Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 10
Developing Class III malocclusions: challenges and solutions
Authors Zere E , Chaudhari PK , Sharan J, Dhingra K, Tiwari N
Received 7 January 2018
Accepted for publication 1 April 2018
Published 22 June 2018 Volume 2018:10 Pages 99—116
DOI https://doi.org/10.2147/CCIDE.S134303
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Christopher E. Okunseri
Edlira Zere,1,* Prabhat Kumar Chaudhari,2,* Jitendra Sharan,3 Kunaal Dhingra,4 Nitesh Tiwari5
1Department of Orthodontic and Craniofacial Anomalies, School of Graduate Dentistry, Rambam Health Care Campus, Technion Faculty of Medicine, Haifa, Israel; 2Division of Orthodontics and Dentofacial Deformities, Centre for Dental Education and Research, All India Institute of Medical Sciences, New Delhi, India; 3Department of Dentistry, All India Institute of Medical Sciences, Bhubaneswar, India; 4Division of Periodontics, Centre for Dental Education and Research, All India Institute of Medical Sciences, New Delhi, India; 5Division of Pedodontics and Preventive Dentistry, Centre for Dental Education and Research, All India Institute of Medical Sciences, New Delhi, India
*These authors contributed equally to this work
Abstract: Class III malocclusion represents a growth-related dentofacial deformity with mandibular prognathism in relation to the maxilla and/or cranial base. Its prevalence varies greatly among and within different races, ethnic groups, and geographic regions studied. Class III malocclusion has a multifactorial etiology, which is the expression of a moderate distortion of normal development as a result of interaction between innate factors or genetic hereditary with environmental factors. Various skeletal topographies of underlying Class III malocclusion are due to discrepancy in the maxillary and mandibular growth along with vertical and/or transverse problems apart from sagittal malformations. The spectrum of complications for Class III malocclusion ranges in gravity from dentoalveolar problems with functional anterior shift of the mandible to true skeletal problems with serious maxillomandibular discrepancies, which makes its diagnosis highly challenging in growing children. Concern regarding early treatment and the need for interceptive care in the case of Class III malocclusion has always been a dilemma, knowing that not all problems will be solved in these cases until maxillomandibular growth is further completed, and the long-term outcome of various treatment approaches may depend on the growth tendency of an individual. Interceptive treatment of Class III malocclusions should be undertaken if it prevents damage to the oral tissues and/or significantly reduces the amount or severity of future orthodontic and surgical interventions. This paper presents an overview of developing Class III malocclusion, with the emphasis on challenges and their solutions based on the best current available evidence.
Keywords: Class III malocclusion, facemask therapy, maxillary expansion, chin cup appliance, bone-anchored maxillary protraction, growth treatment response vector
Introduction
The father of modern orthodontics, Edward Hartley Angle, in 1899 classified malocclusions in Class I, Class II, and Class III based on permanent first maxillary and mandibular molars relationship and alignment (or lack of it) of teeth with reference to the line of occlusion.1 Gradually, Angle’s classification was modified and additional information such as jaw relationship and the pattern of growth were also included. Thus, a Class III jaw relationship suggests that the mandible has acquired a more mesial position in relation to the maxilla and/or cranial base.2,3 Occasionally, due to dental compensation, sometimes there is Class I dental relationship on the Class III skeletal base.
Further, Charles Henry Tweed classified Class III malocclusions as a pseudo Class III malocclusion with normal mandible and underdevelopment of maxilla (category A) and skeletal Class III malocclusion with prognathic mandible or an underdevelopment of maxilla (category B).4
Class III problems may arise due to deficient growth of maxilla in the downward and forward direction and more forward growth or reduced downward growth of mandible. Hence, a hypodivergent growth pattern accentuates the Class III problem due to more growth rotation of the mandible in the upward and forward direction, while a vertical growth pattern alleviates it due to downward and backward rotation, provided that excessive facial height does not become the problem instead.5
Nonsurgical treatment of Class III problems remains a challenge in our profession. However, prompt diagnosis and early intervention of Class III malocclusion may be helpful to reduce the extent of burden for severe Class III malocclusion in late adolescence.6 This paper presents an overview of developing Class III malocclusion, with the emphasis on challenges and their solutions based on the best current available evidence.
Prevalence
Existing literature regarding the global prevalence of Class III malocclusions has shown that its prevalence varies greatly among and within different races, ethnic groups, and geographic studied regions (Tables 1 and 2). There is a wide range of reported prevalence, even with conflicting results, and the discrepancies in the prevalence rate might be attributed to the variation among samples, the timing of investigation, and type of analysis performed.7
  | Table 1 Reported prevalence of Class III malocclusion globally and in different continents |
  | Table 2 Reported prevalence of Class III malocclusion among different nationality groups |
A recent systematic review7 reported a global prevalence of Angle Class III malocclusion within the interval of 0%–26.7% for different populations. Prevalence rates of 15.80%, 15.69%, and 16.59% were revealed for Southeast Asian countries, Chinese, and Malaysian groups, respectively. Among Japanese it was around 14%, for Koreans 9%–19%, and about 1.65% for Taiwanese. For Indian children aged from 5 to 15 years, the prevalence varied within 0%–4.76%.7 Further, from a global viewpoint, Indians had the lowest prevalence of 1.19% among all other racial groups. A prevalence of 10.18% was reported for Middle Eastern populations, and among them, for Israeli Arabs it was 1.3%, Iranians about 15.2%, Turkish about 10.30%–11.5%, and Egyptians showed a rate from 4% to 11.38%. Regarding African countries,7 the prevalence rate was found to be 4.59% and varying for Kenya, Tanzania, and Nigeria (between 1% and 16.8%). Class III malocclusions have been found to be more prevalent in Hispanic than in African or Caucasian groups. Prevalence of about 9.1% and 8.3% were reported for Americans and Mexican Americans, respectively.8 Factors such as the method of malocclusion study and the age group studied may influence the varying prevalence in Caucasians between 3% and 5%.9–15 Prevalences of ~5% and from 2% to 6% have been found in Latin and European populations, respectively.8 Furthermore, the White population in United Kingdom and Scandinavia had a Class III incidence of about 3%–5%,16 and about 6% for Sweden.17
For Americans, the prevalence was found to be about 5%.15,18 Studies on US African-American population groups found the prevalence in the range of 3%–6%.19–21 Similar studies conducted on other nationalities revealed a Class III malocclusion prevalence of about 3% for Brazilian,22 14% for Syrian,23 and 9.4% for Saudi Arabian individuals.24
Etiology of Class III malocclusion
Similar to most of the malocclusions and dentofacial deformities, the etiology of Class III malocclusion is multifactorial. It results from a distortion of normal development, rather than from any pathological process. Expressions of Class III malocclusion are results of interaction between innate factors or genetic hereditary with environmental factors.25–27
Studies of human inheritance have provided sufficient evidence to establish the fact that mandibular growth is mainly affected by heredity.27–31 Familiar genetic inheritance has a strong influence on skeletal craniofacial dimensions contributing to Class III malocclusion and a significantly higher incidence of this malocclusion has been found to have a familial occurrence between members of many generations.32,33 The best known example of familial inheritance is Habsburg Jaw, in which mandibular prognathism recurred over multiple generations in the European royalty.34,35 The pattern of transmission of Class III malocclusion still remains an issue of controversy. According to some authors, the transmission is autosomal recessive, and according to others, it is autosomal dominant with complete or incomplete penetrance; yet, some others support the polygenic transmission mode.36,37
Environmental factors known to contribute and influence this malocclusion include wrong postural habits of the mandible which pathologically alter the mandibular condyle positioning within the fossa and as a result the final mandibular spatial position expressed with a forward slide of the mandible. Various factors such as growth stimulus, history of prolonged sucking or resting tongue habits, atypical swallowing, nasal airway obstruction, mouth breathing, functional mandibular shifts because of respiratory needs, tongue size and pharyngeal airway shape and size altered (enlarged tonsils, large tongue, adenoids), hormonal imbalances and disturbances such as gigantism or pituitary adenomas, trauma, premature loss of primary teeth, congenital anatomic defects (ie, cleft lip, cleft palate), and muscle dysfunction alone or in combination with other environmental factors play a definitive etiological role.38–43
Component of Class III malocclusion
Class III malocclusion represents a complex three-dimensional facial skeletal imbalance between maxillary and mandibular growth along with varying degrees of dentoalveolar and soft tissue compensations which can be expressed in many morphological ways.44 Class III malocclusion may be associated with maxillary growth deficiency (and/or maxillary retrognathia), mandibular growth excess (and/or mandibular prognathism), or a combination of both along with vertical and transverse malformations.45–49 Based on the position of the maxilla relative to the craniofacial skeleton, Park and Baik classified Class III malocclusions into three basic types: true mandibular prognathism type A – individual with normal maxilla and prognathic mandible; type B – individual with excessive growth of maxilla and mandible, but with relatively more growth of mandible; type C – individual with maxillary hypoplasia, obtuse nasolabial angle, and concave facial profile. Type C individuals can easily be camouflaged orthodontically by dentoalveolar compensation.50
Common skeletal features such as shortened anterior (N-S) and posterior cranial base (S-Ar/Ba), reduced saddle angle (N-S-Ar), and an increased gonial angle (Ar-Go-Gn) were identified to lead to a more forward positioning of the glenoid fossa resulting in Class III malocclusion.51–53 Studies about the skeletal and dental components of Class III malocclusions have revealed the establishment of a facial pattern at early childhood which has a tendency to worsen with growth.54–58 Skeletal Class III malocclusions can be a result of various factors:
- prognathic and/or macrognathic mandible with a normal maxilla both in position and in size;
- retrognathic and/or micrognathic maxilla with a normal mandible both in position and in size;
- combination of retrognathic and/or micrognathic maxilla with prognathic and/or macrognathic mandible;
- normal skeletal jaw relationship with reverse overjet in the presence of centric relation (CR)–centric occlusion (CO) discrepancy, also known as a “pseudo” Class III relationship.
