Back to Journals » Risk Management and Healthcare Policy » Volume 15
Determinants of Health-Related Quality of Life Among Community-Dwelling Thai Older Adults in Chiang Mai, Northern Thailand
Authors Aung TNN , Moolphate S, Koyanagi Y, Angkurawaranon C , Supakankunti S, Yuasa M, Aung MN
Received 13 May 2022
Accepted for publication 2 August 2022
Published 20 September 2022 Volume 2022:15 Pages 1761—1774
DOI https://doi.org/10.2147/RMHP.S370353
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Mecit Can Emre Simsekler
Thin Nyein Nyein Aung,1,2 Saiyud Moolphate,3 Yuka Koyanagi,4 Chaisiri Angkurawaranon,1,2 Siripen Supakankunti,5 Motoyuki Yuasa,6,7 Myo Nyein Aung6– 8
1Department of Family Medicine, Faculty of Medicine, Chiang Mai University, Chiang Mai, 50200, Thailand; 2Global Health and Chronic Conditions Research Group, Chiang Mai University, Chiang Mai, 50200, Thailand; 3Department of Public Health, Faculty of Science and Technology, Chiang Mai Rajabhat University, Chiangmai, 50300, Thailand; 4Department of Medical and Health Science, Tokyo Ariake University, Tokyo, 135-0063, Japan; 5Centre of Excellence for Health Economics, Faculty of Economics, Chulalongkorn University, Bangkok, 10330, Thailand; 6Department of Global Health Research, Graduate School of Medicine, Juntendo University, Tokyo 113-8421, Japan, and; 7Faculty of International Liberal Arts, Juntendo University, Tokyo, 113-8421, Japan; 8Advanced Research Institute for Health Sciences, Juntendo University, Tokyo, 113-8421, Japan
Correspondence: Myo Nyein Aung, Department of Global Health Research, Graduate School of Medicine, Juntendo University, Tokyo, 113-8421, Japan, Email [email protected]
Background: Population aging has been growing worldwide and Thailand has become an aged society with 20% of its population aged 60 and over. Age-related decline in physical and mental health impacts the health-related quality of life (HRQOL) of older adults.
Purpose: We aimed to describe the HRQOL of Thai older adults, residing in the community.
Methods: This cross-sectional survey was part of a Community-Integrated Intermediary Care project (CIIC), TCTR20190412004. A total of 1509 participants from an intervention arm of a cluster randomized controlled trial were included. A Thai version of the Euro-Qol questionnaire (EQ-5D-5L) was used to determine the HRQOL and associated sociodemographic background, health behaviors and underlying diseases of a representative sample from Maehia, Chiang Mai, Thailand. SPSS version 24 was used to analyze data via descriptive analysis and binary logistic regression.
Results: The mean age of the participants was 69.31± 7.10 years, and nearly a quarter (23.8%) was older than 75 years. The mean EQ index score was 0.81± 0.23 and older age, lower educational attainment, unemployment, lack of exercise habits, current smokers, having history of a fall in the last 6 months, diabetes, hyperlipidemia, dependency assessed using Barthel’s Activity of Daily Living (ADL) Index, and depression using the Geriatric Depression Scale (GDS) were more likely to represent HRQOL-related problems.
Conclusion: Our findings have highlighted the factors affecting the HRQOL of community-dwelling older adults which could be of importance in preparing for active and healthy aging communities. The routine dependency assessment using the ADL index will be useful in estimating the HRQOL of the aging population. Fall prevention programs are also recommended to reduce dependency. Moreover, the association of having diabetes and hyperlipidemia with problems in HRQOL dimensions highlight the need for public health intervention not only to prevent the increasing burden of non-communicable diseases but also to improve the HRQOL of older adults.
