Back to Journals » International Journal of Women's Health » Volume 14
Determinants of Meconium-Stained Amniotic Fluid at Hadiya Zone Hospitals, Southern Ethiopia; Unmatched Case-Control Study
Authors G/silassie R, Gebretsadik W , Degefa N, Getahun D , Kassie N
Received 1 June 2022
Accepted for publication 8 September 2022
Published 16 September 2022 Volume 2022:14 Pages 1351—1360
DOI https://doi.org/10.2147/IJWH.S376963
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Rediet G/silassie,1 Woiynshet Gebretsadik,2 Nega Degefa,2 Dinkalem Getahun,2 Nigus Kassie3
1Department of Midwifery, College of Medicine and Health Sciences, Wachemo University, Hossana, Ethiopia; 2Schools of Nursing, College of Medicine and Health Sciences, Arba Minch University, Arba Minch, Ethiopia; 3Department of Midwifery, College of Medicine and Health Sciences, Dire Dawa University, Dire Dawa, Ethiopia
Correspondence: Rediet G/silassie, Email [email protected]
Background: Meconium-stained amniotic fluid (MSAF) refers to an amniotic fluid that is green in color or mixed with meconium. MSAF leads to a serious maternal complication that increases the likelihood of operative delivery and poses a hazard to the fetus or the neonate. This in turn enhances the chances of maternal and neonatal mortality and morbidity. So, the identification of determinants helps to breach this vicious cycle. The current study aimed to assess the determinants of MSAF.
Methods: An institution-based, unmatched case-control study with a sample size of 363 participants (121 cases and 242 controls) was conducted on mothers who gave birth at Hadiya zone public hospitals between March and April 2020. A proportionate distribution was made to each facility depending on the volume of patients, and cases and control mothers were chosen sequentially. The data was gathered through in-person interviews and secondary data extraction. In multivariable logistic regression, variables with (p < 0.25) in bivariate analysis were included. After multivariable logistic regression was finished, statistical significance was declared at (p < 0.05).
Results: A total of 121 cases and 242 controls were included in this study Multivariable logistic regression analysis showed that gestational age ≥ 41 week (AOR = 3.44, 95% CI: 1.02– 11.63), premature rupture of membrane (AOR = 3.71, 95% CI: 1.98– 6.93) obstructed labor (AOR = 2.90, 95% CI: 1.15– 7.33) preeclampsia (AOR = 4.16, 95% CI: 1.29– 13.35) and non-reassuring fetal heart rate (AOR = 6.75, 95% CI: 3.45– 13.19) were significantly associated with MSAF.
Conclusion: Advanced gestational age, an early membrane rupture, an obstructed labor, preeclampsia, and non-reassuring fetal heart rate all increase the incidence of meconium-stained amniotic fluid in laboring mothers. Making every effort to prevent, identify, and treat those obstetric determinants as early as feasible should be taken into consideration throughout follow-up of pregnancy, labor, and delivery could assist to lower the incidence of MSAF.