Dental features of Class III individuals include Class III molar and canine relationship, maxillary incisors protrusion and mandibular incisors retrusion with edge-to-edge bite or anterior crossbite. Based on various combinations of skeletal components, patients with Class III malocclusion exhibit a wide range of underlying skeletal and craniofacial features similar to the prevalence of Class III malocclusion, which can vary among different racial and ethnic groups as shown by comparative studies. For example, Mongoloid populations (Japanese, Koreans, and Chinese) with Class III phenotypes present with characteristic features such as acute anterior cranial base angle and a prominent and elongated mandible with a short and hypoplastic maxilla, while normal maxillary size and position were observed for Caucasians.51,59
Differential diagnosis of Class III malocclusion
The specter of problems of Class III malocclusion ranges in gravity from dentoalveolar problems with functional anterior shift of the mandible to true skeletal problems with serious maxillomandibular discrepancies, which leads to its highly challenging diagnosis.60
Differential diagnosis of Class III malocclusions and anterior crossbite in a step by step approach has been presented here based on the work of authors Ngan et al,6 Battagel,61 and Turley.62
History of the mandibular prognathism or anterior crossbite
The first question that should be asked to the patient or parents (caregiver) should concern mandibular prognathism or anterior crossbite in the family and close relatives. A history of it indicates a genetic cause of Class III malocclusion.
Examination of any functional shift
The second most important step is to access the relationship of maxilla and mandible in CR and CO to determine any functional shift. Molar and incisor relationship in this group of malocclusion is one of the most important diagnostic criteria. Class III malocclusion with positive overjet or edge-to-edge incisors relation accompanied by lingually inclined mandibular incisors represents a compensated form of Class III malocclusion. Anterior repositioning of the mandible may be due to abnormal tooth contact in CR that forces the mandible forward in CO.63 These pseudo Class III malocclusion individuals have a Class I skeletal pattern, orthognathic profile, and Class I molar relation in CR, but a Class III skeletal and dental pattern in CO.64 Elimination of the CO or CR discrepancy should show whether it is a simple Class I malocclusion or a compensated Class III malocclusion.65 In these individuals early correction proves to be a favorable environment for future growth.
Clinical assessment
This should be carried out while the patient is sitting upright in natural head position (NHP) to evaluate the sagittal and vertical facial proportions. The profile of the patient should be evaluated in NHP using “a line down from the bridge of the nose to the base of the upper lip and a second one extending from that point downward to the chin. A straight or concave profile in young patients indicates a skeletal Class III jaw relationship.”66 Similarly, the transverse dimension should be assessed to evaluate any facial or dental asymmetries. Examination of the temporomandibular joint, oral musculature, and intraoral soft and hard tissue should also be performed. Evaluation of the anterior crossbite aimed to differentiate a true Class III malocclusion from a pseudo Class III malocclusion has been described by Ngan et al,60,65 and the given diagnostic scheme can be adapted (Figure 1).
  | Figure 1 Summary of clinical practice guidelines for developing Class III malocclusion. Abbreviations: CR, centric relation; CO, centric occlusion; GTRV, growth treatment response vector. |
Lateral cephalogram analysis
Best analyses for cephalometric assessment of Class III malocclusion are those that correlate the maxilla to the mandible and each of them to the anterior cranial base. These are ANB (2°), Wits (0 mm), maxillomandibular differential (linear measurement from condylion to point A and condylion to gnathion: 23 mm for 12 years old), nasion perpendicular to point A (+2.3 mm), and nasion perpendicular pogonion (0 mm). Values of each of the cephalometric measurements presented here are for normal individuals.
It has been found in discriminant analysis that “Wits” appraisal is the most important factor in the decision making from orthodontic camouflage treatment to surgical options.66 A “Wits” appraisal from 0 to −5 mm may be suggestive of a Class III problem being resolved by means of orthodontic camouflage treatment with facemask or chin cup therapy.67 A “Wits” appraisal between −4 and −12 mm requires further growth treatment response vector (GTRV) analysis using serial cephalometric radiographs before a decision can be made of whether to camouflage or wait for comprehensive growth before surgical treatment.68
Growth trends of Class III malocclusion
For effective treatment planning and realistic prediction of stability of treatment outcomes in Class III growing patients, knowledge of growth trends is of paramount importance. Concern regarding early treatment and the need for interceptive care in the case of Class III treatment has always been a dilemma for clinicians as well as patients, knowing that not all problems will be solved in these cases until growth is further completed, and the outcomes in long term irrespective of treatment approaches may depend on the growth tendency of an individual.
Turpin69 in his editorial published in the American Journal of Orthodontics and Dentofacial Orthopaedics has emphasized that a deep understanding of the individual patient’s growth weighs much more than the treatment timing and treatment mechanics used on a specific Class III malocclusion growing patient whose timing of treatment is considered to be controversial. In essence, he summarized the studies of Mitani et al70 on Class III growth assessment over the years, as “the basic pattern of mandibular prognathism is established before puberty and does not change fundamentally. However, their total growth increments were about the same as those with a normal mandible after the pubertal growth peak.” The points raised by Turpin suggest that in spite of a controversial treatment timing the clinician should continue to have an interest in early interceptive treatment of Class III malocclusion as and when required.