Keywords: aging, Community-Integrated Intermediary Care, CIIC, health-related quality of life, HRQOL, Thailand
Introduction
Increasing population aging is a characteristic of the 21st century around the world. Thailand too is experiencing this phenomenon. Thailand ranks fourth behind Japan, South Korea, and Singapore in Asia where aging is the fastest in the world. Thailand has now become an aged society. Life expectancy at birth increased from 74 years in 2010 to 77 years in 2020, and 20% of its population is aged 60 and over. This is estimated to reach over 30% of the total population by 2040.1 The demands on medical and health services will soar with this increased life expectancy due to the chronic diseases and disabilities that accompany old age. A person’s age reflects the duration of time exposed to health risk factors such as smoking and physical inactivity. The increased population of older adults leads to greater demands for prevention and treatment of non-communicable diseases. Moreover, biologically, cells damage over time resulting in weakened immune systems making elderly people prone to becoming a host for different diseases.2 But these biological changes are not consistent and the WHO has indicated that not only genes and personal characteristics but also social changes, such as shifts in social roles and loss of close relationships, can determine the health and well-being of older people as they age. It is important to encourage active aging and aging in place. WHO defines “active aging” as “the process of optimizing opportunities for health, participation and security in order to enhance the quality of life as people age”.3 Maintaining autonomy and independence, improving physical and mental health, social inclusion, and quality of life of all older adults are the key objectives of WHO’s active aging. The concept of aging in place is to encourage the older adults to stay in their original, familiar habitat with a favorable age-friendly environment allowing them to continue to be active members of the community.4,5
Most Thai older adults stay at home, sharing the same house with their children. Institutionalized care or private/public aging homes are not yet popular.6 Co-residence with family is common and family members are the main source of health and material support for the older adults in Thailand. Traditionally, the adult children have to take care of their parents within the concept of generalized reciprocity. This family-based long-term care model is currently practiced in Thailand.7 The older adults mostly stay together with their children and grandchildren, and the contributions they provide to household activities include taking care of grandchildren and giving advice based on Thai customs, values, and beliefs. Such intergenerational families are common to other South East Asian countries like Myanmar and Vietnam, and Thai old people rank their children as their most frequently contacted social ties.8 The recognition and support by the family and community encourage the older adults to be a part of the social development resources in their society, leading to a valued and dignified life. Social ties and a socially active life play an important role in the physical and mental well-being of the older adults which can influence their healthy life expectancy.8,9,52
Quality of life (QOL) is one of the key factors for healthy life expectancy. It is a broad concept which evaluates subjectively the positive and negative aspects of an individual’s life. Age-related decline in physical and mental health impacts upon the health-related quality of life (HRQOL) of older adults. Whilst several studies show that the decline in physical fitness due to aging is evident, one should not assume this as general, since previous levels of physical activity, health-related behaviors and level of academic studies may cast doubt on this association.10–12 The HRQOL becomes an important public health concern, related to both self-reported chronic diseases, which are costly to individuals, families and the health care system, and their risk factors. The HRQOL, as defined by the Center for Disease Control and Prevention is “an individual’s or group’s perceived physical and mental health over time”.13 Measuring the HRQOL of older adults can help determine the burden of preventable diseases and their negative consequences and provide valuable new insights into the associated risk factors. Previous studies have explored more about the quality of life of Thai patients with specific diseases, for example, rheumatoid arthritis, kidney transplantation, or peritoneal dialysis.14,15 Research about HRQOL and its determinants of community-dwelling older adults is still limited. Previous cross-sectional surveys conducted in northern and northeastern Thailand determined the QOL and associated sociodemographic factors and health-related problems of community-dwelling older adults in the rural setting.16,17 International studies assessing the HRQOL of Thai older adults have been carried out using different measurement tools in different settings. Therefore, we aimed to describe the HRQOL, using representative samples from Northern Thailand, of community-dwelling Thai older adults residing in the urban setting, using the Euro-Qol questionnaire (EQ-5D-5L), and investigate the influence of sociodemographic background, health behaviors and underlying diseases on their HRQOL.
Materials and Methods
Study Design, Setting and Study Participants
This cross-sectional survey was part of a Community-Integrated Intermediary Care project (CIIC), TCTR20190412004, analyzing the baseline characteristics of participants from an intervention arm of a cluster randomized controlled trial. The study site was Chiang Mai, Northern Thailand where 18.2% of the total population is comprised of elderly people. The trial consisted of six intervention clusters and six control clusters, recruiting 2000 participants in each arm. The sample size was calculated using STATA version 11SE (Stata Corporation, College Station, TX). The study participants from Maehia subdistrict, Mueang district, Chiang Mai city were selected as the intervention arm by means of cluster randomization. People aged 60 years and above, either male or female, and residents in the study site were recruited with their voluntarily participation and written informed consent. Those who did not consent and those with cognitive impairment or severe impairment in decision-making abilities were excluded. About 2000 resident older adults were screened of which 479 residents of private housing estates (23.95%) declined to participate in the study and 15 people (0.75%) were ineligible. A total 1509 participants were recruited with their written informed consent.
Data Collection Tools, Procedures, and Data Quality Control
The structured questionnaires included demographic characteristics, health behaviors, health status, and research instruments. The research instruments we used were Thai versions of the EQ-5D-5L, Barthel’s Activities of Daily Living (ADL) index, and the Geriatric Depression Scale (GDS). Following the WHO process of translation and adaptation of research instruments, independent language experts translated all study instruments into Thai, back translated into English and retranslated into Thai. Conceptually translated questions were revised many times after investigating the readability and comprehension among the older adults. A pilot study with 30 participants using the Thai version questionnaires was carried out. The research team revised and edited all instruments thoroughly after pilot testing.18 The overall reliability coefficients using Cronbach’s alpha of the EQ-5D-5L, ADL index and GDS were 0.89, 0.90 and 0.80, respectively. Folowing the study protocol and using the interviewer administered survey questionnaires, data collection was undertaken by well-trained research assistants, visiting each household door-to-door for a period of about 6 months in 2019.19 Throughout data collection, the research assistants were supervised at each site, with the completeness and consistency of the filled questionnaires being checked.
Outcome Variables
The main outcome variable was the quality of life, measured by scores of the Thai versions of the Euro-Qol five-dimension five-level (EQ-5D-5L) index and visual analog scale (EQ-VAS).