Keywords: amniotic fluid, determinants, meconium stained
Background
Amniotic fluid is the liquid that retains and insulates a fetus in the uterus throughout pregnancy. Meconium, a dark greenish first stool that is typically passed by the newborn during the first 48 hours after birth. The amniotic fluid turns green if a baby passes meconium before birth (while still within the uterus). Meconium stained amniotic fluid (MSAF) is the name for this property of liquor. Meconium is made up of 70–80% water, digestive contents, desquamated cells, lanugo, amniotic fluid, bile acids, salts, mucus, and other inflammatory modulators. Bile pigments are thought to be responsible for the greenish color of the meconium.1,2
There are three categories of meconium-stained liquor, with Grade I (light) containing the least quantity of meconium and the most amniotic fluid. Only a tiny greenish or yellowish tint results from this on the waters. When there is a decent volume of amniotic fluid, yet it is stained with meconium, that condition is known as grade II (moderate) meconium staining. The water seems really severe green or brown in this situation. When there is little amniotic fluid and a lot of meconium, the staining becomes grade III (heavy/quite thick), and it can be very dark green or black.3,4
Exposure to and aspiration of particulate meconium, either intrauterine or during the first breath, causes birth asphyxia, respiratory distress and may cause serious respiratory morbidity, such as Meconium Aspiration Syndrome (MAS).5,6 In addition to endangering the fetus or the baby MSAF can result in major maternal problems such as chorioamnionitis, surgical site infection, and puerperal endometritis. Besides, evidence suggests that MSAF raises the rates of instrumental births and cesarean sections.7–9
Around the world, MSAF complicates 10–15% of births, and research has shown that as gestational age increases, so does the prevalence of the condition. It happens in 5% of preterm births, 25% of term births, and up to 52% of post-term babies.10,11
According to studies, the incidence of MSAF varies from 6.13% to 19% in Asia3,7 reaching up to 23.5% in the Australian population.12 It is about 11.15% in Africa and Inhaling meconium is a possibility in about 10% of all births in Sub-Saharan African countries.13,14 According to studies, there are roughly 16.7% cases of MSAF in Ethiopia.15,16
MSAF affects 15% of all live-birth infants worldwide. About 5–12% of these newborns go on to develop MAS, which is characterized by severe respiratory distress and necessitates mechanical ventilation in about 50% of affected neonates. MAS continues to be a threat to many newborns around the world, with a case fatality rate of 5% to 40%.6,17,18
Although the precise cause of MSAF is uncertain, it has been suggested that it is physiological and shows signs of gastrointestinal and central nervous system maturation. Additionally, it is thought to be an indication of fetal discomfort in reaction to a short-term or long-term hypoxic insult.19,20
Recent studies conducted globally in various locations revealed that, an advanced maternal age, status of Antenatal Care (ANC) follow up, anemia, prim gravidity, previous caesarean section scar, advanced gestational age, preeclampsia, Induction of labor, fetal distress, labor dystocia, prolonged labor, birth weight of the neonate, and sex of the neonate as significant determinants for the occurrence of MSAF.15,21–24
The existing evidence in Ethiopia emphasized on the magnitude and consequences of MSAF. Information on the determinants is scarce. To the best of our knowledge, no study has examined the determinants of MSAF in the study area. Therefore, the aim of this study was to identify the determinants of MSAF at public hospitals in the Hadiya zone of southern Ethiopia.
Methods and Materials
Study Area and Period
The study was conducted in Ethiopia’s Southern nations, nationalities, and people’s region in public hospitals of Hadiya zone. One of the region’s 14 zones, in the zone, 26.9% of deliveries were attended in medical facilities, and 86.3% of ANC services were used.24,25 In the zone, there are three primary hospitals located in three different woredas (Homacho, Shone, and Gimbichu primary hospitals), which have 145, 160, and 87 average monthly deliveries, respectively, and one referral hospital (Wachemo University Nigist Elleni Mohammod memorial teaching and referral hospital) located in Hosana town, which is found 232 kilometers south of the capital Addis Ababa and 194 kilometers away from the regional capital, Hawassa. This study was conducted from March 16 – to April 16, 2020.
Study Design
An institution-based unmatched case-control study was conducted.
Participants
All mothers that gave birth in public hospitals of the Hadiya zone during the study period were the study population.
Cases: Mothers who were diagnosed with MSAF regardless of the grade of staining.
Controls: Mothers who were not diagnosed with MSAF but admitted to the labor and delivery ward of the same hospital.
Inclusion Criteria
Those mothers who delivered a live baby were included.
Exclusion Criteria
Mothers who had postpartum hemorrhages, mothers who were unconscious, and clients whose records were insufficient (ie, lacked basic laboratory tests) were not included in the study.
Sample Size Determination
The sample size was determined by EpiInfo-7 Stat Calc using the double population proportion exposure difference formula, taking into account the percentage of controls exposed for induction of labor is 67.6% (main exposure variable), the percentage of cases with exposure is 84.4% from a study conducted in Felege Hiwot Hospital Bahirdar Ethiopia.15 95% CI, 90% power of the study, and a 1:2 ratio of the case to control is assumed with a 2.6 odds ratio. A 10% non-response rate was added, resulting in a final sample size of 363 people (121 cases and 242 controls).