Assessment of growth and prognosis in Class III patients
The prognosis of orthopedic treatment for skeletal Class III malocclusion is favorable when treatment is administered before the pubertal growth peak.71–74 However, a Class III malocclusion may worsen due to growth if a patient is left untreated. Therefore, early treatment is recommended for skeletal Class III malocclusion to obtain a balanced skeletal relationship and, by doing this, there is a possibility to minimize the need of further future complicated treatment such as orthognathic surgery.71–75
Studies have suggested that the posttreatment outcome of orthopedic treatment may not be stable depending on the residual growth.76 When unfavorable growth is expected, treatment would not be initiated in the early phase or would be delayed until completion of growth, because a discrepancy between maxillary, mandibular, and skeletal base growth during the pubertal phase can result in relapse of the corrections which have been achieved earlier,77 and as a result some patients ultimately may require orthognathic surgery at a later stage. This is a disappointing situation, not only for patients but also for clinicians, and may be prevented if accurate prediction of the eventual prognosis of early orthopedic treatment for skeletal Class III malocclusion would have been possible before commencing and executing treatment. As a result, patient selection and decision making regarding reliability of decisions and the timing of treatment would be much easier.78
Thus, the million dollar question which arises here is: Is the prediction of growth of mandible in growing Class III patient possible with optimal accuracy and reliability? Several investigators have taken this challenge and attempted to predict the prognosis of Class III malocclusion based on the evaluation of the patient’s single cephalogram for morphological characteristics and cephalometric analysis.79–83
Björk,79 based on single cephalogram analysis, defined seven structural signs of extreme growth rotation of mandible in the early developmental stage. These seven signs are “the inclination of the condylar head, curvature of the mandibular canal, shape of the lower border of the mandible, width of the symphysis, interincisal angle, intermolar angle, and anterior lower face height.” Even though seven structural signs of growth rotation have been reported,79 growth prediction of the mandible still remains a challenge, probably because mandibular growth shows wide variations in terms of amount, direction, and time or because the prediction procedure is based on individual reasoning.
Several cephalometric variables have been identified based on mandibular morphology by various studies to predict the results of early treatments.77,80–83 These studies reported long-term success rates of 50.0%–71.4% for orthopedic treatment of skeletal Class III malocclusion. Because of treatment success criteria, patient characteristics, and time points of outcome evaluation differed among studies; the reported success rates ranged widely and cannot be generalized to all patients treated for skeletal Class III malocclusion. In a recent study, Choi et al78 evaluated the long-term success of orthopedic treatment in growing skeletal Class III malocclusions, and verified previously reported success rates and prediction models. This research group found the same results published by previous researchers and concluded that no particular method or factor can predict the long-term success of orthopedic treatment for growing skeletal Class III malocclusions.
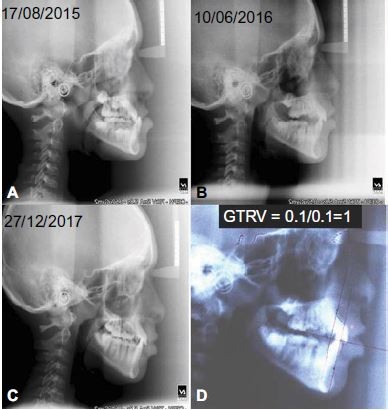
Assessment of direction and magnitude of mandibular and maxillary growth was proposed by Musich by using a serial cephalograms (D Musich, Growth treatment response vector analysis, personal communication, November 1, 2001). He proposed the GTRV analysis to predict the possibility of excessive mandibular growth after early interceptive orthopedic treatment in Class III patients. Based on immense clinical and extensive research experience in Class III malocclusion, Ngan described the use of serial cephalometric radiographs for GTRV analysis to predict excessive mandibular growth.84–86
GTRV
According to Ngan,84–86 “the horizontal growth changes of the maxilla and mandible are determined by locating the A and B points on the posttreatment lateral cephalometric radiograph. Another cephalogram should be taken during 2–4 years of follow-up visits after the treatment of Class III malocclusion with facemask therapy.” The incisal tip of maxillary incisor and mesiobuccal cusp tip of maxillary molar are used as a landmark to construct the occlusal plane (O). Point A and point B should be marked on the lateral cephalogram and connecting points A and B perpendicular to the occlusal plane would construct the lines AO and BO. Using stable landmarks on the midsagittal cranial structure, the nasion (N), and sella turcica (S), post-facemask treatment tracing (first tracing) is superimposed on the follow-up radiograph and the lines AO and BO are again constructed on the follow-up radiograph on the occlusal plane of the first tracing. The distance between the A points and point B of the two tracings along the occlusal plane represents the growth changes of the maxilla and mandible, respectively (Figure 2). After the measurements are completed, the GTRV ratio for each patient can be determined by using the formula:
GTRV = horizontal growth changes of the maxilla/horizontal growth changes of the mandible.
Hence, GTRV is defined as “the horizontal growth changes at A point divided by the horizontal growth changes at B point on the post-facemask and follow-up lateral cephalogram.” For an individual with the age range of 6–16 and with normal growth pattern, the GTRV ratio is 0.77. This suggests that the horizontal growth of mandible exceeds 23% as compared to the maxilla to maintain a normal skeletal relationship.
In studies by Ngan86 and Youssef et al,87 in patients treated with early interceptive orthopedic treatment, the GTRV ratios were significantly different for successful cases and unsuccessful cases. For successful cases, GTRV was in the range of 0.33–0.88 (mean 0.45) and for unsuccessful cases it was in the range of 0.06–0.38 (mean 0.22). This suggests that subjects with mild to moderate Class III malocclusion can be camouflaged orthodontically after successful early interceptive treatment, if the GTRV ratio ranges between 0.33 and 0.88. Class III patients with a GTRV ratio between 0.33 and 0.38 can be considered as borderline cases which can either be treated successfully with facemask or turn out to be surgical cases at the end and would better be warned of future need for surgical intervention, if the GTRV ratio is <0.38. Hence, the GTRV analysis as suggested by Ngan84–86 is helpful to the clinicians to assess the growth of the mandible to predict the prognosis after early interceptive orthopedic treatment of Class III malocclusion.
Treatment timing
It is an accepted fact that skeletal Class III malocclusion establishes itself early in life, is not a self-correcting disharmony,70,88 and is often associated with maxillary constriction. Intervention at an early stage, such as deciduous dentition, or prepubertal growth phase has been recommended.73,89 In particular, the prepubertal treatment of Class III malocclusion by means of rapid palatal expansion and facemask protraction yields favorable growth corrections both in maxilla and in the mandible.73 In a controlled long-term study, it has been found that patients who have been treated before the pubertal growth phase showed a stable increment in the maxillary skeletal width, maxillary intermolar width, and lateronasal width, while patients treated after the pubertal growth phase showed only dentoalveolar effects after the follow-up of ~8 years.90
The proper timing of interventions may therefore rely on chronological age91 and phases of dentition92 for very young patients, and on other radiological indicators, such as cervical vertebral maturation and/or hand and wrist maturation methods for older children.93 A summary of the timing of interventions and main indicators for Class III malocclusion has been presented in Table 3.
Treatment of developing Class III malocclusion
It is very critical to make a decision for developing Class III malocclusion on whether to treat or wait for further growth and dental development. Although a Class III malocclusion may be identified in the developing dentition, a decision needs to be made as to whether it is better to treat it at this stage or wait for further dental development and growth. The timing of early treatment is crucial for a successful outcome. Some studies have reported that treatment should be carried out in patients <10 years of age to enhance the orthopedic effect.71,94–96 In contrast, some studies found that age of the patient had little influence on treatment response and outcome.97,98 There is no strong evidence to support the notion that early treatment would be beneficial.
The main goals of early intervention are to create a more favorable environment for growth and to improve the occlusal relationship: for example, correcting the crossbite and facial esthetics.71 Hence, interceptive treatment of Class III malocclusions should be undertaken if it prevents damage to the oral tissues and prevents or significantly reduces the amount, or severity, of future orthodontic and surgical intervention.
Turpin99 developed a list of positive and negative factors that helped decision making on developing Class III malocclusions (Table 4) and these guidelines were reviewed by Campbell for deciding when to intercept Class III malocclusion.71 Turpin suggested that early interceptive treatment of Class III malocclusion should be considered for patients who presented with positive characteristics as mentioned. The author also recommended that individuals with negative characteristics should delay treatment until the completion of growth. He also suggested that patients should be warned that surgery may be needed in future, even after an early successful interceptive treatment.
  | Table 4 Turpin’s positive and negative factors for decision making for interception of developing Class III malocclusion |
Common cephalometric predictors for successful Class III camouflage for the evaluation of the maxillary and mandibular position include:
- ANB (<−2° to −3°);
- Wits appraisal (−2 to −6 mm for nonsurgical treatment, −6 to −9 mm for a compromised orthodontic result);
- maxillomandibular differential and gonial angle within the normal range.
