Back to Journals » Cancer Management and Research » Volume 13
Development and Validation of Artificial Neural Networks for Survival Prediction Model for Patients with Spontaneous Hepatocellular Carcinoma Rupture After Transcatheter Arterial Embolization
Authors Qiu Y , Wang T, Yang X, Shen S , Yang Y, Wang W
Received 7 July 2021
Accepted for publication 11 September 2021
Published 27 September 2021 Volume 2021:13 Pages 7463—7477
DOI https://doi.org/10.2147/CMAR.S328307
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Seema Singh
Yiwen Qiu, Tao Wang, Xianwei Yang, Shu Shen, Yi Yang, Wentao Wang
Department of Liver Surgery and Liver Transplantation Center, West China Hospital of Sichuan University, Chengdu, 610041, People’s Republic of China
Correspondence: Wentao Wang
Department of Liver Surgery and Liver Transplantation Center, West China Hospital of Sichuan University, 37 Guoxue Road, Chengdu, 610041, People’s Republic of China
Tel +86 18980601895
Fax +86 28-85422871
Email [email protected]
Background: Spontaneous rupture bleeding is a fatal hepatocellular carcinoma (HCC) complication and a significant determinant of survival outcomes. This study aimed to develop and validate a novel artificial neural network (ANN)-based survival prediction model for patients with spontaneous HCC rupture after transcatheter arterial embolization (TAE).
Methods: Patients with spontaneous HCC rupture bleeding who underwent TAE at our hospital between January 2010 and December 2018 were included in our study. The least absolute shrinkage and selection operator (LASSO) Cox regression model was used to screen clinical variables related to prognosis. We incorporated the above clinical variables identified by LASSO Cox regression into the ANNs model. Multilayer perceptron ANNs were used to develop the 1-year overall survival (OS) prediction model for patients with spontaneous HCC ruptured bleeding in the training set. The area under the receiver operating characteristic curve and decision curve analysis were used to compare the predictive capability of the ANNs model with that of existing conventional prediction models.
Results: The median survival time for the whole set was 11.8 months, and the 1-year OS rate was 47.5%. LASSO Cox regression revealed that sex, extrahepatic metastasis, macroscopic vascular invasion, tumor number, hepatitis B surface antigen, hepatitis B e antigen, tumor size, alpha-fetoprotein, fibrinogen, direct bilirubin, red blood cell, and γ-glutamyltransferase were risk factors for OS. An ANNs model with 12 input nodes, seven hidden nodes, and two corresponding prognostic outcomes was constructed. In the training set and the validation set, AUCs for the ability of the ANNs model to predict the 1-year OS of patients with spontaneous HCC rupture bleeding were 0.923 (95% CI, 0.890– 0.956) and 0.930 (95% CI, 0.875– 0.985), respectively, which were higher than that of the existing conventional models (all P < 0.0001).
Conclusion: The ANNs model that we established has better survival prediction performance.
Keywords: hepatocellular carcinoma spontaneous rupture bleeding, HCC spontaneous rupture bleeding, least absolute shrinkage and selection operator regression, LASSO regression, artificial neural networks, ANNs, survival, prognosis
Introduction
Hepatocellular carcinoma (HCC) is the fourth most common cause of cancer-related death worldwide.1 The incidence of HCC is rising worldwide because of the increasing prevalence of viral hepatitis and nonalcoholic steatohepatitis.2–4 The Asia–Pacific region, particularly China, has a high incidence of HCC.5 Spontaneous tumor rupture bleeding is one of the most severe and life-threatening complications of HCC, with an occurrence rate of approximately 3–15% and high mortality rates.6–8 The initial symptoms of these patients are mainly abdominal pain, bloating, and shock. According to previous research reports, the incidence of spontaneous rupture of HCC shows significant geographical differences. The incidence of spontaneous HCC rupture in Asia–Pacific region is higher than in Western countries.9–11 Spontaneous HCC rupture might be related to the rapid growth of the tumor leading to intratumor necrosis and tumor vascular hyperplasia, with vascular dysfunction caused by the degeneration of the vessel structure composition (elastin, collagen IV).12,13
The current treatment strategy for patients with spontaneous HCC rupture remains controversial. At present, surgical treatments such as emergent liver resection, injection of absolute alcohol, hepatic artery ligation, and transcatheter arterial embolization (TAE) are available for HCC patients with spontaneous rupture bleeding. Considering the continuous improvement of surgical techniques and perioperative management, some doctors believe that resection of tumor lesions might be the best treatment, given that it can fully restore hemostasis and improve clinical prognosis.6,14,15 However, the general condition and liver function of HCC patients are relatively poor; the tumor is usually unresectable, large, or multifocal and might be accompanied by invasion of major intrahepatic vessels and extrahepatic metastasis; surgical treatment could not bring curative resection to the patient, and the chance of severe complications after surgery might be significantly increased.