Sampling Procedure
The Hadiya zone’s public hospitals were all included (one referral hospital and three primary hospitals). Based on each institution’s average monthly labor and delivery report from the previous year, the entire sample was distributed to them in proportion. Finally, cases were chosen sequentially by looking through their birth cards for reported diagnoses in MSAF. The next two consecutive mothers who gave birth after the index case in the same hospital but did not get a diagnosis of MSAF were chosen for the control group. After the first four hours following delivery, both cases and controls were enrolled in the immediate post-natal unit (Figure 1)
 |
Figure 1 Schematic diagram of sampling procedure to identify determinants of MSAF in Hadiya zone public hospitals southern Ethiopia, 2020. |
Study Variables
Dependent Variable
Meconium stained amniotic fluid.
Independent Variables
Socio-demographic determinants: - maternal age, residency, educational status, marital status and occupation.
Obstetric related determinants:- gestational age, Antenatal care (ANC) follow up, number of ANC follow up, iron intake during ANC, gravidity, history of abortion, previous caesarean section scar, PROM, prolonged PROM, induction of labor, preeclampsia, eclampsia, cord prolapsed, duration of labor, obstructed labor, NRFHR.
Medical related determinants: - anemia, hepatitis virus, Rh factor, Human Immune Virus (HIV), chronic hypertension.
Behavioral related determinants: - Cigarette smoking, Cocaine use, marijuana addict and chat chewing.
Neonatal related determinants: - birth weight and sex of the neonate.
Operational Definition
Meconium-stained amniotic fluid (MSAF): Amniotic fluid is stained with meconium, after a natural or artificial rupture of the membranes, and can be visually identified by speculum or per vaginal examination.15
Data Collection Tools and Procedure
An interviewer-administered questionnaire and a data extraction guide from previous literature15 were used for data collection. The questionnaire was prepared with the category of interest socio-demographic characteristics, prepared with the category of socio-demographic characteristics, obstetric related determinants, and medical-related determinants, behavioral and neonatal related determinants. The developed questionnaire’s English version was converted to the Amharic version, which is widely spoken in the study area, and then returned to English to ensure consistency. Four diploma midwives collected the data under the supervision of two Bsc midwives who had previous experience in data collection.
After four hours of delivery (when the mother becomes stable), a face-to-face interview with the index mothers was conducted in the immediate post-natal unit. Then, using the data extraction guide, pertinent information was gathered from their record.
Data Quality Management
Before collecting data, data collectors and supervisors received two days of training on the data collection tool, collection methods, ethical issues, and study goal. In order to check for consistency and any unclear questions in the tool, a pretest was carried out in Doyogena primary hospital with 18 respondents, or 5% of the calculated sample size, consisting of 6 cases and 12 controls. The period of data collection was closely supervised. The supervisor also went over the information to look for any mistakes or omissions that might have crept into the records.
Data Processing, Analysis, and Interpretation
Data was cleaned, coded, and put into the Epi-data program version 3.1 before being exported to SPSS version 25 for analysis. Data were then reviewed for completeness and consistency. The data were subjected to a descriptive analysis, and the study’s final findings were presented as text and tables. The Variance Inflation Factor (VIF) evaluated the presence of multi co-linearity to identify determinants of MSAF, a binary logistic regression was conducted, and a crude odds ratio (COR) and an adjusted odds ratio (AOR) with a 95% CI were estimated. A multivariable logistic regression model was used to input and assess the variables that exhibited a relationship in the bivariate model (p < 0.25), in order to determine the independent contribution of each factors to the occurrence of MSAF. Hosmer and Leme show’s goodness of fit test was checked, and it was found to be insignificant (p-value= 0.56) which indicates the model was good fitted and the full logistic regression model was a significant prediction performance [omnibus test of model coefficients (p < 0.00)].
Ethical Consideration
The Arba Minch University College of Medicine and Health Science’s Institutional Research Ethics Review Board granted approval for the study. The institution requested authorization to collect data from the appropriate Hadiya zone public hospitals and administrative entities in a formal letter. Before the in-person interview, each respondent gave written informed consent;
Individuals under the age of 18 provided informed consent on their own behalf, a formal written asset was obtained from each, and the ethics committee approved the consent process for those participants. To protect the privacy of respondents, questionnaires were filled out anonymously. Thoroughly, our research complies with the required principles of Declaration of Helsinki General Assembly, Seoul, Korea, and October 2008.