The most important factor is clinical assessment to evaluate the need to optimize the facial esthetic. The combination of clinical and cephalometric information will identify which type of Class III malocclusion can be treated in the mixed dentition and help in deciding the best interceptive approach. A Class III patient with mild to moderate Class III skeletal patterns with a GTRV ratio between 0.33 and 0.88 can be successfully camouflaged orthodontically later after initial interceptive treatment in mixed dentition, and a GTRV ratio <0.38 should be warned. However, the GTRV ratio requires a serial lateral cephalogram to be obtained; so, this tool may not be suitable for decision making for new patients.84
In mixed dentition from the treatment point of view, there are effectively three types of Class III malocclusions:100,101
- dental: incorrect inclination or position of maxillary or mandibular incisors;
- pseudo: anterior positioning of the mandible as a result of premature dental contacts deflecting the mandible anteriorly to allow the patient to achieve full intercuspation;
- skeletal: true skeletal discrepancies in the maxilla and/or mandible.
Treatment of simple dentoalveolar anterior crossbites
A simple anterior crossbite can be corrected with either a removable appliance or a fixed appliance. The percentage of success is increased if there is a minimal existing proclination of the upper incisors and adequate overbite to maintain correction at the end of treatment. Types and indications of both types of appliances are provided below.
- Removable appliances: there are three types of removable appliances used to intercept the developing crossbite:
- inclined plane;
- modified inclined plane;
- active Hawley appliance.
- Fixed appliance:
- 2 by 4 appliance.
Inclined plane
An inclined plane is a good treatment choice in deciduous dentition or early mixed dentition.102 It is indicated in patients with:
- retroclined maxillary anterior teeth with an anterior crossbite with or without functional shift;
- well-aligned mandibular anterior teeth without proclination;
- normal to deep overbite;
- average to horizontal growth pattern patients.
The inclined plane is fixed onto the lower anterior teeth with temporary cement. Appropriate angulation between the inclined plane and the upper anterior teeth in crossbite should be determined by considering the vertical discrepancy between the teeth in crossbite and the adjacent teeth, as well as the degree of overbite of the teeth in crossbite by adjusting the different contact angulations. Most anterior dental crossbites can be corrected within 3–4 weeks using an inclined plane.
Modified inclined plane
Modified inclined plane is indicated in patients with an anterior dental crossbite, with lingually inclined maxillary incisors and labially inclined mandibular incisors; for this reason, an inclined plane is contraindicated because it may cause mandibular incisors proclination.103,104 A modified inclined plane is similar to that of a Hawley appliance plus an inclined plane on the anterior part. The inclined plane portion covers the lower anterior teeth up to their incisal third. When the patient bites, the inclined plane portion raises the bite and proclines the upper anterior teeth labially. The metal wire parts consist of a labial bow and Adam’s clasps on the first permanent molars for better appliance retention and stability. The labial bow is placed on the labial side of the lower incisors, near the cervical third, to ensure that the force application is closer to the center of resistance of the lower anterior teeth. The acrylic resin lingual to the lower incisors may be trimmed to allow lingual movement of the lower anterior teeth when the labial bow is activated. Anterior crossbite problems can be corrected within 3–4 weeks using a modified inclined plane. After the correction of anterior crossbite, the same appliance may be used as retainer by trimming of the anterior inclined plane portion.
Active Hawley appliance
A removable Hawley appliance is indicated in patients with anterior crossbite in mixed dentition stage.100 This appliance has an active component anteriorly to procline the upper anterior tooth or teeth to correct the anterior crossbite. This active component can either be a palatal “Z” spring, which is activated by the clinician, or a screw, which the patient activates. Usage of the Jack expansion screw is recommended to procline maxillary anterior teeth at the rate of one turn at every third day till the correction of anterior crossbite. The turning of the screw by a quarter turn (90°) brings about 0.18 mm of linear movement depending upon the pitch of the screw. Correction of 2 mm of overjet with this appliance can be achieved in 5–6 weeks. The appliance also incorporates retentive components (preferably Adam’s clasp) to keep the appliance in place and possibly posterior bite plate to disclude the occlusion to aid in uninterrupted proclination of anterior teeth. A removable appliance can only tip the teeth; so it should be only used if simple tipping movements of the upper anterior teeth are required.
Fixed appliance
This appliance is often referred to as a “2 by 4” or “2 by 6” appliance as it is only bonded on the two upper first permanent molars and the four upper incisors or six anterior teeth. Fixed appliances mostly use late mixed dentition or early permanent dentition. An open coil NiTi spring often compressed between the molars and the incisors to procline the incisors or a 0.016-inch stainless steel stoppered arch wire may be used to increase the arch length. Glass ionomer cement may be placed temporarily as a posterior fixed bite plane on the molars if disclusion is required. Fixed appliances allow tipping, bodily movement, and correction of rotations as and when required.
It has been seen that both types of appliances work well and the results are equally stable. Fixed appliance treatment is quicker and cheaper and has less effect on the patient’s speech than a removable appliance, but patients may complain of slightly more difficulty in chewing and biting initially with the fixed appliance.101–107
Growth modification and orthopedic treatment
Growth modification in developing Class III malocclusion is indicated in patients with skeletal discrepancy. The basic aim of this interceptive treatment for developing Class III malocclusion is to improve or correct the skeletal discrepancy to allow future treatment of such patients by orthodontic camouflage only without the need of orthognathic surgery. This approach of growth modification in Class III patients can be achieved through functional appliances, chin cup therapy, protraction facemask, and bone-anchored appliances. A brief description of each modality based on current evidence has been given below.
Functional appliances
Functional appliances have been used to modify the skeletal pattern by enhancing the growth of the maxilla and restricting or redirecting the growth of the mandible. Two commonly used functional appliances to intercept Class III malocclusion are Frankel functional regulator III appliance (FR III) and reverse twin-block appliance.
FR III has maxillary vestibular shields in the depth of the sulcus. These shields are placed away from the maxilla to stretch the periosteum and encourage anterior development of the maxilla. The lower part of the appliance attempts to restrict mandibular growth or redirect it posteriorly. In the reverse twin-block appliance, the blocks are positioned so that there are posterior forces on the mandible and anterior forces on the maxilla.
Current research suggests that functional appliances can improve occlusal relationships, but this is principally due to dentoalveolar changes, proclining upper incisors, and retroclining the lowers incisors.108–110 Evidence from a recent systematic review suggests that the FR III might restrict mandibular growth but not stimulate forward movement of the maxilla.111
Current evidence suggests that functional appliances can successfully correct a developing Class III malocclusion, but they have principally dentoalveolar effects, with minimal or no effects on the underlying skeletal pattern. Functional appliances especially FR III can be challenging to wear in the mouth and are subject to breakage; hence, a simpler method like orthodontic camouflage may be used in place of functional appliances.
Chin cup
Chin cup appliance treatment is indicated in young growing patients with mandibular prognathism. It has been found that chin cup therapy does not restrain mandibular growth but redirects the mandible growth vertically, causing a backward rotation of the mandible.112 These changes in the direction of mandibular growth help to improve Class III malocclusion. Recent systematic reviews showed that there is considerable agreement between studies in that chin cup therapy may be used for interceptive treatment of growing Class III malocclusion based on short-term favorable results.113,114
It has been seen that these changes are not maintained in the long term and the normal growth pattern of the mandible reestablishes itself, if chin cup appliance therapy is discontinued before growth completion.115 Hence, it is recommended that patients with Class III malocclusion with mandibular prognathism wear the chin cup appliance until growth is completed to maintain the treatment effects of chin cup therapy. Special care should be taken while deciding chin cup therapy in patients who present in the mixed dentition with marked mandibular prognathism, particularly if associated with increased vertical proportions, as these patients are often best treated by surgical orthognathic approach, when their growth is completed. As the long-term prognosis of chin cup therapy is unpredictable, patient caregivers should always be fully informed of this before initiating chin cup therapy. Line of force of applied force for chin cup therapy should be directed along the lines from the chin point to the condyle heads, bilaterally in the range of 400–500 g, 10–14 hours per day. While trying the chin cup appliance on patients, care should be taken to ensure that the chin cup does not impinge on the lower lips as it may cause retroclination of the lower incisors and recession of labial gingiva (Figure 3).