EQ-5D-5L
The EQ-5D-5L was developed by the EuroQoL group and has been widely used internationally.20 It is a practical, simple and easy to administer tool for the elderly population.21 It has been validated in the Thai setting and widely used.14,15 It is comprised of two parts: a descriptive health classifying system (EQ-5D-5L) and a visual analogue scale (EQ-VAS). The descriptive part assesses the QOL in five dimensions: (i) mobility, (ii) self-care, (iii) usual activities, (iv) pain/discomfort, and (v) anxiety/depression. Each dimension has five levels (1–5) of severity ranging from “no problem” to “severe impairment/unable to”. The digits for the five dimensions can be combined into a 5-digit number that is converted to a single summary index (EQ-5D index) by using the crosswalk calculator with reference to the Thailand value set. The EQ-VAS is a rating scale method to provide a global assessment of self-rated health status “today”, from 0 (worst imaginable health state) to 100 (best imaginable health state).22
Independent Variables
The independent variables included potential factors associated with HRQOL: socio demographic characteristics (age, sex, marital status, educational attainment, employment status); health behaviors (smoking, alcohol, exercise habits); and health status (underlying diseases: hypertension; diabetes; hyperlipidemia, history of a fall in the last 6 months, dependency according to Barthel’s Activities of Daily Living index (ADL), depression according to the Geriatric Depression Scale (GDS)). Age was measured in completed years and it was dichotomized into young-old (younger than 75 years) and old-old (more than or equal to 75 years). Marital status was categorized into two groups: married or not married. Educational attainment was categorized as “completed primary school” or “secondary school and above”. The participants were 60 years old and above with the former government employees having already retired from the government service. Some of the participants, however, continued to work in private companies or in their own business. These participants were grouped as “currently working”, and those who were no longer currently working to earn money were termed as “not currently working”. Regarding health behaviors, the participants who smoked regularly or on some occasions within the previous 3 months were regarded as “Yes” and those who quit or never smoke were defined as “No” for current smoking. Similarly, “Yes” for alcohol drinking status was defined for the participants who drink alcoholic drinks daily or sometimes during the past 3 months, and “No” alcohol drinking for those who never drink or who have quit alcohol. For exercise, “Yes” or “No” was defined according to the WHO physical activity guideline for elderly people. Those who did moderate physical activity for about 150 minutes per week were regarded as “Yes” for exercise, and those who did not exercise or did not meet the recommended hours of physical activity were defined as “No” for exercise in this study.
Barthel’s Activities of Daily Living (ADL) Index
Barthel’s ADL index is a standardized scale commonly used by researchers and validated in the Thai setting.23 The 10 fundamental daily activities for assessment include feeding, grooming, bathing, dressing, bowel and bladder care, toilet use, ambulation, transfer, and climbing stairs. Total ADL scores range from 0 to 20 and are categorized into two groups: severely to moderately dependent (0–11), and mildly dependent to independent (≥12).
Geriatric Depression Scale (GDS)
The assessment of geriatric depression via the Geriatric Depression Scale (GDS) is commonly used by researchers internationally. It is also validated and used in Thailand.24 The GDS short form consists of 15 questions with “yes” or “no” responses. Each response is scored either as 0 or 1 point, with the maximum score being 15. Total scores are categorized into two groups: no depression (GDS total score 0–5), and probable depression (GDS total score 6–15).
Data Management and Analysis
Data were entered, cleaned, validated, and analyzed using IBM SPSS version 24. Sociodemographic characteristics, health behaviors, and health status variables were analyzed using descriptive analysis. Frequency and percentage were used for the categorical variables, stratified by the problems in each dimension of the EQ-5D-5L. The mean (M) and standard deviation (SD) were used for the continuous variables (age, EQ index, and EQ VAS). The mean differences of the EQ index and EQ VAS between different groups were tested using nonparametric statistics (Mann–Whitney U-test or Kruskal–Wallis’s test) as their distributions were not normal. Binary logistic regression was applied to explore the determinants of HRQOL of older adults for problems at each dimension of the EQ-5D-5L. A p value of <0.05 was defined as statistically significant with an adjusted odds ratio (adj OR) at a 95% confidence interval.
Results
Sample Characteristics
The baseline survey results from an intervention arm of a cluster randomized controlled trial consisted of 1509 older adults with a survey response rate of 75.45%. Their mean age was 69.31±7.10 years and nearly a quarter (23.8%) of study participants was older than 75 years. And, 61.8% of the participants were females and the distribution of our study population according to age and sex was comparable with that of Chiang Mai province, as shown in Table 1. Of these participants, 59.8% were married, 61.6% finished primary school, and 69.1% were currently working in private business. Regarding health behaviors and underlying diseases, 6.5% were current smokers and 22.2% did not exercise regularly. Hypertension was the most common underlying disease (46.8%), followed by dyslipidemia (21.5%) and diabetes (17.6%). Of these participants, 10.3% had history of a fall during the previous 6 months, with females comprising a higher prevalence of fall history (64.1%) compared to males (35.9%).
 |
Table 1 Distribution of Respondents According to Age and Sex, Maehia Subdistrict, Chiang Mai, Thailand 2019 |
Dependency Using Barthel’s ADL Index Scoring
The mean ADL total score was 19.23±2.50. Almost all participants (97.7%) were mildly dependent to independent (total ADL scores ≥12), whilst 2.3% had moderate-to-severe dependency (total ADL scores 0–11). The details of ADL scores showed that the dependency in the activities of daily living was highest for bladder control (12.9%), followed by bowel control (7.7%), using stairs (7.1%), mobility (6.0%), transfer (5.6%), toilet use (3.8%), feeding (3.7%), grooming (3.4%), and dressing (2.1%), respectively.