Owing to its relative safety and effectiveness for hemostasis, TAE was introduced as a method that can be widely used for hemostasis and the treatment of spontaneous HCC rupture. Notably, increasing evidence supports the application of TAE in patients with advanced-stage HCC or patients with Child-Pugh grade C liver function.16–18 A recent study showed that TAE might bring a long-term survival benefit similar to open surgery to HCC patients with spontaneous rupture.19 To date, most previous studies have mainly focused on comparing the safety of all kinds of treatment methods in patients during the perioperative period, and there is no prognostic model for predicting the prognosis of HCC patients with spontaneous rupture bleeding after TAE.
As a type of machine learning, artificial neural networks (ANNs), which are essentially mathematical tools driven by the biological nervous system, have been widely used in the risk assessment of disease prognosis.20 In this study, we first evaluated the efficacy and safety of TAE treatment on spontaneous HCC rupture. Then we used the ANNs model to develop a simple, specific, and reliable prognostic model to predict the long-term survival outcomes based on large-sample preoperative data from a single center, which was further validated using internal validation sets. This study helps predict prognosis in patients with spontaneous HCC rupture after TAE and identifies optimal candidates for whom TAE treatment can help achieve tumor downgrade and obtain the opportunity for radical surgical resection.
Patients and Methods
A retrospective study was conducted on spontaneous HCC rupture patients who underwent TAE therapy between January 2010 and December 2018. The diagnosis of HCC followed the criteria recommended by the American Association for the Study of Liver Diseases (AASLD) of conclusive contrast-enhanced ultrasonography and magnetic resonance imaging without biopsy.21 The diagnosis of spontaneous HCC ruptured bleeding relies on enhanced computed tomography (CT) of the abdomen to show that the integrity of the tumor is disrupted and that there is hematoma around the liver. Abdominal paracentesis is also a reliable procedure used to confirm the diagnosis.9 The patient selection criteria for our study included the following (1) patients with unresectable spontaneous HCC rupture bleeding who were initially treated with TAE therapy; and (2) patients with detailed clinical characteristics. The exclusion criteria for this study were as follows: (1) the patients had another concurrent malignancy or severe nonmalignant illness; (2) patients with severe cardiopulmonary, renal, or cerebral dysfunction; and (3) patients with poor clinical data integrity. In this study, the whole set was randomly divided into two sets, 225 (70%) were included in the training set, and 97 (30%) were included in the validation set. The flowchart of the present study selection is shown in Figure 1, and the clinicopathologic characteristics of patients in the training and validation sets are listed in Table 1. Written informed consent was obtained from all patients to use their data for research purposes. This retrospective study was approved by the Ethics Committee of West China Hospital of Sichuan University and was performed in accordance with the 1975 Declaration of Helsinki.
 |
Table 1 Baseline Characteristics of Patients with Spontaneous Hepatocellular Carcinoma Rupture in the Different Sets |
 |
Figure 1 The flowchart of the present study selection. Abbreviations: HCC, hepatocellular carcinoma; TAE, transcatheter arterial embolization. |
Data Collection
The clinical data of patients with spontaneous HCC rupture were gathered from the electronic medical records, including demographics, liver cirrhosis, portal hypertension, Child-Pugh score, preoperative serum biochemistry data, preoperative coagulation parameters, preoperative serum tumor markers, imaging characteristics of tumors, complications after TAE, clinical data required for conventional staging systems and the corresponding clinical staging of each patient.22–29 Unresectable HCC was defined as liver malignancy not suitable for liver surgery due to the extent of malignant tumor invasion or the refusal to undergo surgical liver resection. Portal hypertension was defined by the presence of either esophageal varices or splenomegaly with a decreased platelet count (100 × 109/L or less). Liver failure was defined using the International Study Group of Liver Surgery (ISGLS) score.30 The liver reserve of all the patients was evaluated using the albumin-bilirubin (ALBI) classification (ALBI = log10 bilirubin × 0.66–0.085 × albumin). The ALBI score was stratified into 3 classifications: ALBI grade I (≤ −2.60), grade II (>−2.60 to ≤ −1.39), and grade III (> −1.39).29
Treatment and Follow-Up
The initial treatment was rapid infusion to maintain circulation stability and correct the shock state promptly. Given that patients with HCC usually have a background of liver cirrhosis and poor blood coagulation, it is necessary to transfuse plasma and provide fresh blood promptly to ensure that the patients have normal signs of life. Experienced interventional radiologists performed all TAE procedures. In the emergency embolization treatment, the patient was required to be in a supine position with the knee flexed, and the Seldinger intubation technique was used to insert the hepatic artery from the right femoral artery into the abdominal trunk or superior mesenteric artery and then perform the tumor‐feeding arteries for selective embolization. After embolization, angiography was performed to determine the extent of vascular occlusion and to assess blood flow in other arterial vessels. All patients received liver protection, anti-infection and anti-shock treatments after surgery. Transarterial chemoembolization (TACE) is recommended to be carried out every 2 months after surgery, depending on the patient’s physical status and liver function. All patients were followed up after discharge through outpatient clinic visits or phone calls. The primary endpoint of the study was overall survival (OS), which was defined as the period between discharge from the hospital and death.
