Back to Journals » Patient Preference and Adherence » Volume 10
Development of internalized and personal stigma among patients with and without HIV infection and occupational stigma among health care providers in Southern China
Authors Li J, Assanangkornchai S , Lu L, Jia MH, McNeil EB , You J, Chongsuvivatwong V
Received 14 May 2016
Accepted for publication 23 August 2016
Published 8 November 2016 Volume 2016:10 Pages 2309—2320
DOI https://doi.org/10.2147/PPA.S112771
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Naifeng Liu
Jing Li,1,2,* Sawitri Assanangkornchai,1,* Lin Lu,3 Manhong Jia,3,* Edward B McNeil,1,* Jing You,4,* Virasakdi Chongsuvivatwong1,*
1Epidemiology Unit, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand; 2School of Public Health, Kunming Medical University, 3Yunnan Center for Disease Prevention and Control, 4Infectious Diseases Department, The First Affiliated Hospital of Kunming Medical University, Kunming, Yunnan Province, People’s Republic of China
*These authors contributed equally to this work
Background: HIV/AIDS-related stigma is a major barrier of access to care for those infected with HIV. The aim of this study was to examine, validate, and adapt measuring scales of internalized, personal, and occupational stigma developed in Africa into a Chinese context.
Methods: A cross-sectional study was conducted from January to September 2015 in Kunming, People’s Republic of China. Various scales were constructed on the basis of the previous studies with modifications by experts using exploratory and confirmatory factor analyses (EFA + CFA). Validation of the new scales was done using multiple linear regression models and hypothesis testing of the factorial structure invariance.
Results: The numbers of subjects recruited for the development/validation samples were 696/667 HIV-positive patients, 699/667 non-HIV patients, and 157/155 health care providers. EFA revealed a two-factor solution for internalized and personal stigma scales (guilt/blaming and being refused/refusing service), which were confirmed by CFA with reliability coefficients (r) of 0.869 and 0.853, respectively. The occupational stigma scale was found to have a three-factor structure (blaming, professionalism, and egalitarianism) with a reliability coefficient (r) of 0.839. Higher correlations of factors in the HIV patients (r=0.537) and non-HIV patients (r=0.703) were observed in contrast to low-level correlations (r=0.231, 0.286, and 0.266) among factors from health care providers.
Conclusion: The new stigma scales are valid and should be used to monitor HIV/AIDS stigma in different groups of Chinese people in health care settings.
Keywords: HIV/AIDS-related stigma, exploratory factor analysis, confirmatory factor analysis, guilt, blaming, being refused, refusing service
Introduction
With the pandemic of HIV/AIDS1 predominantly characterized by sexual transmissions2 and in the People’s Republic of China, the majority of people living with HIV/AIDS (PLWHA) are faced with HIV/AIDS-related stigma (HIV/AIDS stigma) – a major barrier for access to prevention, care, and treatment services. Studies have shown that HIV/AIDS stigma is a barrier for PLWHA-seeking health care due to lack of community HIV/AIDS knowledge, lack of understanding supportive clinic environments, absence of personal financial resources,3 and lack of employment opportunities.4 Although attention to stigma has steadily increased, it is especially important to comprehensively understand HIV/AIDS stigma under a measurable conceptual framework from different individuals’ perspectives in order to improve access to HIV health care.
The concept of HIV/AIDS stigma is often not explicitly defined – it usually refers to discrimination and violation of human rights as “a mark of disgrace.”5 Stigma linked to the reproduction of social differences in special settings will intimately contribute to existing inequalities. Existing theories have already delineated a framework to understand how stigma impacts individuals on their psychology, health, and behaviors.6,7 Some other existing theories have demonstrated concepts to understand how stigmatization as a social control mechanism impacts the HIV/AIDS epidemic and communities.8,9 However, existing conceptual frameworks have not clearly identified how HIV-positive patients experience HIV/AIDS stigma in health care settings.
