.
TVS 4D-HyCoSy
Tubal patency test was performed using the Voluson E10 (GE Healthcare, Zipf, Austria) ultrasound system with a RIC 5-9-D volume probe (5–9 MHz) and a dedicated contrast-imaging software. All measurements were performed by 2 ultrasound physicians experienced in the use of TVS 4D-HyCoSy. The procedure was performed between the third and tenth days after their last menstrual period. Prior to 4D-HyCoSy, the reproductive system was initially evaluated by transvaginal 2D and 3D sonography, and the uterine endometrial thickness was measured. After the balloon catheter was confirmed, the 4D-HyCoSy mode was activated after positioning the probe at the level of the sectional plane of the uterus to display bilateral uterine horns and surrounding tissues. SonoVue contrast agent (SonoVue, Bracco International BV, Amsterdam, the Netherlands) was made by mixing 59 mg of SonoVue freeze-dried powder with 5 mL of 0.9% saline solution. The SonoVue solution was then diluted into a 15-mL suspension with 0.9% sterile saline solution and injected into the uterus. The contrast-enhanced volume images were saved as 4D cine clips without 2D image reconstruction. The tubal patency was assessed by playing back the 4D imaging videos, while observing whether the intravasation progressed to the myometrium or venous plexus.
Characteristics of Intravasation
Intravasation near the myometrium appears as a strong echo near the myometrium after the formation of uterine cavity, with characteristics of “spot like”, “mesh like”, or “cloud like” in volume images (Figure 1A). With respect to the intravasation in the venous plexus, cord or “net like” echo amplification was observed around the uterus (Figure 1B).
Nomogram Establishment
The preprocedural characteristics of infertile women were compared in the study and control groups (univariate analysis). The variables that were statistically significant in the univariate analysis were included in the multivariate Logistic regression model to investigate the predictors independently associated with intravasation. By assigning each predictor a number with a weight equal to the odds ratios (OR) value from the multivariate Logistic regression model, we established a nomogram to determine the likelihood of intravasation prior to TVS 4D-HyCoSy. The performance of the nomogram was verified internally.
Statistical Analyses
Continuous data were expressed as median (25,75 percentiles) when they are skewed distributed, and the Mann–Whitney U-test was used. Categorical data were analyzed using the Chi-squared test. The nomogram model was composed of the independent predictors and their odds ratios (OR) calculated by the multivariate Logistic regression. For the verification of the nomogram, a bootstrap resampling (1000 times) analysis was applied. The C-index and Hosmer-Lemeshow (HL) test were used to assess the discrimination and calibration of the nomogram. The receiver operating characteristic (ROC) curve and the calibration curve were used to show their distribution. The clinical net benefits were assessed using decision curve analysis (DCA). The statistical analyses were performed using IBM SPSS Statistics 22.0 (IBM Corp., Armonk, NY, USA), MedCalc (Version 22.0.1; MedCalc Software, Ostend, Belgium), and R package version 3.6.2.
Results
Comparison of the Preprocedural Characteristics in Patients with or without Intravasation
Contrast intravasation was observed in 62 of 276 women with patent fallopian tubes, representing an overall incidence of 22.5%. Table 1 summarizes the preprocedural characteristics in patients between the study and control groups. Intravasation was associated with infertility type, examination schedule, endometrial thickness, and history of uterine curettage (all P < 0.05). There were no significant differences in age, infertility duration, intrauterine lesions, and history of pelvic surgery and pelvic inflammatory disease (all P > 0.05).
 |
Table 1 Comparison of Clinical Data Prior to TVS 4D-HyCoSy Between the Control and Study Groups |
Independent Predictors Associated with Intravasation
Multivariate Logistic analysis further revealed that history of uterine curettage (OR = 2.341, P = 0.009), endometrial thickness (OR = 0.587, P < 0.001), and examination schedule (OR = 0.790, P = 0.024) were found to be the independent influencing factors associated with intravasation (Figure 2). There was no correlation between infertility type and intravasation (P = 0.134), although secondary infertility was more likely to cause intravasation than primary infertility.
Nomogram Development
Based on these independent predictors, a nomogram was constructed to predict the likelihood of intravasation prior to TVS 4D-HyCoSy (Figure 3). The estimated risk of intravasation was calculated by summing the scores of each predictor, with the weight equal to the OR value from the multivariate Logistic regression model.