Depression Using the Geriatric Depression Scale
Assessment of geriatric depression using a Thai version of the 15-item GDS scale indicated that 6.5% of the study participants had probable depression (GDS total scores of 6–15), whilst the remaining 93.5% did not have depression (GDS total score 0–5).
HRQOL by EQ-5D-5L
The mean score of the Euro-Qol five-dimension five-level (EQ-5D-5L) index was 0.81±0.23 and that of the visual analog scale (EQ-VAS) was 77.18±14.00. From the results of each level of the five dimensions, shown in Figure 1, the highest proportion of respondents reporting any problems was in Pain/Discomfort (47.7%), followed by Mobility (21.7%), Usual Activities (14.4%), Anxiety/Depression (12.4%), while the lowest percentage was in Self-care (10.5%). Moreover, 24.8% of the study participants reported a “Moderate” problem on at least one dimension, whereas 4.6% of the participants had some form of “Extreme” problem. The characteristics of respondents according to the EQ-5D-5L index and EQ-VAS scores are described in Table 2.
 |
Table 2 Characteristics of Respondents by Euro-QoL Five-Dimension Five-Level (EQ-5D-5L) Index and Visual Analog Scale (EQ-VAS Scores), Maehia Subdistrict, Chiang Mai, Thailand 2019 |
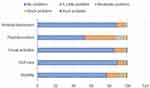 |
Figure 1 Distribution of EQ-5D dimensions among Thai older adults, Maehia subdistrict, Chiang Mai, Thailand 2019. |
Determinants of Reported Problems in Each Dimension of HRQOL
The associated factors affecting the reported problems in each dimension of HRQOL are described in Table 3. Sociodemographic factors significantly affecting the lower HRQOL were older age, lower education, and current employment status. The mean EQ index scores of the older age group (≥75 years) and the younger age group (<75 years) were 0.73±0.27 and 0.84±0.21, respectively, and those of the EQ VAS were 78.31±13.66 and 73.47±14.48, respectively, showing that the older age group had a significantly lower HRQOL both in terms of mean EQ index and EQ VAS compared to the younger age group. It was also associated with problems in all EQ dimensions with the exception of eq5 (anxiety/depression). Gender did not affect the HRQOL as we noted no significant differences in means of the EQ index and EQVAS between males and females, and no significant association with any reported problems in the EQ-5D-5L dimensions. Although there were significant differences in the means of the EQ index (0.83±0.22 vs 0.79±0.25) and EQ-VAS (75.71±14.28 vs 78.16±13.73) between married and unmarried participants, marital status did not significantly relate with problems in any of the EQ-5D-5L dimensions. The mean EQ index among those with lower education (primary education group) vs higher education (secondary and above group) were 0.78±0.24 and 0.87±0.20, respectively, whilst those of the EQ VAS were 76.41±14.55 and 78.41±12.99, respectively. The lower education group was found to be significantly associated with mean differences in both the EQ index and EQ-VAS, and also with reported problems in some EQ dimensions, especially for eq1 (mobility), eq2 (usual activities), and eq4 (pain/discomfort). Participants who were unemployed significantly related to reported problems in eq1 (mobility), as compared to the study participants who were currently working, with the means of the EQ index for these groups being 0.80±0.24 and 0.85±0.20, respectively. The EQ-VAS mean scores of 79.54±13.28 and 76.12±14.19 were significantly different between these two groups.
 |
Table 3 Association Between Participants’ Characteristics and Problems at Euro-QoL Five-Dimensions, Maehia Subdistrict, Chiang Mai, Thailand 2019 |
Regarding health-related behaviors, the means of the EQ index and EQ-VAS were significantly different between the “exercise group” and the “no exercise group”. The “no exercise group” had a mean EQ index score of 0.75±0.31, and an EQ VAS mean score of 71.52±15.01, whilst those of the “exercise group” were 0.83±0.19 and 78.19±13.27, respectively. Moreover, respondents who did not exercise were more likely to report problems across all EQ dimensions with the exception of eq4 (pain/discomfort). Current smokers reported problems relating to eq3 (usual activities) and eq4 (pain/discomfort); however, there were no differences in the EQ index and EQ VAS scores between current smokers and non-smokers.
The EQ index mean scores among the participants with the underlying diseases hypertension, dyslipidemia, and diabetes were 0.79±0.24, 0.76±0.22, and 0.73±0.27, respectively, whereas the EQ index mean scores among the participants with no hypertension, no dyslipidemia, and no diabetes were 0.83±0.22, 0.83±0.23, and 0.83±0.22, respectively. The means of EQ-VAS were significantly lower among those with underlying diseases such as hypertension vs no hypertension (74.62±14.66 vs 79.42±13.00), dyslipidemia vs no dyslipidemia (74.14±14.61 vs 78.01±13.72), and diabetic vs non-diabetic (72.06±13.33 vs 78.27±13.46). When exploring the effects of underlying diseases on the reported problems of EQ dimensions, hypertension did not have any significant effect on the problems of EQ-5D-5L. However, having dyslipidemia was significantly associated with problems in eq4 (pain/discomfort), and those with diabetes were more likely to have problems in all EQ dimensions which were significantly higher than non-diabetic participants.