Because of time- and context-specific characteristics of stigma, a stigma instrument needs to address the specific nature of people’s perceptions in each local context.10,11 For an individual not infected with HIV, personal stigma can be manifested in three predominant ways toward PLWHA,12 including negative emotions/feelings toward HIV-infected people (prejudice),13,14 prejudiced behavioral expressions to PLWHA (discrimination), and stereotyping as group-based beliefs about PLWHA (stereotype).15 For HIV-positive individuals, internalized stigma refers to the degree to which PLWHA endorse the negative beliefs and feelings associated with HIV/AIDS about themselves. Moreover, the health care sector is one of main environments where HIV-positive individuals experience stigma and discrimination.16,17 Stigma toward PLWHA can lead to lower access to care18 by PLWHA. Additionally, Chinese culture is more collectivist19 compared to western cultures. Individuals in the People’s Republic of China tend to maintain the same opinions with the mainstream rather than to go against it. Therefore, development of scales simultaneously to measure internalized stigma, personal stigma, and occupational stigma are necessary in the same health care setting.
In the People’s Republic of China, previous studies have shown that keeping social distance based on fears of stigmatization20 and negative feelings toward PLWHA21 may act as barriers for seeking health care services among PLWHA. Two equivalent stigma scales measuring internalized and personal stigma22 match the two core elements. However, the stigma scales were built on a series of shared beliefs that HIV is associated with immoral behavior, religious punishment, and lack of adherence to cultural norms.23,24 It is similar to the HIV/AIDS stigma in the People’s Republic of China, but different in the expression form of specific perceptions and behaviors. Therefore, exploration of the latent levels of these two scales is necessary. Additionally, other studies have revealed that Chinese service providers’ stigmatizing attitude and behavior are a key barrier for HIV testing and treatment such as differential treatment and denial of care, their perception of social norms, and concerns about their occupational safety.25,26 A Chinese scale27 measuring stigma among service providers has already been developed. However, it mainly focuses on occupational stigma in general hospitals at different levels rather than infectious disease hospitals that are responsible for HIV care in the Chinese health care system. Thus, there is a need to further improve it for the assessment of HIV/AIDS stigma in special hospitals among different groups of people in order to target key populations to improve quality of HIV/AIDS care.
This current study aims to develop and validate scales for measuring individual HIV-related stigma among HIV patients, non-HIV patients, and health care providers. The study was divided into two stages. The first stage aimed to modify the scales and examine the factor structure using exploratory factor analysis (EFA). In the second stage, the construct validity was evaluated using confirmatory factor analysis (CFA), and the discriminative validity was assessed in another group of subjects. In addition, difference in stigma perceived by HIV versus non-HIV patients was also examined and covariates with the stigma were identified.
Framework for HIV/AIDS stigma
Our understanding of HIV/AIDS stigma framework in hospital settings stems from previous studies.12,22,27 Earnshaw and Chaudoir12 in 2009 developed the conceptual framework for HIV stigma mechanisms from HIV-infected and non-HIV people. Visser et al22 in 2008 developed a parallel scale among HIV-infected and non-HIV people while Stein and Li27 in 2008 developed a multidimensional scale of HIV-related stigma among Chinese service providers. Figure 1 shows the conceptual framework of the study. Internalized stigma and personal stigma were developed using parallel scales for HIV-positive and non-HIV patients, while occupational stigma was developed for health care providers using a separate scale.
  | Figure 1 Conceptual framework of the study. |
Methods
Study settings
A cross-sectional study was conducted in the infectious disease departments of Kunming Infectious Disease Hospital and Kunming General Hospital, Yunnan Province, People’s Republic of China. These two hospitals serve both HIV/AIDS and non-HIV patients at out- and in-patient departments. HIV status was confirmed by Western blot test. The majority of the non-HIV patients were diagnosed with viral hepatitis or other infectious diseases. Although this group could not represent general non-HIV patients, they were served by the same hospital and were worthwhile to compare with the HIV group.
Study subjects
All HIV and non-HIV patients aged ≥15 years consecutively attending the study hospitals were consecutively screened for eligibility. Patients with tuberculosis were excluded in order to avoid confusion from tuberculosis stigma. Those who were too ill to be interviewed were also excluded. Doctors, nurses, and experimenters attending HIV and non-HIV clinics of the study hospitals were also recruited.