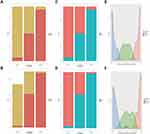
Statistical Analysis
Continuous data are expressed as medians and interquartile ranges (IQR25-75) and were compared by the Mann–Whitney U-test, and categorical variables are expressed as frequencies and percentages and were compared by the chi-squared test and two-tailed Fisher’s exact test. We identified the optimal structure of input layer parameters using a penalized Cox regression model with the least absolute shrinkage and selection operator (LASSO) penalty based on minimal criteria. ANNs model uses a multilayer perceptron (MLP) structure, including the input, hidden, and output layers. The input layer is the clinical variables identified by the LASSO Cox regression, and the output layer is the corresponding prognosis outcome. We used SPSS statistical software version 25.0 (IBM Corporation, Armonk, NY) to train the ANNs model. The discriminative ability of the ANNs model was assessed using the area under the receiver operating characteristic (ROC) curve (AUC), which was further compared with the results from conventional scoring systems, including the TNM (8th edition), Okuda,22 Barcelona Clinic Liver Cancer (BCLC),23 Cancer of the Liver Italian Program (CLIP),24 Chinese University Prognostic Index (CUPI),25 Japan Integrated Staging (JIS),26 China integrated score (CIS),27 ALBI grade,29 and Child-Pugh score systems. Decision curve analysis (DCA) was used to determine the clinical net benefits and performance of the ANNs models and the above-mentioned conventional staging systems at each risk threshold probability.31 All patients were stratified into 3 groups according to the tertiles of risk prediction values. OS was calculated with the Kaplan-Meier method. In addition, histogram and density plots were plotted in the training set and validation set. R version 4.0.0 (http://www.r-project.org/) was used for data analysis, LASSO Cox regression, C-index assessment, DCA, Kaplan-Meier curve analysis, and histogram and density plot construction. In all analyses, P < 0.05 was considered to indicate statistical significance.
Results
Patient Characteristics
After rigorous review, we enrolled a total of 322 patients who underwent TAE for patients in spontaneous HCC ruptured bleeding between January 2012 and December 2018 at West China Hospital. All patients were followed up until June 2020. All patients were randomly divided into a training set (n = 225, 75%) and a validation set (n = 97, 25%). A total of 114 (50.7%) patients died within 1 year in the training set, and 56 (57.7%) patients died within 1 year in the validation set. The demographic and clinical characteristics of the patients in the training and validation sets are listed in Table 1. The baseline demographic and clinical characteristics of the patients in the training and validation sets were similar (P > 0.05). Among the entire set, the median OS of the 322 patients with spontaneous HCC ruptured bleeding was 11.8 months. There was no statistically significant difference in the OS rate between the training set and validation set in the Kaplan-Meier analysis (all log-rank P=0.6), as shown in Supplementary Figure S1.
The Safety and Effectiveness of TAE Treatment
The common adverse reactions after TAE included fever, abdominal pain, nausea, and vomiting. Twenty-three patients had serious complications, including respiratory failure (n=4), liver and kidney failure (n=6), heart failure (n=2), pulmonary embolism (n=2), and gastrointestinal hemorrhage (n=5). In addition, four patients had recurrent tumor rupture. Two patients died due to severe complications and shock during the hospitalization period. All the remaining patients recovered and were discharged after symptomatic and supportive treatment.