  | Figure 3 Chin cup appliance with line of force passing through the condyle. |
Protraction facemask
Protraction facemask also referred to as reverse headgear is one of the most commonly used interceptive tools to intercept developing skeletal Class III malocclusion.116 The appliance is composed of two components: an extraoral framework (facemask) that fits on the forehead and chin, and an intraoral attachment to the maxillary dentition (Figure 4). The chin and forehead part of the extraoral framework are connected by a middle bar for the connection of the elastics to the intraoral attachment to the maxillary dentition. The intraoral attachment is of various designs, including removable, banded, and acrylic-bonded versions. They all incorporate hooks bilaterally positioned near the maxillary canines. To minimize unwanted rotation of the palatal plane, Class III elastics should be attached near the maxillary canines at 30° to the occlusal plane. Bonded expansion appliance is preferred as it provides a temporary bite plane effect in hyperdivergent cases and facilitates the jumping of anterior crossbite in deep bite cases. The elastic forces are typically 400–450 g per side (14 to 16 OZ) and need to be worn 12–14 hours per day. The total treatment time is usually 6–9 months. An increased release of growth hormone and other growth promoting endocrine factors has been observed during evening and night than during the day. As a result, it is recommended to wear the appliance during evening and nighttime.
One controversial area is the use of rapid maxillary expansion (RME) at the same time as the protraction facemask. Often patients with a Class III skeletal pattern have a constricted maxilla in the transverse dimension as well as the anteroposterior dimension; so this expansion is a helpful component of the treatment. It has been suggested that expansion may loosen the circummaxillary sutures and increase forward movement of the maxilla. Results of a recent randomized controlled trial (RCT)117 and data from meta-analysis support the notion that facemask with and without RME treatment are both equally effective clinically in early treatment methods for skeletal Class III malocclusion. Hence, in case of no transverse discrepancy facemask without RME treatment can be undertaken. Maxillary expansion and protraction treatment for early permanent dentition is undertaken in case of transverse maxillary constriction.118 The expansion appliance is activated twice daily (0.25 mm per turn) for 7–10 days. In case of severely constricted maxilla, activation of the screw is carried out for ≥2 weeks.
In a randomized controlled clinical trial (CCT) comparing protraction facemask with no treatment, successful correction of the reverse overjet was observed in 70% of patients, with an average increase in overjet of 4 mm, and significant skeletal changes, principally due to forward movement of the maxilla and improvement in the ANB angle of 2.6° compared to the control at the end of treatment.119 These patients were followed up 6 years later to see if favorable changes were maintained toward the end of growth and in particular to assess whether the interceptive use of a facemask in the developing dentition can help reduce the need for orthognathic surgery.120 Of the patients that wore a protraction facemask, 36% needed orthognathic surgery at the age of 15, whereas 66% of patients in the control group required orthognathic surgery. Encouragingly, 68% of patients who wore the protraction facemask had a positive overjet after 6 years. To conclude, it appears that the use of a protraction facemask in the developing dentition will correct Class III malocclusion and reduce the need for orthognathic surgery in the future in the following types of cases:
- child under the age of 10;
- mild–moderate Class III;
- retrusive maxilla;
- average or reduced vertical proportions.
As the mandible resumes its original downward and forward growth after Phase I (facemask) therapy, patients may have reduced corrected overjet and more Class III molar relation during follow up and the second phase of orthodontic camouflage. Hence, the use of an extraoral orthopedic appliance (eg, chin cup) is recommended after the first phase of interceptive therapy with facemask till the completion of mandibular growth. It is also recommended to take the serial posttreatment cephalogram to calculate the GTRV to make a decision on whether to opt for orthodontic camouflage or wait till the completion of growth. A recent review published in 2017, in evidence-based dentistry, by Smyth and Ryan assessed early treatment of Class III malocclusion with facemask therapy and included randomized clinical trials and controlled clinical trials in children aged 7–12 years undergoing fixed or removable orthodontic treatment with the primary outcome of correction of the reverse overjet. The authors concluded that there is a moderate amount of evidence to show that early treatment with a facemask appliance has positive improvement for both skeletal and dental effects in the short term.121
Bone-anchored appliances
Interceptive treatment of Class III malocclusions with a tooth-borne protraction appliance (eg, facemask) often poses problems of unwanted dental changes such as:
- buccal tilting of maxillary molars and extrusion may lead to an increase in vertical dimensions and downward and backward growth of the mandible;
- decreased arch length due to mesial movement of maxillary molars leading to crowding in the anterior teeth.
In an attempt to overcome the limitations of tooth-borne appliances in the interceptive treatment of Class III malocclusions, bone-anchored maxillary protraction (BAMP) appliances have recently been used.122 BAMP appliances typically involve the use of Class III elastics attached between miniplates placed in the infrazygomatic crest to miniplates placed in the mandibular symphysis region or attached to the extraoral facemask (Figure 5). The success of these miniplates is related to the surgical technique and the thickness and quality of the bone. Particularly in the maxilla, the bone quality is often not as good until the patient is at least 11 years old; so this interceptive technique tends to be used in slightly older patients than the tooth-borne appliances. The results of an initial study on the effects of BAMP compared with growth of the untreated Class III subjects showed that the BAMP protocol induced an average increment on skeletal and soft tissue advancement of maxillary structures of about 4 mm with negligible changes in the maxillary incisor inclination and vertical skeletal pattern.123 Recent research also found that a Hybrid Hyrax bone-anchored rapid palatal expansion appliance minimized the side effect encounter by tooth-borne rapid palatal expansion appliances for maxillary expansion and protraction and may serve as an alternative treatment appliance for correcting Class III patients with a hyperdivergent growth pattern.124 Hence, BAMP has demonstrated promising initial results in its potential to offer greater skeletal changes, with less unwanted displacement of the dentition. However, there are unpredictable variations in individual outcomes, and high-quality research is needed to further investigate this technique.
Summary
For accurate diagnosis and successful execution of orthodontic treatment, it is very important that children with developing Class III malocclusion must be evaluated for family history, and should undergo dental examination for molar and incisor relationships, functional assessment to evaluate CO or CR shift on mandibular closure, and cephalogram analysis to determine sagittal jaw discrepancy. Evaluation of GTRV to determine the individual growth direction and rate should always be performed in borderline cases. A summary of diagnosis and treatments of developing Class III malocclusions is presented and Figure 1 may be used for quick reference.
- Interceptive treatment of Class III malocclusions may be undertaken if it prevents damage to the oral tissues and/or prevents or significantly reduces the amount, or severity, of future orthodontic treatment.
- Simple anterior dental crossbites can be successfully corrected with removable or fixed appliances in mixed dentition.
- Treatment with chin cup or functional appliances can correct a Class III incisor relationship, but any orthopedic changes are likely to be minimal with these appliances.
- Optimal timing for interceptive treatment with facemask is in the deciduous or early mixed dentition stage. Early interceptive treatment with a facemask allows for favorable sutural response for maxillary expansion and protraction; correction of any CO or CR discrepancies; and improvement in the facial profile and self-esteem in patients who are under 10, with mild to moderate Class III and a retrusive maxilla and with average or reduced vertical proportions. In case of mandibular prognathism, after facemask therapy patients should be advised to the wear the chin cup appliance until growth completion. A follow-up lateral cephalogram should be taken at 2–4 years after maxillary protraction to calculate the GTRV ratio. Information obtained from the GTRV ratio and from the cephalogram for the mandibular growth rate and direction is helpful in deciding whether Class III malocclusion can be camouflaged orthodontically or surgical intervention would be needed in the future. A case of Class III malocclusion treated successfully with facemask therapy has been presented in Figures 6–13.