Having history of a fall in the previous 6 months was significantly associated with problems in all EQ dimensions except eq2 (self-care), and significant differences in the means of the EQ index (0.68±0.28 vs 0.83±0.22) and EQ-VAS (74.65±14.47 vs 77.47±13.92) were noted between those participants with history of fall and no history of a fall in the previous 6 months. The ambulatory status of the participants, as described by Barthel’s ADL index significantly affected the means of the EQ index and EQ-VAS. The participants with moderate-to-severe dependency (ADL<12) had lower means of both the EQ index and EQ-VAS compared to those with no dependency (ADL>12) (0.33±0.53 vs 0.82±0.20 and 63.12±15.83 Vs 77.50±13.79, respectively). ADL scores <12 was significantly associated with problems with eq2 (self-care) and eq3 (usual activities). Having probable depression (GDS>6) was significantly associated with lower means of both the EQ index and EQ-VAS when compared to those with no depression (0.53±0.37 vs 0.83±0.20 and 67.71±16.89 vs 77.83±13.45 respectively). Moreover, the participants classified as depressed had significant problems in all EQ dimensions.
Discussion
We tried to describe the HRQOL of community-dwelling older adults, residing in northern Thailand, expressed in the EQ-5D-5L, via the EQ index and EQ VAS values. The mean of the EQ index of our study participants was 0.81±0.23 and that of the EQ VAS was 77.18±14.00. When compared to another study of Thai older adults in a rural area of northeastern Thailand, the EQ index mean of our study participants was lower (0.81 vs 0.84), whereas the EQ VAS mean was higher (77.18 vs 70.28).25 The health-related quality of life of our study population was significantly affected not only by their sociodemographic background but also by their underlying diseases, history of a fall in the previous 6 months, and ambulatory status, reflected by their activities of daily living scores.
We observed that older age, not surprisingly, negatively affects the HRQOL in all EQ dimensions with the exception of the anxiety/depression domain. This finding is comparable to another study of elderly Vietnamese people where the EQ index mean score of 0.87 and lower HRQOL was associated with older age.26 If their living conditions are satisfactory, increasing age may not have negative impacts on an elderly person’s mental health, especially in relation to anxiety/depression. Therefore, it is important to limit the impact of age on physical health in order to give the aging population a higher HRQOL. Unlike some previous studies,27–29 we noted that the gender and marital status of the present study participants were not significantly associated with the problems in any of the EQ dimensions despite the significant mean differences in the EQ index and EQ VAS mean scores between married and unmarried participants. Education is one of the social determinants of health and represents an important indicator which may directly or indirectly influence HRQOL through its association with higher social class and economic status. We noted those with lower education had a lower HRQOL compared to those with higher education, a finding which is consistent with other studies.30,31 Moreover, the participants who were currently working had a better HRQOL in comparison with those who were not working. Higher education and current employment may be related with having higher awareness of a healthy lifestyle and easier access to health care services, leading to improved physical health and a higher HRQOL.32
Regarding health risk behaviors, the participants who exercise regularly had a better HRQOL, whilst current smokers had more problems in relation to the EQ dimensions. This is consistent with the findings of other studies.33–35 Exercise has positive impacts on a person’s HRQOL by improving physical health in terms of enhanced resistance to illness, increased functional independence, and delayed onset of diabetes or hypertension.36 Non-communicable diseases are on an increasing trend generally and especially among the old age population. This can lead to the double burden of both the negative consequences of NCDs and increased age-related dependency. Aging is associated with progressive degeneration of tissue and is the most common known risk factor for many chronic diseases.37 Diabetes is a common chronic disease with older diabetic people more at risk of diabetes-related complications. They often have one or more coexisting conditions, such as cognitive impairment, which impacts negatively on diabetes education and management. Diabetes, its complications and its symptoms, adversely affects a person’s overall health and HRQOL.38–40 The prevalence of diabetes (17.6%) in our study population was higher than the national figure for Thailand which was 9.6% in 201641 The negative impact of having diabetes on the HRQOL of the elderly participants, as found in this study, is consistent with other studies carried out in Thailand.14,42,43 Healthy life expectancy is crucial for older adults in the era of population aging and the direct consequences from complications of diabetes could make them dependent, further impair their activities of daily living, and lead to subsequent problems across all EQ dimensions. Dyslipidemia is common in Thailand with 66.5% of Thais having some form of this disease.44 This study’s finding of its association with poor HRQOL is of importance in terms of designing health promotion activities to reduce the subsequent NCDs burden and improve the HRQOL of older adults. Other studies support our findings that depression is closely related to poor HRQOL, depressed older adults have a lower HRQOL than those with other chronic medical conditions31,45 and subjective happiness and life satisfaction determine the level of HRQOL among depressed older adults.46