The first group of HIV patients, non-HIV patients, and health care providers was enrolled during January 1 to February 15, 2015, and was used to develop the scale. EFA was used to identify the underlying stigma constructs. The second group of HIV patients, non-HIV patients, and health care providers was enrolled between July 20 and September 10, 2015, and was used to validate the scale. The same questionnaires were applied for both the groups. Any subject who was involved in the development sample was excluded from the validation sample. CFA was conducted on the basis of the model developed from the first part.
Sample sizes
The required sample size needed for EFA is usually 5–10 times the number of questionnaire items.28 Initially, each of the three scales contained 17 items. A sample size of ~85–170 HIV and non-HIV patients per group was determined to be sufficient. For CFA, the recommended sample size required is 15–20 times the number of questionnaire items,28 and there were 10 and 11 items in internalized stigma scale and personal stigma scale, respectively. The required sample size was thus determined to be at least 150 HIV and non-HIV patients per group.
Study instruments
Internalized stigma and personal stigma scales developed by Visser et al22 were translated from English into Chinese by JL, and the Chinese version was checked for accuracy against the original English version by two other researchers. All the three scales were modified by the main researcher to suit the local hospital context. For example, one item about “Do not drink from the same tap with PLWH” changed to “Do not eat together with PLWH.” A team of health care experts including two chief physicians from the infectious departments of two hospitals and an expert of HIV/AIDS prevention in the Centre for Disease Control of Yunnan Province reviewed and finalized the Chinese version. Finally, five HIV and 10 non-HIV patients were individually requested to complete the questionnaires and comment on the understandability of the questions and on whether the intent of each question was accurately conveyed. The respondents were also asked to elaborate on the reasons why a particular response category was chosen for a question. According to their suggestions, the scales were further modified for clearer comprehensibility and cultural suitability.
The contents of the questionnaire items for HIV (internalized stigma) and non-HIV patients (personal stigma) were the same, but worded according to the perspective of the HIV status of the reader, for example, HIV group: “Do you think that you should be ashamed of yourself due to HIV/AIDS?”; non-HIV group: “Do most people think that PLWH should be ashamed of themselves?” A total of 17 parallel items were framed as two positive and 15 negative statements. Responses were rated on a scale of 1–4 where 1= strongly disagree, 2= disagree, 3= agree, and 4= strongly agree. Questions in two scales were worded from different perspectives.
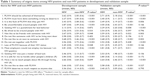
The occupational stigma scale27 completed by service providers also consisted of 17 items with the similar 1–4 rating scale reflecting the level of prejudicial attitudes. These items are listed in Tables 1 and 2.
Analysis of stigma scales
Mean scores for each item among the three scales were compared using Student’s t-tests, and two-way analysis of variance was used to compare items adjusting for the type of sample (development and validation). The total scores of the three stigma scales were obtained by adding the scores of the 17 items for each scale. All four responses were summed to obtain a total score for each scale, with a possible range of 17–68, where higher scores indicate higher stigma toward HIV/AIDS.
EFA was done on the three scales using principal components analysis with oblimin rotation to allow for possible correlation among factors and thus obtain more interpretable factors.29 Scree plots were used to identify the optimum number of factors. Items that had a factor loading of >0.4 were considered part of a factor. Items that did not have a factor loading of ≥0.4 were not included on any factor. Cronbach’s alpha coefficient was used to assess the internal consistency of scores.
CFA was used to validate the construct suggested by EFA in the development sample. Goodness-of-fit was assessed using a chi-square test of exact fit (non-significant P-value as a good fit), root mean square errors of approximation (RMSEA: <0.08 as a good fit), comparative fit index (CFI: >0.90), and Tucker Lewis index (TLI: >0.90).30
Among the internalized stigma scale, seven items were dropped in EFA and confirmed in CFA; six items were dropped in EFA and another item was dropped in CFA among personal stigma scale; and in terms of occupational stigma scale, there were six items dropped in EFA and confirmed in CFA.
Finally, univariate analyses were performed separately for each factor of HIV/AIDS stigma after EFA and CFA in order to assess their independent association with demographic and socioeconomic variables. Variables having a P-value of <0.05 were considered significant. All analyses were performed using R language and environment.31
Ethical considerations
The ethical aspects of this study were approved by Prince Songkla University Faculty of Medicine Institutional Review Board (57-246-18-5) and Kunming Medical University. Anonymity of the data was assured, and written informed consent was obtained from the participants to participate in the survey, after providing them with detailed information on the survey procedures.