Development of the ANNs Model for Predicting the 1-Year OS
In the training set, we used the LASSO Cox regression model to identify the clinical variables for predicting OS (Figure 2). The identified clinical variables included the following: sex, extrahepatic metastasis, MCI, tumor number, hepatitis B surface antigen (HBsAg), hepatitis B e antigen (HBeAg), tumor size, alpha-fetoprotein (AFP), fibrinogen (FIB), direct bilirubin (DBIL), red blood cell (RBC), γ-glutamyltransferase (γ-GGT). Then, these variables were included and used to construct the ANNs model. In the end, the ANNs model was constructed with a three-layer neural network including 12 input nodes, seven hidden nodes, and two corresponding prognosis outcomes (output nodes). The importance of the 12 relevant clinical variables was standardized (Figure 3). The corresponding clinical variables with the most and least importance were AFP with 100% importance and HBeAg with 14.7% importance, respectively.
Comparison of the Diagnostic Accuracy of the ANNs Model and Other Conventional Scoring Systems for 1-Year OS
In the training set, ROC analysis revealed that the predictive performance of the ANNs model for predicting 1-year OS was very high, with an AUC value of 0.880 (95% confidence interval [CI] 0.836–0.925), which was significantly higher than all the conventional scoring systems in predicting the 1-year OS of patients with spontaneous HCC rupture (ANNs: 0.923 vs CLIP: 0.717, JIP: 0.629, Liver Cancer Study Group of Japan (LCSGJ): 0.644, Okuda: 0.622, CUPI: 0.577, CIS: 0.626, TNM: 0.626; ALBI: 0.567, BCLC stage: 0.648, and Child-Pugh score: 0.506, P< 0.05 for all). In the validation set, the ANNs model was still superior to the conventional staging systems and had similar results as those obtained in the training set (Figure 4 and Table 2). In DCA, the ANNs model that we established demonstrated superior clinical usefulness in both the training set and validation set, compared with the existing conventional staging systems (Figure 5). This finding indicates that the ANNs model has superior clinical practicability compared with other models.
 |
Table 2 Predictive Accuracy of ANNs Model and Existing Staging System for 1-Year OS Status in the Training Set and Validation Set |
Application of the ANNs Model for Risk Stratification
According to the tertiles of the risk prediction values obtained from the ANNs model in the training set (low risk: 0.262, intermediate risk: 0.262–0.736, and high risk: 0.736). The clinicopathologic characteristics of patients with spontaneous HCC rupture according to risk stratification are shown in Table 3. The Kaplan–Meier OS curves revealed significant differences in the OS rate between different risk groups in both the training and validation sets (P <0.001 for all, as shown in Figure 6). In the training set, taking the low-risk group as the reference, the hazard ratios (HRs) of OS of the intermediate-risk group and the high-risk group were 2.565 (95% CI, 1.819–3.617) and 8.623 (95% CI, 5.898–12.607) (P < 0.0001), respectively. In the validation set, the HRs for OS of the intermediate-risk and high-risk groups were 3.655 (95% CI, 2.080–6.421) and 12.903 (95% CI, 6.591–25.259) (P<0.0001), respectively, compared with the low-risk group. In addition, the high-risk group had a noticeably increased possibility of the 1-year probability of death in the training set and validation set. Density plots of the 1-year probability of death predicted by the ANNs model illustrated significant differences among the high-, intermediate-, and low-risk groups in the training and validation sets (Figure 7).
 |
Table 3 Clinicopathologic Characteristics of Patients with Spontaneous Hepatocellular Carcinoma Rupture According to Risk Stratification |
Discussion
Spontaneous tumor rupture is an essential factor related to the poor prognosis of HCC patients, and its incidence ranges from 34% to 71%.32,33 According to the LCSG) staging (the 5th edition), the spontaneous HCC rupture is classified into stage IV regardless of the size and number of tumors.32 However, not all patients with liver cancer rupture and bleeding have a poor prognosis after effective therapy.34 There is no consistent conclusion about the optimal treatment approach for spontaneous HCC rupture.35 Studies have reported that liver resection is an essential treatment for spontaneous HCC rupture patients.36 However, spontaneous tumor rupture usually occurs in patients with advanced HCC. For unresectable patients, radical liver resection is not feasible due to severe liver cirrhosis and poor liver function, and palliative liver resection will bring considerable trauma. Moreover, whether palliative liver resection can bring a survival benefit to patients with unresectable liver cancer rupture remains controversial. It has been reported that TAE effectively achieves immediate hemostasis for spontaneously ruptured HCC.19,37 Previous research suggested that TAE conferred similar acceptable tolerability and favorable survival rate as liver resection.19 In our study, all patients tolerated TAE treatment well. The general adverse reactions following TAE were minor and self-limiting.