Our study noted that those study participants who had history of a fall in the previous 6 months had a lower HRQOL than participants without a fall, which is similar to the finding in other studies.17,47 The prevalence of a fall in the 6 months before the date of the interview was 10.3% of our study participants. This is higher than the overall prevalence of a fall among elderly people in the northern region of Thailand (5.5%).48 Consistent with other studies, female study participants had a fall prevalence which was higher than their male counterparts (64.1% vs 35.9%), owing to gender-defined differences in terms of bone density and muscle strength.49,50 A fall has several negative consequences, including fall-related injuries, adverse psychosocial effects, such as fear of falling, limited physical activity, and impaired HRQOL.53 The incidence of falls can result in raised dependency leading to an increased family burden and greater healthcare expenditures. Measuring disabilities is an important indicator of the level of the elderly person’s independence and their needs for social care services. Our study found that participants with higher EQ index and EQ VAS mean scores had higher ADL scores, and those with lower ADL scores had more problems in relation to some EQ-5D dimensions. This supports a previous study finding that independence in the ADL has positive impacts on an elderly person’s HRQOL.51
This study has several limitations. One limitation is the cross-sectional nature of the study. We explored the current perception of HRQOL of older adults, but the causal relationship and long-term effects of the determinants of HRQOL were not explored. Furthermore, regarding the underlying diseases, the questionnaires asked whether the participants had those diseases or not. The duration of chronic diseases was not explored in this study, which might affect the participants’ HRQOL. Additionally, people with cognitive impairment were excluded from our research, yet this population might represent an important portion of the older adult population. By our exclusion, there could be some limitations to the generalizability of our research findings. However, a community survey of home-dwelling older adult residents via door-to-door contact prior to the COVID-19 pandemic is a strength of this study. It is a good representation of Chiang Mai, which is the most populated province in Northern Thailand where 18.2% of the entire population are older adults. Moreover, this survey provided an additional insight into how certain diseases and disease states impact the quality of life for older adults, which could be an important resource for future public health interventions.
Conclusion
The findings from this study have highlighted the state of the health-related quality of life among community-dwelling older adults and the factors determining problems across EQ dimensions. It supports the preexisting findings relating to the negative impacts of sociodemographic background and dependency status on HRQOL. Moreover, having diabetes and its adverse effects on problems across all EQ dimensions is an important and alarming feature for public health practitioners, not only to prevent complications of NCDs but also to promote active and healthy aging with increased healthy life expectancy. Fall risk assessment, home modification, and fall prevention exercise programs are recommended for ambulatory community residents, as poor HRQOL was significantly noted among those with a history of falls. Future research should devise a community-based health promotion program, such as a group exercise program, in order to improve physical activity, promote socializing with peers, and prevent dependency, leading to a subsequent increase in HRQOL. Our findings can help health policy makers design strategies to provide effective intervention within a community setting for healthy aging in place of Thai community-dwelling older adults population.
Data Sharing Statement
The individual deidentified participant data presented in this study are available on request from the corresponding author. The data are not publicly available because this study was a subgroup analysis of baseline data of an intervention cluster from a cluster randomized trial and the final analysis was ongoing and publications of the whole cluster randomized trial has not yet finished.
Ethical Approval and Informed Consent
This study was conducted according to the Declaration of Helsinki. The research project was approved by the World Health Organization (WHO) Ethical Review Committee (WHO/ERC ID; ERC.0003064) and Boromrajonani College of Nursing, Lampang, Thailand Ethics Review Committee (E2562/005). It has been registered in the Thailand Clinical Trial Registry, with trial registration number TCTR20190412004.
Acknowledgments
The study participants, village health volunteers, head nurses of primary care units – Mueang Chiang Mai, Thailand; Mayor of Maehia municipality, Mueang Chiang Mai, Thailand; and The Faculty of Science and Technology, Chiang Mai Rajabhat University, Chiang Mai, Thailand – are acknowledged for their contribution to and cooperation in this study. Richard Lawrence Mann is acknowledged for refining the English.
Funding
This research was supported by the World Health Organization Centre for Health Development (WHO Kobe Centre – WKC: K18020). This research was partially supported by the Chiang Mai University (TNNA, CA).
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Bank. Country Profile Thailand; 2020.
2. Weiskopf D, Weinberger B, Grubeck‐Loebenstein B. The aging of the immune system. Transpl Int. 2009;22(11):1041–1050. doi:10.1111/j.1432-2277.2009.00927.x
3. World Health Organization. Active ageing: a policy framework. Geneva: World Health Organization; 2002.
4. Löfqvist C, Granbom M, Himmelsbach I, Iwarsson S, Oswald F, Haak M. Voices on relocation and aging in place in very old age—a complex and ambivalent matter. Gerontologist. 2013;53(6):919–927. doi:10.1093/geront/gnt034
5. Aung MN, Koyanagi Y, Ueno S, Tiraphat S, Yuasa M. A contemporary insight into an age-friendly environment contributing to the social network, active ageing and quality of life of community resident seniors in Japan. J Aging Environ. 2020;35:1–16.
6. Glinskaya EEW, Wanniarachchi T, Jinadhi T. Labor markets and social policy in a rapidly transforming: caring for Thailand’s aging population. AUS0002170. Thailand; 2021: 54.