Nomogram Verification
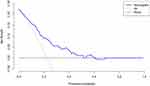
The overfitting-corrected C-index obtained after 1000 bootstrapping in the verification was 0.765 (95% CI: 0.710–0.814), indicating an acceptable discrimination. The calibration test demonstrated no significant difference between the predicted and actual likelihood of intravasation (χ2 = 3.328, P = 0.912), indicating good calibration. Figure 4A and B display the ROC curve and calibration curve for analyzing the discrimination and calibration of the nomogram. However, the DCA revealed that the nomogram yielded clinical net benefit only when the threshold probability was less than 0.5 (Figure 5).
Discussion
Intravasation in 4D-HyCoSy may affect the identification of the fallopian tube, resulting in false-negative results in the evaluation of tubal patency.9 Accurate prediction of intravasation prior to TVS 4D-HyCoSy may avoid re-evaluation due to the failure of tubal patency test. In the present study, we established a nomogram incorporating the preprocedural features (endometrial thickness, examination schedule, and history of uterine curettage) to predict the risk of intravasation in patients with patent fallopian tubes. To our knowledge, this is the first study to estimate the likelihood of intravasation prior to TVS 4D-HyCoSy via a prediction model. Despite the fact that this model excluded data of fallopian occlusion, which was the most critical influencing factor that could not be determined before 4D-HyCoSy, the nomogram yet yielded net benefits when the predicted probability was less than 50%. It suggested that it might become a triage test for infertile women to prevent intravasation as much as possible in 4D-HyCoSy.
Although contrast intravasation seldom results in serious complications (such as embolization), it is necessary to minimize intravasation in the tubal patency test. The development of intravasation depends on the preprocedural and procedural factors.13 The primary influencing factor of intravasation, according to the reported studies, is increased intrauterine pressure induced by fallopian occlusion.11,15,16 However, they are only of limited benefit in preventing intravasation because they cannot be identified in advance. On the other hand, the investigation of preprocedural factors of intravasation helps to minimize the occurrence of intravasation. Our study therefore purposely analyzed the characteristics of patients with patent fallopian tubes to avoid the effect of fallopian occlusion on intravasation. In the present study, we found that intravasation during 4D-HyCoSy was observed in 22.5% of women with patent fallopian tubes. It meant that identifying and improving the preprocedural factors of these patients was expected to reduce the likelihood of intravasation.
Endometrial thickness, examination schedule, and history of uterine curettage were revealed to be the independent predictors of intravasation prior to 4D-HyCoSy in this investigation. Among them, endometrial thickness and examination schedule were recognized influencing factors, which were also reported in the studies by Shi et al and Wang et al10,12 It is known that endometrial dating is related to endometrial maturation during menstrual cycles.17,18 In patients with regular cycles, 4D-HyCoSy should be administered at 3 to 10 days after the menstrual cycle.19,20 However, it is unreliable in individuals with irregular menstruation, and individual variances contribute to a wide range of endometrial thickness. If the endometrium is thin and has not been fully repaired, it is easy to cause intravasation during HyCoSy. Endometrial thickness was found to be associated with vascular permeability in histopathologic studies. The exposure of microvessels to the contrast agents may increase the risk of contrast agents penetrating into the myometrium and venous plexus due to incomplete repair of periodically stripped endometrium.21,22 History of uterine curettage is the third independent predictor obtained in this study. Uterine curettage may induce endometrial injury, increasing the likelihood of some complications such as reproductive tract infection and intrauterine adhesions, which result in intravasation due to the high intrauterine pressure.23 Curettage, on the other hand, can easily damage the basal layer of endometrium, resulting in contrast agents infiltrating the venous plexus through the injured blood vessels.24
In the verification experiment, the established nomogram showed strong calibration. Although the discrimination of the nomogram was only 0.765 due to the absence of an important predictor - fallopian occlusion, the nomogram was still useful for predicting intravasation. DCA revealed that when the anticipated risk was less than 50%, the prediction of the nomogram could achieve a net benefit for clinical decision-making. It suggests that the nomogram including preprocedural features is only suitable for predicting the negative outcome of intravasation. For example, a 30-year-old infertile woman with a history of uterine curettage is planned to receive TVS 4-D HyCoSy. Her endometrial thickness and examination schedule are 6 mm and the 5th day, respectively. The total score of the nomogram is about 110, which indicates that the risk of intravasation is less than 40%. TVS 4D-HyCoSy is advised for this patient. However, if the estimated risk is greater than 50%, it is recommended to adjust the schedule and perform 4D-HyCoSy when the risk is less than 50%.