Results
Socio-Demographic Characteristics
A total of 363 mothers—121 cases and 242 controls—participated in this study, yielding a response rate of 100%. For cases, the median age of mothers is 27.00 (IQR ± 8), while for controls, it is 27.00 (IQR ± 6). Most of the participants (69.4% cases and 73.1% controls) were Hadiya ethnicity followed by 9.9% of cases and 10.7% of controls were Kembata ethnicity. Out of the total mothers 61.2%and 62.0% had protestant, and orthodox religion followers for cases 24.85% and 20.2% for controls, respectively (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Mothers for the Study of MSAF in Hadiya Zone Public Hospitals of Southern, Ethiopia, 2020 |
Obstetric and Medical Related Determinants of MSAF
This study revealed that more than half of 65 (53.7%) cases and 163 (67.4%) controls were multigravidas. Among those multi gravidas 10 (15.4%) cases 15 (9.2%) controls and 15 (23.1%) cases and 27 (16.6%) controls had history of abortion and cesarean section scar, respectively. Most of the mothers 103 (85.1%) among cases and 202 (83.5%) among controls had ever got ANC service. And among those who attained ANC follow up, 92 (89.3%) cases and 186 (92.1%) controls had history of iron intake during pregnancy. Nearly almost all 118 (97.5%) cases and 238 (98.3%) controls had less than 24 hours duration of labor. Regarding medical conditions of mothers, six (5.0%) cases and sixteen (6.6%) controls had Hepatitis B virus, 12 (9.9%) cases, and 17 (7.0%) control mothers had anemia (Table 2).
 |
Table 2 Obstetric and Medical-Related Determinants of MSAF in Hadiya Zone Public Hospitals of Southern Ethiopia, 2020 (n = 363) |
Behavioral Related Determinants of MSAF
The finding of this study showed that almost all mothers, neither from cases nor from controls had no history of any drug addiction and cigarette smoking.
Neonatal Related Determinants of MSAF
In this study more than half of 68 (56.2%) cases and 141 (58.3%) controls had delivered male neonates and 47 (38.8%) newborns from cases 118 (48.8%) from control’s weight was between 3000–3499-gram (Figure 2).
 |
Figure 2 Neonatal weight in the study of determinants of MSAF in Hadiya zone public hospital of southern Ethiopia, 2020 (cases = 121, controls = 242). |
Determinants Associated with Meconium-Stained Amniotic Fluid
The multivariable logistic regression result showed that Gestational age, PROM, preeclampsia, obstructed labor, and Non-Reassuring Fetal Heart Rate (NRFHR) were significantly associated with MSAF.
The odds of having MSAF were about 3.4 times higher among women with a gestational age of ≥41 weeks (late-term) compared to women who had a gestational age <37 weeks (preterm) and between 37 and 40 weeks (term) (AOR = 3.44, 95% CI: 1.02–11.63). Accordingly, the odds of MSAF occurrence were around four times higher among women with rupture of membrane before the onset of labor compared to women without PROM (AOR = 3.71, 95% CI: 1.98–6.93).
The odds of developing MSAF were almost three times higher among women who had obstruction of labor as compared to those who had good labor progress (AOR = 2.90, 95% CI: 1.15–7.33). In addition to this, preeclampsia has significantly associated with the occurrence of MSAF, the odds of having MSAF was four times higher among mothers who had preeclampsia during labor were, compared to those without preeclampsia (AOR = 4.16, 95% CI: 1.29–13.35).
The odds of MSAF occurrence were around seven times higher among mothers who had an abnormal fetal heart rate pattern during labor as compared to their counterparts (AOR = 6.75, 95% CI: 3.45–13.19) (Table 3).
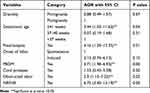 |
Table 3 Bivariable and Multivariable Logistic Regression Analysis Result for the Study of Determinants of MSAF in Hadiya Zone Public Hospitals of Southern Ethiopia, 2020 |
Discussion
The finding of this study indicated that mothers with Gestational Age ≥41 weeks, premature rupture of membrane, preeclampsia, obstructed labor, and non-reassuring fetal heart rate during labor had an increased risk of MSAF.