Results
Out of 800 consecutive eligible HIV patients approached in both the groups, 696/800 (87%) in the first group and 667/800 (83%) in the second group consented to join the study, whereas 699/1,059 (66%) in the first group and 667/1,059 (63%) in the second group among the invited non-HIV patients agreed to join the study. The development/validation samples included 696/667 HIV patients, 699/667 non-HIV patients and 157/155 health care providers, respectively.
Sample characteristics
Table 3 presents the sociodemographic characteristics of the patients in each sample. The majority was male, of Han ethnicity, married or cohabiting, and employed. Most reported having no religious affiliation. About half achieved a junior high school level of education, had a monthly household income of ≤5,000 RMB, and were living in a family with 2–4 members. HIV-positive patients were more likely to belong to a minority ethnicity, have a religious affiliation, live in rural areas, have a higher education level, be separated, divorced, or widowed, have a lower household income, live with fewer family members, and be self-employed.
  | Table 3 Distribution of characteristics among HIV and non-HIV patients |
Table 4 shows the demographic characteristics of the health care providers in the exploratory and validation samples. The majority was female, of Han ethnicity, married or cohabiting, employed at the elementary level, working as nurses, achieved a university or equivalent level of education, and had a household income ranging from 5,000 to 8,000 RMB.
  | Table 4 Distribution of characteristics among health care providers |
Tables 1 and 2 show the distribution of items of the three scales in the exploratory and validation phases. In the patient scales, the item “PLWH deserves as much respect as anyone else” had the highest score reflecting positive attitude toward PLWH by HIV and non-HIV patients. In 12 items, the HIV group had significantly higher mean scores compared to the non-HIV group (10 items in both development and validation samples, one item in the development sample alone, and one item in the validation sample alone). The mean (standard deviation) scores of stigma scales among HIV patients, non-HIV patients, and health care providers were 45.0 (7.9), 40.7 (6.1), and 35.3 (9.6), respectively. Thus, internalized stigma was generally stronger than personal stigma. Stigma scores in the validation sample were generally higher than those in the development sample for all items. The same applied for items among health care providers.
EFA
Patient scales
The scree plots from both the analyses shown in Figure 2 suggested two factors. Among the HIV group, the first factor loaded highly on seven items and reflected a feeling of “being refused.” The second factor loaded highly on three items and reflected a feeling of “guilt.” Among the non-HIV group, the first factor loaded highly on seven items reflecting a feeling of “refusal” and the second factor loaded highly on three items and reflected a feeling of “blaming” (Table 5).
  | Table 5 Factor loadings among HIV and non-HIV patients and health care providers in development and validation samples |
Health care providers’ scale
EFA identified three factors (Figure 2) reflecting feelings of “blame,” “professionalism,” and “egalitarianism” among the health care providers (Table 5).
Internal consistency
Cronbach’s alpha coefficients for all factors were >0.85, except for egalitarianism, which had a value of 0.78, thus reflecting a high level of inter-item consistency (Table 5).
Correlation among factors
Table 6 summarizes correlation coefficients among factors within each group of subjects. The absolute values ranged from 0.23 to 0.70, indicating that the factors had a low to moderate correlation.
  | Table 6 Correlation of latent factors in three scales |
Confirmatory and validation analyses
After testing the validity of the factors on the corresponding validation sample, the factor loadings from the validation sample are shown in the last column of Table 5. In general, the coefficients were moderate for HIV and non-HIV patients (between 0.41 and 0.67), whereas those for health care provider’s validation sample were high (between 0.50 and 1.04). For test statistics, all RMSEA were <0.08, all CFI were >0.90, and all TLI were >0.90. Thus, CFA confirmed that the factors identified from the development samples fit the validation sample. However, all P-values from the chi-squared goodness-of-fit tests were <0.001.