TAE can achieve hemostasis effectively and create the possibility of downstaging the treatment of tumors and even regaining the opportunity for surgical treatment. To date, many clinical predictive staging systems have been used to predict the survival outcomes of advanced-stage HCC patients. However, few specifically designed predictive models have been reported on the prognosis of patients with spontaneous HCC rupture following TAE treatment and related factors affecting the prognosis. Furthermore, the prognosis of patients with spontaneous unresectable HCC rupture is likely to be determined based on the nonlinear regression of numerous clinical variables rather than simply using the clinical features described in the current clinical stage. Therefore, our research established an ANNs predictive model using machine learning to predict the 1-year OS rate of spontaneous HCC rupture patients for the first time. We wanted to determine which patients with spontaneous HCC rupture would benefit the most from TAE. Using a LASSO Cox regression model to reduce high dimensionality, twelve variables were selected for the ANNs model, including sex, extrahepatic metastasis, MCI, tumor number, HBsAg, HBeAg, tumor size, AFP, FIB, DBIL, RBC, and γ-GGT. Our results showed that the predictive power of the ANNs model, which is a nonlinear model, was significantly superior to that of existing prediction staging systems in predicting the 1-year OS of spontaneous HCC rupture patients.
The TNM staging and BCLC staging systems, usually used to guide patients in choosing the best treatment strategy, have been widely used in clinical practice.38 The ALBI grade and Child-Pugh score also have a specific value in predicting the prognosis of HCC patients.39,40 However, the above staging systems are usually applied to patients undergoing surgical resection, and their predictive ability in patients with spontaneous HCC rupture is poor. Our study found that they are not suitable for predicting the prognosis of patients with spontaneous HCC rupture because they are usually used to assess liver reserve function. In addition, the above staging systems did not contain some critical factors that affect the prognosis, such as tumor size and number. The ALBI grade or Child-Pugh score alone can hardly accurately predict the prognosis of patients with spontaneous HCC rupture. The CLIP score incorporated the characteristics of the tumor, Child-Pugh score, AFP, and MCI variables into a quantifiable system. The CLIP score has good predictive ability in both the training and validation sets, with C-indexes of 0.717 and 0.737, respectively. CLIP score was second only to the ANNs model in predicting the 1-year OS of spontaneous HCC rupture patients. However, this staging system was not specifically designed for patients with spontaneous HCC rupture and did not contain essential serum indicators.
Large and multiple tumors are essential factors that reflect tumor burden, which is significantly associated with poor prognosis.41 MCI can cause portal hypertension and damage the liver function of patients. In addition, portal vein involvement and increased intratumoral pressure caused by portal vein invasion were the main reasons for HCC recurrence and metastasis.42 TAE treatment is generally prohibited for patients with PVTT in the main portal vein due to ischemic liver damage.43 However, we can use the super-selective TAE method to achieve hemostasis as soon as possible and reduce the risk of postoperative liver failure. Our study found that the preoperative serum AFP level is an independent risk factor for poor short-term survival in patients with spontaneous HCC rupture. Increased serum AFP usually reflects poor cellular differentiation, biological aggressiveness, and tumor spread. FIB is a 340-KDa acute phase glycoprotein associated with increased fibrinogen deposits in tumor tissue, and it could lead to promoting the angiogenesis, metastasis, and proliferation of cancer cells.44 Consistent with the findings of previous studies, in our study, preoperative GGT levels were found to be an essential risk factor,45 and high serum GGT levels might reflect the severity of the liver injury status.
Moreover, some studies have revealed that the elevated GGT expression could facilitate tumor progression, metastasis, cell apoptosis, and even DNA damage.46,47 HBsAg-positive patients usually have severe liver cirrhosis, accompanied by more severe coagulation dysfunction. In contrast, HBeAg-positivity in patients indicates active viral replication and is closely related to the occurrence and development of HCC. Continuous active replication of the hepatitis B virus (HBV) may lead to the necrosis of hepatocytes, thereby causing the malignant transformation, which is not conducive to the prognosis of patients. HBeAg positivity could decrease p53 activity by interacting with NUMB, consequently leading to the progression of HCC.47 We found that compared with patients who did not receive repeated TACE treatment, the prognosis of patients receiving repeated TACE treatment did not show a survival benefit, which might be related to the poor general condition of patients with spontaneous HCC rupture and their inability to tolerate regular repeated TACE treatment.