This study found a statistically significant association between MSAF and gestational age ≥41 weeks (late-term) pregnancy. Findings from earlier studies carried out in Australia12 and Iran22 provide evidence in favor of this finding. This could be because in late-term pregnancy the placenta has reached its maximum size and the age of the placental tissue has started to diminish its function, failing to deliver enough oxygen and nutrients to the fetus, which causes uteroplacental vascular insufficiency and increases the risk of MSAF.26
Statistically significant differences were demonstrated between the two groups when analyzing PROM with MSAF. This finding is similar to studies reported from India in 201727 and Cameron in 2016.14 This could be due to the fact that sterile protective amniotic fluid has been lost; an unborn child will be exposed to nutritional loss, bacterial infections, and inflammation of the fetal membrane (chorioamnionitis). Then the one infection results in intrauterine fetal hypoxia, all of which enhance the risk of MSAF taking place.28
Additionally, it was found that obstructed labor had a strong correlation with MSAF. This finding is supported by a study carried out in Ethiopia15 and India.24 This may be the result of the presenting part becoming impacted into the pelvic wall during obstructed labor despite strong uterine contractions, which causes fetal discomfort and hypoxia and ultimately results in the development of MSAF.
There was a statistically significant correlation between preeclampsia and MSAF. This result is consistent with research from tertiary care facilities in India24 and Ethiopia.15 The cause may be attributed to the potential of preeclampsia-related poor placentation, which alters utero-placental blood flow and causes intermittent perfusion and prolonged hypoxia that culminating in a meconium passage at last.30 Similar to this, NRFHR showed a strong correlation with the development of MSAF, with laboring mothers who had aberrant fetal heartbeat tracings having a roughly seven-fold increased risk compared to their counterparts. This result is in line with research conducted in Israel in 201531 as well as in India in 2016 and 2018.23,24
This may be the result of the fetal compensatory mechanisms switching to anaerobic cellular metabolism in the presence of an abnormal fetal heart rate pattern. This results in the production of ATP and large amounts of lactic acids, which must then be converted back to pyruvic acid by the liver and muscles. Because of that, the body uses a lot more oxygen for conversion than it would otherwise. This is referred to as “paying off the debt” and exposes the body to hypoxia. Some lactic acids are left in the muscle fibers where they contribute to muscular exhaustion and impair the function of the rectal sphincters, causing meconium to flow.32
The strength of this study is that the measurement of the outcome variable was based on a professionally verified diagnosis of MSAF, and the study employed an appropriate control group for the cases that were chosen. Both groups were enrolled in the same hospital’s immediate postnatal ward.
The limitation of this study is, due to the case-control study’s characteristic retrospective nature, which makes it difficult to establish causation; this study simply tries to find correlations between independent variables and the outcome variable.
Conclusion
The results of this study reveal that Gestational Age ≥41 weeks, premature rupture of membrane; preeclampsia, obstructed labor, and non-reassuring fetal heart rate during labor are all statistically significant independent predictors of MSAF risk in women.
Recommendations
In order to avoid the negative effects of post-term pregnancy, the authors recommend health practitioners who monitor the progress of pregnancies to take into account stripping or sweeping the membranes and inducing labor before 41 weeks of gestation.
Additionally, it is advised that preeclampsia prevention efforts should focus on encouraging pregnant mothers to drink plenty of water daily, avoid junk food and fried foods, get enough sleep, and exercise regularly. If a mother has more than one moderate risk factor or more than one high-risk factor for preeclampsia, her doctor may also recommend her to take low-dose aspirin after 12 weeks of pregnancy. Similar to this, supplementing with vitamin C after the 14th week of pregnancy is advised in order to prevent PROM.
Assessing the pelvic outlet, determining the baby’s presentation and position, gauging the fetal head’s descent, and monitoring labor with a partograph are all strategies to improve the capacity to identify obstructed labor early and prevent its impact on the development of MSAF. Additionally, it is preferable to advance the auscultation of the fetal heart rate for all mothers who are in labor, and when the NRFHR trace is first observed, it is preferable to carry out stringent management procedures such rehydration, oxygen administration, and left lateral posture.