Covariates for each domain of stigma
Table 7 presents the results of the univariate analysis to predict each domain of stigma. Age was associated with feelings of being refused among HIV patients; those being >40 years of age were more likely to feel refused by others. Age was also associated with a tendency to refuse and blame HIV patients among non-HIV patients; those >40 years of age were more likely to refuse and blame HIV patients. Health care providers who were aged >40 years were more likely to adhere to professionalism when they treated HIV patients. HIV patients who were married often felt that they were refused and felt guilty, whereas non-HIV patients who were married also had a tendency to refuse and blame HIV patients. Health care providers who were married were less likely to be professional. Health care providers who had higher education levels were less inclined to blame HIV patients and were more professional and egalitarian. Gender was also significantly associated with being refused, while ethnicity and household income were associated with guilt among HIV patients. Among non-HIV patients, religion was associated with refusing. Among health care providers, marital status was associated with professionalism while gender and household income were significantly associated with egalitarianism.
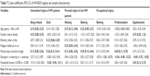  | Table 7 Crude coefficients (95% CI) of HIV/AIDS stigmas and sample characteristics |
Discussion
This study revealed that stigma scales developed in Africa can be modified for use in a Chinese setting. EFA suggested two latent factors for HIV-positive and non-HIV patients, which were confirmed by CFA. With small differences, items in each factor of the two scales among HIV patients corresponded well with those among non-HIV patients. Two factors were identified in each group: being refused and guilt among HIV patients and refusing and blaming among non-HIV patients. Among health care providers, three factors that reflected feelings of contradiction between social norms (blaming) and professional values (professionalism and egalitarianism) were identified. There were significant relationships between various demographic characteristics and these latent factors. However, there was no consistent pattern among the three groups.
Being refused versus refusing and guilt versus blaming were two latent factors among internalized and personal stigma scales suggested by EFA and CFA. Perceptions of guilt and shame are two self-conscious emotions. Some researchers have repeatedly confirmed their distinctiveness.32,33 Guilt is associated with self-blame related to one’s own behavior, whereas shame is associated with self-blame at a deeper level where the individual sees their global self as being at fault.34 One of the common characteristics associated with shame and guilt is the desire to hide or withdraw from social situations, in part to avoid situations that may elicit further guilt.35 Thus, guilt-prone individuals may utilize more avoidant strategies such as abandoning utilization of health care in order to avoid social interactions. It may also help to explain the characteristics of individual internalizing symptoms among HIV-positive patients who may have faced a significantly higher level of internalized stigma and participation restriction.
Being refused for HIV patients and refusing for non-HIV patients were powerfully associated with internalized and personal stigma among HIV and non-HIV patients, respectively. Due to guilt- and shame-proneness of HIV patients, they frequently tended to withdraw from social situations36 so as to avoid further refusal. Being refused is also manifested in the forms of social isolation37 from family, friends, and community. Correspondingly, non-HIV patients also mainly tend to refuse infectious subjects for the same reason.
Two items namely “people would not date me due to HIV/AIDS” and “neighbors would not like to live next door to me” were included in our results among patients who were not included in the African study.22 This implies that Chinese tend to refuse HIV-positive patients more compared to the African context which is known to be the epicenter of HIV/AIDS. Feelings of refusing and blaming not only come from non-HIV patients but are also stemmed from community members who reside near PLWHA.
Our study found consistent blaming factors among non-HIV patients and health care providers. Struening et al38 showed that strained, distant relationships with family members or friends or both were a source of shame. Based on the labeling theory of Scheff,39 the application of deviant stereotypes makes those who are faced with changed self-perceptions and social opportunities devalue and be labeled. The majority of the general population does not want to employ PLWHA or be their neighbor, friend, or intimate partner and tends to regard them as being less trustworthy, intelligent, and competent. Once a person is labeled, powerful social forces come into play to encourage a stable pattern of stigma.
Guilt and feelings of being refused had a relatively higher correlation among HIV patients (0.54) than among health care providers (0.23–0.39). The correlation between blaming and refusing was even higher (0.70) among the non-HIV group. These correlations resulted from our use of oblimin rotation of the factors. While changing the viewing angle of space by oblimin, two interpreted factors indicated the delicate difference among guilt and being blamed in internalized stigma as well as among blaming and refusing in personal stigma. Just as mentioned earlier, those who had perceptions of guilt- and shame-proneness inclined to be refused or refuse infectious patients. Factors of guilt/blaming primarily emphasized the perceptions of patients, while being refused/refusing mainly focus on behaviors.