Several limitations should be taken into consideration when interpreting our findings. First, our research findings came from a single-center study. Due to the characteristics of retrospective studies, there inevitably might be potential inherent defects and selection bias, although a validation set was used to increase the reliability of our research. The relatively small sample size of this study will limit the full use of the predictive power of the ANNs model. Second, as most of the patients included in this study were hepatitis virus-infected, the established ANNs model warrants further investigation on its performance in patients with other etiologies.
Conclusion
In summary, we successfully developed and validated the ANNs model based on important clinical variables for predicting the 1-year OS of spontaneous HCC rupture patients who underwent TAE. Our established ANN model showed significantly better discriminative capability and a more accurate survival prediction ability than other prediction models; moreover, we could accurately identify low-risk, intermediate-risk, and high-risk patients.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Ethical Statement
The study was approved by the ethics committee of Sichuan University, and informed consent was taken from all the patients.
Acknowledgments
We would like to acknowledge with gratitude the contribution of the colleagues from the Department of Liver Surgery, West China Hospital of Sichuan University.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published, have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was supported by the Science and Technology Program of Sichuan Science and Technology Department (Nos. 2019YFS0029 and 2019YFS0529), the National Natural Science Foundation of China (Nos. 81770566 and 82000599), and the New Medical Technology Foundation of West China Hospital of Sichuan University (No. XJS2016004). The corresponding author Wentao Wang is the guarantor. The funding body financed the costs of the study and contributed to the study design, interpretation of data, and revision of the manuscript.
Disclosure
All the authors disclose no conflicts of interest for this work.
References
1. Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. 2019;16(10):589–604. doi:10.1038/s41575-019-0186-y
2. Bosch FX, Ribes J, Díaz M, Cléries R. Primary liver cancer: worldwide incidence and trends. Gastroenterology. 2004;127(Suppl 5):S5–S16. doi:10.1053/j.gastro.2004.09.011
3. Liu Z, Suo C, Mao X, et al. Global incidence trends in primary liver cancer by age at diagnosis, sex, region, and etiology, 1990–2017. Cancer. 2020;126(10):2267–2278. doi:10.1002/cncr.32789
4. Dasgupta P, Henshaw C, Youlden DR, Clark PJ, Aitken JF, Baade PD. Global trends in incidence rates of primary adult liver cancers: a systematic review and meta-analysis. Front Oncol. 2020;10:171. doi:10.3389/fonc.2020.00171
5. Zhu RX, Seto WK, Lai CL, Yuen MF. Epidemiology of hepatocellular carcinoma in the Asia-Pacific region. Gut Liver. 2016;10(3):332–339. doi:10.5009/gnl15257
6. Lin HM, Lei LM, Zhu J, Li GL, Min J. Risk factor analysis of perioperative mortality after ruptured bleeding in hepatocellular carcinoma. World J Gastroenterol. 2014;20(40):14921–14926. doi:10.3748/wjg.v20.i40.14921
7. Kirikoshi H, Saito S, Yoneda M, et al. Outcomes and factors influencing survival in cirrhotic cases with spontaneous rupture of hepatocellular carcinoma: a multicenter study. BMC Gastroenterol. 2009;9(1):29. doi:10.1186/1471-230x-9-29
8. Dewar GA, Griffin SM, Ku KW, Lau WY, Li AK. Management of bleeding liver tumours in Hong Kong. Br J Surg. 1991;78(4):463–466. doi:10.1002/bjs.1800780424
9. Lai EC, Lau WY. Spontaneous rupture of hepatocellular carcinoma: a systematic review. Arch Surg. 2006;141(2):191–198. doi:10.1001/archsurg.141.2.191
10. Min HJ, Lee OJ, Kang DY, et al. [The clinical study on spontaneously ruptured hepatocellular carcinoma]. Korean J Gastroenterol. 2004;44(3):160–167. Korean.