Abbreviations
ANC, Antenatal care; AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crud Odds Ratio; HIV, Human Immunodeficiency Virus; MAS, Meconium Aspiration Syndrome; MSAF, Meconium Stained Amniotic Fluid; NRFHR, Non-Reassuring Fetal Heart Rate; PROM, Premature Rupture of Membranes.
Data Sharing Statement
The datasets used and/or analyzed for the current study are available from the corresponding author on reasonable request.
Acknowledgment
Our special gratitude and appreciation go to Arba Minch University, study participants, data collectors, supervisors, and Hadiya zone public hospital staff for their valuable support.
Funding
Arba Minch University funded the research and it is open for the researchers to publish the manuscript. The funder had no role in study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors have declared that no competing interests exist.
References
1. Mitchell S, Chandraharan E. Meconium-stained amniotic fluid. Obstet Gynaecol Reprod Med. 2018;28(4):120–124. doi:10.1016/j.ogrm.2018.02.004
2. Soni A, Vaishnav GD, Gohil J. Meconium and its significance and obstetric outcome. Med Sci. 2015;4(1):1861–1868. doi:10.5455/medscience.2014.03.8183
3. Thunga S, Singh P. Clinical study of meconium stained amniotic fluid. Int J Biomed Adv Res. 2014;5(12):612–614.
4. Jahan K, Haque A, Jahan L. Perinatal outcome in high-risk pregnancies with and without meconium stained liquor amnii. JMSCR. 2019;7. doi:10.18535/jmscr/v7i2.68
5. Nadia M, Hafiz T, Arjumand S, Syed R. AliMeconium stained liquor and its neonatal outcome. Pak J Med Sci. 2018;34:1392.
6. Hutton EK, Thorpe J. Consequences of meconium stained amniotic fluid: what does the evidence tell us? Early Hum Dev. 2014;90(7):333–339. doi:10.1016/j.earlhumdev.2014.04.005
7. Nesa F, Chowdhury F, Yasmeen BN, Rahman S, Begum N, Hossain SA. Mode of delivery and fetal outcome in meconium stained amniotic fluid in DMCH. North Int Med Coll J. 2018;9(2):304–307. doi:10.3329/nimcj.v9i2.38912
8. Brabbing-Goldstein D, Nir D, Cohen D, Many A, Maslovitz S. Preterm meconium-stained amniotic fluid is an ominous sign for the development of chorioamnionitis and for in utero cord compression. J Matern Fetal Neonatal Med. 2017;30(17):2042–2045. doi:10.1080/14767058.2016.1236246
9. Mohammad N, Jamal T, Sohaila A, Ali SR. Meconium stained liquor and its neonatal outcome. Pak J Med Sci. 2018;34(6):1392–1396. doi:10.12669/pjms.346.15349
10. Kliegman R, Stanton B, Geme JW, Schor NF, Behrman RE. Nelson Textbook of pediatrics. Phialdelphia, PA: Elsevier; 2016.
11. Balchin I, Whittaker JC, Lamont RF, Steer PJ. Maternal and fetal characteristics associated with meconium-stained amniotic fluid. Obstet Gynecol. 2011;117(4):828–835. doi:10.1097/AOG.0b013e3182117a26
12. Carr BL, Copnell B, McIntyre M. Differences in meconium stained amniotic fluid in an Australian population: a retrospective study. Women Birth J Aust Coll Midwives. 2019;32(2):e259–63. doi:10.1016/j.wombi.2018.06.001
13. Anwar M. Effects of meconium aspiration in new-born in developing countries in Sub-Saharan African perspective. Journal of Pediat Ther. 2016;6(1):39.
14. Edmond NM, Philip NN, Julienne SN, Julius SD, Evelyn M. Perinatal outcome in term pregnancies with meconium stained amniotic fluid in two referral hospitals of yaoundé- Cameroon. Biomed J Sci Tech Res. 2018;2(2):2533–2537.