Low levels of correlation among stigma factors found in health care workers in our study reflect independence. A previous study27 identified internalized shame among health care providers, a contrast to our study. The attitude of health care providers toward HIV patients is mainly built on a mainstream culture of associations between HIV/AIDS and immoral behaviors. A coexistence of blaming on one hand and professionalism40,41 and equalitarianism42 on the other hand indicated a contradiction between knowledge/competence in care and attitudes toward HIV/AIDS patients.25,43,44 It also reflected a contradiction between stigmatized attitudes acquired from the community and professional knowledge and competence on HIV/AIDS care.
Among the three study groups, each of the subscales associated with measures of sample characteristics further validated the independence of each factor reflecting that they are representative of an independent sub-stigma mechanism.6–8
Marital status was the strongest covariate across all latent factors of internalized and personal stigma among both the patient groups. Marital status strongly influences disclosure of HIV status45 and is also known to have a significant association with quality of life.46 The association may stem from relationships between marital status and psychology reflecting unmet inner needs and emotional frustrations. Based on social cognitive theory,47 symbolic communication influences human thought and action as the link of their marriage. Thus, a perception of betrayal of marriage was associated with being refused, refusing, guilt, and blaming.
Education was significantly associated with blaming, professionalism, and egalitarianism among occupational stigma of health care providers. Those having a higher education were less likely to blame patients and more likely to treat patients professionally and equally. One study48 suggested that poor knowledge of HIV resulted in more blaming toward PLWHA. A spirit of professionalism and excellence of patient care provided a strong foundation for the planning and delivery of health services.49 Furthermore, egalitarianism of health care providers should compensate for those who were HIV-positive including the sufficient magnitude of health care providers for HIV patients in order to close inequalities.
The World Health Organization and other international organizations such as The Joint United Nations Programme on HIV/AIDS (UNAIDS) and The South African National Aids Council (SANAC) have advocated “zero discrimination” since 2011. Overall, our study has highlighted that HIV/AIDS stigma is still common in 2014. In the People’s Republic of China, the strategy to control HIV indeed achieves universal health coverage and promotes a people-centered approach grounded in principles of human rights and health equity. However, for over 10 years, >50% of PLWHA were still fearful of disclosing their infectious status, whereas ~80% were afraid of being blamed or being refused in 2013.50 More efforts are still needed to achieve these goals, especially in health settings.
Limitations
Some limitations should be noted in our study. First, patients were recruited from only two hospitals, thus generalizability is limited. Second, the sample size of health care providers was rather small, thus it is possible that the situation in other institutes may be different. Third, a poorer response rate among the non-HIV group may have affected the internal validity of the study. Fourth, the non-HIV patient group in our study cannot represent all PLWHA, so generalizability of personal stigma is limited.
Conclusion
In terms of construct and discriminative validity, it could be said that the current stigma scales developed so far are valid and should be used to monitor HIV/AIDS stigma in different groups of Chinese people in health care settings.
Acknowledgments
The authors are grateful to staff of the School of Public Health of Kunming Medical University: Dr Le Cai for supporting the fieldwork, and the Third People’s Hospital of Kunming: Dr YingRong Du for supporting the fieldwork. This study is a part of the first author’s thesis in partial fulfillment of the requirements for a PhD in Epidemiology at Prince of Songkla University, Thailand, and the China Medical Board under the project of “Join Research Capacity Strengthening of the Western Rural Health Network, China” provided the financial support.
Disclosure
The fieldwork was supported by Yunnan Center for Disease Prevention and Control. The authors report no other conflicts of interest in this work.