- Bone-anchored appliances may offer the potential for more skeletal changes, but before its routine use more evidence is needed. Furthermore, bone-anchored appliances require help from surgeons.
  | Figure 6 Pretreatment photographs showing Class III malocclusion. |
  | Figure 7 Pretreatment digital study models showing Class III malocclusion. |
  | Figure 8 Maxillary splint with Hyrax expander cemented for facemask therapy. |
  | Figure 9 Posttreatment photographs. |
  | Figure 10 Posttreatment digital study models. |
  | Figure 11 Pretreatment and posttreatment cephalometric and panoramic radiographs. |
  | Figure 13 Posttreatment chin cup appliance therapy for mandibular growth redirection. |
Written informed consent was obtained from the parents or legal guardians of the children, to have the images published.
Acknowledgment
The authors are grateful to Professor OP Kharbanda, Chief of the Centre for Dental Education and Research, All India Institute of Medical Sciences (AIIMS), New Delhi for all clinical facilities, Dr Pradip Sangroula, Ex-Orthodontic resident, AIIMS for Figure 5, and Mr Netrapal, Dental Technician, AIIMS for scanning of models.
Disclosure
The authors report no conflicts of interest in this work.
References
Angle EH. Classification of malocclusion. Dent Cosmos. 1899;41:248–264. | ||
Ngan P, Moon W. Evolution of Class III treatment in orthodontics. Am J Orthod Dentofacial Orthop. 2015;148(1):22–36. | ||
Sugawara J. Clinical practice guidelines for developing Class III malocclusion. In: Nanda R, editor. Biomechanics and Esthetic Strategies in Clinical Orthodontics. 1st ed. Philadelphia: WB Saunders Co; 2005:211–242. | ||
Tweed CH. Clinical Orthodontics. St Louis: Mosby; 1966:715–726. | ||
De Clerck HJ, Proffit WR. Growth modification of the face: a current perspective with emphasis on Class III treatment. Am J Orthod Dentofacial Orthop. 2015;148(1):37–46. | ||
Ngan P, Hu AM, Fields HW. Treatment of Class III problems begins with differential diagnosis of anterior crossbites. Pediatr Dent. 1997;19(6):386–395. | ||
Hardy DK, Cubas YP, Orellana MF. Prevalence of angle Class III malocclusion: a systematic review and meta-analysis. Open J Epidemiol. 2012;2:75–82. | ||
Silva RG, Kang DS. Prevalence of malocclusion among Latino adolescents. Am J Orthod Dentofacial Orthop. 2001;119(3):313–315. | ||
Humphreys HF, Leighton BC. A survey of antero-posterior abnormalities of the jaws in children between the ages of 2 and 5 1/2 years of age. Br Dent J. 1950;88(1):3–15. | ||
Massler M, Frankel JM. Prevalence of malocclusion in children aged 14 to 18 years. Am J Orthod. 1951;37(10):751–768. | ||
Huber RE, Reynolds JW. A dentofacial study of male students at the University of Michigan in the physical hardening program. Am J Orthod Oral Surg. 1946;32(1):1–21. | ||
Newman GV. Prevalence of malocclusion in children six to fourteen years of age and treatment in preventable cases. J Am Dent Assoc. 1956;52(5):566–575. | ||
Goose DH, Thomson DG, Winter FC. Malocclusion in school children of the West Midlands. Brit Dent J. 1957;102:174–178. | ||
Ast DB, Carlos JP, Cons NC. The prevalence and characteristics of malocclusion among senior high school students in upstate New York. Am J Orthod. 1965;51(6):437–445. | ||
Hill IN, Blayney JR, Wolf W. The Evanston dental caries study. J Dent Res. 1959;38:782–794. | ||
Prabhat KC, Sandhya M, Sanjeev KV, Mohd T, Syed NZ. Modified fixed nanobite tandem appliance for rapid correction of developing Class III malocclusion. Orthodontics (Chic). 2013;14(1):e178–e185. | ||
Thilander B, Myrberg N. The prevalence of malocclusion in Swedish schoolchildren. Scand J Dent Res. 1973;81(1):12–21. | ||
Proffit WR, Fields HW, Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthodon Orthognath Surg. 1998;13(2):97–106. | ||
Garner LD, Butt MH. Malocclusion in black American and Nyeri Kenyans. An epidemiologic study. Angle Orthod. 1985;55(2):139–146. | ||
Horowitz HS, Doyle J. Occlusal relations in children born and reared in an optimally fluoridated community. II. Clinical findings. Angle Orthod. 1970;40(2):104–111. | ||
Emrich RE, Brodie AG, Blayney JR. Prevalence of Class I, Class II, and Class III malocclusions (angle) in an urban population. An epidemiological study. J Dent Res. 1965;44(5):947–953. | ||
da Silva Filho OG, de Freitas SF, Cavassan Ade O. [Prevalence of normal occlusion and malocclusion in Bauru (Sao Paulo) students. 2. Influence of socioeconomic level]. Rev Odontol Univ Sao Paulo. 1990;4(3):189–196. Portuguese. | ||
Mouakeh M, Sulaiman M. [Prevalence of malocclusion in a population of Syrian children and adults]. Aleppo Univ J Sci Res. 1996;23:17–22. Arabic. | ||
Toms AP. Class III malocclusion: a cephalometric study of Saudi Arabians. Br J Orthod. 1989;16(3):201–206. | ||
Kawala B, Antoszewska J, Necka A. Genetics or environment? A twin-method study of malocclusions. World J Orthod. 2007;8(4):405–410. | ||
Watnick SS. Inheritance of craniofacial morphology. Angle Orthod. 1972;42(4):339–351. | ||
Jena AK, Duggal R, Mathur VP, Parkash H. Class-III malocclusion: genetics or environment? A twins study. J Indian Soc Pedod Prev Dent. 2005;23(1):27–30. | ||
Litton SF, Ackermann LV, Isaacson RJ, Shapiro BL. A genetic study of class III malocclusion. Am J Orthod. 1970;58(6):565–577. | ||
Marković M. Results of a genetic study of triplets with class III malocclusion. Zahn Mund Kieferheilkd Zentralbl. 1983;71(2):184–190. | ||
Mossey PA. The heritability of malocclusion: part 1—genetics, principles and terminology. Br J Orthod. 1999;26(2):103–113. | ||
Harris JE, Kowalski CJ, Watnick SS. Genetic factors in the shape of the craniofacial complex. Angle Orthod. 1973;43(1):107–111. | ||
Nakasima A, Ichinose M, Nakata S, Takahama Y. Hereditary factors in the craniofacial morphology of Angle’s Class II and Class III malocclusions. Am J Orthod. 1982;82(2):150–156. | ||
Mossey PA. The heritability of malocclusion: part 2. The influence of genetics in malocclusion. Br J Orthod. 1999;26(2):195–203. | ||
Hodge GP. A medical history of the Spanish Habsburgs—as traced in portraits. JAMA. 1977;238(11):169–174. | ||
Chudley AE. Genetic landmarks through philately – the Habsburg jaw. Clin Genet. 1998;54(4):283–284. | ||
Huang CM, Mi MP, Vogt DW. Mandibular prognathism in the rabbit: discrimination between single-locus and multifactorial models of inheritance. J Hered. 1981;72(4):296–298. | ||
Cruz RM, Krieger H, Ferreira R, Mah J, Hartsfield J, Oliveira S. Major gene and multifactorial inheritance of mandibular prognathism. Am J Med Genet A. 2008;146A(1):71–77. | ||
Rakosi T, Schilli W. Class III anomalies: a coordinated approach to skeletal, dental, and soft tissue problems. J Oral Surg.1981;39(11):860–870. | ||
Chung JC. Redirecting the growth pattern with rapid maxillary expander and chin cup treatment: changing breathing pattern from oral to nasal. World J Orthod. 2006;7(3):236–253. | ||
Harris EF. Size and form of base of the skull in isolated cleft lip and palate. Cleft Palate Craniofac J. 1993;30(2):170–174. | ||