Two limitations in this study have to be considered. First, it is a retrospective study that only included patients with patent fallopian tubes, which inevitably leads to selection bias. Second, only internal validation was performed in this study (with no external validation yet due to the limitations of the retrospective study). A large-scale prospective validation study is required to validate the prediction model.
Conclusion
We established a nomogram incorporating the preprocedural characteristics (endometrial thickness, examination schedule, and history of uterine curettage) to predict the likelihood of intravasation prior to TVS 4D-HyCoSy. The nomogram achieved a net benefit for clinical decision-making when the estimated risk was less than 50%. It is recommended to change the schedule for patients with an estimated risk of more than 50% and perform 4D-HyCoSy when the risk is less than 50%.
Data Sharing Statement
The data during the current study are available from the corresponding author on reasonable request.
Ethical Approval
Ethical approval for the study was obtained from the ethics committee of the First People’s Hospital of Wenling (KY-2021-1016-01).
Informed Consent
Informed consents were obtained from all participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Study design: Yi Jin and Wendi Huang.
Data collection and analysis: Yi Jin, Wendi Huang, Qinhong Qv, and Shuling Liu.
Supervision: Yi Jin.
Statistics: Wendi Huang, Qinhong Qv, and Shuling Liu.
Manuscript writing: Yi Jin, Wendi Huang, Qinhong Qv, and Shuling Liu.
Manuscript revision: Yi Jin and Wendi Huang.
Approval of the manuscript: all authors.
Funding
Social Development Science and Technology Project of Wenling City (2021S00220).
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. National Collaborating Centre for Ws, Children’s H. National Institute for Health and Clinical Excellence: Guidance. Fertility: Assessment and Treatment for People with Fertility Problems. London: Royal College of Obstetricians & Gynaecologists Copyright © 2013, National Collaborating Centre for Women’s and Children’s Health; 2013.
2. He Y, Geng Q, Liu H, Han X. First experience using 4-dimensional hysterosalpingo-contrast sonography with SonoVue for assessing fallopian tube patency. J Ultrasound Med. 2013;32(7):1233–1243. doi:10.7863/ultra.32.7.1233
3. Alcázar JL, Martinez-Astorquiza Corral T, Orozco R, Dominguez-Piriz J, Juez L, Errasti T. Three-Dimensional Hysterosalpingo-Contrast-Sonography for the Assessment of Tubal Patency in Women with Infertility: a Systematic Review with Meta-Analysis. Gynecol Obstet Invest. 2016;81(4):289–295. doi:10.1159/000443955
4. Wang Y, Qian L. Three- or four-dimensional hysterosalpingo contrast sonography for diagnosing tubal patency in infertile females: a systematic review with meta-analysis. Br J Radiol. 2016;89(1063):20151013. doi:10.1259/bjr.20151013
5. Wang W, Zhou Q, Gong Y, Li Y, Huang Y, Chen Z. Assessment of Fallopian Tube Fimbria Patency With 4-Dimensional Hysterosalpingo-Contrast Sonography in Infertile Women. J Ultrasound Med. 2017;36(10):2061–2069. doi:10.1002/jum.14244
6. Yu J, Cai M, Liang W, Deng Z, Xie Y. Diagnostic efficacy of 3-D hysterosalpingo-contrast sonography in the detection of tubal occlusion: systematic meta-analysis. J Obstet Gynaecol Res. 2015;41(9):1418–1425. doi:10.1111/jog.12728
7. Luo MH, Yeh CK, Situ B, Yu JS, Li BC, Chen ZY. Microbubbles: a Novel Strategy for Chemotherapy. Curr Pharm Des. 2017;23(23):3383–3390. doi:10.2174/1381612823666170113092148