15. Addisu D, Asres A, Gedefaw G, Asmer S. Prevalence of meconium stained amniotic fluid and its associated factors among women who gave birth at term in Felege Hiwot comprehensive specialized referral hospital, North West Ethiopia: a facility based cross-sectional study. BMC Pregnancy Childbirth. 2018;18(1):429. doi:10.1186/s12884-018-2056-y
16. Woldie M. Meconium stained amniotic fluid: factors affecting maternal and perinatal outcomes at Jimma university specialized teaching hospital, South West Ethiopia. Gynecol Obstet. 2016;10(6):1–6.
17. Jain PG, Sharma R, Bhargava M. Perinatal outcome of meconium stained liquor in pre-term, term and post-term pregnancy. Indian J Obstet Gynecol Res. 2021;4(2):146–150.
18. Yurdakök M. Meconium aspiration syndrome: do we know? Turk J Pediatr. 2011;53(2):121–129.
19. Argyridis S, Arulkumaran S. Meconium stained amniotic fluid. Obstet Gynaecol Reprod Med. 2016;26(8):227–230. doi:10.1016/j.ogrm.2016.05.001
20. Monen L, Hasaart TH, Kuppens SM. The aetiology of meconium-stained amniotic fluid: pathologic hypoxia or physiologic foetal ripening? (Review). Early Hum Dev. 2014;90(7):325–328. doi:10.1016/j.earlhumdev.2014.04.003
21. Rao KS, Pathapati S, Vansipriya C. Risk factors for meconium stained liquor and outcome of neonate in meconium stained amniotic fluid. Indian J Obstet Gynecol Res. 2021;4(1):1–5.
22. Zarepur A, Arab Maghsoudi M, Zarepur E, Zarepur R, Zarepur F, Gharlipour Z. Study of the relationship between meconium passage and newborns birth weight and its related factors in pregnant women. Int J Pediatr. 2017;5(1):4185–4192.
23. Rathoria R, Rathoria E, Bansal U, et al. Study of risk factors and perinatal outcome in meconium stained deliveries from a district of Uttar Pradesh, India. Int J Reprod Contracept Obstet Gynecol. 2018;7(9):3605–3609. doi:10.18203/2320-1770.ijrcog20183761
24. Sundaram R, Murugesan A. Risk factors for meconium stained amniotic fluid and its implications. Int J Reprod Contracept Obstet Gynecol. 2017;5(8):2503–2506.
25. Abosse Z, Woldie M, Ololo S. Factors influencing antenatal care service utilization in Hadiya zone. Ethiop J Health Sci. 2010;20(2):75–82. doi:10.4314/ejhs.v20i2.69432
26. Asseffa NA, Bukola F, Ayodele A. Determinants of use of health facility for childbirth in rural Hadiya zone, Southern Ethiopia. BMC Pregnancy Childbirth. 2016;16(1):355. doi:10.1186/s12884-016-1151-1
27. Ayyavoo A, Derraik JG, Hofman PL, Cutfield WS. Postterm births: are prolonged pregnancies too long? J Pediatr. 2014;164:45. doi:10.1016/j.jpeds.2013.11.010
28. Desai D, Maitra N, Patel P. Fetal heart rate patterns in patients with thick meconium staining of amniotic fluid and its association with perinatal outcome. Int J Reprod Contracept Obstet Gynecol. 2017;6(3):1030–1035. doi:10.18203/2320-1770.ijrcog20170579
29. Dayal S, Hong PL. Premature Rupture of Membranes. Stat Pearls Publishing; 2019. PMID: 30422483.
30. Rugolo LMSS, Bentlin M, Trindade C. Preeclampsia: effect on the Fetus and Newborn. NeoReviews. 2011;1(12):e198–205. doi:10.1542/neo.12-4-e198
31. Hiersch L, Ashwal E, Aviram A, Gabbay-Benziv R, Wiznitzer A, Yogev Y. 351: Meconium stained amniotic fluid in low risk pregnancies at term – is it really a clinical entity? Am J Obstet Gynecol. 2015;212(1):S185.
32. Gravett C, Eckert LO, Gravett MG, et al. Non-reassuring fetal status: case definition & guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine. 2016;34(49):6084–6092. doi:10.1016/j.vaccine.2016.03.043
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