7. Aung TNN, Aung MN, Moolphate S, Koyanagi Y, Supakankunti S, Yuasa M. Caregiver burden and associated factors for the respite care needs among the family caregivers of community dwelling senior citizens in Chiang Mai, Northern Thailand. Int J Environ Res Public Health. 2021;18(11):5873. doi:10.3390/ijerph18115873
8. Aung MN, Moolphate S, Aung TNN, Katonyoo C, Khamchai S, Wannakrairot P. The social network index and its relation to later-life depression among the elderly aged≥ 80 years in Northern Thailand. Clin Interv Aging. 2016;11:1067. doi:10.2147/CIA.S108974
9. Kawachi I, Berkman LF. Social ties and mental health. J Urban Health. 2001;78:458–467. doi:10.1093/jurban/78.3.458
10. Milanović Z, Pantelić S, Trajković N, Sporiš G, Kostić R, James N. Age-related decrease in physical activity and functional fitness among elderly men and women. Clin Interv Aging. 2013;8:549–556. doi:10.2147/cia.s44112
11. Notthoff N, Reisch P, Gerstorf D. Individual characteristics and physical activity in older adults: a systematic review. Gerontology. 2017;63(5):443–459. doi:10.1159/000475558
12. Anokye NK, Trueman P, Green C, Pavey TG, Taylor RS. Physical activity and health related quality of life. BMC Public Health. 2012;12(1):1–8. doi:10.1186/1471-2458-12-624
13. Prevention C.f.D.C.a. Measuring healthy days: population assessment of health-related quality of life; 2001.
14. Sakthong P, Sonsa-Ardjit N, Sukarnjanaset P, Munpan W. Psychometric properties of the EQ-5D-5L in Thai patients with chronic diseases. Qual Life Res. 2015;24(12):3015–3022. doi:10.1007/s11136-015-1038-z
15. Kimman M, Vathesatogkit P, Woodward M, et al. Validity of the Thai EQ-5D in an occupational population in Thailand. Qual Life Res. 2013;22(6):1499–1506. doi:10.1007/s11136-012-0251-2
16. Yodmai K, Somrongthong R, Kumar R. Determinants of quality of life among rural elderly population in Khonkean province of Thailand. J Liaquat Uni Med Health Sci. 2018;17:180–184.
17. Taburee W, Sirilak S, Khotcharrat R, et al. Health-related problems and drivers of health-related quality of life among community-dwelling older adults. J Prim Care Community Health. 2020;11:2150132720913724. doi:10.1177/2150132720913724
18. World Health Organization. Process of translation and adaptation of instruments; 2009. Available from: http://www.who.int/substance_abuse/research_tools/translation/en/.
19. Aung NM, Moolphate S, Yuasa M, et al. Community-Integrated Intermediary Care (CIIC) Service Model to Enhance Family-Based, Long-Term Care for Older People: Protocol for a Cluster Randomized Controlled Trial in Thailand. JMIR Res Protoc. 3/24 2021;10(3):e20196.
20. Devlin NJ, Brooks R. EQ-5D and the EuroQol group: past, present and future. Appl Health Econ Health Policy. 2017;15(2):127–137. doi:10.1007/s40258-017-0310-5
21. Holland R, Smith RD, Harvey I, Swift L, Lenaghan E. Assessing quality of life in the elderly: a direct comparison of the EQ‐5D and AQoL. Health Econ. 2004;13(8):793–805. doi:10.1002/hec.858
22. van Reenen M, Janssen B. EQ-5D-5L User Guide: Basic Information on How to Use the EQ-5D-5L Instrument. Rotterdam: EuroQol Research Foundation; 2015.
23. Wade D, Collin C. The Barthel ADL Index: a standard measure of physical disability? Int Disabil Stud. 1988;10(2):64–67. doi:10.3109/09638288809164105
24. Greenberg SA. The geriatric depression scale (GDS). Best Pract Nurs Care Older Adults. 2012;4:1–2.
25. Rachasrimuang S, Bumrerraj S. Effectiveness of a home visit programme by youth volunteers on health-related quality of life and depression among elderly persons: results from a cluster randomized controlled trial in Rural Thailand. J Med Assoc Thai. 2018;101:S189–S195.
26. Huong NT, Ha LTH, Tien TQ. Determinants of health-related quality of life among elderly: evidence from Chi Linh Town, Vietnam. Asia Pac J Public Heath. 2017;29(5_suppl):84S–93S. doi:10.1177/1010539517704041
27. Hoi LV, Chuc NTK, Lindholm L. Health-related quality of life, and its determinants, among older people in rural Vietnam. BMC Public Health. 2010;10(1):549. doi:10.1186/1471-2458-10-549
28. Pengpid S, Peltzer K. The impact of chronic diseases on the quality of life of primary care patients in Cambodia, Myanmar and Vietnam. Iran J Public Health. 2018;47(9):1308–1316.
29. Somrongthong R, Wongchalee S, Ramakrishnan C, Hongthong D, Yodmai K, Wongtongkam N. Influence of socioeconomic factors on daily life activities and quality of life of Thai elderly. J Public Health Res. 2017;6:21.