References
Ministry of Health PsRoC. Joint United Nations Programme on HIV/AIDS: estimates for the HIV/AIDS epidemic in China. (Chinese). World Health Organization. 2011;53(Suppl 1):S74. | ||
Zhang K-L, Detels R, Liao S, Cohen M, Yu D-B. China’s HIV/AIDS epidemic: continuing challenges. Lancet. 2008;372(9652):1791–1793. | ||
Johnson M, Samarina A, Xi H, et al. Barriers to access to care reported by women living with HIV across 27 countries. AIDS Care. 2015;27(10):1220–1230. | ||
Lazarus L, Deering KN, Nabess R, Gibson K, Tyndall MW, Shannon K. Occupational stigma as a primary barrier to health care for street-based sex workers in Canada. Cult Health Sex. 2012;14(2):139–150. | ||
Link BG, Phelan JC. Conceptualizing stigma. Ann Rev Sociol. 2001;27:363–385. | ||
Alonzo AA, Reynolds NR. Stigma, HIV and AIDS: an exploration and elaboration of a stigma trajectory. Soc Sci Med. 1995;41(3):303–315. | ||
Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–1795. | ||
Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57(1):13–24. | ||
Mill JE, Edwards N, Jackson RC, MacLean L, Chaw-Kant J. Stigmatization as a social control mechanism for persons living with HIV and AIDS. Qual Health Res. 2010;20(11):1469–1483. | ||
Malcolm A, Aggleton P, Bronfman M, Galvao J, Mane P, Verrall J. HIV-related stigmatization and discrimination: Its forms and contexts. Crit Public Health. 1998;8(4):347–370. | ||
Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991–1999. Am J Public Health. 2002;92(3):371–377. | ||
Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–1177. | ||
Allport GW. The Nature of Prejudice. Basic Books; a member of the Perseus Books Group, New York; 1979. | ||
Brewer MB. The social psychology of intergroup relations: social categorization, ingroup bias, and outgroup prejudice. In: DeLamater J, Ward A, editors. Social psychology: Handbook of basic principles. 2nd ed. New York: Guilford Press; 2007. | ||
Kanahara S. A review of the definitions of stereotype and a proposal for a progressional model. Ind Diff Res. 2006;4(5):306. | ||
Nyblade L, Stangl A, Weiss E, Ashburn K. Combating HIV stigma in health care settings: what works? J Int AIDS Soc. 2009;12(1):15. | ||
Andrewin A, Chien L-Y. Stigmatization of patients with HIV/AIDS among doctors and nurses in Belize. AIDS Patient Care STDs. 2008;22(11):897–906. | ||
Kinsler JJ, Wong MD, Sayles JN, Davis C, Cunningham WE. The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care STDs. 2007;21(8):584–592. | ||
Ho DY-F, Chiu C-Y. Component ideas of individualism, collectivism, and social organization: an application in the study of Chinese culture. Individualism and collectivism: Theory, method, and applications., (pp. 137–156). Thousand Oaks, CA, US: Sage Publications. 1994. | ||
Lieber E, Li L, Wu Z, Rotheram-Borus MJ, Guan J; Group NIoMHCHPT. HIV/STD stigmatization fears as health-seeking barriers in China. AIDS Behav. 2006;10(5):463–471. | ||
Chen J, Choe MK, Chen S, Zhang S. Community environment and HIV/AIDS – related stigma in China. AIDS Educ Prev. 2005;17(1):1–11. | ||
Visser MJ, Kershaw T, Makin JD, Forsyth BW. Development of parallel scales to measure HIV-related stigma. AIDS Behav. 2008;12(5):759–771. | ||
Bond V, Chase E, Aggleton P. Stigma, HIV/AIDS and prevention of mother-to-child transmission in Zambia. Eval Program Plann. 2002;25(4):347–356. | ||
Niehaus I. Leprosy of a deadlier kind: conceptions of AIDS, sex and death in the South African lowveld. Paper presented at: Institute for Social and Economic Research, Rhodes University; 2006. | ||
Li L, Wu Z, Wu S, Zhaoc Y, Jia M, Yan Z. HIV-related stigma in health care settings: a survey of service providers in China. AIDS Patient Care STDs. 2007;21(10):753–762. | ||
Zhang L, Chow EPF, Zhang J, Jing J, Wilson DP. Suppl 1: Describing the Chinese HIV surveillance system and the influences of political structures and social stigma. Open AIDS J. 2012;6:163. | ||