11. Roussel E, Bubenheim M, Le Treut Y-P, et al. Peritoneal carcinomatosis risk and long-term survival following hepatectomy for spontaneous hepatocellular carcinoma rupture: results of a multicenter French study (French-AFC). Ann Surg Oncol. 2020;27(9):3383–3392. doi:10.1245/s10434-020-08442-5
12. Kwon JH, Song GW, Hwang S. et al. Surgical outcomes of spontaneously ruptured hepatocellular carcinoma. World J Gastrointest Surg. 2020;25(4):941–953. doi:10.1007/s11605-020-04555-0
13. Yoshida H, Mamada Y, Taniai N, Uchida E. Spontaneous ruptured hepatocellular carcinoma. Hepatol Res. 2016;46(1):13–21. doi:10.1111/hepr.12498
14. Yeh CN, Lee WC, Jeng LB, Chen MF, Yu MC. Spontaneous tumour rupture and prognosis in patients with hepatocellular carcinoma. Br J Surg. 2002;89(9):1125–1129. doi:10.1046/j.1365-2168.2002.02188.x
15. Yang T, Sun YF, Zhang J, et al. Partial hepatectomy for ruptured hepatocellular carcinoma. Br J Surg. 2013;100(8):1071–1079. doi:10.1002/bjs.9167
16. Xiang X, Lau W-Y, Wu Z-Y, et al. Transarterial chemoembolization versus best supportive care for patients with hepatocellular carcinoma with portal vein tumor thrombus: a multicenter study. Eur J Surg Oncol. 2019;45(8):1460–1467. doi:10.1016/j.ejso.2019.03.042
17. Le Y, Shen J-X, Zhang Y-F, et al. Transarterial chemoembolization related to good survival for selected patients with advanced hepatocellular carcinoma. J Cancer. 2019;10(3):665–671. doi:10.7150/jca.28528
18. Fan WZ, Zhang YQ, Yao W, et al. Is emergency transcatheter hepatic arterial embolization suitable for spontaneously ruptured hepatocellular carcinoma in Child-Pugh C cirrhosis? J Vasc Interv Radiol. 2018;29(3):404–412.e3. doi:10.1016/j.jvir.2017.09.022
19. Zou J, Li C, Chen Y, et al. Retrospective analysis of transcatheter arterial chemoembolization treatment for spontaneously ruptured hepatocellular carcinoma. Oncol Lett. 2019;18(6):6423–6430. doi:10.3892/ol.2019.11037
20. Hu X, Cammann H, Meyer HA, Miller K, Jung K, Stephan C. Artificial neural networks and prostate cancer–tools for diagnosis and management. Nat Rev Urol. 2013;10(3):174–182. doi:10.1038/nrurol.2013.9
21. Marrero JA, Kulik LM, Sirlin CB, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the study of liver diseases. Hepatology. 2018;68(2):723–750. doi:10.1002/hep.29913
22. Okuda K, Obata H, Nakajima Y, Ohtsuki T, Okazaki N, Ohnishi K. Prognosis of primary hepatocellular carcinoma. Hepatology. 1984;4(1 Suppl):3s–6s. doi:10.1002/hep.1840040703
23. Llovet JM, Brú C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19(3):329–338. doi:10.1055/s-2007-1007122
24. Cancer of the Liver Italian Program (CLIP) Investigators. A new prognostic system for hepatocellular carcinoma: a retrospective study of 435 patients: the Cancer of the Liver Italian Program (CLIP) investigators. Hepatology. 1998;28(3):751–755. doi:10.1002/hep.510280322
25. Leung TW, Tang AMY, Zee B, et al. Construction of the Chinese university prognostic index for hepatocellular carcinoma and comparison with the TNM staging system, the Okuda staging system, and the cancer of the liver Italian program staging system: a study based on 926 patients. Cancer. 2002;94(6):1760–1769. doi:10.1002/cncr.10384
26. Kudo M, Chung H, Osaki Y. Prognostic staging system for hepatocellular carcinoma (CLIP score): its value and limitations, and a proposal for a new staging system, the Japan Integrated Staging score (JIS score). J Gastroenterol. 2003;38(3):207–215. doi:10.1007/s005350300038
27. Zhang BH, Wang XH, Yue HY, Ling CQ. A new staging system is more discriminant than conventional staging systems for unresectable hepatocellular carcinoma. J Cancer Res Clin Oncol. 2010;136(6):821–827. doi:10.1007/s00432-009-0722-1
28. Zhou J, Sun H-C, Wang Z, et al. Guidelines for diagnosis and treatment of primary liver cancer in China (2017 Edition). Liver Cancer. 2018;7(3):235–260. doi:10.1159/000488035
29. Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33(6):550–558. doi:10.1200/jco.2014.57.9151
30. Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149(5):713–724. doi:10.1016/j.surg.2010.10.001
31. Vickers AJ, Elkin EB. Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making. 2006;26(6):565–574. doi:10.1177/0272989x06295361
32. Aoki T, Kokudo N, Matsuyama Y, et al. Prognostic impact of spontaneous tumor rupture in patients with hepatocellular carcinoma: an analysis of 1160 cases from a nationwide survey. Ann Surg. 2014;259(3):532–542. doi:10.1097/SLA.0b013e31828846de
33. Forner A, Llovet JM, Bruix J. Hepatocellular carcinoma. Lancet. 2012;379(9822):1245–1255. doi:10.1016/s0140-6736(11)61347-0
34. Zhou C, Zu Q-Q, Liu X-L, et al. Treatment strategies and prognosis for initially unresectable ruptured hepatocellular carcinoma: a single-center experience in 94 patients. Diagn Interv Radiol. 2020;26(3):223–229. doi:10.5152/dir.2019.19049
35. Wang B, Lu Y, Zhang XF, Yú L, Pan CE, Wu Z. Management of spontaneous rupture of hepatocellular carcinoma. ANZ J Surg. 2008;78(6):501–503. doi:10.1111/j.1445-2197.2008.04543.x
36. Liu CL, Fan S-T, Lo C-M, et al. Management of spontaneous rupture of hepatocellular carcinoma: single-center experience. J Clin Oncol. 2001;19(17):3725–3732. doi:10.1200/jco.2001.19.17.3725
37. Raoul JL, Forner A, Bolondi L, Cheung TT, Kloeckner R, de Baere T. Updated use of TACE for hepatocellular carcinoma treatment: how and when to use it based on clinical evidence. Cancer Treat Rev. 2019;72:28–36. doi:10.1016/j.ctrv.2018.11.002
38. Huitzil-Melendez FD, Capanu M, O’Reilly EM, et al. Advanced hepatocellular carcinoma: which staging systems best predict prognosis? J Clin Oncol. 2010;28(17):2889–2895. doi:10.1200/jco.2009.25.9895
39. Liao R, Li DW, Du CY, Li M. Combined preoperative ALBI and FIB-4 is associated with recurrence of hepatocellular carcinoma after curative hepatectomy. World J Gastrointest Surg. 2018;22(10):1679–1687. doi:10.1007/s11605-018-3810-1
40. Ye L, Liang R, Zhang J, et al. Postoperative albumin-bilirubin grade and albumin-bilirubin change predict the outcomes of hepatocellular carcinoma after hepatectomy. Ann Transl Med. 2019;7(16):367. doi:10.21037/atm.2019.06.01
41. Battula N, Madanur M, Priest O, et al. Spontaneous rupture of hepatocellular carcinoma: a Western experience. Am J Surg. 2009;197(2):164–167. doi:10.1016/j.amjsurg.2007.10.016
42. Yamagata M, Maeda T, Ikeda Y, Shirabe K, Nishizaki T, Koyanagi N. Surgical results of spontaneously ruptured hepatocellular carcinoma. Hepato-gastroenterology. 1995;42(5):461–474.
43. Zhu K, Chen J, Lai L, et al. Hepatocellular carcinoma with portal vein tumor thrombus: treatment with transarterial chemoembolization combined with sorafenib–a retrospective controlled study. Radiology. 2014;272(1):284–293. doi:10.1148/radiol.14131946
44. Martino MM, Briquez PS, Ranga A, Lutolf MP, Hubbell JA. Heparin-binding domain of fibrin(ogen) binds growth factors and promotes tissue repair when incorporated within a synthetic matrix. Proc Natl Acad Sci USA. 2013;110(12):4563–4568. doi:10.1073/pnas.1221602110
45. Ruhl CE, Everhart JE. Elevated serum alanine aminotransferase and gamma-glutamyltransferase and mortality in the United States population. Gastroenterology. 2009;136(2):477–85.e11. doi:10.1053/j.gastro.2008.10.052
46. Kunutsor SK. Gamma-glutamyltransferase-friend or foe within? Liver Int. 2016;36(12):1723–1734. doi:10.1111/liv.13221
47. Corti A, Duarte TL, Giommarelli C, et al. Membrane gamma-glutamyl transferase activity promotes iron-dependent oxidative DNA damage in melanoma cells. Mutat Res. 2009;669(1–2):112–121. doi:10.1016/j.mrfmmm.2009.05.010
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.