30. Lasheras C, Patterson AM, Casado C, Fernandez S. Effects of education on the quality of life, diet, and cardiovascular risk factors in an elderly Spanish community population. Exp Aging Res. 2001;27(3):257–270. doi:10.1080/036107301300208691
31. Tajvar M, Arab M, Montazeri A. Determinants of health-related quality of life in elderly in Tehran, Iran. BMC Public Health. 2008;8(1):1–8. doi:10.1186/1471-2458-8-323
32. Pengpid S, Peltzer K. Chronic conditions, multimorbidity, and quality of life among patients attending monk healers and primary care clinics in Thailand. Health Qual Life Outcomes. 2021;19(1):61. doi:10.1186/s12955-021-01707-x
33. Heyworth ITM, Hazell ML, Linehan MF, Frank TL. How do common chronic conditions affect health-related quality of life? Br J Gen Pract. 2009;59(568):e353–e358. doi:10.3399/bjgp09X453990
34. Tillmann M, Silcock J. A comparison of smokers’ and ex-smokers’ health-related quality of life. J Public Health Med. 1997;19(3):268–273. doi:10.1093/oxfordjournals.pubmed.a024629
35. Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ. 1998;316(7133):736–741. doi:10.1136/bmj.316.7133.736
36. Ellingson T, Conn VS. Exercise and quality of life in elderly individuals. J Gerontol Nurs. 2000;26(3):17–25. doi:10.3928/0098-9134-20000301-06
37. MacNee W, Rabinovich RA, Choudhury G. Ageing and the border between health and disease. Eur Respir J. 2014;44(5):1332. doi:10.1183/09031936.00134014
38. Peyrot.; RRRM. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15(3):205–218. doi:10.1002/(SICI)1520-7560(199905/06)15:3<205::AID-DMRR29>3.0.CO;2-O
39. Trikkalinou A, Papazafiropoulou AK, Melidonis A. Type 2 diabetes and quality of life. World J Diabetes. 2017;8(4):120. doi:10.4239/wjd.v8.i4.120
40. Sinclair A, Saeedi P, Kaundal A, Karuranga S, Malanda B, Williams R. Diabetes and global ageing among 65–99-year-old adults: findings from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract. 2020;162:108078. doi:10.1016/j.diabres.2020.108078
41. World Health Organization (WHO). Diabetes country profiles, 2016. Thailand; 2016.
42. Pattanaphesaj J, Thavorncharoensap M. Measurement properties of the EQ-5D-5L compared to EQ-5D-3L in the Thai diabetes patients. Health Qual Life Outcomes. 2015;13(1):1–8. doi:10.1186/s12955-014-0203-3
43. Choowattanapakorn T, Karuna R, Konghan S, Tangmettajittakun D. Factors predicting quality of life in older people with diabetes in Thailand. Songklanakarin J Sci Technol. 2016;38:61.
44. Aekplakorn W, Taneepanichskul S, Kessomboon P, et al. Prevalence of dyslipidemia and management in the Thai population, National Health Examination Survey IV, 2009. J Lipids. 2014;2014:5.
45. Unützer J, Patrick DL, Diehr P, Simon G, Grembowski D, Katon W. Quality adjusted life years in older adults with depressive symptoms and chronic medical disorders. Int Psychogeriatr. 2000;12(1):15–33. doi:10.1017/S1041610200006177
46. Jorm A. The epidemiology of depressive states in the elderly: implications for recognition, intervention and prevention. Soc Psychiatry Psychiatr Epidemiol. 1995;30(2):53–59. doi:10.1007/BF00794942
47. Thiem U, Klaaßen-Mielke R, Trampisch U, Moschny A, Pientka L, Hinrichs T. Falls and EQ-5D rated quality of life in community-dwelling seniors with concurrent chronic diseases: a cross-sectional study. Health Qual Life Outcomes. 2014;12(1):2. doi:10.1186/1477-7525-12-2
48. National Statistical Office. Report on the 2017 survey of the older persons in Thailand; 2018.
49. Khongboon P, Kespichayawatt J. Accidental falls and associated factors among the elderly in Thailand: a national cross-sectional study in 2007, 2011, 2014 and 2017. J Health Res. 2021. doi:10.1108/JHR-07-2020-0308
50. Romli MH, Tan MP, Mackenzie L, Lovarini M, Suttanon P, Clemson L. Falls amongst older people in Southeast Asia: a scoping review. Public Health. 2017;145:96–112. doi:10.1016/j.puhe.2016.12.035
51. Hongthong D, Somrongthong R, Ward P. Factors influencing the Quality of Life (QoL) among Thai older people in a rural area of Thailand. Iran J Public Health. 2015;44(4):479.
52. Aung MN, Koyanagi Y, Ueno S, Tiraphat S, Yuasa M. Age‐Friendly Environment and Community‐Based Social Innovation in Japan: A Mixed‐Method Study. Gerontologist. 2022;62(1):89–99. doi:10.1093/geront/gnab121
53. Aung TNN, Moolphate S, Koyanagi Y, et al. Depression and Associated Factors among Community‐Dwelling Thai Older Adults in Northern Thailand: The Relationship between History of Fall and Geriatric Depression. Int J Environ Res Public Health. 2022;19(17):10574. Published 2022 Aug 25. doi:10.3390/ijerph191710574
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