Cortés J, Granic X. Caractéristiques cranio-faciales chez un groupe de patients chiliens atteints de fente labio-maxillo-palatine unilatérale opérée. [Characteristic craniofacial features in a group of unilateral cleft lip and palate patients in Chile]. Rev Stomatol Chir Maxillofac. 2006;107(5):347–353. French. | ||
Graber TM. The “three M’s”: muscles, malformation, and malocclusion. Am J Orthod. 1963;49(6):418–450. | ||
Sugawara Y, Ishihara Y, Takano-Yamamoto T, Yamashiro T, Kamioka H. Orthodontic treatment of a patient with unilateral orofacial muscle dysfunction: the efficacy of myofunctional therapy on the treatment outcome. Am J Orthod Dentofacial Orthop. 2016;150(1):167–180. | ||
Sanborn RT. Differences between the facial skeletal patterns of Class III malocclusion and normal occlusion. Angle Orthod. 1955;25(4):208–222. | ||
Staudt CB, Kiliaridis S. Different skeletal types underlying Class III malocclusion in a random population. Am J Orthod Dentofacial Orthop. 2009;136(5):715–721. | ||
Ellis E, McNamara JA. Components of adult Class III malocclusion. J Oral Maxillofac Surg. 1984;42(5):295–305. | ||
Guyer EC, Ellis EE, McNamara JA, Behrents RG. Components of class III malocclusion in juveniles and adolescents. Angle Orthod. 1986;56(1):7–30. | ||
Jacobson A, Evans WG, Preston CB, Sadowsky PL. Mandibular prognathism. Am J Orthod. 1974;66(2):140–171. | ||
Williams S, Andersen CE. The morphology of the potential Class III skeletal pattern in the growing child. Am J Orthod. 1986;89(4):302–311. | ||
Park JU, Baik SH. Classification of Angle Class III malocclusion and its treatment modalities. Int J Adult Orthodon Orthognath Surg. 2001;16(1):19–29. | ||
Ngan P, Hagg U, Yiu C, Merwin D, Wei SH. Cephalometric comparisons of Chinese and Caucasian surgical Class III patients. Int J Adult Orthodon Orthognath Surg. 1997;12(3):177–188. | ||
Innocenti C, Giuntini V, Defraia E, Baccetti T. Glenoid fossa position in Class III malocclusion associated with mandibular protrusion. Am J Orthod Dentofacial Orthop. 2009;135(4):438–441. | ||
Baccetti T, Antonini A, Franchi L, Tonti M, Tollaro I. Glenoid fossa position in different facial types: a cephalometric study. Br J Orthod. 1997;24(1):55–59. | ||
Reyes BC, Baccetti T, McNamara JA Jr. An estimate of craniofacial growth in Class III malocclusion. Angle Orthod. 2006;76(4):577–584. | ||
Baccetti T, Franchi L, McNamara JA Jr. Growth in the untreated class III subject. Semin Orthod. 2007;13(3):130–142. | ||
Zionic Alexander AE, McNamara JA, Franchi L, Baccetti T. Semilongitudinal cephalometric study of craniofacial growth in untreated Class III malocclusion. Am J Orthod Dentofacial Orthop. 2009;135(6):700.e1–700.e14. | ||
Dietrich UC. Morphological variability of skeletal Class 3 relationships as revealed by cephalometric analysis. Rep Congr Eur Orthod Soc. 1970;46:131–143. | ||
Hopkin GB, Houston WJ, James GA. The cranial base as an aetiological factor in malocclusion. Angle Orthod. 1968;38(3):250–255. | ||
Mouakeh M. Cephalometric evaluation of craniofacial pattern of Syrian children with Class III malocclusion. Am J Orthod Dentofacial Orthop. 2001;119(6):640–649. | ||
Ngan P. Treatment of Class III malocclusion in the primary and mixed dentitions. In: Bishara SE, editor. Textbook of Orthodontics. Philadelphia: WB Saunders; 2001:375–414. | ||
Battagel JM. The aetiological factors in Class III malocclusion. Eur J Orthod. 1993;15(5):347–370. | ||
Turley PK. Treatment of the Class III malocclusion with maxillary expansion and protraction. Semin Orthod. 2007;13(3):143–157. | ||
Hidaka O, Adachi S, Takada K. The difference in condylar position between centric relation and centric occlusion in pretreatment Japanese orthodontic patients. Angle Orthod. 2002;72(4):295–301. | ||
Rabie ABM, Gu Y. Diagnostic criteria for pseudo-Class III malocclusion. Am J Orthod Dentofacial Orthop. 2000;117(1):1–9. | ||
Ngan P, Hu AM, Fields HW. Treatment of Class III problems begins with differential diagnosis of anterior crossbites. Pediatr Dent. 1997;19(6):386–395. | ||
Stellzig-Eisenhauer A, Lux CJ, Schuster G. Treatment decision in adult patients with Class III malocclusion: orthodontic therapy or orthognathic surgery? Am J Orthod Dentofacial Orthop. 2002;122(1):27–37. | ||
Ngan P. Early treatment of Class III malocclusion: is it worth the burden? Am J Orthod Dentofacial Orthop. 2006;129(4):S82–S85. | ||
Ngan P, Wei SHY. Early treatment of Class III patients to improve facial aesthetics and predict future growth. Hong Kong Dent J. 2004;1:24–30. | ||
Turpin DL. Good time for discussion of early treatment. Am J Orthod Dentofacial Orthop. 2000;118(3):247. | ||
Mitani H, Sato K, Sugawara J. Growth of mandibular prognathism after pubertal growth peak. Am J Orthod Dentofacial Orthop. 1993;104(4):330–336. | ||
Campbell PM. The dilemma of Class III treatment. Early or late? Angle Orthod. 1983;53(3):175–191. | ||
Joondeph DR. Early orthodontic treatment. Am J Orthod Dentofacial Orthop. 1993;104(2):199–200. | ||
Westwood PV, McNamara JA, Baccetti T, Franchi L, Sarver DM. Long-term effects of Class III treatment with rapid maxillary expansion and facemask therapy followed by fixed appliances. Am J Orthod Dentofacial Orthop. 2003;123(3):306–320. | ||
Ngan PW, Hagg U, Yiu C, Wei SH. Treatment response and long-term dentofacial adaptations to maxillary expansion and protraction. Semin Orthod. 1997;3(4):255–264. | ||
Wells AP, Sarver DM, Proffit WR. Long-term efficacy of reverse pull headgear therapy. Angle Orthod. 2006;76(6):915–922. | ||
Ryu H-K, Chong H-J, An K-Y, Kang K-H. Short-term and long-term treatment outcomes with Class III activator. Korean J Orthod. 2015;45(5):226–235. | ||
Yoshida I, Yamaguchi N, Mizoguchi I. Prediction of post-treatment outcome after combined treatment with maxillary protraction and chincap appliances. Eur J Orthod. 2006;28(1):89–96. | ||
Choi YJ, Chang JE, Chung CJ, Tahk JH, Kim K-H. Prediction of long-term success of orthopedic treatment in skeletal Class III malocclusions. Am J Orthod Dentofacial Orthop. 2017;152(2):193–203. | ||
Björk A. Prediction of mandibular growth rotation. Am J Orthod. 1969;55(6):585–599. | ||
Hägg U, Tse A, Bendeus M, Rabie ABM. Long-term follow-up of early treatment with reverse headgear. Eur J Orthod. 2003;25(1):95–102. | ||
Baccetti T, Franchi L, McNamara JA. Cephalometric variables predicting the long-term success or failure of combined rapid maxillary expansion and facial mask therapy. Am J Orthod Dentofacial Orthop. 2004;126(1):16–22. | ||
Ghiz MA, Ngan P, Gunel E. Cephalometric variables to predict future success of early orthopedic Class III treatment. Am J Orthod Dentofacial Orthop. 2005;127(3):301–306. | ||
Moon Y-M, Ahn S-J, Chang Y-I. Cephalometric predictors of long-term stability in the early treatment of Class III malocclusion. Angle Orthod. 2005;75(5):747–753. | ||
Ngan P. Biomechanics of maxillary expansion and protraction in Class III patients. Am J Orthod Dentofacial Orthop. 2002;121(6):582–583. | ||
Ngan P. Early timely treatment of Class III malocclusion. Semin Orthod. 2005;11(3):140–145. | ||