Stein JA, Li L. Measuring HIV-related stigma among Chinese service providers: confirmatory factor analysis of a multidimensional scale. AIDS Behav. 2008;12(5):789–795. | ||
Everitt B. Multivariate analysis: the need for data, and other problems. Br J Psychiatry. 1975;126(3):237–240. | ||
Yaremko RM, Harari H, Harrison RC, Lynn E. Handbook of Research and Quantitative Methods in Psychology: For Students and Professionals. Psychology Press, London: Lawrence Erlbaum Associates; 2013. | ||
Schumacker RE, Lomax RG. A Beginner’s Guide to Structural Equation Modeling. Psychology Press, London: Lawrence Erlbaum Associates; 2004. | ||
Chongsuvivatwong V. Analysis of epidemiological data using R and Epicalc. Book Unit, Faculty of Medicine, Prince of Songkla University Thailand; 2008. | ||
Tangney JP, Miller RS, Flicker L, Barlow DH. Are shame, guilt, and embarrassment distinct emotions? J Pers Soc Psychol. 1996;70(6):1256. | ||
Leith KP, Baumeister RF. Empathy, shame, guilt, and narratives of interpersonal conflicts: guilt – prone people are better at perspective taking. J Pers. 1998;66(1):1–37. | ||
Barr P. Guilt- and shame-proneness and the grief of perinatal bereavement. Psychol Psychother. 2004;77(4):493–510. | ||
Tangney JP, Dearing RL. Shame and Guilt (Emotions and Social Behavior). New York: Guilford Press; 2002. | ||
Tangney JP, Dearing RL, editors. Emotions and social behavior. In: Shame and Guilt. New York: Guilford Press; 2002;10(9781412950664):n388. | ||
Stadler J. Rumor, gossip and blame: implications for HIV/AIDS prevention in the South African lowveld. AIDS Educ Prev. 2003;15(4):357–368. | ||
Struening EL, Perlick DA, Link BG, Hellman F, Herman D, Sirey JA. Stigma as a barrier to recovery: the extent to which caregivers believe most people devalue consumers and their families. Psychiatr Serv. 2001;52(12):1633–1638. | ||
Scheff TJ. Being Mentally Ill: A Sociological Theory. New Baunswick: Transaction Publishers; 1970. | ||
Wynia MK, Latham SR, Kao AC, Berg JW, Emanuel LL. Medical professionalism in society. N Engl J Med. 1999;341(21):1612–1616. | ||
Langendyk V, Mason G, Wang S. How do medical educators design a curriculum that facilitates student learning about professionalism? Int J Med Educ. 2016;7:32–43. | ||
Shiloh A. Equalitarian and hierarchal patients: an investigation among hadassah hospital patients. Med Care. 1965;3(2):87–95. | ||
Webber G. Chinese health care providers’ attitudes about HIV: a review. AIDS Care. 2007;19(5):685–691. | ||
Operario D, Wang D, Zaller ND, et al. Effect of a knowledge-based and skills-based programme for physicians on risk of sexually transmitted reinfections among high-risk patients in China: a cluster randomised trial. Lancet. 2016;4(1):e29–e36. | ||
Okareh OT, Akpa OM, Okunlola JO, Okoror TA. Management of conflicts arising from disclosure of HIV status among married women in southwest Nigeria. Health Care Women Int. 2015;36(2):149–160. | ||
Subramanian T, Gupte MD, Dorairaj VS, Periannan V, Mathai AK. Psycho-social impact and quality of life of people living with HIV/AIDS in South India. AIDS Care. 2009;21(4):473–481. | ||
Bandura A. Social cognitive theory of mass communication. Media Psychol. 2001;3(3):265–299. | ||
Memish ZA, Filemban SM, Bamgboyel A, Al Hakeem RF, Elrashied SM, Al-Tawfiq JA. Knowledge and attitudes of doctors toward people living with HIV/AIDS in Saudi Arabia. J Acquir Immune Defic Syndr. 2015;69(1):61–67. | ||
Goosby EP, von Zinkernagel D. The medical and nursing education partnership initiatives. Acad Med. 2014;89(8 Suppl):S5–S7. | ||
UNAIDS. Report of stigma and discrimination among people living with HIV/AIDS in China (Chinese). 2013. Available from: http://wenku.baidu.com/view/e12aad4ae45c3b3567ec8b40.html. Accessed October 3, 2016. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.