8. Chen ZY, Wang YX, Zhao YZ, et al. Apoptosis induction by ultrasound and microbubble mediated drug delivery and gene therapy. Curr Mol Med. 2014;14(6):723–736. doi:10.2174/1566524014666140804165245
9. Ludwin A, Ludwin I, Martins WP. Venous intravasation during evaluation of tubal patency by ultrasound contrast imaging. Ultrasound Obstet Gynecol. 2018;51(1):143–145. doi:10.1002/uog.17405
10. Shi J, Li S, Wu H, et al. The Influencing Factors of Venous Intravasation During Transvaginal Four-dimensional Hysterosalpingo-contrast Sonography With SonoVue. Ultrasound Med Biol. 2019;45(9):2273–2280. doi:10.1016/j.ultrasmedbio.2019.05.003
11. He Y, Wu H, Xiong R, et al. Intravasation Affects the Diagnostic Image Quality of Transvaginal 4-Dimensional Hysterosalpingo-Contrast Sonography With SonoVue. J Ultrasound Med. 2019;38(8):2169–2180. doi:10.1002/jum.14914
12. Wang W, Zhou Q, Zhou X, Chen Z, Zhang H. Influence Factors on Contrast Agent Venous Intravasation During Transvaginal 4-Dimensional Hysterosalpingo-Contrast Sonography. J Ultrasound Med. 2018;37(10):2379–2385. doi:10.1002/jum.14594
13. Dusak A, Soydinc HE, Onder H, et al. Venous intravasation as a complication and potential pitfall during hysterosalpingography: re-emerging study with a novel classification. J Clin Imaging Sci. 2013;3:67. doi:10.4103/2156-7514.124105
14. Nunley WC, Bateman BG, Kitchin JD 3rd, Pope TL. Intravasation during hysterosalpingography using oil-base contrast medium–a second look. Obstet Gynecol. 1987;70(3 Pt 1):309–312.
15. Chang MC, Shim JJ. Venous intravasation: a potential pitfall of confirmatory hysterosalpingogram following essure hysteroscopic sterilization. J Radiol Case Rep. 2012;6(9):18–22. doi:10.3941/jrcr.v6i9.1106
16. Bhoil R, Sood D, Sharma T, et al. Contrast Intravasation During Hysterosalpingography. Pol J Radiol. 2016;81:236–239. doi:10.12659/pjr.896103
17. Ng EH, Chan CC, Tang OS, Yeung WS, Ho PC. Endometrial and subendometrial blood flow measured during early luteal phase by three-dimensional power Doppler ultrasound in excessive ovarian responders. Hum Reprod. 2004;19(4):924–931. doi:10.1093/humrep/deh205
18. van der Gaast MH, Macklon NS, Beier-Hellwig K, et al. The feasibility of a less invasive method to assess endometrial maturation–comparison of simultaneously obtained uterine secretion and tissue biopsy. Bjog. 2009;116(2):304–312. doi:10.1111/j.1471-0528.2008.02039.x.
19. Practice AIUM. Guideline for the Performance of Sonohysterography. J Ultrasound Med. 2015;34(8):1–6. doi:10.7863/ultra.34.8.15.13.0005
20. Coutifaris C, Myers ER, Guzick DS, et al. Histological dating of timed endometrial biopsy tissue is not related to fertility status. Fertil Steril. 2004;82(5):1264–1272. doi:10.1016/j.fertnstert.2004.03.069
21. de Agostini A. An unexpected role for anticoagulant heparan sulfate proteoglycans in reproduction. Swiss Med Wkly. 2006;136(37–38):583–590.
22. McDonough PG. Grading a developmental continuum–elegy on the rise and fall of the endometrial biopsy. Fertil Steril. 2004;82(5):1286–1292. doi:10.1016/j.fertnstert.2004.07.932
23. Jiao Y, Xue N, Zou C, Shui X, Wang H, Hu C. Assessment of early damage of endometrium after artificial abortion by shear wave elastography. Insights Imaging. 2020;11(1):28. doi:10.1186/s13244-020-0841-4
24. Cao Y, Sun H, Zhu H, et al. Allogeneic cell therapy using umbilical cord MSCs on collagen scaffolds for patients with recurrent uterine adhesion: a Phase I clinical trial. Stem Cell Res Ther. 2018;9(1):192. doi:10.1186/s13287-018-0904-3
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.