Ngan P. Early treatment of Class III malocclusion: is it worth the burden? Am J Orthod Dentofacial Orthop. 2006;129(4):S82–S85. | ||
Youssef MS, Nevzatoğlu S, Acar A. Growth treatment response vector (GTRV) analysis in Class III patients. Turkish J Orthod. 2012;25(3):214–223. | ||
Baccetti T, Reyes BC, McNamara JA. Craniofacial changes in Class III malocclusion as related to skeletal and dental maturation. Am J Orthod Dentofacial Orthop. 2007;132(2):171.e1–171.e12. | ||
Cha K-S. Skeletal changes of maxillary protraction in patients exhibiting skeletal Class III malocclusion: a comparison of three skeletal maturation groups. Angle Orthod. 2003;73(1):26–35. | ||
Baccetti T, Franchi L, Cameron CG, McNamara JA. Treatment timing for rapid maxillary expansion. Angle Orthod. 2001;71(5):343–350. | ||
Baccetti T, Franchi L, De Toffol L, Ghiozzi B, Cozza P. The diagnostic performance of chronologic age in the assessment of skeletal maturity. Prog Orthod. 2006;7(2):176–188. | ||
Franchi L, Baccetti T, De Toffol L, Polimeni A, Cozza P. Phases of the dentition for the assessment of skeletal maturity: a diagnostic performance study. Am J Orthod Dentofacial Orthop. 2008;133(3):395–400. | ||
Perinetti G, Franchi L, Contardo L. Determination of timing of functional and interceptive orthodontic treatment: a critical approach to growth indicators. J World Fed Orthod. 2017;6(3):93–97. | ||
Baccetti T, Tollaro I. A retrospective comparison of functional appliance treatment of Class III malocclusions in the deciduous and mixed dentitions. Eur J Orthod. 1998;20(3):309–317. | ||
Kim JH, Viana MA, Graber TM, Omerza FF, BeGole EA. The effectiveness of protraction face mask therapy: a meta-analysis. Am J Orthod Dentofacial Orthop. 1999;115(5):675–685. | ||
Battagel JM, Orton HS. A comparative study of the effects of customized facemask therapy or headgear to the lower arch on the developing Class III face. Eur J Orthod. 1995;17(6):467–482. | ||
Kapust AJ, Sinclair PM, Turley PK. Cephalometric effects of face mask/expansion therapy in Class III children: a comparison of three age groups. Am J Orthod Dentofacial Orthop. 1998;113(2):204–212. | ||
Atalay Z, Tortop T. Dentofacial effects of a modified tandem traction bow appliance. Eur J Orthod. 2010;32(6):655–661. | ||
Turpin DL. Early Class III treatment. Presented at: 81st Annual Session, American Association of Orthodontists; 1981; San Francisco. | ||
Littlewood SJ. Class III malocclusion. Chapter 10. In: Cobourne MT, editor. Orthodontic Management of Developing Dentition: An Evidence-Based Guide. Basel, Switzerland: Springer International Publishing AG; 2017:169–183. | ||
Ngan P, He H, Wilmes B. Treatment in Class III malocclusions in the growing patients. Chapter 4. Orthodontic Treatment of Class III Malocclusions. Sharjah: Bentham Science Publishers Ltd; 2014:61–115. | ||
Chang FH, Chang JZ. Treatment strategies for developing Class III patients. In: Nanda R, editor. Biomechanics and Esthetic Strategies in Clinical Orthodontics. St Louis: Elsevier; 2009:243–263. | ||
Ash MM, Ramfjord S. Occlusion. 4th ed. Philadelphia: WB Saunders; 1995:377–378. | ||
Wiedel A, Bondemark L. Fixed versus removable orthodontic appliances to correct anterior crossbite in the mixed dentition – a randomised controlled trial. Eur J Orthod. 2015;32(2):123–127. | ||
Wiedel A, Bondemark L. A randomized controlled trial of self-perceived pain, discomfort, and impairment of jaw function in children undergoing orthodontic treatment with fixed or removable appliances. Angle Orthod. 2015;86(2):324–330. | ||
Wiedel A, Bondemark L. Stability of anterior crossbite correction: a randomized controlled trial with a 2-year follow-up. Angle Orthod. 2016;85(2):189–195. | ||
Wiedel A, Norlund A, Petren S, Bondemark L. A cost minimization analysis of early correction of anterior crossbite – a randomized controlled trial. Eur J Orthod. 2016;38(2):140–145. | ||
Ulgen M, Firatli S. The effects of Fränkel’s function regulator on the Class III malocclusion. Am J Orthod. 1994;105(6):561–567. | ||
Seehra J, Fleming PS, Mandall N, DiBiase AT. A comparison of two different techniques for early correction of Class III malocclusion. Angle Orthod. 2012;82(1):96–101. | ||
Kidner G, DiBiase A, DiBiase D. Class III twin blocks: a case series. J Orthod. 2003;30(3):197–201. | ||
Yang X, Li C, Bai D, et al. Treatment effectiveness of Fränkel function regulator on the Class III malocclusion: a systematic review and meta-analysis. Am J Orthod Dentofacial Orthop. 2014;146(2):143–154. | ||
Uner O, YuKsel S, Ucuncu N. Long-term evaluation after chin cup treatment. Eur J Orthod. 1995;17(2):135–141. | ||
Tsolakis I, Ferdianakis E, Tsolakis AI. The effect of chin-cup therapy in Class III malocclusion: a systematic review. Open Dent J. 2016;10:664–679. | ||
Chatzoudi MI, Ioannidou-Marathiotou I, Papadopoulos MA. Clinical effectiveness of chin cup treatment for the management of Class III malocclusion in pre-pubertal patients: a systematic review and meta-analysis. Prog Orthod. 2014;15(1):62. | ||
Sugawara J, Asano T, Endo N, Mitani H. Long-term effects of chin cup therapy on skeletal profile in mandibular prognathism. Am J Orthod Dentofacial Orthop. 1990;98(2):127–133. | ||
Watkinson S, Harrison JE, Furness S, Worthington HV. Orthodontic treatment for prominent lower front teeth (Class III malocclusion) in children. Cochrane Database Syst Rev. 2013;9:CD003451. | ||
Liu W, Zhou Y, Wang X, Liu D, Zhou S. Effect of maxillary protraction with alternating rapid palatal expansion and constriction vs expansion alone in maxillary retrusive patients: a single center, randomized controlled trial. Am J Orthod Dentofacial Orthop. 2015;148(4):641–651. | ||
Zhang W, Qu H-C, Yu M, Zhang Y. The effects of maxillary protraction with or without rapid maxillary expansion and age factors in treating Class III malocclusion: a meta-analysis. PLoS One. 2015;10(6):e0130096. | ||
Anne Mandall N, Cousley R, DiBiase A, et al. Is early class III protraction facemask treatment effective? A multicentre, randomized, controlled trial: 3-year follow-up. J Orthod. 2012;39(3):176–185. | ||
Mandall N, Cousley R, DiBiase A, et al. Early class III protraction facemask treatment reduces the need for orthognathic surgery: a multi-centre, two-arm parallel randomized, controlled trial. J Orthod. 2016;43(3):164–175. | ||
Smyth RSD, Ryan FS. Early treatment of Class III malocclusion with facemask. Evid Based Dent. 2017;18(4):107–108. | ||
De Clerck HJ, Proffit WR. Growth modification of the face: a current perspective with emphasis on Class III treatment. Am J Orthod Dentofacial Orthop. 2015;148(1):37–46. | ||
De Clerck H, Cevidanes L, Baccetti T. Dentofacial effects of bone-anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am J Orthod Dentofacial Orthop. 2010;138(5):577–581. | ||
Ngan P, Wilmes B, Drescher D, Martin C, Weaver B, Gunel E. Comparison of two maxillary protraction protocols: tooth-borne versus bone-anchored protraction facemask treatment. Prog Orthod. 2015;16(1):26. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





